Preliminary Evidence of the Efficacy of Nitric Acid Treatment in Onychomycosis
Abstract
:1. Introduction
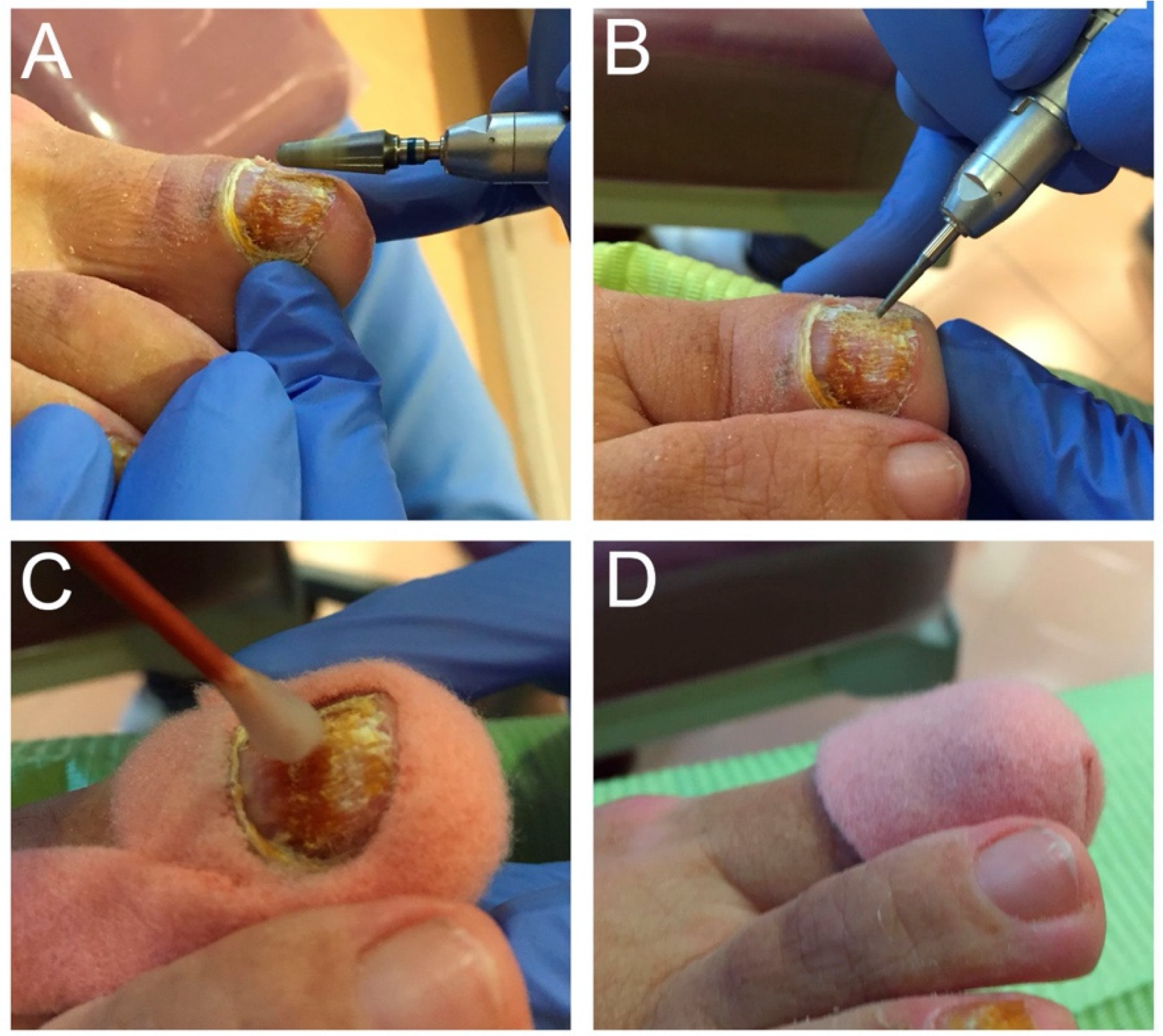
2. Materials and Methods
2.1. Patients
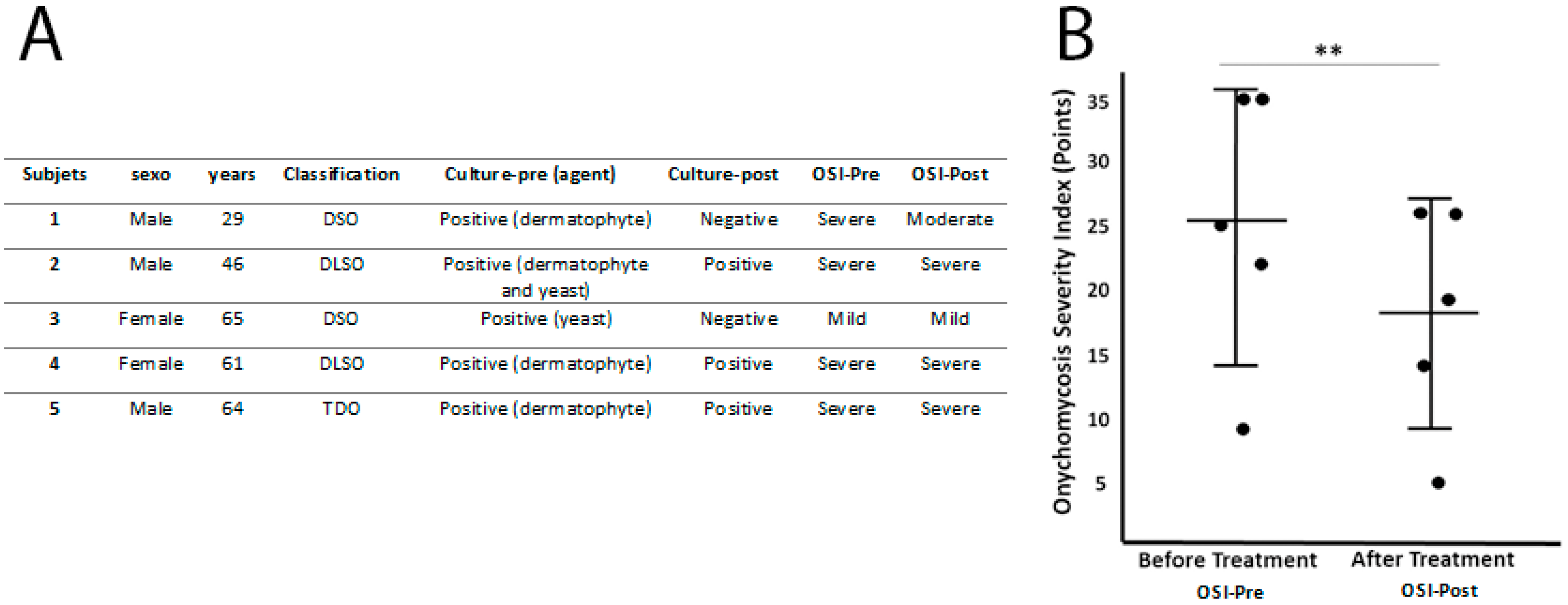
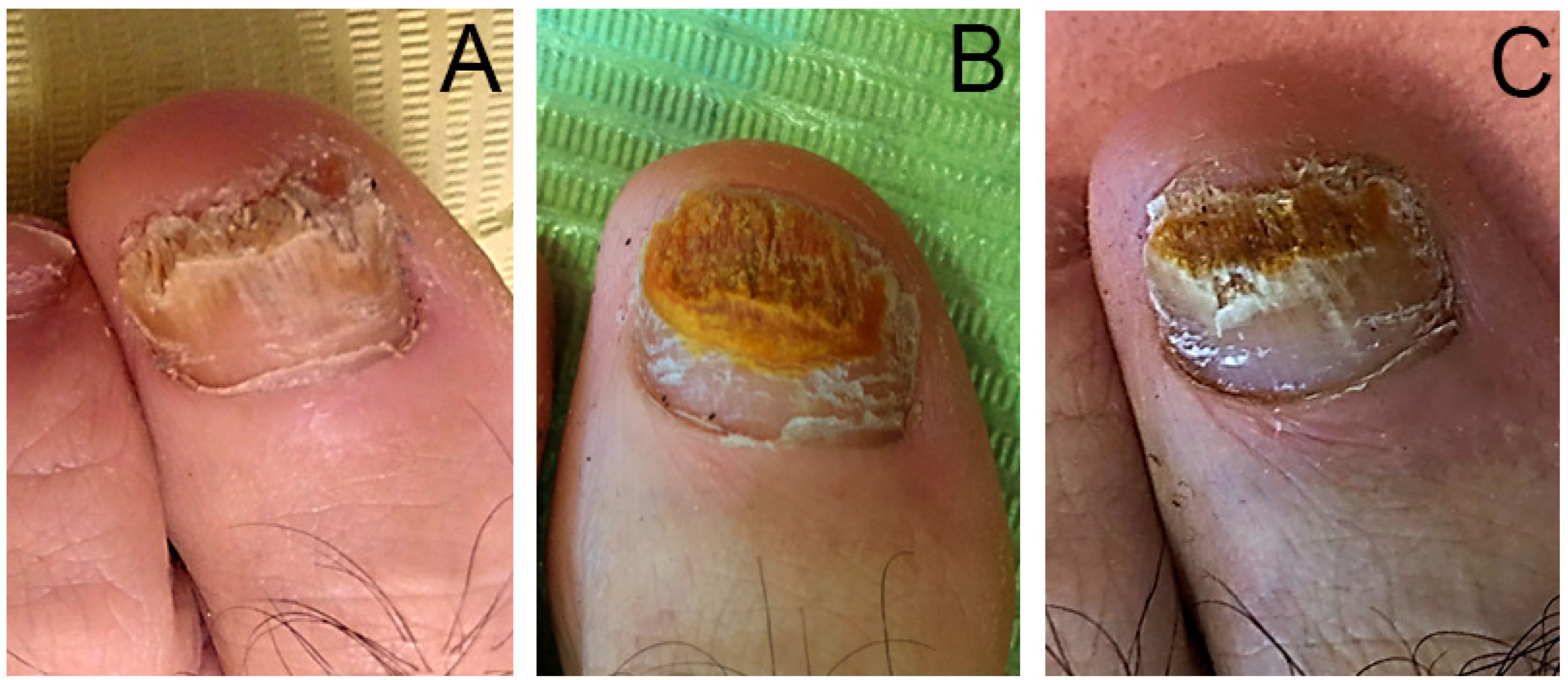
2.2. Clinical Evaluation
2.3. Treatment
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gupta, A.K.; Versteeg, S.G.; Shear, N.H. Onychomycosis in the 21st Century: An Update on Diagnosis, Epidemiology, and Treatment. J. Cutan. Med. Surg. 2017, 21, 525–539. [Google Scholar] [CrossRef] [PubMed]
- Tchernev, A.P.G.; Penev, P.K.; Nenoff, M.P.; Zisova, A.P.L.G.; Cardoso, J.C.; Taneva, T.; Ginter-Hanselmayer, A.P.G.; Ananiev, J.; Gulubova, A.P.M.; Hristova, R.; et al. Onychomycosis: Modern diagnostic and treatment approaches. Wien. Med. Wochenschr. 2012, 163, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lipner, S.R.; Scher, R.K. Onychomycosis. J. Am. Acad. Dermatol. 2018, 80, 835–851. [Google Scholar] [CrossRef] [PubMed]
- Dogra, A.; Arora, A.K. Nail psoriasis: The journey so far. Indian J. Dermatol. 2014, 59, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Rich, P.; Elewski, B.; Scher, R.K.; Pariser, D. Diagnosis, Clinical Implications, and Complications of Onychomycosis. Semin. Cutan. Med. Surg. 2013, 32, S5–S8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scher, R.K.; Rich, P.; Elewski, B.; Pariser, D. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin. Cutan. Med. Surg. 2013, 32, S2–S4. [Google Scholar] [CrossRef] [PubMed]
- Chacon, A.; Franca, K.; Fernandez, A.; Nouri, K. Psychosocial impact of onychomycosis: A review. Int. J. Dermatol. 2013, 52, 1300–1307. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K.; Mays, R.R. The Impact of Onychomycosis on Quality of Life: A Systematic Review of the Available Literature. Ski. Appendage Disord. 2018, 4, 208–216. [Google Scholar] [CrossRef]
- Achterman, R.R.; White, T.C. A Foot in the Door for Dermatophyte Research. PLOS Pathog. 2012, 8, e1002564. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.K.; Daigle, D.; Carviel, J.L. The role of biofilms in onychomycosis. J. Am. Acad. Dermatol. 2016, 74, 1241–1246. [Google Scholar] [CrossRef]
- Gupta, A.K.; Cernea, M.; Foley, K.A. Improving Cure Rates in Onychomycosis. J. Cutan. Med. Surg. 2016, 20, 517–531. [Google Scholar] [CrossRef]
- Leelavathi, M.; Noorlaily, M. Onychomycosis nailed. Malays. Fam Physician 2014, 9, 2–7. [Google Scholar] [PubMed]
- Lipner, S.R.; Scher, R.K. Onychomycosis. J. Am. Acad. Dermatol. 2018, 80, 853–867. [Google Scholar] [CrossRef] [PubMed]
- Francuzik, W.; Fritz, K.; Salavastru, C. Laser therapies for onychomycosis - critical evaluation of methods and effectiveness. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 936–942. [Google Scholar] [CrossRef]
- Finnen, M.; Hennessy, A.; McLean, S.; Bisset, Y.; Mitchell, R.; Megson, I.; Weller, R. Topical application of acidified nitrite to the nail renders it antifungal and causes nitrosation of cysteine groups in the nail plate. Br. J. Dermatol. 2007, 157, 494–500. [Google Scholar] [CrossRef]
- Nova, A.M.; Marcos-Tejedor, F.; Martín, B.G.; Sánchez-Rodríguez, R.; Escamilla-Martínez, E. Bioceramic-fiber socks have more benefits than cotton-made socks in controlling bacterial load and the increase of sweat in runners. Text. Res. J. 2017, 88, 696–703. [Google Scholar] [CrossRef]
- Marcos-Tejedor, F.; Sánchez-Rodríguez, R.; Mayordomo, R.; Martínez-Nova, A. The bacteriostatic effect of controlled-flux electrolyzed acidic solution on healthy hallucal skin. J. Tissue Viability 2019, 29, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Conforti, F.; Statti, G.; Tundis, R.; Bianchi, A.; Agrimonti, C.; Sacchetti, G.; Andreotti, E.; Menichini, F.; Poli, F. Comparative chemical composition and variability of biological activity of methanolic extracts from Hypericum perforatum L. Nat. Prod. Res. 2005, 19, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Altıparmak, M.; Eskitaşçıoğlu, T. Comparison of Systemic and Topical Hypericum Perforatum on Diabetic Surgical Wounds. J. Investig. Surg. 2016, 31, 29–37. [Google Scholar] [CrossRef]
- Soares, F.; Fernandes, C.; Silva, P.; Pereira, L.; Gonçalves, T. Antifungal activity of carrageenan extracts from the red alga Chondracanthus teedei var. lusitanicus. Environ. Boil. Fishes 2016, 28, 2991–2998. [Google Scholar] [CrossRef]
- Marcos-Tejedor, F.; González-García, P.; Mayordomo, R. Solubilization in vitro of tea tree oil and first results of antifungal effect in onychomycosis. Enfermedades Infecc. y Microbiol. Clin. (English ed.) 2021, 39, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Carney, C.; Tosti, A.; Daniel, R.; Scher, R.; Rich, P.; DeCoster, J.; Elewski, B. A New Classification System for Grading the Severity of Onychomycosis. Arch. Dermatol. 2011, 147, 1277–1282. [Google Scholar] [CrossRef] [PubMed]
- Price, D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef]
- Effendy, I.; Lecha, M.; De Chauvin, M.F.; Di Chiacchio, N.; Baran, R. Epidemiology and clinical classification of onychomycosis. J. Eur. Acad. Dermatol. Venereol. 2005, 19, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, H.; Miyata, K.; Sugita, T.; Hiruma, M.; Hiruma, M. Treatment of Onychomycosis Using a 1064nm Nd: YAG Laser. Med. Mycol. J. 2013, 54, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Marcos-Tejedor, F.; Mayordomo, R.; Pico, A.P.; Cantero-Garlito, P.; Iglesias-Sánchez, M. Quantitative Evaluation of the Clinical Evolution of Traumatic Onycholysis after Laser Treatment. Appl. Sci. 2021, 11, 6817. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcos-Tejedor, F.; Santos-Carnicero, N.; Mayordomo, R. Preliminary Evidence of the Efficacy of Nitric Acid Treatment in Onychomycosis. Int. J. Environ. Res. Public Health 2021, 18, 13371. https://doi.org/10.3390/ijerph182413371
Marcos-Tejedor F, Santos-Carnicero N, Mayordomo R. Preliminary Evidence of the Efficacy of Nitric Acid Treatment in Onychomycosis. International Journal of Environmental Research and Public Health. 2021; 18(24):13371. https://doi.org/10.3390/ijerph182413371
Chicago/Turabian StyleMarcos-Tejedor, Félix, Natividad Santos-Carnicero, and Raquel Mayordomo. 2021. "Preliminary Evidence of the Efficacy of Nitric Acid Treatment in Onychomycosis" International Journal of Environmental Research and Public Health 18, no. 24: 13371. https://doi.org/10.3390/ijerph182413371
APA StyleMarcos-Tejedor, F., Santos-Carnicero, N., & Mayordomo, R. (2021). Preliminary Evidence of the Efficacy of Nitric Acid Treatment in Onychomycosis. International Journal of Environmental Research and Public Health, 18(24), 13371. https://doi.org/10.3390/ijerph182413371







