Peri-Implantitis: Application of a Protocol for the Regeneration of Deep Osseous Defects. A Retrospective Case Series
Abstract
:1. Introduction
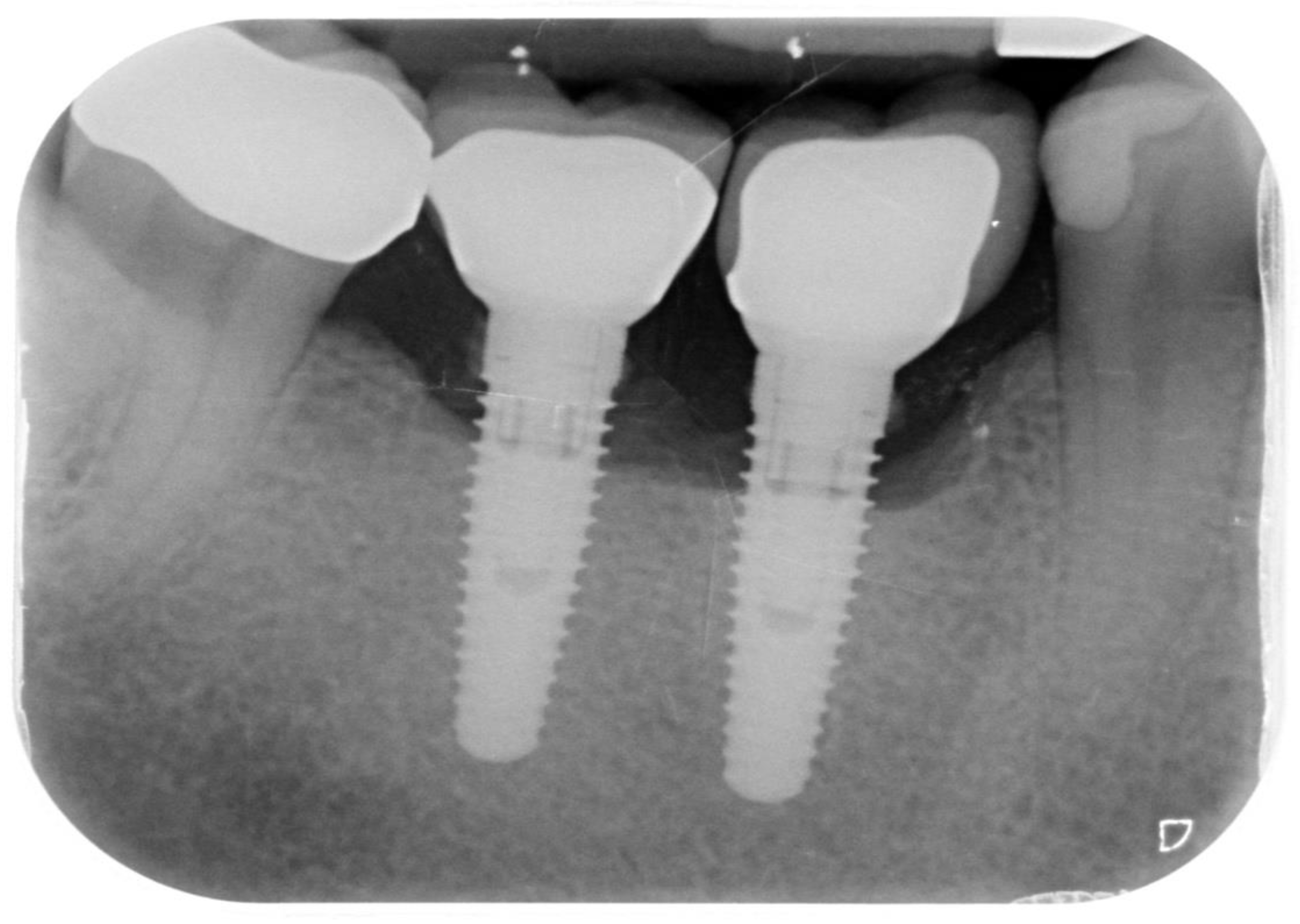
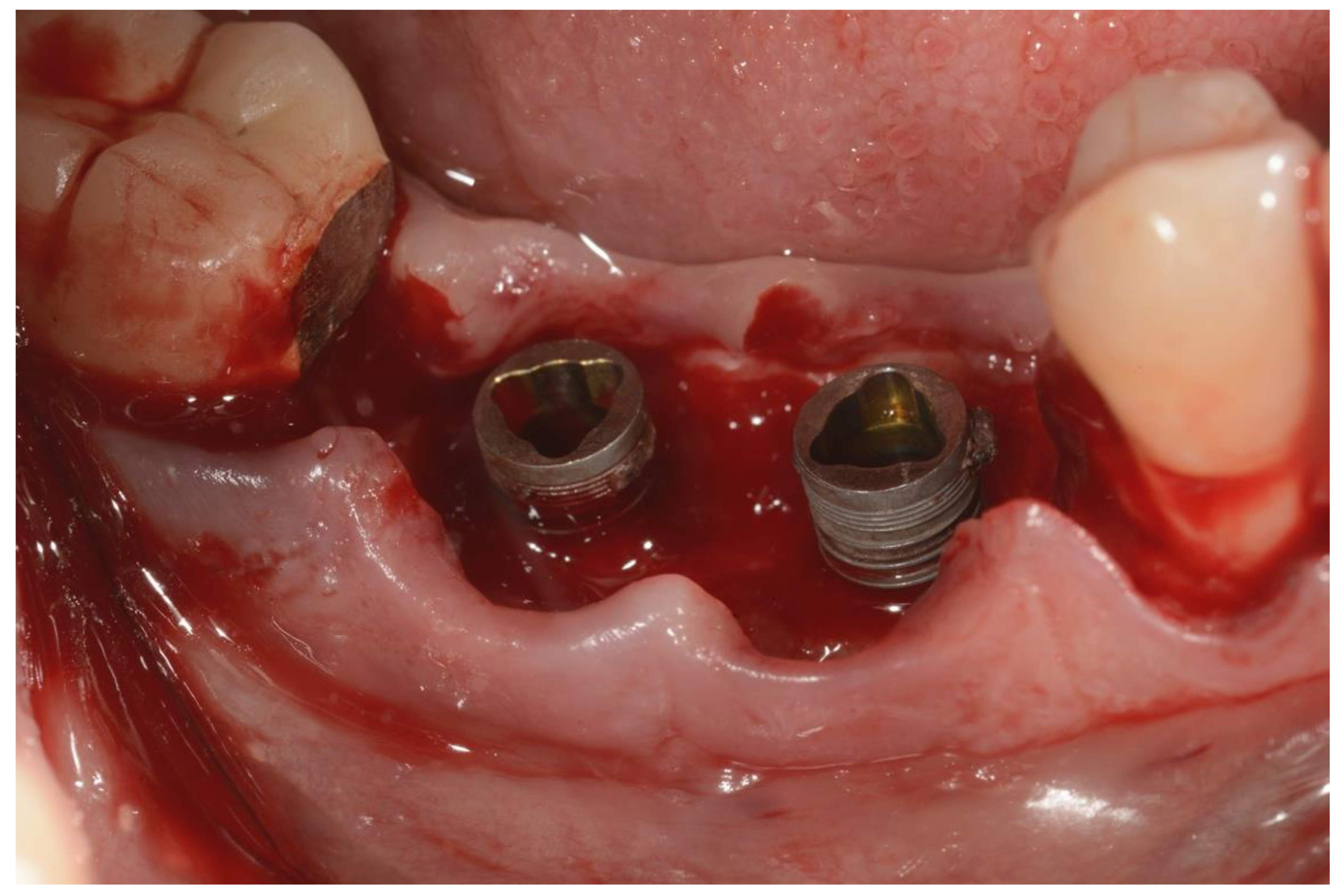
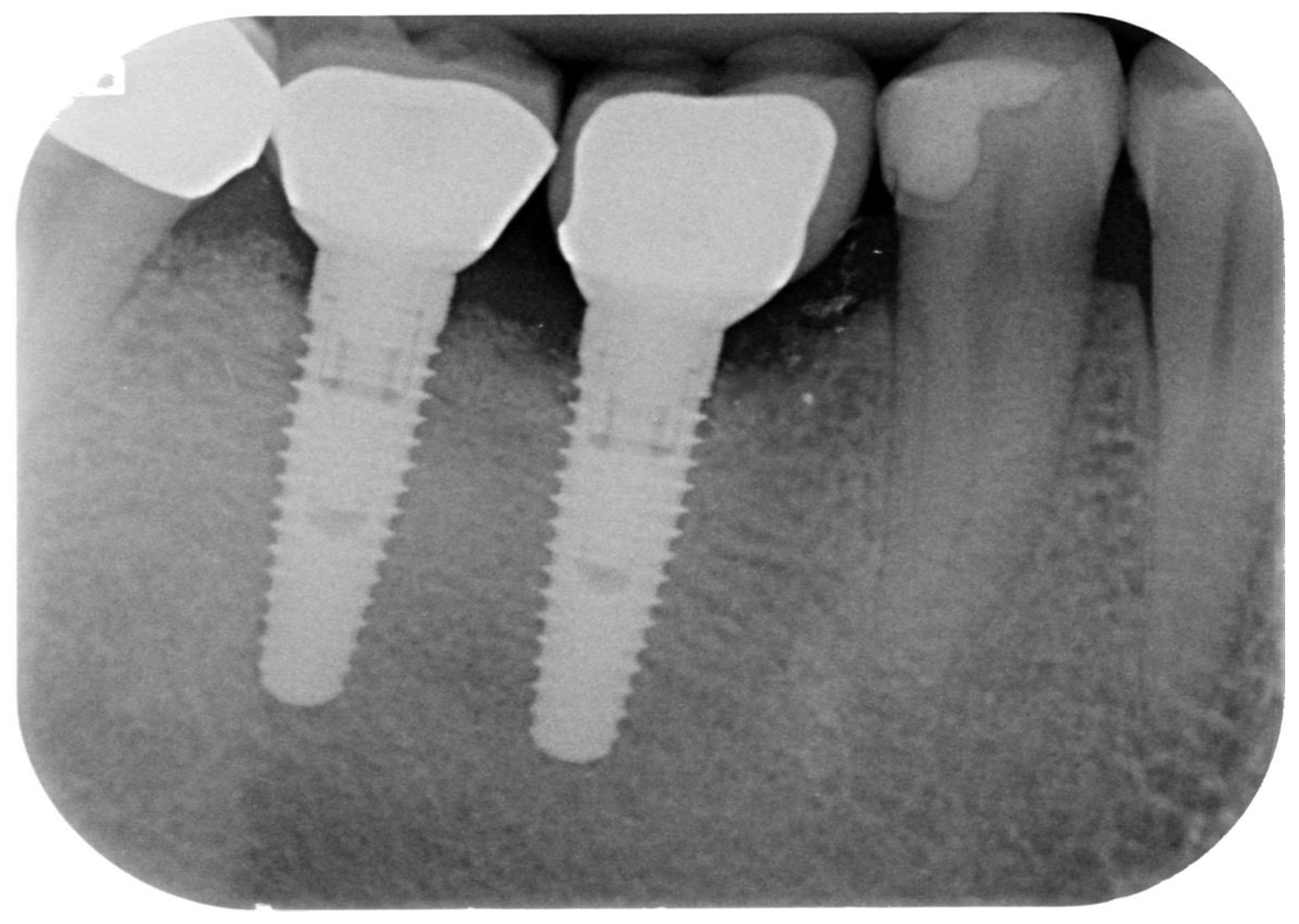
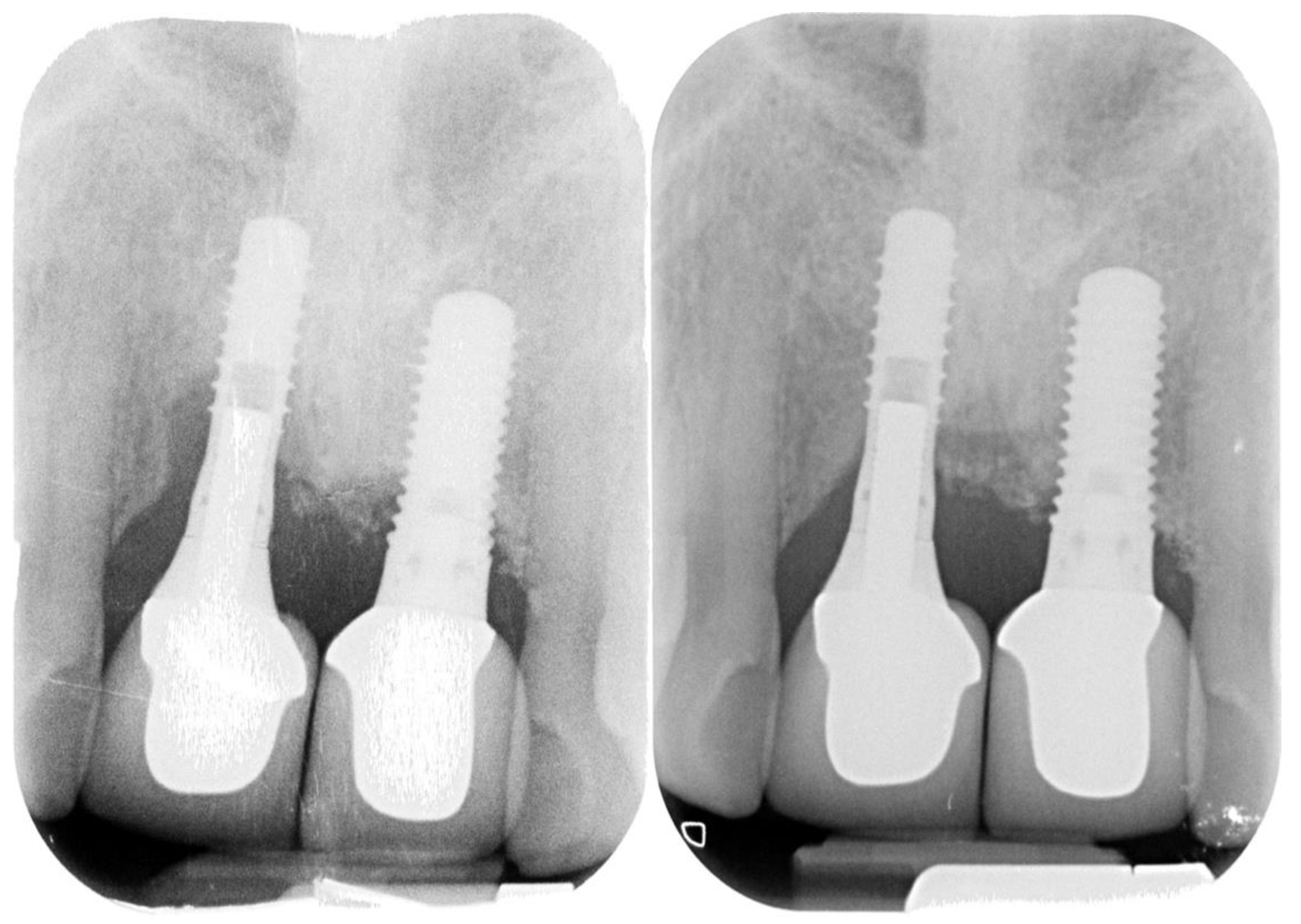
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.-L. Peri-implantitis. J. Periodontol. 2018, 89, S267–S290. [Google Scholar] [CrossRef] [PubMed]
- Levignac, J. L’ostéolyse periimplantaire, périimplantose—Périimplantite. Rev. Fr. D’Odonto-Stomatol. 1965, 12, 1251–1260. [Google Scholar]
- Wilson, T.G., Jr. The positive relationship between excess cement and peri-implant disease: A prospective clinical endoscopic study. J. Periodontol. 2009, 80, 1388–1392. [Google Scholar] [CrossRef] [PubMed]
- Mombelli, A.; van Oosten, M.A.; Schurch, E.; Land, N.P. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol. Immunol. 1987, 2, 145–151. [Google Scholar] [CrossRef]
- Valente, N.A.; Andreana, S. Peri-implant disease: What we know and what we need to know. J. Periodontal Implant. Sci. 2016, 46, 136–151. [Google Scholar] [CrossRef] [Green Version]
- Mombelli, A. Maintenance therapy for teeth and implants. Periodontol. 2000 2019, 79, 190–199. [Google Scholar] [CrossRef]
- Lindhe, J.; Meyle, J. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontol. J. Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papathanasiou, E.; Finkelman, M.; Hanley, J.; Parashis, A.O. Prevalence, Etiology and Treatment of Peri-Implant Mucositis and Peri-Implantitis: A Survey of Periodontists in the United States. J. Periodontol. 2016, 87, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Salvi, G.E.; Aglietta, M.; Eick, S.; Sculean, A.; Lang, N.P.; Ramseier, C.A. Reversibility of experimental peri-implant mucositis compared with experimental gingivitis in humans. Clin. Oral Implant. Res. 2012, 23, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Bordin, S.; Flemmig, T.F.; Verardi, S. Role of fibroblast populations in peri-implantitis. Int. J. Oral Maxillofac. Implant. 2009, 24, 197–204. [Google Scholar]
- Verardi, S.; Quaranta, M.; Bordin, S. Peri-implantitis fibroblasts respond to host immune factor C1q. J. Periodontal Res. 2010, 46, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Doornewaard, R.; Jacquet, W.; Cosyn, J.; de Bruyn, H. How do peri-implant biologic parameters correspond with implant survival and peri-implantitis? A critical review. Clin. Oral Implant. Res. 2018, 29, 100–123. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Ortiz, G.A.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri- implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S286–S291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramanauskaite, A.; Fretwurst, T.; Schwarz, F. Efficacy of alternative or adjunctive measures to conventional non-surgical and surgical treatment of peri-implant mucositis and peri-implantitis: A systematic review and meta-analysis. Int. J. Implant. Dent. 2021, 7, 1–61. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Roos-Jansåker, A.M.; Claffey, N. Non-surgical treatment of peri-implant mucositis and peri-implantitis: A literature review. J. Clin. Periodontol. 2008, 35, 305–315. [Google Scholar] [CrossRef]
- Romeo, E.; Ghisolfi, M.; Murgolo, N.; Chiapasco, M.; Lops, D.; Vogel, G. Therapy of peri-implantitis with resective surgery. Clin. Oral Implant. Res. 2004, 16, 9–18. [Google Scholar] [CrossRef]
- Matarasso, S.; Iorio Siciliano, V.; Aglietta, M.; Andreuccetti, G.; Salvi, G.E. Clinical and radiographic outcomes of a combined resective and regenerative approach in the treatment of peri-implantitis: A prospective case series. Clin. Oral Implant. Res. 2014, 25, 761–767. [Google Scholar] [CrossRef]
- Schwarz, F.; Sahm, N.; Becker, J. Combined surgical therapy of advanced peri-implantitis lesions with concomitant soft tissue volume augmentation. A case series. Clin. Oral Implant. Res. 2014, 25, 132–136. [Google Scholar] [CrossRef]
- Schwarz, F.; Alcoforado, G.; Guerrero, A.; Jönsson, D.; Klinge, B.; Lang, N.; Mattheos, N.; Mertens, B.; Pitta, J.; Ramanauskaite, A.; et al. Peri-implantitis: Summary and consensus statements of group 3. The 6th EAO Consensus Conference 2021. Clin. Oral Implant. Res. 2021, 32, 245–253. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Pini-Prato, G.; Cortellini, P. Effect of cigarette smoking on periodontal healing following GTR in infrabony defects. J. Clin. Periodontol. 1995, 22, 229–234. [Google Scholar] [CrossRef]
- Hentenaar, D.F.M.; de Waal, Y.C.M.; Strooker, H.; Meijer, H.J.A.; van Winkelhoff, A.-J.; Raghoebar, G.M. Implant decontamination with phosphoric acid during surgical peri-implantitis treatment: A RCT. Int. J. Implant. Dent. 2017, 3, 1–9. [Google Scholar] [CrossRef]
- Bennani, V.; Hwang, L.; Tawse-Smith, A.; Dias, G.J.; Cannon, R.D. Effect of air-polishing on titanium surfaces, biofilm removal, and biocompatibility: A pilot study. BioMed Res. Int. 2015, 2015, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, L.; Zhang, P.; Wang, X.; Kasugai, S. A doxycycline-treated hydroxyapatite implant surface attenuates the progression of peri-implantitis: A radiographic and histological study in mice. Clin. Implant. Dent. Relat. Res. 2019, 21, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Martín, I.; Paeng, K.; Park, H.; Cha, J.K.; Jung, U.W.; Sanz, M. Significance of implant design on the efficacy of different peri-implantitis decontamination protocols. Clin. Oral Investig. 2020, 25, 3589–3597. [Google Scholar] [CrossRef]
- Almohandes, A.; Carcuac, O.; Abrahamsson, I.; Lund, H.; Berglundh, T. Re-osseointegration following reconstructive surgical therapy of experimental peri-implantitis. A pre-clinical in vivo study. Clin. Oral Implant. Res. 2019, 30, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Rühling, A.; Kocher, T.; Kreusch, J.; Plagmann, H.-C. Treatment of subgingival implant surfaces with Teflon®-coated sonic and ultrasonic scaler tips and various implant curettes. An in vitro study. Clin. Oral Implant. Res. 1994, 5, 19–29. [Google Scholar] [CrossRef]
- Blasi, A.; Iorio-Siciliano, V.; Pacenza, C.; Pomingi, F.; Matarasso, S.; Rasperini, G. Biofilm removal from implants supported restoration using different instruments: A 6-month comparative multicenter clinical study. Clin. Oral Implant. Res. 2016, 27, e68–e73. [Google Scholar] [CrossRef]
- França, F.L.; Honorio-França, A.C.; Honorio, M.S.; da Silva, F.H.; Fujimori, M.; França, E.L.; da Silva Araújo, F.G. Dental implant surfaces treated with phosphoric acid can modulate cytokine production by blood MN cells. Braz. Oral Res. 2019, 33, e040. [Google Scholar] [CrossRef]
- Lasserre, J.; Brecx, M.; Toma, S. Implantoplasty Versus Glycine Air Abrasion for the Surgical Treatment of Peri-implantitis: A Randomized Clinical Trial. Int. J. Oral Maxillofac. Implant. 2020, 35, 197–206. [Google Scholar] [CrossRef]
- Keim, D.; Nickles, K.; Dannewitz, B.; Ratka, C.; Eickholz, P.; Petsos, H. In vitro efficacy of three different implant surface decontamination methods in three different defect configurations. Clin. Oral Implant. Res. 2019, 30, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Fageeh, H.N.; Moussa, H.; Maddi, A.; Ciancio, S.; Dziak, R. Nano-Calcium Sulfate as a Local Delivery System for Antibiotics. Int. J. Dent. Oral Health 2017, 3, 1–7. [Google Scholar]
- Patianna, G.; Valente, N.A.; D’Addona, A.; Andreana, S. In vitro evaluation of controlled-release 14% doxycycline gel for decontamination of machined and sandblasted acid-etched implants. J. Periodontol. 2018, 89, 325–330. [Google Scholar] [CrossRef]
- Mombelli, A.; Feloutzis, A.; Brägger, U.; Lang, N.P. Treatment of peri-implantitis by local delivery of tetracycline. Clinical, microbiological and radiological results. Clin. Oral Implant. Res. 2001, 12, 287–294. [Google Scholar] [CrossRef]
- Mercado, F.; Hamlet, S.; Ivanovski, S. Regenerative surgical therapy for peri-implantitis using deproteinized bovine bone mineral with 10% collagen, enamel matrix derivative and Doxycycline—A prospective 3-year cohort study. Clin. Oral Implant. Res. 2018, 29, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, M.; Pittoni, D.; Roccuzzo, A.; Charrier, L.; Dalmasso, P. Surgical treatment of peri-implantitis intrabony lesions by means of deproteinized bovine bone mineral with 10% collagen: 7-year-results. Clin. Oral Implant. Res. 2017, 28, 1577–1583. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, M.; Fierravanti, L.; Pittoni, D.; Dalmasso, P.; Roccuzzo, A. Implant survival after surgical treatment of peri-implantitis lesions by means of deproteinized bovine bone mineral with 10% collagen: 10-year results from a prospective study. Clin. Oral Implant. Res. 2020, 31, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Sharma, D. Management of Peri-Implant Diseases: A Survey of Australian Periodontists. Dent. J. 2020, 8, 100. [Google Scholar] [CrossRef]
- Irshad, M.; Alam, M.K.; Ali, S.; Alawneh, A.; Alhadi, M.; Alhadi, A.; Alfawzan, A.A. Effects of Implant Surface Debridement and Systemic Antibiotics on the Clinical and Microbiological Variables of Periimplantitis. BioMed Res. Int. 2021, 2021, 6660052. [Google Scholar] [CrossRef]
- Blanco, C.; Pico, A.; Dopico, J.; Gándara, P.; Blanco, J.; Liñares, A. Adjunctive benefits of systemic metronidazole on non-surgical treatment of peri-implantitis. A randomized placebo-controlled clinical trial. Clin. Periodontol. 2021, in press. [Google Scholar] [CrossRef]
- Sinno, S.; Lee, D.S.; Khachemoune, A. Vitamins and cutaneous wound healing. J. Wound Care 2011, 20, 287–293. [Google Scholar] [CrossRef]
- Tian, C.F.; Su, B.Y.; Li, Y.J.; Tong, Y.H.; Zhao, X.H.; Liang, J.Y.; Li, S.B.; Gao, B.L. Management of antibiotic-associated pseudomembranous colitis in Non-hospitalized and hospitalized patients. Pak. J. Pharm. Sci. 2016, 29, 1805–1810. [Google Scholar] [PubMed]
- Esposito, M.; Grusovin, M.G.; Kakisis, I.; Coulthard, P.; Worthington, H.V. Interventions for replacing missing teeth: Treatment of perimplantitis. Cochrane Database Syst. Rev. 2008, 1, 1–42. [Google Scholar]



| Patients | Implants | Sex | Mean Age | Smokers (n.) | History of Periodontitis (n) | BoP | Pus | Mean PD |
|---|---|---|---|---|---|---|---|---|
| 23 | 29 | 11/12 | 53.78 | 9 | 11 | 28 | 15 | 8.14 ± 1.156 mm |
| Baseline | One Year | Final | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean + SD (mm) | Median + MAD (mm) | 95% CI | Mean + SD (mm) | Median + MAD (mm) | 95% CI | Mean + SD (mm) | Median + MAD (mm) | 95% CI | ||
| PD | 8.14 ± 1.156 | 8 ± 1 | 7.7, 8.6 | 3.72 ± 0.649 | 4 ± 4 | 3.5, 4 | 4.14 ± 1.093 | 4 ± 4 | 3.7, 4.5 | p < 0.0005 |
| n. of sites | n. of sites | |||||||||
| BoP | 28 | 7 | p < 0.0005 | |||||||
| Pus | 15 | 1 | p = 0.001 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verardi, S.; Valente, N.A. Peri-Implantitis: Application of a Protocol for the Regeneration of Deep Osseous Defects. A Retrospective Case Series. Int. J. Environ. Res. Public Health 2021, 18, 12658. https://doi.org/10.3390/ijerph182312658
Verardi S, Valente NA. Peri-Implantitis: Application of a Protocol for the Regeneration of Deep Osseous Defects. A Retrospective Case Series. International Journal of Environmental Research and Public Health. 2021; 18(23):12658. https://doi.org/10.3390/ijerph182312658
Chicago/Turabian StyleVerardi, Simone, and Nicola Alberto Valente. 2021. "Peri-Implantitis: Application of a Protocol for the Regeneration of Deep Osseous Defects. A Retrospective Case Series" International Journal of Environmental Research and Public Health 18, no. 23: 12658. https://doi.org/10.3390/ijerph182312658
APA StyleVerardi, S., & Valente, N. A. (2021). Peri-Implantitis: Application of a Protocol for the Regeneration of Deep Osseous Defects. A Retrospective Case Series. International Journal of Environmental Research and Public Health, 18(23), 12658. https://doi.org/10.3390/ijerph182312658







