A Systematic Review of Child Health and Developmental Outcomes Associated with Low Birthweight and/or Small for Gestational Age in Indigenous Children from Australia, Canada and New Zealand
Abstract
:1. Introduction
1.1. Definitions
First Nations Peoples
1.2. Birth Outcomes
1.3. Consequences of Low Birthweight in Indigenous Populations
2. Materials and Methods
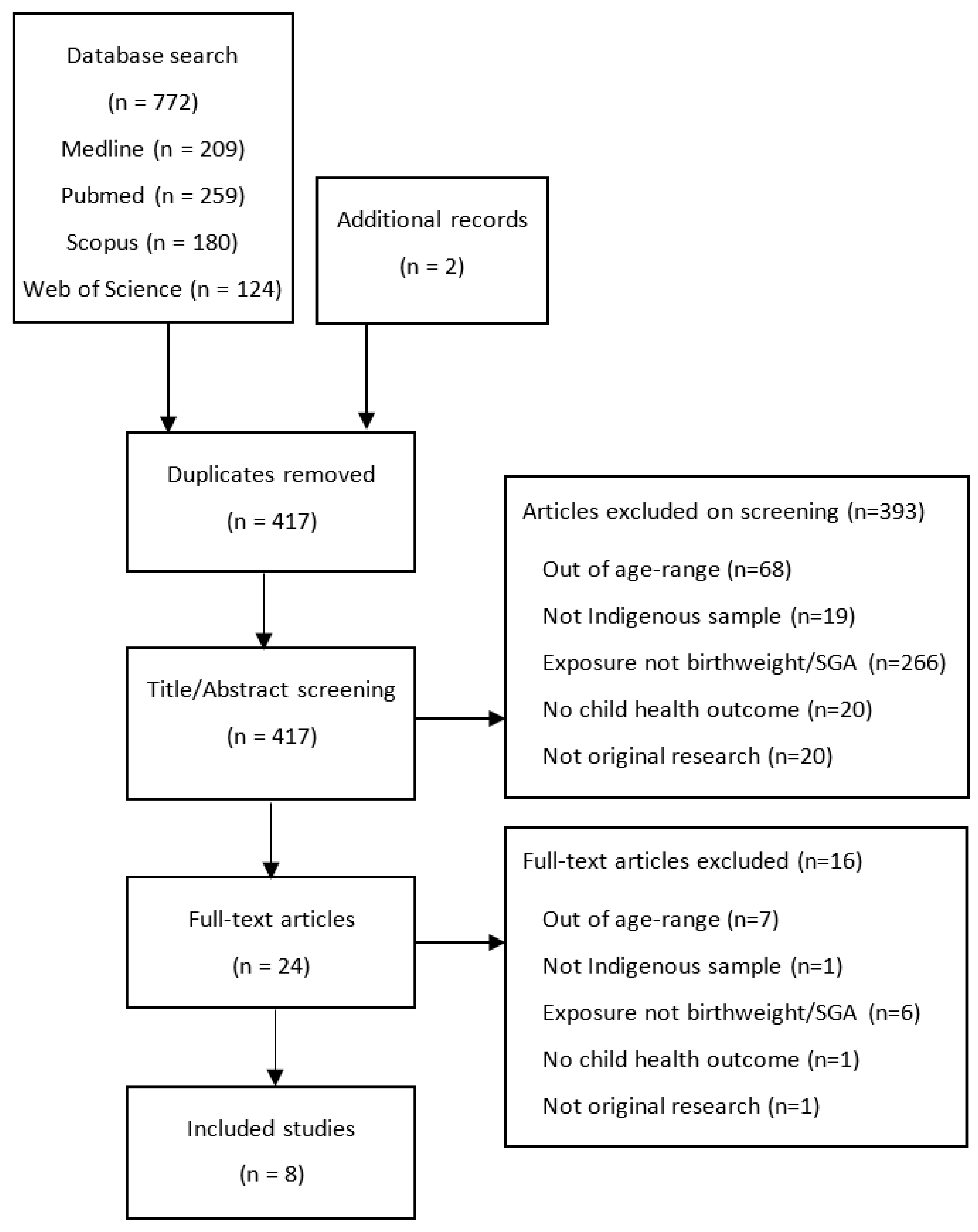
2.1. Search Strategy
2.2. Study Selection
2.2.1. Inclusion Criteria
- Original peer-reviewed research.
- Prospective or retrospective cohort studies and cross-sectional studies.
- Indigenous study populations within Australia, Canada and New Zealand.
- Studies reporting data on birthweight and/or size for gestational age.
- Studies reporting on child developmental, physical and/or mental health outcomes at age 5–12 years stratified by low birthweight or SGA.
2.2.2. Exclusion Criteria
2.3. Data Extraction
2.4. Critical and Cultural Appraisal
3. Results
3.1. Study Characteristics
3.2. Birthweight, Birth Size and Child Health Outcomes
3.3. Child Health Outcomes Reported in Included Studies (Aim 1)
3.4. Asthma
3.5. Academic Performance
3.6. Developmental Vulnerability
3.7. Child BMI
3.8. Global Measures of Child Health and Disability
3.9. Cultural and Community Strengths (Aim 2)
3.10. Critical Appraisal
3.11. Cultural Appraisal
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Department of Health Australia. National Aboriginal and Torres Strait Islander Health Plan 2013–2023. Australia 2013. Available online: https://www.health.gov.au/health-topics/aboriginal-and-torres-strait-islander-health/how-we-support-health/health-plan (accessed on 22 February 2021).
- Sayers, S.; Powers, J. Risk factors for Aboriginal low birthweight, intrauterine growth retardation and preterm birth in the Darwin Health Region. Aust. N. Z. J. Public Health 1997, 21, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Rousham, E.K.; Gracey, M. Factors affecting birthweight of rural Australian Aborigines. Ann. Hum. Biol. 2002, 29, 363–372. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. International Statistical Classification of Diseases and Related Health Problems; 11th Revision; World Health Organisation: Geneva, Switzerland, 2021. [Google Scholar]
- Mandy, G.T. Infants with Fetal (Intrauterine) Growth Restriction Uptodate [Updated 21 Sepember 2020]. Available online: https://www.uptodate.com/contents/infants-with-fetal-intrauterine-growth-restriction?search=low%20birth%20weight&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2 (accessed on 7 February 2021).
- Blencowe, H.; Krasevec, J.; de Onis, M.; Black, R.E.; An, X.; Stevens, G.A.; Borghi, E.; Hayashi, C.; Estevez, D.; Cegolon, L.; et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: A systematic analysis. Lancet Glob. Health 2019, 7, e849–e860. [Google Scholar] [CrossRef] [Green Version]
- Brown, S.J.; Yelland, J.S.; Sutherland, G.A.; Baghurst, P.A.; Robinson, J.S. Stressful life events, social health issues and low birthweight in an Australian population-based birth cohort: Challenges and opportunities in antenatal care. BMC Public Health 2011, 11, 196. [Google Scholar] [CrossRef] [Green Version]
- McEwen, E.C.; Boulton, T.J.; Smith, R. Can the gap in Aboriginal outcomes be explained by DOHaD. J. Dev. Orig. Health Dis. 2019, 10, 5–16. [Google Scholar] [CrossRef]
- Edwards, M. The Barker Hypothesis. In Handbook of Famine, Starvation, and Nutrient Deprivation: From Biology to Policy; Preedy, V., Patel, V.B., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 1–21. [Google Scholar]
- Lee, A.C.; Kozuki, N.; Cousens, S.; Stevens, G.A.; Blencowe, H.; Silveira, M.F.; Sania, A.; Rosen, H.E.; Schmiegelow, C.; Adair, L.S.; et al. Estimates of burden and consequences of infants born small for gestational age in low and middle income countries with INTERGROWTH-21(st) standard: Analysis of CHERG datasets. BMJ 2017, 358, j3677. [Google Scholar] [CrossRef] [Green Version]
- Sacchi, C.; Marino, C.; Nosarti, C.; Vieno, A.; Visentin, S.; Simonelli, A. Association of Intrauterine Growth Restriction and Small for Gestational Age Status With Childhood Cognitive Outcomes: A Systematic Review and Meta-analysis. JAMA Pediatr. 2020, 174, 772–781. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Australia’s Children; AIHW: Canberra, Australia, 2020. [Google Scholar]
- Hoy, W.E.; Nicol, J.L. The Barker hypothesis confirmed: Association of low birth weight with all-cause natural deaths in young adult life in a remote Australian Aboriginal community. J. Dev. Orig. Health Dis. 2019, 10, 55–62. [Google Scholar] [CrossRef] [Green Version]
- Davy, C.; Harfield, S.; McArthur, A.; Munn, Z.; Brown, A. Access to primary health care services for Indigenous peoples: A framework synthesis. Int. J. Equity Health 2016, 15, 163. [Google Scholar] [CrossRef] [Green Version]
- Buckskin, M.; Kit, J.A.; Glover, K.; Mitchell, A.; Miller, R.; Weetra, D.; Wiebe, J.; Yelland, J.S.; Newbury, J.; Robinson, J.; et al. Aboriginal Families Study: A population-based study keeping community and policy goals in mind right from the start. Int. J. Equity Health 2013, 12, 41. [Google Scholar] [CrossRef] [Green Version]
- The Lowitja Institute. Close the Gap 2020; The Close the Gap Campaign Steering Committee: Melbourne, Australia, 2020. [Google Scholar]
- Jackson Pulver, L.; Haswell, M.R.; Ring, I.; Waldon, J.; Clark, W.; Whetung, V.; Kinnon, D.; Graham, C.; Chino, M.; LaValley, J.; et al. Indigenous Health—Australia, Canada, Aotearoa New Zealand, and the United States—Laying Claim to a Future that Embraces Health for Us All: World Health Report; World Health Organisation: Geneva, Switzerland, 2010. [Google Scholar]
- Anderson, I.; Robson, B.; Connolly, M.; Al-Yaman, F.; Bjertness, E.; King, A.; Tynan, M.; Madden, R.; Bang, A.; Coimbra, C.E., Jr.; et al. Indigenous and tribal peoples’ health (The Lancet—Lowitja Institute Global Collaboration): A population study. Lancet 2016, 388, 131–157. [Google Scholar] [CrossRef]
- CASP Checklist 2019. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 31 May 2021).
- Harfield, S.; Pearson, O.; Morey, K.; Kite, E.; Canuto, K.; Glover, K.; Gomersall, J.S.; Carter, D.; Davy, C.; Aromataris, E.; et al. Assessing the quality of health research from an Indigenous perspective: The Aboriginal and Torres Strait Islander quality appraisal tool. BMC Med. Res. Methodol. 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guthridge, S.; Li, L.; Silburn, S.; Li, S.Q.; McKenzie, J.; Lynch, J. Impact of perinatal health and socio-demographic factors on school education outcomes: A population study of Indigenous and non-Indigenous children in the Northern Territory. J. Paediatr. Child. Health 2015, 51, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Guthridge, S.; Li, L.; Silburn, S.; Li, S.Q.; McKenzie, J.; Lynch, J. Early influences on developmental outcomes among children, at age 5, in Australia’s Northern Territory. Early Child. Res. Q. 2016, 35, 124–134. [Google Scholar] [CrossRef]
- Strobel, N.A.; Richardson, A.; Shepherd, C.C.; McAuley, K.E.; Marriott, R.; Edmond, K.M.; McAullay, D.R. Modelling factors for Aboriginal and Torres Strait Islander child neurodevelopment outcomes: A latent class analysis. Paediatr. Perinat. Epidemiol. 2020, 34, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Ou, L.; Chen, J.; Hillman, K. Have the health gaps between Indigenous and non-Indigenous Australian children changed over time? Results from an Australian National Representative Longitudinal Study. Matern. Child Health J. 2012, 16, 814–823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, H.J.; Beach, J.; Senthilselvan, A. Prevalence and risk factors of asthma in off-reserve Aboriginal children and adults in Canada. Can. Respir. J. 2012, 19, e68–e74. [Google Scholar] [CrossRef] [Green Version]
- Senthilselvan, A.; Niruban, S.J.; King, M.; Majaesic, C.; Veugelers, P.; Laing, L.; Rowe, B.H. Prevalence and risk factors of asthma in First Nations children living on reserves in Canada. Can. J. Public Health 2016, 106, e483–e488. [Google Scholar] [CrossRef]
- Westrupp, E.M.; D’Esposito, F.; Freemantle, J.; Mensah, F.K.; Nicholson, J.M. Health outcomes for Australian Aboriginal and Torres Strait Islander children born preterm, low birthweight or small for gestational age: A nationwide cohort study. PLoS ONE 2019, 14, e0212130. [Google Scholar] [CrossRef]
- Kim, S.; Macaskill, P.; Baur, L.A.; Hodson, E.M.; Daylight, J.; Williams, R.; Kearns, R.; Vukasin, N.; Lyle, D.M.; Craig, J.C. The differential effect of socio-economic status, birth weight and gender on body mass index in Australian Aboriginal Children. Int. J. Obes. 2016, 40, 1089–1095. [Google Scholar] [CrossRef]
- Gee, G.D.P.; Schultz, C.; Hart, A.; Kelley, K. Understanding Social and Emotional Wellbeing and Mental Health from an Aboriginal and Torres Strait Islander perspective. In Working Together: Aboriginal and Torres Strait Islander Health and Wellbeing Principles and Practice, 2nd ed.; Chapter 3; Dudgeon, P., Milroy, H., Walker, R., Eds.; Australian Council for Education Research and Telethon Institute for Child Health Research, Office for Aboriginal and Torres Strait Islander Health, Department of Health and Ageing: Canberra, Autrialia, 2014. [Google Scholar]
- Lin, C.Y.; Loyola-Sanchez, A.; Boyling, E.; Barnabe, C. Community engagement approaches for Indigenous health research: Recommendations based on an integrative review. BMJ Open 2020, 10, e039736. [Google Scholar] [CrossRef] [PubMed]
- Department of Social Services. Footprints in Time the Longitudinal Study of Indigenous Children (LSIC): Australian Government. Available online: https://www.dss.gov.au/about-the-department/publications-articles/research-publications/longitudinal-data-initiatives/footprints-in-time-the-longitudinal-study-of-indigenous-children-lsic (accessed on 27 July 2021).
- National Health and Medical Research Council. Ethical Conduct in Research with Aboriginal and Torres Strait Islander Peoples and Communities: Guidelines for Researchers and Stakeholders; Commonwealth of Australia: Canberra, Autralia, 2018. [Google Scholar]
- Canadian Institutes of Health Research. Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council, Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans; Chapter 9; Research Involving the First Nations; Inuit and Métis Peoples of Canada: Ottawa, ON, Canada, 2018. [Google Scholar]
- SAHMRI. South Australian Aboriginal Health Research Accord: South Australian Health and Medical Research Institute. 2014. Available online: https://www.sahmri.org/aboriginal-health-equity-theme/resource-6/ (accessed on 15 June 2021).
- Casey, P.H. Growth of Low Birth Weight Preterm Children. Semin Perinatol. 2008, 32, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.K.; Chang, A.B.; Anderson, J.; Dunbar, M.; Arnold, D.; O’Grady, K.A.F. Characteristics and respiratory risk profile of children aged less than 5 years presenting to an urban, Aboriginal-friendly, comprehensive primary health practice in Australia. J. Paediatr. Child Health 2017, 53, 636–643. [Google Scholar] [CrossRef]
- Grant, C.C.; Wall, C.R.; Gibbons, M.J.; Morton, S.M.; Santosham, M.; Black, R.E. Child nutrition and lower respiratory tract disease burden in New Zealand: A global context for a national perspective. J. Paediatr. Child. Health 2011, 47, 497–504. [Google Scholar] [CrossRef] [PubMed]
- McEwen, E.C.; Guthridge, S.L.; He, V.Y.; McKenzie, J.W.; Boulton, T.J.; Smith, R. What birthweight percentile is associated with optimal perinatal mortality and childhood education outcomes? Am. J. Obstet. Gynecol. 2018, 218, S712–S724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bankhead, C.R.S.E.; Nunan, D. Information bias. Sackett Catalogue of Biases. 2019. Available online: https://catalogofbias.org/biases/information-bias/ (accessed on 23 March 2021).
| Paper | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Author | Year | Country | Study Type | Setting | Sample (n) | Indigenous Sample (n) | Female (%) | Administrative Records | Caregiver Survey | Caregiver Interview | Child Survey | Clinical Assessment |
| Ou [21] | 2011 | Australia | Prospective Longitudinal | Community | 10,090 | 419 | 49.5 | X | X | |||
| Guthridge [22] | 2015 | Australia | Record Linkage | Community | 7601 | 4603 | 48.7 | X | ||||
| Guthridge [23] | 2016 | Australia | Record Linkage | Community | 1922 | 1110 | 53 | X | ||||
| Kim [24] | 2016 | Australia | Prospective Longitudinal | Community | 3418 | 1949 | 49.4 | X | X | |||
| Westrupp [25] | 2019 | Australia | Prospective Longitudinal | Community | 1483 | 1485 | 49.9 | X | X | |||
| Strobel [26] | 2019 | Australia | Record Linkage | Community | 2715 | 2715 | 50.4 | X | ||||
| Chang [27] | 2012 | Canada | Cross-sectional | Community | 48,921 | 48,921 | 48.2 | X | X | |||
| Senthilselvan [28] | 2015 | Canada | Cross-sectional | Community | 6657 | 6657 | 40.2 | X | ||||
| Study Details | Child Outcomes | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Author | Population | Age at Outcome (Years) | Birthweight Source | Low Birthweight | Small for Gest. Age | Measures | Asthma | BMI | Global Health | Disability | Academic Performance | Developmental Vulnerability |
| n (%) | n (%) | |||||||||||
| Ou | Indigenous Australian | 4–9 | Caregiver | B-cohort: 11 (5) | Physical Outcome Index Composite | X | ||||||
| K-cohort: 8 (4) | ||||||||||||
| Guthridge (2015) | Indigenous Australian | 8 | Administrative records | 580 (13) | National Assessment Program (reading and numeracy) | X | ||||||
| Guthridge (2016) | Indigenous Australian | 4–6 | Administrative records | 142 (13) | Australian Early Development Census | X | ||||||
| Kim | Indigenous Australian | 11 | Caregiver | 102 (5) | Height and weight | X | ||||||
| Westrupp | Indigenous Australian | 5–8 | Caregiver | 430 (29) | 430 (29) | Height, weight, SF12 global health item, caregiver report of disability | X | X | X | |||
| Strobel | Indigenous Australian | 5 | Administrative records | 323 (12) | Australian Early Development Census | X | ||||||
| Chang | Indigenous Canadian | 6–14 | Caregiver | 11,741 (24) | Study designed measure | X | ||||||
| Senthilselvan | Indigenous Canadian | 0–4 | Caregiver | Not reported | Study designed measure | X | ||||||
| 5–11 | ||||||||||||
| First Author | Critical Appraisal Quality | Cultural Appraisal Quality |
|---|---|---|
| Ou | High | Low |
| Guthridge (2015) | High | Low |
| Guthridge (2016) | Medium | Low |
| Kim | High | Low |
| Westrupp | High | Low |
| Strobel | High | Medium |
| Chang | High | Low |
| Senthilselvan | Medium | Low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batchelor, M.; Brown, S.J.; Glover, K.; Gartland, D. A Systematic Review of Child Health and Developmental Outcomes Associated with Low Birthweight and/or Small for Gestational Age in Indigenous Children from Australia, Canada and New Zealand. Int. J. Environ. Res. Public Health 2021, 18, 12669. https://doi.org/10.3390/ijerph182312669
Batchelor M, Brown SJ, Glover K, Gartland D. A Systematic Review of Child Health and Developmental Outcomes Associated with Low Birthweight and/or Small for Gestational Age in Indigenous Children from Australia, Canada and New Zealand. International Journal of Environmental Research and Public Health. 2021; 18(23):12669. https://doi.org/10.3390/ijerph182312669
Chicago/Turabian StyleBatchelor, Madeleine, Stephanie J. Brown, Karen Glover, and Deirdre Gartland. 2021. "A Systematic Review of Child Health and Developmental Outcomes Associated with Low Birthweight and/or Small for Gestational Age in Indigenous Children from Australia, Canada and New Zealand" International Journal of Environmental Research and Public Health 18, no. 23: 12669. https://doi.org/10.3390/ijerph182312669
APA StyleBatchelor, M., Brown, S. J., Glover, K., & Gartland, D. (2021). A Systematic Review of Child Health and Developmental Outcomes Associated with Low Birthweight and/or Small for Gestational Age in Indigenous Children from Australia, Canada and New Zealand. International Journal of Environmental Research and Public Health, 18(23), 12669. https://doi.org/10.3390/ijerph182312669






