Come for Information, Stay for Support: Harnessing the Power of Online Health Communities for Social Connectedness during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection and Survey Design
2.2. Measures
2.2.1. Perception of COVID-19
2.2.2. Utilized and Desired Sources of COVID-19 Information and Support
2.2.3. Quality of Life and Health-Related Behavioral Changes
2.2.4. Demographics
2.2.5. Analysis
3. Results
3.1. Participants
3.2. COVID-19 Concern
3.3. Self-Directed Research and Desire for Additional Support
3.4. Burnout, Isolation, and Mental Health Distress
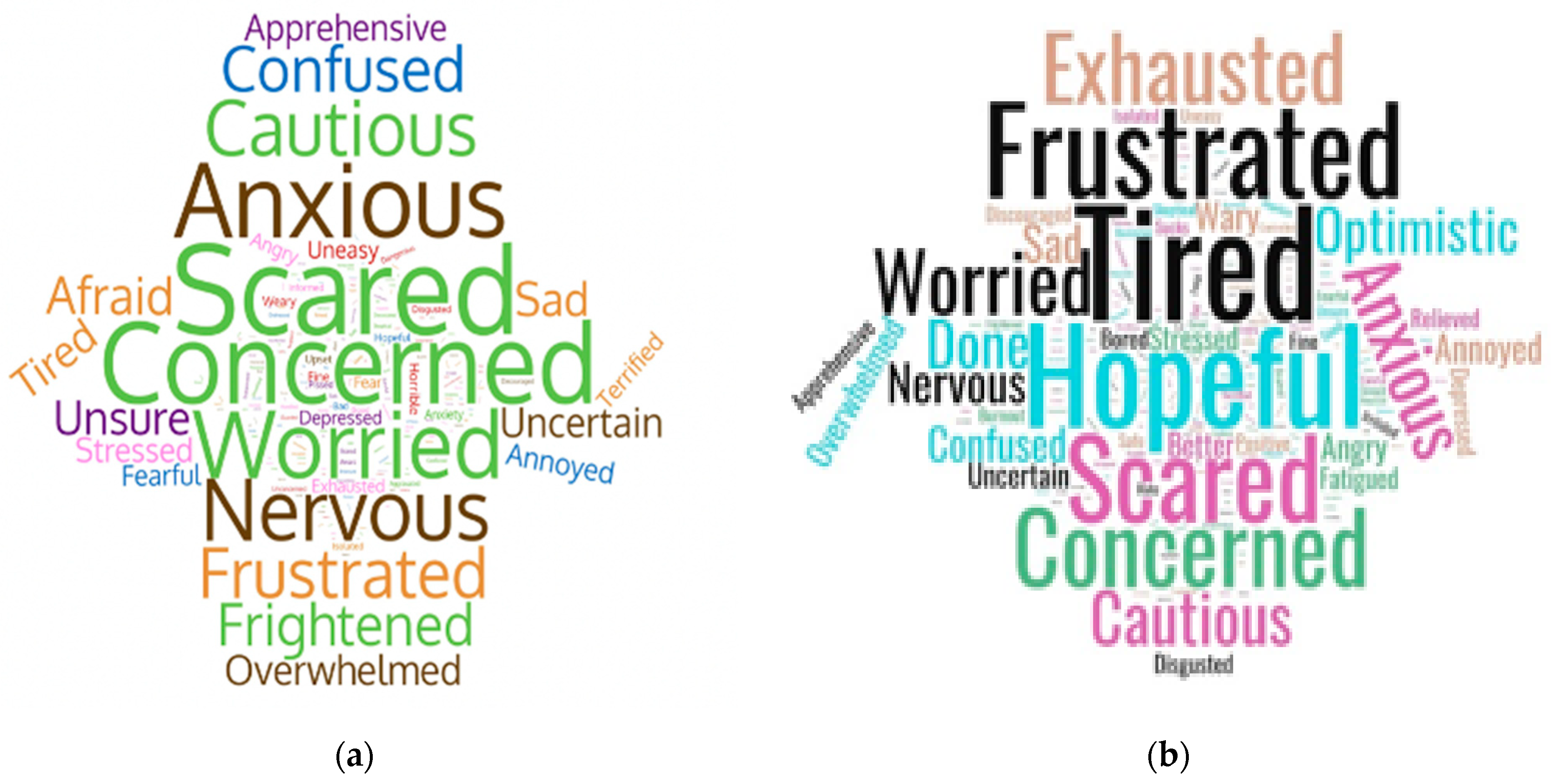
3.5. One-Word Perceptions
3.6. First-Hand Accounts of Isolation and Longing for Connection
“The biggest struggle for me is the isolation. The last time I was out to eat with friends or shopping in a store was the end of February 2020. It’s a more mental/emotional struggle most days.”
“Boredom due to seclusion. Normally I busy myself with helping others but being secluded in my room with little to do has begun to wear down my normally positive attitude.”
“I don’t have any help at home, and it’s hard for me to manage. I feel incredibly isolated-which causes increased depression. I cannot even participate in communal worship because of immunosuppressant medications that increase my risk for COVID. I would like to work, as much as I can, but as a piano teacher, it is not possible, and that is more isolating and makes one feel more ‘useless.’ Being ill, unemployed, and having no one to have physical contact or interactions with is not normal. It is not conducive to mental health, [which is] hard enough for those with chronic pain and health conditions.”
“Warm greetings to everyone in the asthma world! As I sit here on day 22 of isolation during the COVID-19 pandemic, I am reminded of my reasons for wanting to share my experiences as an asthma patient and a lung cancer survivor, to name a couple of my health issues. So I am in isolation and I can’t help but think about how grateful I am to have this forum to turn to. Not just in today’s current environment but always. It is so helpful to hear from so many others who are in the same boat. Asthma often makes me feel isolated and alone. In reality, I am alone, but WE are together in our little corners of the planet doing our best to stay safe and healthy and live our lives. The current climate of the world has intensified that for us.”
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Clement, S.; Schauman, O.; Graham, T.; Maggioni, F.; Evans-Lacko, S.; Bezborodovs, N.; Morgan, C.; Rüsch, N.; Brown, J.S.L.; Thornicroft, G. What is the Impact of Mental Health-Related Stigma on Help-Seeking? A Systematic Review of Quantitative and Qualitative Studies. Psychol. Med. 2014, 45, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Michelle Obama Says She Is Dealing with ‘Low-Grade Depression’. Available online: https://www.nytimes.com/2020/08/06/us/michelle-obama-depression.html (accessed on 15 September 2021).
- Substantial Investment Needed to Avert Mental Health Crisis. Available online: https://www.who.int/news/item/14-05-2020-substantial-investment-needed-to-avert-mental-health-crisis (accessed on 15 September 2021).
- Hossain, M.M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.L.J.; Ahmed, H.U.; Ma, P. Epidemiology of Mental Health Problems in COVID-19: A Review. F1000Research 2020, 9, 636. [Google Scholar] [CrossRef]
- The Lancet Psychiatry. COVID-19 and Mental Health. Lancet Psychiatry 2021, 8, 87. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental Health Before and During the COVID-19 Pandemic: A Longitudinal Probability Sample Survey of the UK Population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Mental Health and Substance Use State Fact Sheets. Available online: https://www.kff.org/statedata/mental-health-and-substance-use-state-fact-sheets/ (accessed on 15 September 2021).
- Can Social Prescribing Support the COVID-19 Pandemic? Available online: https://www.cebm.net/covid-19/can-social-prescribing-support-the-covid-19-pandemic/ (accessed on 15 September 2021).
- Everson-Rose, S.A.; Lewis, T.T. Psychosocial Factors And Cardiovascular Diseases. Annu. Rev. Public Health 2005, 26, 469–500. [Google Scholar] [CrossRef]
- Uchino, B.N. Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes. J. Behav. Med. 2006, 29, 377–387. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [Green Version]
- Daré, L.O.; Bruand, P.E.; Gérard, D. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: A meta-analysis. BMC Public Health 2019, 19, 304. [Google Scholar] [CrossRef] [PubMed]
- Niall, A.; Ozakinci, G. Effectiveness of Psychological Interventions to Improve Quality of Life in People with Long-Term Conditions: Rapid Systematic Review of Randomised Controlled Trials. BMC Psychol. 2018, 6, 1. [Google Scholar] [CrossRef] [Green Version]
- Wonggom, P.; Kourbelis, C.; Newman, P.; Du, H.; Clark, R.A. Effectiveness of avatar-based technology in patient education for improving chronic disease knowledge and self-care behavior: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 1101–1129. [Google Scholar] [CrossRef] [PubMed]
- Magharei, M.; Jaafari, S.; Mansouri, P.; Safarpour, A.; Taghavi, S.A. Effects of Self-Management Education on Self-Efficacy and Quality of Life in Patients with Ulcerative Colitis: A Randomized Controlled Clinical Trial. Int. J. Community Based Nurs. Midwifery 2019, 7, 32–42. [Google Scholar] [CrossRef]
- Smith, T.B.; Workman, C.; Andrews, C.; Barton, B.; Cook, M.; Layton, R. Effects of psychosocial support interventions on survival in inpatient and outpatient healthcare settings: A meta-analysis of 106 randomized controlled trials. PLoS Med. 2021, 18, e1003595. [Google Scholar] [CrossRef]
- Gonzalez, J.S.; Penedo, F.J.; Antoni, M.H.; Durán, R.E.; McPherson-Baker, S.; Ironson, G.; Isabel Fernandez, M.; Klimas, N.G.; Fletcher, M.A.; Schneiderman, N. Social Support, Positive States of Mind, and HIV Treatment Adherence in Men and Women Living With HIV/AIDS. Health Psychol. 2004, 23, 413–418. [Google Scholar] [CrossRef]
- Mirsky, J.B.; Horn, D.M. Chronic Disease Management in the COVID-19 Era. Am. J. Manag. Care 2020, 26, 329–330. [Google Scholar] [CrossRef]
- Liu, C.; Zhao, Y.; Okwan-Duodu, D.; Basho, R.; Cui, X. COVID-19 in Cancer Patients: Risk, Clinical Features, and Management. Cancer Biol. Med. 2020, 17, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.A.; Ahmed, Z.; Younas, S. COVID-19 and Comorbidities: Deleterious Impact on Infected Patients. J. Infect. Public Health 2020, 13, 1833–1839. [Google Scholar] [CrossRef]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. e-Health 2020, 26, 377–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- March, S.; Day, J.; Ritchie, G.; Rowe, A.; Gough, J.; Hall, T.; Yuen, C.Y.J.; Donovan, C.L.; Ireland, M. Attitudes Toward E-Mental Health Services in a Community Sample of Adults: Online Survey. J. Med. Internet. Res. 2018, 20, e59. [Google Scholar] [CrossRef]
- Sundar, K.R. A Patient with COVID-19 is Left Behind as Care Goes Virtual. Health Aff. 2020, 39, 1453–1455. [Google Scholar] [CrossRef] [PubMed]
- van der Eijk, M.; Faber, M.J.; Aarts, J.W.; Kremer, J.A.; Munneke, M.; Bloem, B.R. Using Online Health Communities to Deliver Patient-Centered Care to People With Chronic Conditions. J. Med. Internet. Res. 2013, 15, e115. [Google Scholar] [CrossRef]
- Li, Y.; Yan, X. How Could Peers in Online Health Community Help Improve Health Behavior. Int. J. Environ. Res. Public Health 2020, 17, 2995. [Google Scholar] [CrossRef] [PubMed]
- Merolli, M.; Gray, K.; Martin-Sanchez, F. Health Outcomes and Related Effects of Using Social Media in Chronic Disease Management: A Literature Review and Analysis of Affordances. J. Biomed. Inform. 2013, 46, 957–969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steadman, J.; Pretorius, C. The Impact of an Online Facebook Support Group for People with Multiple Sclerosis on Non-Active Users. Afr. J. Disabil. 2014, 3, 132. [Google Scholar] [CrossRef]
- van Uden-Kraan, C.F.; Drossaert, C.H.; Taal, E.; Seydel, E.R.; van de Laar, M.A. Self-Reported Differences in Empowerment Between Lurkers and Posters in Online Patient Support Groups. J. Med. Internet. Res. 2008, 10, e18. [Google Scholar] [CrossRef] [Green Version]
- Green, B.M.; Van Horn, K.T.; Gupte, K.; Evans, M.; Hayes, S.; Bhowmick, A. Assessment of Adaptive Engagement and Support Model for People With Chronic Health Conditions in Online Health Communities: Combined Content Analysis. J. Med. Internet. Res. 2020, 22, e17338. [Google Scholar] [CrossRef]
- Trump Administration Drives Telehealth Services in Medicaid and Medicare. Available online: https://www.cms.gov/newsroom/press-releases/trump-administration-drives-telehealth-services-medicaid-and-medicare (accessed on 15 September 2021).
- ‘COVID Fatigue’ Is Hitting Hard. Fighting It Is Hard, Too, Says UC Davis Health Psychologist. Available online: https://health.ucdavis.edu/health-news/newsroom/covid-fatigue-is-hitting-hard-fighting-it-is-hard-too-says-uc-davis-health-psychologist/2020/07 (accessed on 15 September 2021).
- COVID-19 Misinformation Remains Difficult To Stop on Social Media. Available online: https://www.forbes.com/sites/petersuciu/2020/04/17/covid-19-misinformation-remains-difficult-to-stop-on-social-media/ (accessed on 15 September 2021).
- Coulson, N.S. Receiving Social Support Online: An Analysis of a Computer-Mediated Support Group for Individuals Living with Irritable Bowel Syndrome. Cyberpsychol. Behav. 2005, 8, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Willis, E. The Making of Expert Patients: The Role of Online Health Communities in Arthritis Self-Management. J. Health Psychol. 2013, 19, 1613–1625. [Google Scholar] [CrossRef]
| Survey Wave | Dates Fielded | Num. of OHCs | Total Completes |
|---|---|---|---|
| Wave 1 | 19–25 March 2020 | 10 | 991 |
| Wave 2 | 14–17 April 2020 | 26 | 2214 |
| Wave 3 | 12–14 May 2020 | 26 | 2210 |
| Wave 4 | 21–23 July 2020 | 26 | 1777 |
| Wave 5 | 23 October–2 November 2020 | 26 | 2005 |
| Wave 6 | 12–19 April 2021 | 28 | 980 |
| Survey Wave | Gender | Mean Age | Employment Status |
|---|---|---|---|
| Wave 1 | 87% Female 12% Male | 58.7 | 35% Employed 34% Retired 21% Disability |
| Wave 2 | 84% Female 16% Male | 57.6 | 33% Employed 30% Retired 24% Disability |
| Wave 3 | 81% Female 19% Male | 56.3 | 30% Employed 38% Retired 21% Disability |
| Wave 4 | 83% Female 17% Male | 59.7 | 31% Employed 36% Retired 22% Disability |
| Wave 5 | 82% Female 18% Male | 58.9 | 30% Employed 38% Retired 21% Disability |
| Wave 6 | 78% Female 21% Male | 60.4 | 31% Employed 39% Retired 19% Disability |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Green, B.M.; Hribar, C.A.; Hayes, S.; Bhowmick, A.; Herbert, L.B. Come for Information, Stay for Support: Harnessing the Power of Online Health Communities for Social Connectedness during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 12743. https://doi.org/10.3390/ijerph182312743
Green BM, Hribar CA, Hayes S, Bhowmick A, Herbert LB. Come for Information, Stay for Support: Harnessing the Power of Online Health Communities for Social Connectedness during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(23):12743. https://doi.org/10.3390/ijerph182312743
Chicago/Turabian StyleGreen, Brian M., Casey A. Hribar, Sara Hayes, Amrita Bhowmick, and Leslie Beth Herbert. 2021. "Come for Information, Stay for Support: Harnessing the Power of Online Health Communities for Social Connectedness during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 23: 12743. https://doi.org/10.3390/ijerph182312743
APA StyleGreen, B. M., Hribar, C. A., Hayes, S., Bhowmick, A., & Herbert, L. B. (2021). Come for Information, Stay for Support: Harnessing the Power of Online Health Communities for Social Connectedness during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(23), 12743. https://doi.org/10.3390/ijerph182312743






