A Comparative Study of Oral Health-Related Quality of Life among Cleft Lip and Palate Patients and Their Families during Orthodontic Treatment
Abstract
:1. Introduction
- There are differences in Oral Health Impact Profile-14 between patients with CLP and healthy controls (non-cleft group) undergoing orthodontic treatment.
- There are differences in Family Impact Scale between parents of children with CLP and parents of healthy children (non-cleft group) who are undergoing orthodontic treatment.
- There are differences in the perception of the quality of life between patients and their parents.
- Age and sex influence the perception of the OHRQoL in CLP and healthy controls groups undergoing orthodontic treatment.
2. Materials and Methods
2.1. Study Design
2.2. Data Collection Procedure
- The Cleft group is composed by individuals from both sexes with cleft lip and palate undergoing orthodontic treatment in the Faculty of Medicine of the University of Coimbra.
- The Control group is composed by individuals who attended the Faculty of Medicine of the University of Coimbra for orthodontics care without cleft lip and palate condition. The same number of patients was selected as control group, using randomized sampling resorting to a simple random allocation process with adaptive probabilities to guarantee a match, regarding age and sex, between the groups. This process aimed to ensure a reliable and unbiased comparison between the control and the CLP group.
2.3. Questionnaires
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Dimension | Question | Response * |
|---|---|---|
| Functional limitation | Have you had trouble pronouncing any words because of problems with your teeth, mouth or dentures? | |
| Have you felt that your sense of taste has worsened because of problems with your teeth, mouth or dentures? | ||
| Physical pain | Have you had painful aching in your mouth? | |
| Have you found it uncomfortable to eat any foods because of problems with your teeth, mouth or dentures? | ||
| Psychological discomfort | Have you been self-conscious because of your teeth, mouth or dentures? | |
| Have you felt tense because of problems with your teeth, mouth or dentures? | ||
| Physical disability | Has your diet been unsatisfactory because of problems with your teeth, mouth or dentures? | |
| Have you had to interrupt meals because of problems with your teeth, mouth or dentures? | ||
| Psychological disability | Have you found it difficult to relax because of problems with your teeth, mouth or dentures? | |
| Have you been a bit embarrassed because of problems with your teeth, mouth or dentures? | ||
| Social disability | Have you been a bit irritable with other people because of problems with your teeth, mouth or dentures? | |
| Have you had difficulty doing your usual jobs because of problems with your teeth, mouth or dentures? | ||
| Handicap | Have you felt that life in general was less satisfying because of problems with your teeth, mouth or dentures? | |
| Have you been totally unable to function because of problems with your teeth, mouth or dentures? |
| Dimension | Question | Response * |
|---|---|---|
| Parental/family activity | Have you or has the other parent taken time off work? | |
| Has your child required more attention from you or the other parent? | ||
| Have you or has the other parent had less time for yourself or other family members? | ||
| Has your sleep or that of the other parent been disrupted? | ||
| Have family activities been interrupted? | ||
| Parental emotions | Have you or has the other parent been upset? | |
| Have you or has the other parent felt guilty? | ||
| Have you or has the other parent worried that your child will have fewer life opportunities? | ||
| Have you felt uncomfortable in public places? | ||
| Family conflicts | Has your child argued with you or the other parent? | |
| Has your child been jealous of you or other family members? | ||
| Has your child´s condition caused disagreement or conflict in the family? | ||
| Has your child blamed you or the other parent? | ||
| Financial Burden | Has your child´s condition caused financial difficulties for your family? |
References
- Bezerra, B.T.; Pinho, J.N.A.; Silva, L.C.F. Tooth Abnormalities In Individuals With Unilateral Alveolar Clefts: A Comparison Between Sides Using Cone-Beam Computed Tomography. J. Clin. Exp. Dent. 2017, 9, e1195–e1200. [Google Scholar] [CrossRef]
- Mossey, P.A.; Little, J.; Munger, R.G.; Dixon, M.J.; Shaw, W.C. Cleft lip and palate. Lancet 2009, 374, 1773–1785. [Google Scholar] [CrossRef]
- Dixon, M.J.; Marazita, M.L.; Beaty, T.H.; Murray, J.C. Cleft lip and palate: Synthesizing genetic and environmental influences. Nat. Rev. Genet. 2011, 12, 167–178. [Google Scholar] [CrossRef] [Green Version]
- Francisco, I.; Caramelo, F.; Fernandes, M.H.; Vale, F. Parental Risk Factors and Child Birth Data in a Matched Year and Sex Group Cleft Population: A Case-Control Study. Int. J. Environ. Res. Public Health 2021, 18, 4615. [Google Scholar] [CrossRef] [PubMed]
- Vettore, M.V.; Campos, A.E.S. Malocclusion characteristics of patients with cleft lip and/or palate. Eur. J. Orthod. 2011, 33, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Sá, J.; Araújo, L.; Guimarães, L.; Maranhão, S.; Lopes, G.; Medrado, A.; Coletta, R.; Reis, S. Dental anomalies inside the cleft region in individuals with nonsyndromic cleft lip with or without cleft palate. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e48–e52. [Google Scholar] [CrossRef] [PubMed]
- Herkrath, A.P.C.Q.; Herkrath, F.J.; Rebelo, M.A.B.; Vettore, M.V. Measurement of health-related and oral health–related quality of life among individuals with nonsyndromic orofacial clefts: A systematic review and meta-analysis. Cleft Palate-Craniofacial J. 2015, 52, 157–172. [Google Scholar] [CrossRef]
- Montes, A.B.M.; Oliveira, T.M.; Gavião, M.B.D.; Barbosa, T.S. Orofacial functions and quality of life in children with unilateral cleft lip and palate. Braz. Oral Res. 2019, 33, e0061. [Google Scholar] [CrossRef]
- Karki, S.; Horváth, J.; Laitala, M.-L.; Vástyán, A.; Nagy, Á.; Sándor, G.K.; Anttonen, V. Validating and assessing the oral health-related quality of life among Hungarian children with cleft lip and palate using Child-OIDP scale. Eur. Arch. Paediatr. Dent. 2021, 22, 57–65. [Google Scholar] [CrossRef] [Green Version]
- Corcoran, M.; Karki, S.; Harila, V.; Kyngäs, H.; Luoto, A.; Ylikontiola, L.P.; Sándor, G.K.; Anttonen, V. Oral health-related quality of life among young adults with cleft in northern Finland. Clin. Exp. Dent. Res. 2020, 6, 305–310. [Google Scholar] [CrossRef]
- Dimberg, L.; Arnrup, K.; Bondemark, L. The impact of malocclusion on the quality of life among children and adolescents: A systematic review of quantitative studies. Eur. J. Orthod. 2015, 37, 238–247. [Google Scholar] [CrossRef]
- Sinko, K.; Jagsch, R.; Preschtl, V.; Watzinger, F.; Hollman, K.; Baumann, A. Evaluation of esthetic, functional and quality-of life outcome in adult cleft lip and palate patients. Cleft Palate-Craniofac J. 2005, 42, 355–361. [Google Scholar] [CrossRef]
- Agou, S.; Locker, D.; Muirhead, V.; Tompson, B.; Streiner, D.L. Does psychological well-being influence oral-health-related quality of life reports in children receiving orthodontic treatment? Am. J. Orthod. Dentofac. Orthop. 2011, 139, 369–377. [Google Scholar] [CrossRef]
- Long, H.; Wang, Y.; Jian, F.; Liao, L.; Yang, X.; Lai, W. Current advances in orthodontic pain. Int. J. Oral Sci. 2016, 8, 67–75. [Google Scholar] [CrossRef]
- Liu, Z.; McGrath, C.; Hägg, U. Changes in oral health-related quality of life during fixed orthodontic appliance therapy: An 18-month prospective longitudinal study. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 214–219. [Google Scholar] [CrossRef]
- Zhang, M.; McGrath, C.; Hagg, U. Changes in oral health-related quality of life during fixed orthodontic appliance therapy. Am J. Orthod. Dentofac. Orthop. 2008, 133, 25–29. [Google Scholar] [CrossRef]
- Antoun, J.S.; Fowler, P.V.; Jack, H.C.; Farella, M. Oral health-related quality of life changes in standard, cleft, and surgery patients after orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 568–575. [Google Scholar] [CrossRef]
- Barros, L.A.N.; Jesuino, F.A.S.; Paiva, J.B.; Rino-Neto, J.; Valladares-Neto, J. An Oral Health-Related Quality of Life Comparison Between Adults With Unilateral Cleft Lip and Palate and Class III Malocclusion. Cleft Palate-Craniofac J. 2019, 56, 1359–1365. [Google Scholar] [CrossRef]
- Rando, G.M.; Jorge, P.K.; Vitor, L.L.R.; Carrara, C.F.C.; Soares, S.; Silva, T.C.; Rios, D.; Machado, M.A.A.M.; Gavião, M.B.; Oliveira, T.M. Oral health-related quality of life of children with oral clefts and their families. J. Appl. Oral Sci. 2018, 26, e20170106. [Google Scholar] [CrossRef] [Green Version]
- Beluci, M.L.; Mondini, C.C.S.D.; Trettene, A.S.; Dantas, R.A.S. Correlation between quality of life and burden of family caregivers of infants with cleft lip and palate. Rev. Esc. Enferm. USP 2019, 53, e03432. [Google Scholar] [CrossRef]
- Nolte, F.M.; Bos, A.; Prahl, C. Quality of Life Among Dutch Children With a Cleft Lip and/or Cleft Palate: A Follow-Up Study. Cleft Palate-Craniofac J. 2019, 56, 1065–1071. [Google Scholar] [CrossRef]
- Broder, H.L. Psychological research of children with craniofacial anomalies: Review, critique, and implications for the future. Cleft Palate-Craniofac J. 1997, 34, 402–404. [Google Scholar] [CrossRef]
- Raghavan, S.; Philip, K.; Batra, P.; Marcusson, A. Aesthetic perceptions and psychosocial impact of malocclusion: Comparison between cleft and non-cleft patients and their parents. Eur. J. Orthod. 2019, 41, 38–45. [Google Scholar] [CrossRef]
- Abreu, L.G.; Corradi-Dias, L.; Santos, T.R.; Melgaço, C.A.; Lages, E.M.B.; Paiva, S.M. Quality of life of families of adolescents undergoing fixed orthodontic appliance therapy: Evaluation of a cohort of parents/guardians of treated and untreated individuals. Int. J. Paediatr. Dent. 2020, 30, 634–641. [Google Scholar] [CrossRef]
- Leopoldo-Rodado, M.; Pantoja-Pertegal, F.; Belmonte-Caro, R.; Garcia-Perla, A.; Gonzalez-Cardero, E.; Infante-Cossio, P. Quality of life in early age Spanish children treated for cleft lip and/or palate: A case-control study approach. Clin. Oral Investig. 2021, 25, 477–485. [Google Scholar] [CrossRef]
- Aravena, P.C.; Gonzalez, T.; Oyarzún, T.; Coronado, C. Oral Health-Related Quality of Life in Children in Chile Treated for Cleft Lip and Palate: A Case-Control Approach. Cleft Palate-Craniofac J. 2017, 54, e15–e20. [Google Scholar] [CrossRef]
- Chen, Y.H.; Liao, Y.F.; Chang, C.S.; Lu, T.C.; Chen, K.T. Patient satisfaction and quality of life after orthodontic treatment for cleft lip and palate deformity. Clin. Oral Investig. 2021, 25, 5521–5529. [Google Scholar] [CrossRef]
- Sundell, A.L.; Törnhage, C.J.; Marcusson, A. A comparison of health-related quality of life in 5- and 10-year-old Swedish children with and without cleft lip and/or palate. Int. J. Paediatr. Dent. 2017, 27, 238–246. [Google Scholar] [CrossRef]
- Khoun, T.; Malden, P.E.; Turton, B.J. Oral health-related quality of life in young Cambodian children: A validation study with a focus on children with cleft lip and/or palate. Int. J. Paediatr. Dent. 2018, 28, 326–334. [Google Scholar] [CrossRef]
- Agnew, C.M.; Page, L.A.F.; Hibbert, S.; Thomson, W.M. Family Impact of Child Oro-Facial Cleft. Cleft Palate-Craniofac J. 2020, 57, 1291–1297. [Google Scholar] [CrossRef] [PubMed]
- Cuyper, E.; Dochy, F.; Leenheer, E.; Hoecke, H.V. The impact of cleft lip and/or palate on parental quality of life: A pilot study. Int. J. Pediatr. Otorhinolaryngol. 2019, 126, 10959. [Google Scholar] [CrossRef] [Green Version]
- Davies, K.; Lin, Y.L.; Callery, P. Parents’ and children’s knowledge of oral health: A qualitative study of children with cleft palate. Int. J. Paediatr. Dent. 2017, 27, 264–272. [Google Scholar] [CrossRef]
- Imani, M.M.; Jalali, A.; Nouri, P.; Golshah, A. Parent’s Experiences During Orthodontic Treatment of Their Children With Cleft Lip and Palate: Phenomenological Study. Cleft Palate-Craniofac J. 2021, 58, 1135–1141. [Google Scholar] [CrossRef]
- McGrath, C.; Broder, H.; Wilson-Genderson, M. Assessing the impact of oral health on the life quality of children: Implications for research and practice. Community Dent. Oral Epidemiol. 2004, 32, 81–88. [Google Scholar] [CrossRef]
| CLP Group (n = 111) | Control Group (n = 115) | ||||
|---|---|---|---|---|---|
| Year of Birth | Female | Male | Female | Male | Total |
| 1994 | 1 | 0 | 1 | 0 | 2 |
| 1995 | 1 | 1 | 1 | 1 | 4 |
| 1996 | 0 | 1 | 0 | 1 | 2 |
| 1997 | 3 | 1 | 3 | 1 | 8 |
| 1998 | 1 | 3 | 1 | 3 | 8 |
| 1999 | 0 | 1 | 0 | 1 | 2 |
| 2000 | 3 | 2 | 3 | 2 | 10 |
| 2001 | 3 | 2 | 3 | 2 | 10 |
| 2002 | 4 | 4 | 4 | 4 | 16 |
| 2003 | 5 | 4 | 5 | 4 | 18 |
| 2004 | 5 | 8 | 5 | 6 | 24 |
| 2005 | 0 | 6 | 0 | 8 | 14 |
| 2006 | 5 | 8 | 5 | 7 | 25 |
| 2007 | 6 | 3 | 6 | 3 | 18 |
| 2008 | 1 | 3 | 1 | 3 | 8 |
| 2009 | 3 | 8 | 3 | 8 | 22 |
| 2010 | 1 | 7 | 1 | 12 | 21 |
| 2011 | 2 | 1 | 2 | 1 | 6 |
| 2012 | 1 | 0 | 1 | 0 | 2 |
| 2013 | 0 | 3 | 0 | 3 | 6 |
| Total | 45 | 66 | 45 | 70 | 226 |
| Demographic Variables | Control (115) | CLP (111) | p |
|---|---|---|---|
| sex (M/F) | 70/45 (60.9%/39.1%) | 66/45 (59.5%/40.5%) | 0.892 § |
| (min/max) | 4.3 (7/36) | 4.3 (7/26) | 0.637 £ |
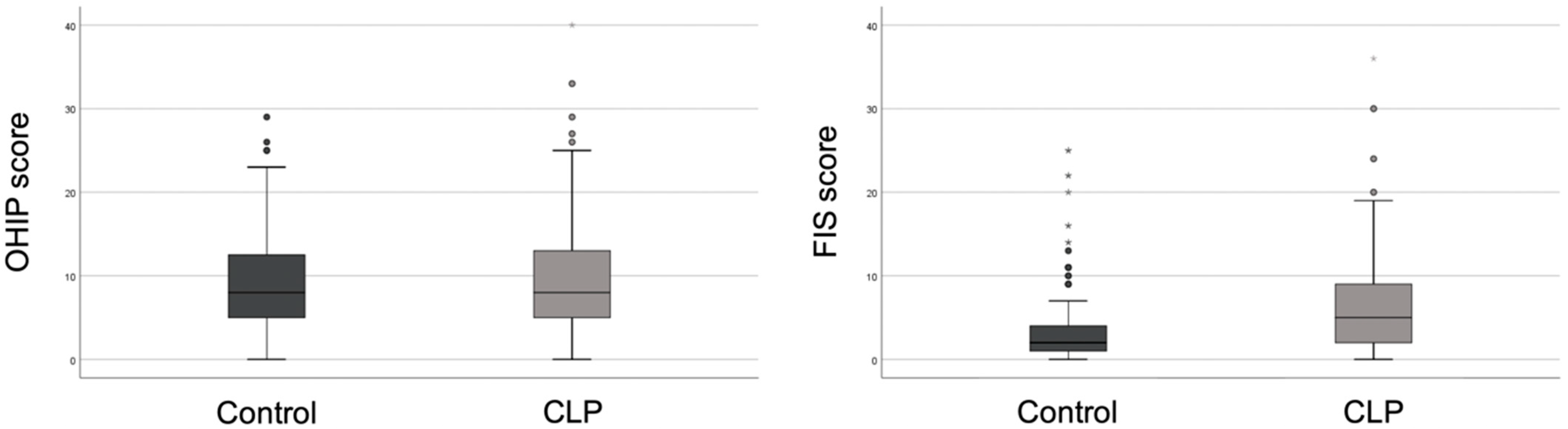
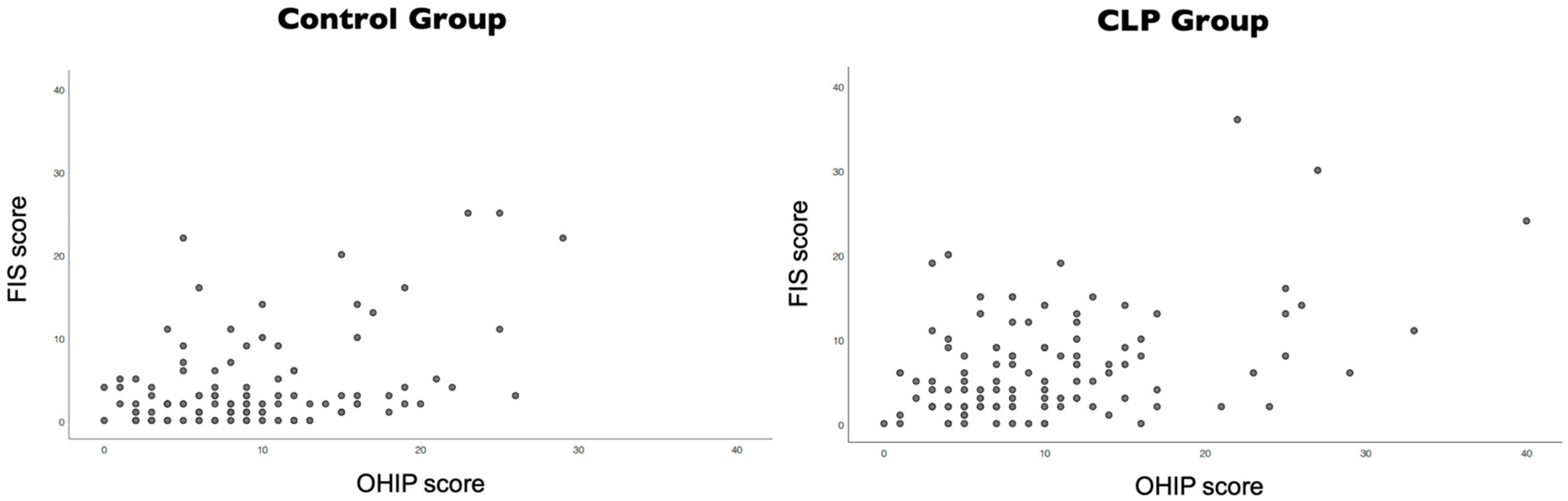
| OHIP and FIS Scores | Control (115) | CLP (111) | p |
|---|---|---|---|
| OHIP (min/max) | 9.4 6.2 (0/29) | 10.2 7.2 (0/40) | 0.572 £ |
| FIS (min/max) | 4.0 5.4 (0/25) | 6.7 6.3 (0/36) | <0.001 £ |
| Control (115) | CLP (111) | p£ | ||
|---|---|---|---|---|
| OHIP | Functional limitation | 1.3 ± 1.0 (0/4) | 1.6 ± 1.4 (0/6) | 0.192 |
| Physical pain | 3.2 ± 1.7 (0/8) | 3.0 ± 1.6 (0/7) | 0.507 | |
| Psychosocial impact | 1.3 ± 1.5 (0/6) | 1.5 ± 1.9 (0/8) | 0.904 | |
| Physical limitation | 1.5 ± 1.8 (0/8) | 1.3 ± 1.6 (0/7) | 0.253 | |
| Psychological limitation | 1.0 ± 1.4 (0/7) | 1.1 ± 1.6 (0/7) | 0.846 | |
| Social limitation | 0.8 ± 1.1 (0/4) | 1.4 ± 1.5 (0/6) | 0.001 | |
| Disability | 0.3 ± 0.7 (0/4) | 0.3 ± 0.9 (0/4) | 0.531 | |
| FIS | Family activities | 2.0 ± 2.6 (0/12) | 3.7 ± 3.2 (0/18) | <0.001 |
| Parental emotions | 0.7 ± 1.6 (0/8) | 1.3 ± 2.1 (0/12) | 0.001 | |
| Family conflict | 0.7 ± 1.6 (0/7) | 1.2 ± 2.0 (0/9) | 0.011 | |
| Family finances | 0.6 ± 0.8 (0/4) | 0.4 ± 0.9 (0/3) | 0.051 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Francisco, I.; Caramelo, F.; Fernandes, M.H.; Vale, F. A Comparative Study of Oral Health-Related Quality of Life among Cleft Lip and Palate Patients and Their Families during Orthodontic Treatment. Int. J. Environ. Res. Public Health 2021, 18, 12826. https://doi.org/10.3390/ijerph182312826
Francisco I, Caramelo F, Fernandes MH, Vale F. A Comparative Study of Oral Health-Related Quality of Life among Cleft Lip and Palate Patients and Their Families during Orthodontic Treatment. International Journal of Environmental Research and Public Health. 2021; 18(23):12826. https://doi.org/10.3390/ijerph182312826
Chicago/Turabian StyleFrancisco, Inês, Francisco Caramelo, Maria Helena Fernandes, and Francisco Vale. 2021. "A Comparative Study of Oral Health-Related Quality of Life among Cleft Lip and Palate Patients and Their Families during Orthodontic Treatment" International Journal of Environmental Research and Public Health 18, no. 23: 12826. https://doi.org/10.3390/ijerph182312826
APA StyleFrancisco, I., Caramelo, F., Fernandes, M. H., & Vale, F. (2021). A Comparative Study of Oral Health-Related Quality of Life among Cleft Lip and Palate Patients and Their Families during Orthodontic Treatment. International Journal of Environmental Research and Public Health, 18(23), 12826. https://doi.org/10.3390/ijerph182312826









