Parks and the Pandemic: A Scoping Review of Research on Green Infrastructure Use and Health Outcomes during COVID-19
Abstract
:1. Introduction
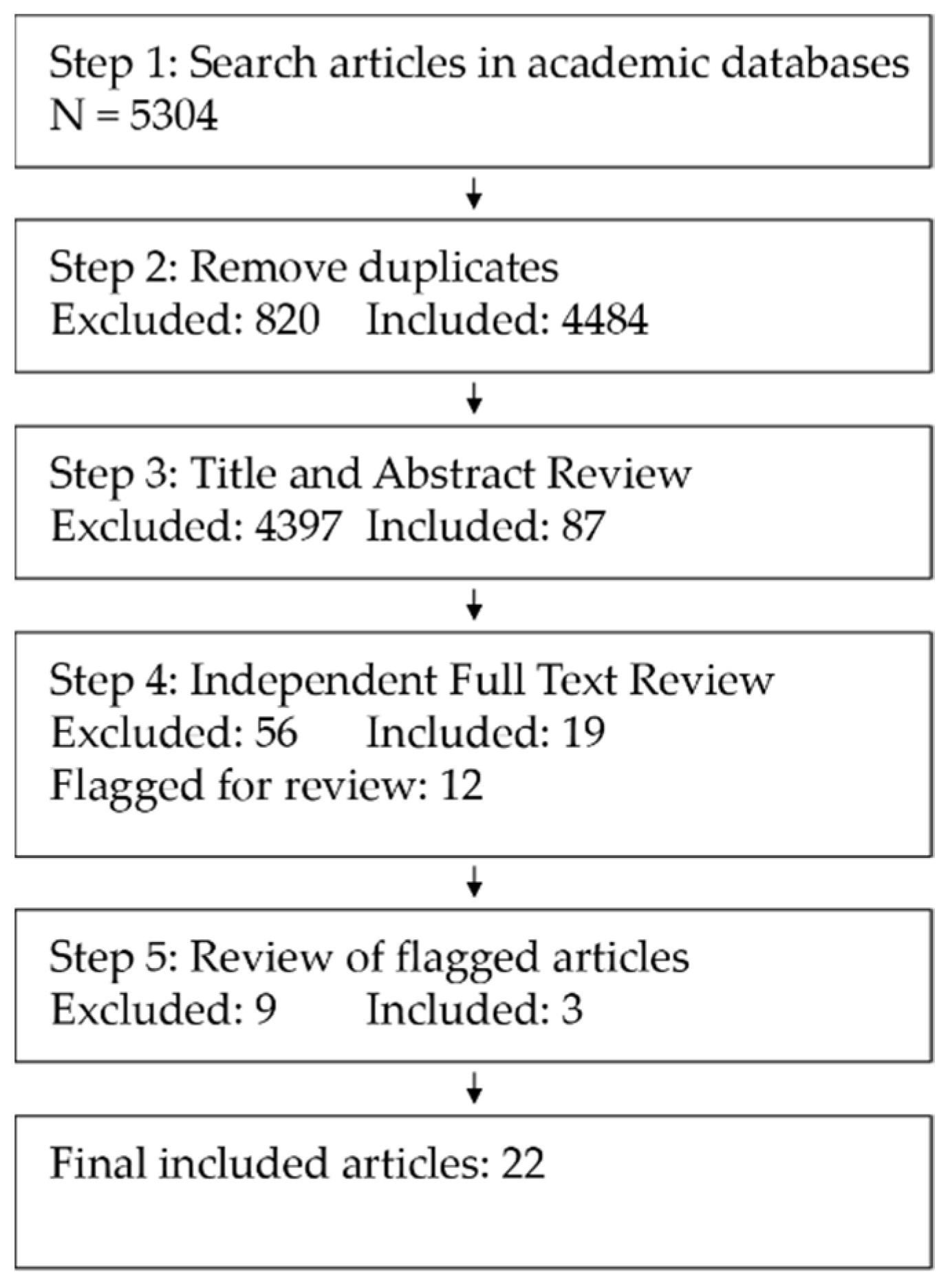
2. Materials and Methods
3. Results
3.1. Theme 1: Studies Exploring the Impact of GI Use on COVID-19-Specific Health Outcomes
3.2. Studies Using GI as Explanatory Variables to Understand Other Health Outcomes within the Context of the Pandemic
4. Discussion
4.1. Impacts of GI Use on COVID-19-Related Health Outcomes
4.2. Impacts of GI on Non-COVID-19 Health Outcomes within the Pandemic
4.3. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Details of Included Articles
| Author (Year) | Title | Theme |
|---|---|---|
| Casa Nova et al. (2021) [29] | Are mobility and COVID-19 related? A dynamic analysis for Portuguese districts | Theme 1: COVID-specific Outcomes |
| DePhillipo et al. (2021) [30] | Mobile phone GPS data and prevalence of COVID-19 infections: Quantifying parameters of social distancing in the U.S. | Theme 1: COVID-specific Outcomes |
| Johnson et al. (2021) [31] | Associations between COVID-19 transmission rates, park use, and landscape structure | Theme 1: COVID-specific Outcomes |
| Kartal, Depren, and Depren (2021) [32] | The relationship between mobility and COVID-19 pandemic: Daily evidence from an emerging country by causality analysis | Theme 1: COVID-specific Outcomes |
| Noland (2021) [33] | Mobility and the effective reproduction rate of COVID-19 | Theme 1: COVID-specific Outcomes |
| Praharaj and Han (2021) [34] | Human mobility impacts on the surging incidence of COVID-19 in India | Theme 1: COVID-specific Outcomes |
| Tyrovolas et al. (2021) [35] | Estimating the COVID-19 spread through real-time population mobility patterns: Surveillance in low- and middle-income countries | Theme 1: COVID-specific Outcomes |
| Corley et al. (2021) [36] | Home garden use during COVID-19: Associations with physical and mental wellbeing in older adults | Theme 2: Non-COVID Health Outcomes |
| Gola et al. (2021) [37] | Influence of Nature at the Time of the Pandemic: An Experience-Based Survey at the Time of SARS-CoV-2 to Demonstrate How Even a Short Break in Nature Can Reduce Stress for Healthcare Staff | Theme 2: Non-COVID Health Outcomes |
| Heo et al. (2021) [38] | Impact of changed use of greenspace during COVID-19 pandemic on depression and anxiety | Theme 2: Non-COVID Health Outcomes |
| Hubbard et al. (2021) [39] | Are rurality, area deprivation, access to outside space, and green space associated with mental health during the COVID-19 pandemic? A cross sectional study (charis-e) | Theme 2: Non-COVID Health Outcomes |
| Jackson et al. (2021) [40] | Outdoor Activity Participation Improves Adolescents’ Mental Health and Well-Being during the COVID-19 Pandemic | Theme 2: Non-COVID Health Outcomes |
| Lee et al. (2021) [41] | Influence of forest visitors’ perceived restorativeness on social–psychological stress | Theme 2: Non-COVID Health Outcomes |
| Lehberger, Kleih and Sparke (2021) [42] | Self-reported well-being and the importance of green spaces—A comparison of garden owners and non-garden owners in times of COVID-19 | Theme 2: Non-COVID Health Outcomes |
| Longman et al. (2021) [43] | Time in nature associated with decreased fatigue in UK truck drivers | Theme 2: Non-COVID Health Outcomes |
| Marques et al. (2021) [44] | Home gardens can be more important than other urban green infrastructure for mental well-being during COVID-19 pandemics | Theme 2: Non-COVID Health Outcomes |
| Mayen Huerta and Utomo (2021) [45] | Evaluating the association between urban green spaces and subjective well-being in Mexico city during the COVID-19 pandemic | Theme 2: Non-COVID Health Outcomes |
| Pearson et al. (2021) [46] | Increased use of porch or backyard nature during COVID-19 associated with lower stress and better symptom experience among breast cancer patients | Theme 2: Non-COVID Health Outcomes |
| Rajoo et al. (2021) [47] | Addressing psychosocial issues caused by the COVID-19 lockdown: Can urban greeneries help? | Theme 2: Non-COVID Health Outcomes |
| Ribeiro et al. (2021) [48] | Exposure to nature and mental health outcomes during COVID-19 lockdown. A comparison between Portugal and Spain | Theme 2: Non-COVID Health Outcomes |
| Rosen et al. (2021) [49] | Promoting youth mental health during the COVID-19 pandemic: A longitudinal study | Theme 2: Non-COVID Health Outcomes |
| Soga et al. (2020) [50] | A room with a green view: the importance of nearby nature for mental health during the COVID-19 pandemic | Theme 2: Non-COVID Health Outcomes |
Appendix B. Additional Details of Theme 1 Studies
| Study | Geographic Extent | Unit of Analysis | Methods | Outcome Variable | Explanatory Variables | Detailed Findings | Proposed Mechanism |
|---|---|---|---|---|---|---|---|
| Casa Nova et al. (2021) [29] | Portugal | Districts | Detrended cross-correlation analysis | Daily new COVID-19 cases | Mobility indices | Mobility in general is positively correlated with new COVID-19 cases, but with a lag of 7–8 days. Parks show a more consistent and lower correlation compared to other forms of mobility. | Lower impact of park mobility compared to other modes suggested to be result of parks as open spaces with lower capacity for contagion. Note potential interaction with population density. Additionally, suggest that containment measures that closed some types of parks may have led to more congestion in open parks, which might make them more prone to increased transmission. |
| DePhillipo et al. (2021) [30] | USA | State | Multivariable linear regression | COVID-19 infection rates | Mobility in each of 6 groups as percent change from baseline | General association between increased mobility and increased COVID-19. When mobility broken into sectors, significant results only for retail and recreation and grocery and pharmacy mobility categories. | Parks not specifically discussed. |
| Johnson et al. (2021) [31] | England | Local government administrative areas | Generalized additive model | Daily COVID-19 case rates | Park use relative to other measures of mobility, population density, population clustering, poor health, population over 70, unemployed percent, green space patchiness, green space availability | Mobility was the most significant predictor of case rates, but park use as share of overall mobility associated with decreased case rates. Park use had more effect when patchiness and amount of green space were low. | The positive impact of park mobility is tied to the extent that time spent in parks replaces time spent in riskier areas. Lower movement is better overall, but parks are suggested as safer option if mobility is required. |
| Kartal, Depren, and Depren (2021) [32] | Turkey | Country | Toda-Yamamoto causality test | Daily number of patients, daily deaths | Walking and driving mobility (Apple data), destination-based mobility (Google). | Causal relationship identified between park mobility and deaths, but not patients. | General discussion of mobility as tied to transmission, but no park-specific mechanism was discussed. |
| Noland (2021) [33] | USA | State | Log-linear models | COVID-19 effective reproduction rate | Destination-based mobility metrics | Positive correlation between all mobility categories except residential and reproductive rate | Park-based mobility has the weakest relationship (smallest coefficient) of all mobility categories, which authors suggest indicates less viral spread at parks compared to other destinations |
| Praharaj and Han (2021) [34] | India | State | Poisson log-linear model | COVID-19 cases | Destination-based mobility metrics | No significant relationship between park mobility and COVID-19 cases | |
| Tyrovolas et al. (2021) [35] | Global, with regional analyses for Latin America, Africa, the Caribbean | Country | Negative binomial mixed model | Daily new COVID-19 cases | Countries’ preparedness in epidemics (INFORM index), COVID-19 testing policy, COVID-19 type of transmission for each country through time, populations’ real-time mobility patterns, their interaction with each level of government control policy, and the country’s income level | Park mobility interacted with government control measures—it exhibited a negative relationship to daily cases overall, but a positive relationship where control measures were in place. This held at the regional level for Latin America and the Caribbean, but not Africa | Individual behavior, dynamic network, and seasonality may be factors, but no discussion offered specifically for parks |
References
- Cranz, G. The Politics of Park Design: A History of Urban Parks in America; The MIT Press: Cambridge, MA, USA, 1982. [Google Scholar]
- Maas, J.; Verheij, R.A.; Groenewegen, P.P.; de Vries, S.; Spreeuwenberg, P. Green space, urbanity, and health: How strong is the relation? J. Epidemiol. Community Health 2006, 60, 587–592. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, R.; Popham, F. Greenspace, urbanity and health: Relationships in England. J. Epidemiol. Community Health 2007, 61, 681–683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulrich, R.S. View through a Window May Influence Recovery from Surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef] [Green Version]
- Lovasi, G.S.; Quinn, J.W.; Neckerman, K.M.; Perzanowski, M.S.; Rundle, A. Children living in areas with more street trees have lower prevalence of asthma. J. Epidemiol. Community Health 2008, 62, 647–649. [Google Scholar] [CrossRef] [Green Version]
- Wolch, J.; Jerrett, M.; Reynolds, K.; McConnell, R.; Chang, R.; Dahmann, N.; Brady, K.; Gilliland, F.; Su, J.G.; Berhane, K. Childhood obesity and proximity to urban parks and recreational resources: A longitudinal cohort study. Health Place 2010, 17, 207–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Besenyi, G.M.; Kaczynski, A.T.; Stanis, S.A.W.; Bergstrom, R.D.; Lightner, J.S.; Hipp, J.A. Planning for health: A community-based spatial analysis of park availability and chronic disease across the lifespan. Health Place 2014, 27, 102–105. [Google Scholar] [CrossRef]
- Maas, J.; Verheij, R.A.; de Vries, S.; Spreeuwenberg, P.; Schellevis, F.G.; Groenewegen, P.P. Morbidity is related to a green living environment. J. Epidemiol. Community Health 2009, 63, 967–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, M.S.; Wheeler, B.W.; White, M.P.; Economou, T.; Osborne, N.J. Urban street tree density and antidepressant prescription rates—A cross-sectional study in London, UK. Landsc. Urban Plan. 2015, 136, 174–179. [Google Scholar] [CrossRef]
- Snell, T.L.; Simmonds, J.G.; Klein, L.M. Exploring the impact of contact with nature in childhood on adult personality. Urban For. Urban Green. 2020, 55, 126864. [Google Scholar] [CrossRef]
- Weber, E.; Schneider, I.E. Blooming alleys for better health: Exploring impacts of small-scale greenspaces on neighborhood wellbeing. Urban For. Urban Green. 2021, 57, 126950. [Google Scholar] [CrossRef]
- Sinha, P.; Coville, R.C.; Hirabayashi, S.; Lim, B.; Endreny, T.A.; Nowak, D.J. Modeling lives saved from extreme heat by urban tree cover✰. Ecol. Modell. 2021, 449, 109553. [Google Scholar] [CrossRef]
- Scott, K.I.; McPherson, E.G.; Simpson, J.R. Air pollutant uptake by Sacramento’s urban forest. J. Arboric. 1995, 24, 224–234. [Google Scholar]
- Nowak, D.J.; Crane, D.E.; Stevens, J.C. Air pollution removal by urban trees and shrubs in the United States. Urban For. Urban Green. 2006, 4, 115–123. [Google Scholar] [CrossRef]
- Egorov, A.I.; Mudu, P.; Braubach, M.; Martuzzi, M. Urban Green Spaces and Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2016; p. 92. [Google Scholar]
- Ahmadpoor, N.; Shahab, S. Realising the value of greenspace: A planners’ perspective on the COVID-19 pandemic. Town Plan. Rev. 2021, 92, 49–56. [Google Scholar] [CrossRef]
- Geary, R.S.; Wheeler, B.; Lovell, R.; Jepson, R.; Hunter, R.; Rodgers, S. A call to action: Improving urban green spaces to reduce health inequalities exacerbated by COVID-19. Prev. Med. (Baltim.) 2021, 145, 106425. [Google Scholar] [CrossRef]
- Levinger, P.; Cerin, E.; Milner, C.; Hill, K.D. Older people and nature: The benefits of outdoors, parks and nature in light of COVID-19 and beyond–where to from here? Int. J. Environ. Health Res. 2021. [Google Scholar] [CrossRef]
- McCunn, L.J. The importance of nature to city living during the COVID-19 pandemic: Considerations and goals from environmental psychology. Cities Health 2020. [Google Scholar] [CrossRef]
- Venkatakrishnan, A.J.; Pawlowski, C.; Zemmour, D.; Hughes, T.; Anand, A.; Berner, G.; Kayal, N.; Puranik, A.; Conrad, I.; Bade, S.; et al. Mapping each pre-existing condition’s association to short-term and long-term COVID-19 complications. npj Digit. Med. 2021, 4, 1–11. [Google Scholar] [CrossRef]
- Hartig, T.; Mang, M.; Evans, G.W. Restorative effects of natural environment experiences. Environ. Behav. 1991, 23, 3–26. [Google Scholar] [CrossRef]
- Schmelzkopf, K. Urban community gardens as contested space. Geogr. Rev. 1995, 85, 364–381. [Google Scholar] [CrossRef]
- Bulfone, T.C.; Malekinejad, M.; Rutherford, G.W.; Razani, N. Outdoor transmission of SARS-CoV-2 and other respiratory viruses: A Systematic Review. J. Infect. Dis. 2021, 223, 550–561. [Google Scholar] [CrossRef] [PubMed]
- Gatersleben, B.; Andrews, M. When walking in nature is not restorative-the role of prospect and refuge. Health Place 2013, 20, 91–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Wu, X.; Wang, R.; He, D.; Li, D.; Yang, L.; Yang, Y.; Lu, Y. Review of associations between built environment characteristics and severe acute respiratory syndrome coronavirus 2 infection risk. Int. J. Environ. Res. Public Health 2021, 18, 7561. [Google Scholar] [CrossRef] [PubMed]
- Wright, H. Understanding green infrastructure: The development of a contested concept in England. Local Environ. 2011, 16, 1003–1019. [Google Scholar] [CrossRef]
- Matsler, A.M.; Meerow, S.; Mell, I.C.; Pavao-Zuckerman, M.A. A ‘green’ chameleon: Exploring the many disciplinary definitions, goals, and forms of “green infrastructure”. Landsc. Urban Plan. 2021, 214, 104145. [Google Scholar] [CrossRef]
- JBI. JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; Joanna Briggs Institute: Adelaide, Australia, 2020; ISBN 9780648848806. [Google Scholar]
- Casa Nova, A.; Ferreira, P.; Almeida, D.; Dionísio, A.; Quintino, D. Are mobility and COVID-19 related? A dynamic analysis for portuguese districts. Entropy 2021, 23, 786. [Google Scholar] [CrossRef]
- DePhillipo, N.N.; Chahla, J.; Busler, M.; LaPrade, R.F. Mobile phone GPS data and prevalence of COVID-19 infections: Quantifying parameters of social distancing in the U.S. Arch. Bone Jt. Surg. 2021, 9, 217–223. [Google Scholar]
- Johnson, T.F.; Hordley, L.A.; Greenwell, M.P.; Evans, L.C. Associations between COVID-19 transmission rates, park use, and landscape structure. Sci. Total Environ. 2021, 789, 148123. [Google Scholar] [CrossRef]
- Kartal, M.T.; Depren, Ö.; Kiliç Depren, S. The relationship between mobility and COVID-19 pandemic: Daily evidence from an emerging country by causality analysis. Transp. Res. Interdiscip. Perspect. 2021, 10, 100366. [Google Scholar] [CrossRef]
- Noland, R.B. Mobility and the effective reproduction rate of COVID-19. J. Transp. Health 2021, 20, 101016. [Google Scholar] [CrossRef]
- Praharaj, S.; Han, H. Human mobility impacts on the surging incidence of COVID-19 in India. Geogr. Res. 2021. [Google Scholar] [CrossRef]
- Tyrovolas, S.; Giné-Vázquez, I.; Fernández, D.; Morena, M.; Koyanagi, A.; Janko, M.; Haro, J.M.; Lin, Y.; Lee, P.; Pan, W.; et al. Estimating the COVID-19 spread through real-time population mobility patterns: Surveillance in Low-and Middle-income countries. J. Med. Internet Res. 2021, 23, e22999. [Google Scholar] [CrossRef] [PubMed]
- Corley, J.; Okely, J.A.; Taylor, A.M.; Page, D.; Welstead, M.; Skarabela, B.; Redmond, P.; Cox, S.R.; Russ, T.C. Home garden use during COVID-19: Associations with physical and mental wellbeing in older adults. J. Environ. Psychol. 2021, 73, 101545. [Google Scholar] [CrossRef]
- Gola, M.; Botta, M.; D’Aniello, A.L.; Capolongo, S. Influence of nature at the time of the pandemic: An experience-based survey at the time of SARS-CoV-2 to demonstrate how even a short break in nature can reduce stress for healthcare staff. Health Environ. Res. Des. J. 2021, 14, 49–65. [Google Scholar] [CrossRef] [PubMed]
- Heo, S.; Desai, M.U.; Lowe, S.R.; Bell, M.L. Impact of changed use of greenspace during COVID-19 pandemic on depression and anxiety. Int. J. Environ. Res. Public Health 2021, 18, 5842. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, G.; Den Daas, C.; Johnston, M.; Murchie, P.; Thompson, C.W.; Dixon, D. Are rurality, area deprivation, access to outside space, and green space associated with mental health during the COVID-19 pandemic? A cross sectional study (charis-e). Int. J. Environ. Res. Public Health 2021, 18, 3869. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.B.; Stevenson, K.T.; Larson, L.R.; Peterson, M.N.; Seekamp, E. Outdoor activity participation improves adolescents’ mental health and well-being during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2506. [Google Scholar] [CrossRef]
- Lee, D.G.; Lee, M.M.; Jeong, Y.M.; Kim, J.G.; Yoon, Y.K.; Shin, W.S. Influence of forest visitors’ perceived restorativeness on social–psychological stress. Int. J. Environ. Res. Public Health 2021, 18, 6328. [Google Scholar] [CrossRef]
- Lehberger, M.; Kleih, A.K.; Sparke, K. Self-reported well-being and the importance of green spaces—A comparison of garden owners and non-garden owners in times of COVID-19. Landsc. Urban Plan. 2021, 212, 104108. [Google Scholar] [CrossRef]
- Longman, D.P.; Shaw, C.N.; Varela-Mato, V.; Sherry, A.P.; Ruettger, K.; Sayyah, M.; Guest, A.; Chen, Y.L.; Paine, N.J.; King, J.A.; et al. Time in nature associated with decreased fatigue in UK truck drivers. Int. J. Environ. Res. Public Health 2021, 18, 3158. [Google Scholar] [CrossRef]
- Marques, P.; Silva, A.S.; Quaresma, Y.; Manna, L.R.; de Magalhães Neto, N.; Mazzoni, R. Home gardens can be more important than other urban green infrastructure for mental well-being during COVID-19 pandemics. Urban For. Urban Green. 2021, 64, 127268. [Google Scholar] [CrossRef] [PubMed]
- Mayen Huerta, C.; Utomo, A. Evaluating the association between urban green spaces and subjective well-being in Mexico City during the COVID-19 pandemic. Health Place 2021, 70, 102606. [Google Scholar] [CrossRef] [PubMed]
- Pearson, A.L.; Breeze, V.; Reuben, A.; Wyatt, G. Increased use of porch or backyard nature during COVID-19 associated with lower stress and better symptom experience among breast cancer patients. Int. J. Environ. Res. Public Health 2021, 18, 9102. [Google Scholar] [CrossRef] [PubMed]
- Sundara Rajoo, K.; Singh Karam, D.; Abdu, A.; Rosli, Z.; James Gerusu, G. Addressing psychosocial issues caused by the COVID-19 lockdown: Can urban greeneries help? Urban For. Urban Green. 2021, 65, 127340. [Google Scholar] [CrossRef]
- Ribeiro, A.I.; Triguero-Mas, M.; Jardim Santos, C.; Gómez-Nieto, A.; Cole, H.; Anguelovski, I.; Silva, F.M.; Baró, F. Exposure to nature and mental health outcomes during COVID-19 lockdown. A comparison between Portugal and Spain. Environ. Int. 2021, 154, 106664. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.L.; Rodman, A.M.; Kasparek, S.W.; Mayes, M.; Freeman, M.M.; Lengua, L.J.; Meltzoff, A.N.; McLaughlin, K.A. Promoting youth mental health during the COVID-19 pandemic: A longitudinal study. PLoS ONE 2021, 16, e0255294. [Google Scholar] [CrossRef]
- Soga, M.; Evans, M.J.; Tsuchiya, K.; Fukano, Y. A room with a green view: The importance of nearby nature for mental health during the COVID-19 pandemic. Ecol. Appl. 2021, 31, 1–10. [Google Scholar] [CrossRef]
- Heo, S.; Lim, C.C.; Bell, M.L. Relationships between local green space and human mobility patterns during COVID-19 for Maryland and California, USA. Sustainability 2020, 12, 9401. [Google Scholar] [CrossRef]
- Souza, C.N.; Rodrigues, A.C.; Correia, R.A.; Normande, I.C.; Costa, H.C.M.; Guedes-Santos, J.; Malhado, A.C.M.; Carvalho, A.R.; Ladle, R.J. No visit, no interest: How COVID-19 has affected public interest in world’s national parks. Biol. Conserv. 2021, 256, 109015. [Google Scholar] [CrossRef]
- Smith, M.K.S.; Smit, I.P.J.; Swemmer, L.K.; Mokhatla, M.M.; Freitag, S.; Roux, D.J.; Dziba, L. Sustainability of protected areas: Vulnerabilities and opportunities as revealed by COVID-19 in a national park management agency. Biol. Conserv. 2021, 255, 108985. [Google Scholar] [CrossRef]
- Hodor, K.; Przybylak, Ł.; Kuśmierski, J.; Wilkosz-Mamcarczyk, M. Identification and analysis of problems in selected european historic gardens during the COVID-19 pandemic. Sustainability 2021, 13, 1332. [Google Scholar] [CrossRef]
- Templeton, A.J.; Goonan, K.; Fyall, A. COVID-19 and its impact on visitation and management at US national parks. Int. Hosp. Rev. 2021. ahead-of-p. [Google Scholar] [CrossRef]
- Ugolini, F.; Massetti, L.; Pearlmutter, D.; Sanesi, G. Usage of urban green space and related feelings of deprivation during the COVID-19 lockdown: Lessons learned from an Italian case study. Land Use Policy 2021, 105, 105437. [Google Scholar] [CrossRef]
- Coombes, E.; Jones, A.P.; Hillsdon, M. The relationship of physical activity and overweight to objectively measured green space accessibility and use. Soc. Sci. Med. 2010, 70, 816–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wendel, H.E.W.; Downs, J.A.; Mihelcic, J.R. Assessing equitable access to urban green space: The role of engineered water infrastructure. Environ. Sci. Technol. 2011, 45, 6728–6734. [Google Scholar] [CrossRef]
- Rigolon, A. A complex landscape of inequity in access to urban parks: A literature review. Landsc. Urban Plan. 2016, 153, 160–169. [Google Scholar] [CrossRef]
- Landry, S.M.; Chakraborty, J. Street trees and equity: Evaluating the spatial distribution of an urban amenity. Environ. Plan. A 2009, 41, 2651–2670. [Google Scholar] [CrossRef]
- Perkins, H.A.; Heynen, N.; Wilson, J. Inequitable access to urban reforestation: The impact of urban political economy on housing tenure and urban forests. Cities 2004, 21, 291–299. [Google Scholar] [CrossRef]
- Hoover, F.-A.; Lim, T.C. Examining privilege and power in US urban parks and open space during the double crises of antiblack racism and COVID-19. Socio-Ecol. Pract. Res. 2020, 3, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Asaria, M.; Stranges, S. COVID-19 and inequality: Are we all in this together? Can. J. Public Health 2020, 111, 415–416. [Google Scholar] [CrossRef] [PubMed]
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, economic, and health inequality and COVID-19 infection in the United States. J. Racial Ethn. Health Disparities 2021, 8, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Chen, L.; Liu, X.; Yang, Y.; Sullivan, W.C.; Xu, W.; Webster, C.; Jiang, B. Green spaces mitigate racial disparity of health: A higher ratio of green spaces indicates a lower racial disparity in SARS-CoV-2 infection rates in the USA. Environ. Int. 2021, 152, 106465. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Unit of Analysis | Health Outcomes | Impact of GI Use | |||||
|---|---|---|---|---|---|---|---|---|
| State/Region/District | Country | COVID-19 Cases | COVID-19 Reproductive Rate | COVID-19 Deaths | Reduced Negative Outcomes | No Impact | Increased Negative Outcomes | |
| Casa Nova et al. (2021) [29] | x | x | x | |||||
| DePhillipo et al. (2021) [30] | x | x | x | |||||
| Johnson et al. (2021) [31] | x | x | x | |||||
| Kartal, Depren, and Depren (2021) [32] | x | x | x | x | x | |||
| Noland (2021) [33] | x | x | x | |||||
| Praharaj and Han (2021) [34] | x | x | x | |||||
| Tyrovolas et al. (2021) [35] | x | x | x | x | x | |||
| Author (Year) | Form of GI Use | Health Outcomes | Impact of GI Use | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Self-reported park/green space visits | Self-reported private GI use | Use of unspecified green or natural area | Anxiety | Cancer symptoms | Depression | Fatigue | Life satisfaction | Loneliness | Mental distress | Mental wellbeing | Physical health | Psychological distress | Psychopathology (internalizing) | Psychopathology (externalizing) | Self-esteem | Sleep quality | Somatization | Stress | Subjective wellbeing | Reduced negative outcomes | Increased positive outcomes | No impact | |
| Corley et al. (2021) [36] | x | x | x | x | x | x | |||||||||||||||||
| Gola et al. (2021) [37] | x | x | x | x | |||||||||||||||||||
| Heo et al. (2021) [38] | x | x | x | x | x | ||||||||||||||||||
| Hubbard et al. (2021) [39] | x | x | x | ||||||||||||||||||||
| Jackson et al. (2021) [40] | x | x | x | ||||||||||||||||||||
| Lee et al. (2021) [41] | x | x | x | ||||||||||||||||||||
| Lehberger, Kleih and Sparke (2021) [42] | x | x | x | x | |||||||||||||||||||
| Longman et al. (2021) [43] | x | x | x | x | x | x | |||||||||||||||||
| Marques et al. (2021) [44] | x | x | x | x | |||||||||||||||||||
| Mayen Huerta and Utomo (2021) [45] | x | x | x | ||||||||||||||||||||
| Pearson et al. (2021) [46] | x | x | x | x | |||||||||||||||||||
| Rajoo et al. (2021) [47] | x | x | x | x | x | ||||||||||||||||||
| Ribeiro et al. (2021) [48] | x | x | x | x | x | x | |||||||||||||||||
| Rosen et al. (2021) [49] | x | x | x | x | |||||||||||||||||||
| Soga et al. (2020) [50] | x | x | x | x | x | x | x | x | |||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heckert, M.; Bristowe, A. Parks and the Pandemic: A Scoping Review of Research on Green Infrastructure Use and Health Outcomes during COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 13096. https://doi.org/10.3390/ijerph182413096
Heckert M, Bristowe A. Parks and the Pandemic: A Scoping Review of Research on Green Infrastructure Use and Health Outcomes during COVID-19. International Journal of Environmental Research and Public Health. 2021; 18(24):13096. https://doi.org/10.3390/ijerph182413096
Chicago/Turabian StyleHeckert, Megan, and Amanda Bristowe. 2021. "Parks and the Pandemic: A Scoping Review of Research on Green Infrastructure Use and Health Outcomes during COVID-19" International Journal of Environmental Research and Public Health 18, no. 24: 13096. https://doi.org/10.3390/ijerph182413096
APA StyleHeckert, M., & Bristowe, A. (2021). Parks and the Pandemic: A Scoping Review of Research on Green Infrastructure Use and Health Outcomes during COVID-19. International Journal of Environmental Research and Public Health, 18(24), 13096. https://doi.org/10.3390/ijerph182413096







