The Correlation between Nurses’ COVID-19 Infections and Their Emotional State and Work Conditions during the SARS-CoV-2 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.4. Ethical Procedures
2.5. Statistical Analysis
3. Results
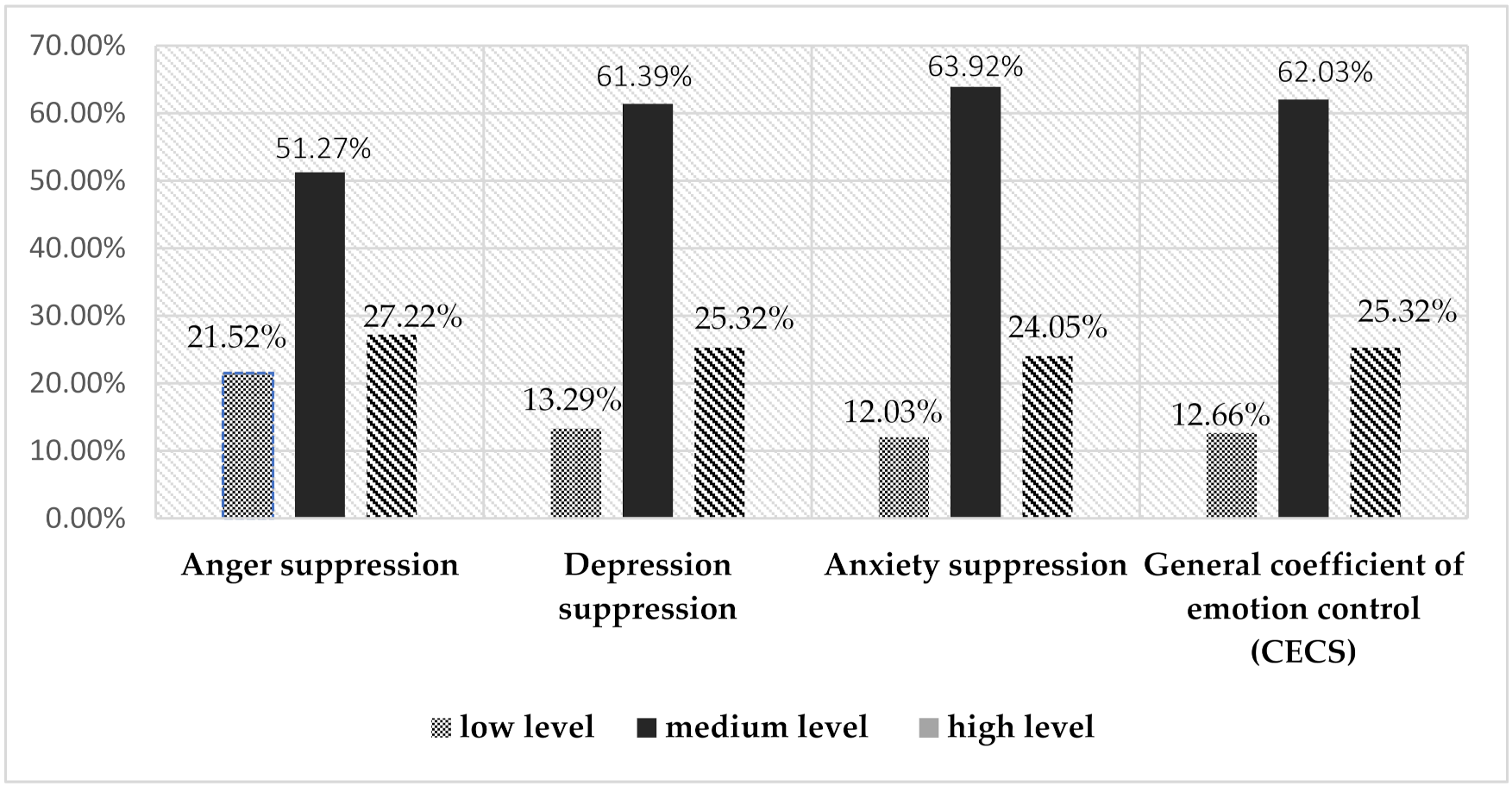
3.1. Analysis of Emotions Experienced by Nurses while Working during the SARS-CoV-2 Pandemic
3.2. Analysis of Work Conditions during the SARS-CoV-2 Pandemic
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Straus, S.E.; Wilson, K.; Ramba ldini, G.; Rath, D.; Lin, Y.; Gold, W. Severe acute respiratory syndrome and its impact on professionalism: Qualitative study of physicians’ behaviour during an emerging healthcare crisis. BMJ 2004, 29, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, C.Y.; Peng, Y.C.; Wu, Y.H.; Chang, J.; Chan, C.H.; Yang, D.Y. The psychological effect of severe acute respiratory syn-drome on emergency department staff. Emerg. Med. J. 2007, 24, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Barry, M.; Robert, A.; Temsah, M.-H.; Bari, S.A.; Akhtar, M.; Al Nahdi, F.; Erlandez, R.; Al-Tawfiq, J.; Al Khushail, A.; Al Hebaishi, Y. COVID-19 Community Transmission among Healthcare Workers at a Tertiary Care Cardiac Center. Med. Sci. 2021, 9, 49. [Google Scholar] [CrossRef]
- Troyer, E.A.; Kohn, J.N.; Hong, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsy-chiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020, 87, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Arnetz, J.E.; Arble, E.; Sudan, S.; Arnetz, B.B. Workplace Cognitive Failure among Nurses during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10394. [Google Scholar] [CrossRef] [PubMed]
- Stelnicki, A.M.; Carleton, R.N.; Reichert, C. Nurses’ Mental Health and Well-Being: COVID-19 Impacts. Can. J. Nurs. Res. 2020, 52, 237–239. [Google Scholar] [CrossRef]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and Addressing Sources of Anxiety among Health Care Professionals during the COVID-19 Pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef] [PubMed]
- Jerg-Bretzke, L.; Kempf, M.; Jarczok, M.N.; Weimer, K.; Hirning, C.; Gündel, H.; Erim, Y.; Morawa, E.; Geiser, F.; Hiebel, N.; et al. Psychosocial Impact of the COVID-19 Pandemic on Healthcare Workers and Initial Areas of Action for Intervention and Prevention—The egePan/VOICE Study. Int. J. Environ. Res. Public Health 2021, 18, 10531. [Google Scholar] [CrossRef] [PubMed]
- McFadden, P.; Neill, R.; Moriarty, J.; Gillen, P.; Mallett, J.; Manthorpe, J.; Currie, D.; Schroder, H.; Ravalier, J.; Nicholl, P.; et al. A Cross-Sectional Examination of the Mental Wellbeing, Coping and Quality of Working Life in Health and Social Care Workers in the UK at Two Time Points of the COVID-19 Pandemic. Epidemiologia 2021, 2, 227–242. [Google Scholar] [CrossRef]
- Goulia, P.; Mantas, C.; Dimitroula, D.; Mantis, D.; Hyphantis, T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect. Dis. 2010, 10, 322. [Google Scholar] [CrossRef] [Green Version]
- Data on the Number of Cases—COVID-19. Available online: https://www.rynekzdrowia.pl/Polityka-zdrowotna/Koronawirus-w-Polsce-2-923-304-potwierdzonych-zakazen-zmarlo-75-869-osob,204119,14.html (accessed on 7 November 2021).
- Data on Deaths of Doctors and Nurses. Available online: https://www.rynekzdrowia.pl/Serwis-Choroby-Zakazne/W-Polsce-zmarlo-231-lekarzy-i-185-pielegniarek-Wszyscy-przez-koronawirusa-Zgony-sa-tez-wsrod-dentystow-i-farmaceutow,222613,1017.html (accessed on 6 November 2021).
- Maciaszek, J.; Ciulkowicz, M.; Misiak, B.; Szczesniak, D.; Luc, D.; Wieczorek, T.; Fila-Witecka, K.; Gawlowski, P.; Ry-maszewska, J. Mental Health od Madical and Non-Medical Professionals Turing the Peak of the COVID-19 Pandemic: A Cross-Sectional Nationwide Study. J. Clin. Med. 2020, 9, 2527. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, e37–e38. [Google Scholar] [CrossRef] [Green Version]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Yang, B.X.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Chui, P.L.; Chong, M.C.; Abdullah, K.L.; Ramoo, V.; Tang, L.Y.; Lee, W.L.; Che, C.C.; Yahaya, N.A.; Rasaiah, K.; Zaini, N.H.; et al. The COVID-19 Global Pandemic and Its Impact on the Mental Health of Nurses in Malaysia. Healthcare 2021, 9, 1259. [Google Scholar] [CrossRef]
- Juczyński, Z. Narzędzia Pomiaru w Promocji i Psychologii Zdrowia; Pracownia Testów Psychologicznych Pol-skiego Towarzystwa Psychologicznego: Warszawa, Poland, 2001; pp. 55–59. [Google Scholar]
- Piksa, M.; Kosiorowska, E.; Golonka, K. Skala Lęku—Cecha (SL-C). May 2020. Available online: https://www.researchgate.net/publication/341756731_Skala_Leku_-_Cecha_SL-C?channel=doi&linkId=5ed2d26492851c9c5e6c112a&showFulltext=true (accessed on 6 November 2021).
- Malinowska-Lipień, I.; Wadas, T.; Sułkowska, J.; Suder, M.; Gabryś, T.; Kózka, M.; Gniadek, A.; Brzostek, T. Emotional Control among Nurses against Work Conditions and the Support Received during the SARS-CoV-2 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 9415. [Google Scholar] [CrossRef] [PubMed]
- Hendy, A.; Abozeid, A.; Sallam, G.; Fattah, H.A.A.; Reshia, F.A.A. Predictive factors affecting stress among nurses providing care at COVID-19 isolation hospitals at Egypt. Nurs. Open 2021, 8, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Buchelt, B.; Kowalska-Bobko, I. Human Resource Management in the Healthcare System; WHO: Geneva, Switzerland, 2020; Available online: https://politykipubliczne.pl/wp-content/uploads/2020/10/Zarzadzanie-zasobami-ludzkimi-w-systemie-ochrony-zdrowia-w-czasach-pandemii.pdf (accessed on 6 November 2021).
- Mocan, A.Ş.; Iancu, S.S.; Băban, A.S. Association of cognitive-emotional regulation strategies to depressive symptoms in type 2 diabetes patients. Rom. J. Intern. Med. 2018, 56, 34–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lenzo, V.; Quattropani, M.C.; Sardella, A.; Martino, G.; Bonanno, G.A. Depression, Anxiety, and Stress among Healthcare Workers during the COVID-19 Outbreak and Relationships with Expressive Flexibility and Context Sensitivity. Front. Psychol. 2021, 12, 623033. [Google Scholar] [CrossRef] [PubMed]
- Nukui, H.; Midorikawa, S.; Murakami, M.; Maeda, M.; Ohtsuru, A. Mental health of nurses after the Fukushima complex disaster: A narrative review. J. Radiat. Res. 2018, 59, ii108–ii113. [Google Scholar] [CrossRef] [PubMed]
- Gniadek, A.; Nawara, W.; Padykuła, M.; Malinowska-Lipień, I. A Polish nurse during SARS-CoV-2 pandemic—Various aspects of following a nursing profession. Zdr. Publiczne I Zarządzanie 2020, 18, 140–154. [Google Scholar]
- Report of the Supreme Chamber of Nurses and Midwives (NIPiP). A Catastrophe of Nurses and Midwives. 8 June 2021. Available online: https://nipip.pl/2021-06-08-raport-nipip-katastrofa-kadrowa-pielegniarek-i-poloznych/ (accessed on 7 November 2021).
- Tan, B.; Chew, N.W.; Lee, G.K.; Jing, M.; Goh, Y.; Yeo, L.L.; Zhang, K.; Chin, H.-K.; Ahmad, A.; Khan, F.A.; et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Ann. Intern. Med. 2020, 173, 317–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozga, D.; Krupa, S.; Mędrzycka-Dąbrowska, W.; Knap, M.; Witt, P. Psychological support provided by national nursing associations in pandemic. Polish ICU nursing experiences. Psychiatr. Polska 2020, 54, 1269–1272. [Google Scholar] [CrossRef] [PubMed]
| Group A (n = 79) | Group B (n = 79) | All Study Nurses (n = 158) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Gender, n (%) | |||||||
| Women | 76 | 96.20 | 76 | 96.20 | 152 | 96.2 | |
| Men | 3 | 3.80 | 3 | 3.80 | 6 | 3.8 | |
| Age, n (%) | |||||||
| 22–30 years | 17 | 21.52 | 13 | 16.46 | 30 | 18.99 | |
| 31–40 years | 22 | 27.85 | 28 | 35.44 | 50 | 31.65 | |
| 41–50 years | 18 | 22.78 | 16 | 20.25 | 34 | 21.52 | |
| 51–66 years | 15 | 18.99 | 21 | 26.58 | 36 | 22.78 | |
| 22–30 years | 7 | 8.86 | 1 | 1.27 | 8 | 5.06 | |
| Marital status, n (%) | |||||||
| Married | 44 | 55.70 | 44 | 55.70 | 88 | 55.7 | |
| Single | 22 | 27.85 | 19 | 24.05 | 41 | 25.95 | |
| Informal relationship | 11 | 13.92 | 14 | 17.72 | 25 | 15.82 | |
| Divorced/Separated | 2 | 2.53 | 2 | 2.53 | 4 | 2.53 | |
| Education, n (%) | |||||||
| Medical secondary education | 10 | 12.66 | 8 | 10.13 | 18 | 11.39 | |
| Bachelor’s degree in nursing | 20 | 25.32 | 22 | 27.85 | 42 | 26.58 | |
| Master’s degree in nursing | 43 | 54.43 | 46 | 58.23 | 89 | 56.33 | |
| Higher education, degree obtained in a faculty other than nursing | 2 | 2.53 | 5 | 6.33 | 7 | 4.43 | |
| Ph.D. degree | 1 | 1.27 | 1 | 1.27 | 2 | 1.27 | |
| Seniority, n (%) | |||||||
| <year | 1 | 1.27 | 3 | 3.80 | 4 | 2.53 | |
| 1–5 years’ work experience | 28 | 35.44 | 29 | 36.71 | 57 | 36.08 | |
| 6–10 years’ work experience | 7 | 8.86 | 12 | 15.19 | 19 | 12.03 | |
| 11–20 years’ work experience | 15 | 18.99 | 11 | 13.92 | 26 | 16.46 | |
| 21–30 years’ work experience | 16 | 20.25 | 18 | 22.78 | 34 | 21.52 | |
| over 30 years’ work experience | 12 | 15.19 | 6 | 7.59 | 18 | 11.39 | |
| Workplace, n(%) | Hospital—infectious diseases ward or 24-h outpatient care | 28 | 33.44 | 26 | 32.91 | 54 | 34.17 |
| Hospital—noninfectious ward | 51 | 64.56 | 53 | 67.09 | 104 | 65.83 | |
| Main Symptoms Accompanying the SARS-CoV-2 Infection in the Researched Group | Group A n = 79 | % |
|---|---|---|
| Asthenia | 72 | 91.14% |
| Headache | 61 | 77.22% |
| Loss of smell | 57 | 72.15% |
| Muscle pain | 55 | 69.62% |
| Loss of taste | 49 | 62.03% |
| Cough | 38 | 48.10% |
| Higher temperature | 32 | 40.51% |
| Dyspnea | 20 | 25.32% |
| Diarrhea | 19 | 24.05% |
| Temperature above 38 °C | 18 | 22.78% |
| No symptoms | 1 | 1.27% |
| Anger Suppression | Depression Suppression | Anxiety Suppression | General Coefficient of Emotion Control (CECS) | Anxiety Level Scale as Traits | |
|---|---|---|---|---|---|
| Mean | Mean | Mean | Mean | Mean | |
| Group A | 18.86 | 18.8 | 18.44 | 56.1 | 26.53 |
| Group B | 17.42 | 17.7 | 18.18 | 53.29 | 24.18 |
| p = 0.06 | p = 0.11 | p = 0.64 | p = 0.08 | p = 0.04 ** |
| SL-C | Anger Suppression | Depression Suppression | Anxiety Suppression | General Coefficient of Emotion Control (CECS) | |
|---|---|---|---|---|---|
| All study nurses | r | 0.084 | 0.208 | 0.044 | 0.134 |
| p | 0.29 | 0.009 ** | 0.7 | 0.09 | |
| Group A | r | 0.137 | 0.288 | 0.081 | 0.194 |
| p | 0.22 | 0.01 ** | 0.48 | 0.08 | |
| Group B | r | −0.017 | 0.086 | −0.003 | 0.024 |
| p | 0.88 | 0.45 | 0.97 | 0.86 | |
| Working Conditions Workplace | All Study Nurses n = 158 | Group A n = 79 | Group B n = 79 | Chi2 p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Hospital—noninfectious ward | 104 | 65.83 | 51 | 64.55 | 53 | 67.08 | ꭓ² = 11.065 p = 0.0008 ** |
| Hospital—infectious diseases ward or 24-h outpatient care | 54 | 34.17 | 28 | 33.45 | 26 | 32.82 | |
| Performing work with patients suspected of being infected with the SARS-COV-2 virus | |||||||
| All the time | 57 | 36.08 | 30 | 37.97 | 27 | 34.18 | ꭓ² = 3.824 p = 0.28 |
| Yes, often or very often | 56 | 35.44 | 26 | 32.91 | 30 | 37.97 | |
| Yes, occasionally | 42 | 26.58 | 23 | 29.11 | 19 | 24.05 | |
| I have no contact with such patients | 3 | 1.90 | 0 | 0.00 | 3 | 3.80 | |
| COVID-19 procedures developed in the ward | |||||||
| Yes | 148 | 93.67 | 75 | 94.94 | 73 | 92.41 | ꭓ² = 4.693 p = 0.09 |
| No | 6 | 3.80 | 4 | 5.06 | 2 | 2.53 | |
| I don’t know | 4 | 2.53 | 0 | 0.00 | 4 | 5.06 | |
| Training for dealing with COVID-19 patients, as well as the use of protective clothing | |||||||
| Yes | 90 | 56.96 | 40 | 50.63 | 50 | 63.29 | ꭓ² = 3.8224 p = 0.014 ** |
| No, I had to learn everything myself | 57 | 36.08 | 31 | 39.24 | 26 | 32.91 | |
| I don’t know | 11 | 6.96 | 8 | 10.13 | 3 | 3.80 | |
| Sufficient provision of personal safety means in the ward | |||||||
| Yes | 110 | 69.62 | 56 | 70.89 | 54 | 68.35 | ꭓ²= 0.029 p= 0.86 |
| No | 48 | 30.38 | 23 | 29.11 | 25 | 31.65 | |
| Possibility of using personal safety resources without limitations | |||||||
| Yes | 111 | 70.25 | 55 | 69.62 | 56 | 70.89 | ꭓ² = 0.0303 p = 0.86 |
| No | 47 | 29.75 | 24 | 30.38 | 23 | 29.11 | |
| Possibility of undergoing a COVID-19 test at the workplace | |||||||
| Yes, without problems | 80 | 50.63 | 34 | 43.04 | 46 | 58.23 | ꭓ² = 22.248 p = 0.00005 ** |
| Yes, but I had to struggle for this | 35 | 22.15 | 11 | 13.92 | 24 | 30.38 | |
| No, because there were no swab points | 16 | 10.13 | 11 | 13.92 | 5 | 6.33 | |
| No, because I failed to obtain permission from my employer | 27 | 17.09 | 23 | 29.11 | 4 | 5.06 | |
| Nursing staff insufficiency | |||||||
| Yes | 133 | 84.18 | 71 | 89.87 | 62 | 78.48 | ꭓ² = 6.307 p = 0.04 ** |
| No | 7 | 4.43 | 4 | 5.06 | 3 | 3.80 | |
| Hard to evaluate | 18 | 11.39 | 4 | 5.06 | 14 | 17.72 | |
| Support from the employer | |||||||
| Yes | 90 | 56.96% | 37 | 46.84% | 53 | 67.09% | ꭓ² = 5.808 p = 0.02 ** |
| No | 68 | 43.04% | 42 | 53.16% | 26 | 32.91% | |
| Support from a psychologist in the workplace | |||||||
| Yes | 40 | 25.32% | 12 | 15.19% | 28 | 35.44% | ꭓ²= 7.531 p = 0.006 ** |
| No | 118 | 74.68% | 67 | 84.81% | 51 | 64.56% | |
| Support from coworkers | |||||||
| Yes | 152 | 96.20% | 77 | 97.47% | 75 | 94.94% | ꭓ² = 0.173 p = 0.67 |
| No | 6 | 3.80% | 2 | 2.53% | 4 | 5.06% | |
| A shortage of nursing staff in the workplace | |||||||
| Yes | 135 | 85.44 | 70 | 88.61 | 65 | 82.28 | ꭓ² = 1.501 p = 0.47 |
| No | 19 | 12.03 | 7 | 8.86 | 12 | 15.19 | |
| I don’t know | 4 | 2.53 | 2 | 2.53 | 2 | 2.53 | |
| Working overtime during the pandemic | |||||||
| Yes | 109 | 68.99 | 56 | 70.89 | 53 | 67.09 | ꭓ² = 0.183 p = 0.73 |
| No | 49 | 31.01 | 23 | 29.11 | 26 | 32.91 | |
| Number of work hours during the pandemic | |||||||
| 7.35 h shifts | 18 | 11.39 | 8 | 10.13 | 10 | 12.66 | ꭓ² = 3.665 p = 0.45 |
| 12 h shifts | 91 | 57.59 | 44 | 55.70 | 47 | 59.49 | |
| 12 and 24 h shifts | 26 | 16.46 | 14 | 17.72 | 12 | 15.19 | |
| 24 h shifts | 21 | 13.29 | 13 | 16.46 | 8 | 10.13 | |
| >24 h shifts | 2 | 1.27 | 0 | 0.00 | 2 | 2.53 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malinowska-Lipień, I.; Suder, M.; Wadas, T.; Gabryś, T.; Kózka, M.; Gniadek, A.; Brzostek, T. The Correlation between Nurses’ COVID-19 Infections and Their Emotional State and Work Conditions during the SARS-CoV-2 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 12715. https://doi.org/10.3390/ijerph182312715
Malinowska-Lipień I, Suder M, Wadas T, Gabryś T, Kózka M, Gniadek A, Brzostek T. The Correlation between Nurses’ COVID-19 Infections and Their Emotional State and Work Conditions during the SARS-CoV-2 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(23):12715. https://doi.org/10.3390/ijerph182312715
Chicago/Turabian StyleMalinowska-Lipień, Iwona, Magdalena Suder, Tadeusz Wadas, Teresa Gabryś, Maria Kózka, Agnieszka Gniadek, and Tomasz Brzostek. 2021. "The Correlation between Nurses’ COVID-19 Infections and Their Emotional State and Work Conditions during the SARS-CoV-2 Pandemic" International Journal of Environmental Research and Public Health 18, no. 23: 12715. https://doi.org/10.3390/ijerph182312715
APA StyleMalinowska-Lipień, I., Suder, M., Wadas, T., Gabryś, T., Kózka, M., Gniadek, A., & Brzostek, T. (2021). The Correlation between Nurses’ COVID-19 Infections and Their Emotional State and Work Conditions during the SARS-CoV-2 Pandemic. International Journal of Environmental Research and Public Health, 18(23), 12715. https://doi.org/10.3390/ijerph182312715






