Determinants of the Underlying Causes of Mortality during the First Wave of COVID-19 Pandemic in Saudi Arabia: A Descriptive National Study
Abstract
:1. Introduction
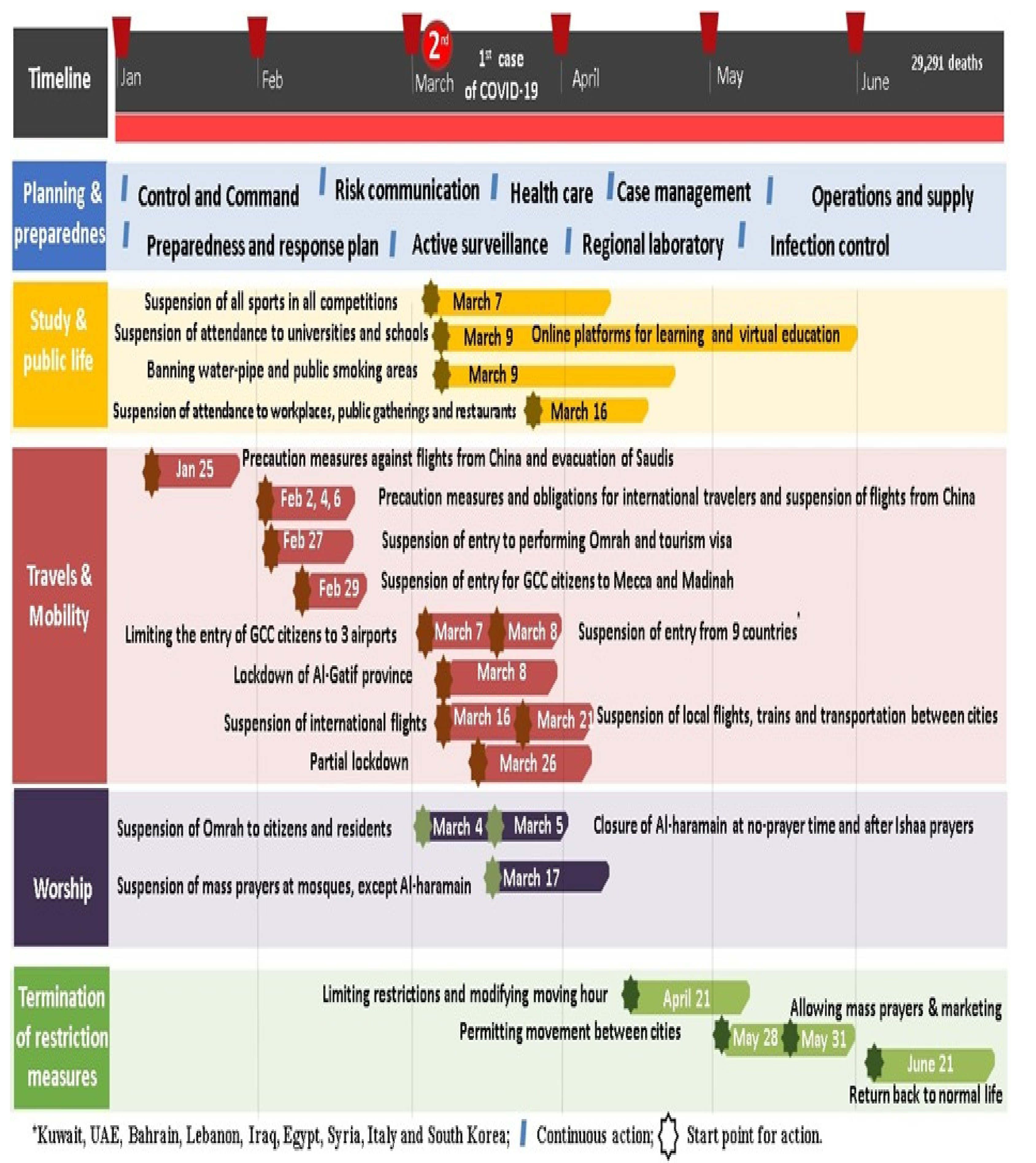
2. Methodology
2.1. Participants
2.2. Data Collection
2.3. Statistical Analysis
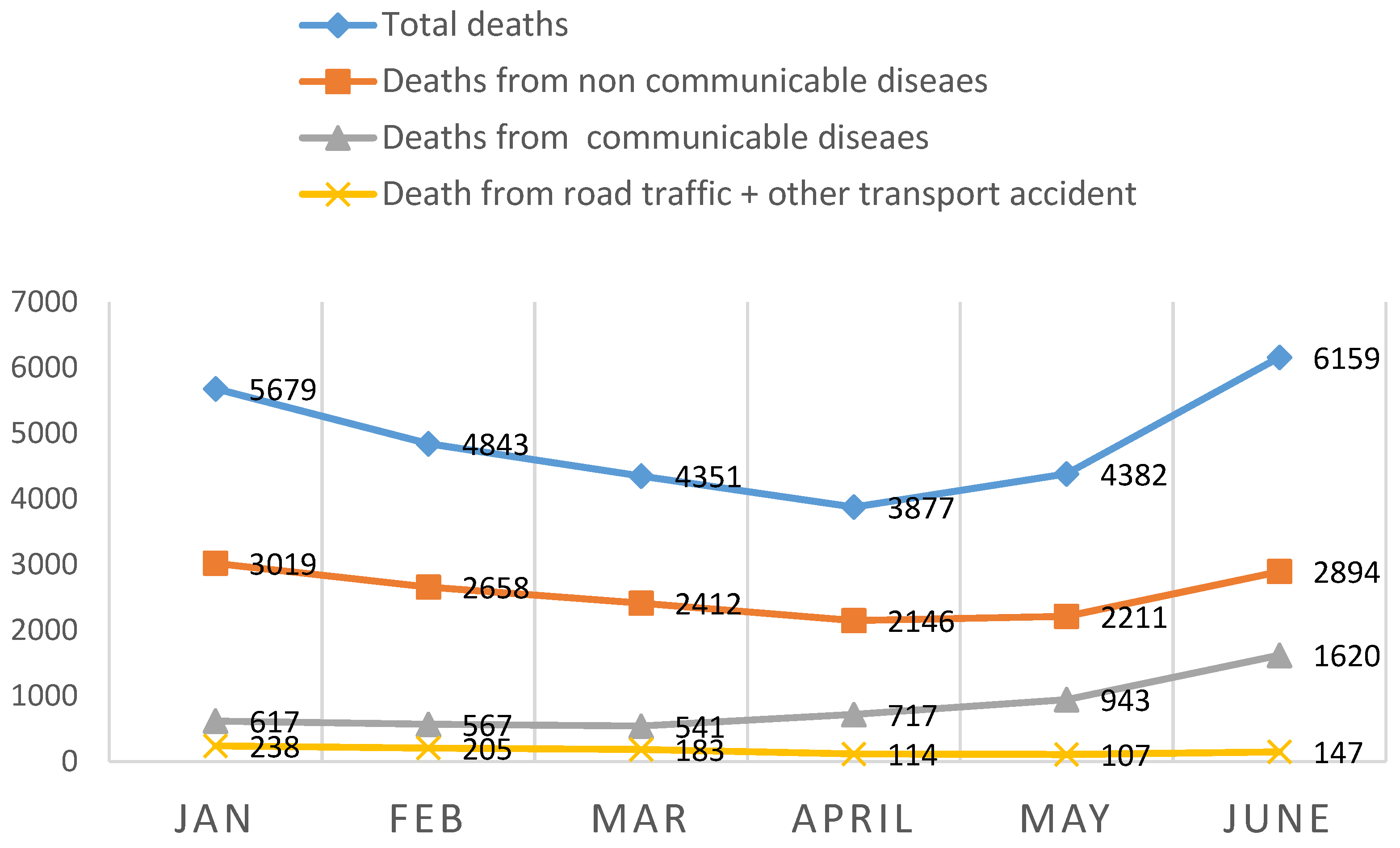
3. Results
4. Discussion
4.1. Limitations
4.2. Strength
5. Conclusions
6. Recommendations
7. Ethical Considerations
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Director-General is Opening Remarks at the Media Briefing on COVID-19–11 March 2020. 2020. Published online March 11. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 23 April 2020).
- World Health Organization. WHO/Europe Past Pandemics. 2020. Available online: http://www.euro.who.int/en/health-topics/communicable-diseases/influenza/pandemic-influenza/past-pandemics (accessed on 24 April 2020).
- World Health Organization. Global Health Observatory Country Views. 2020. Available online: https://apps.who.int/gho/data/node.country.country-SAU (accessed on 20 July 2020).
- He, F.; Deng, Y.; Li, W. Coronavirus disease 2019: What we know? J. Med. Virol. 2020, 92, 719–725. [Google Scholar] [CrossRef] [Green Version]
- O’Donovan, M.R.; Sezgin, D.; Liew, A.; O’Caoimh, R. Burden of disease, disability-adjusted life years and frailty prevalence. QJM Int. J. Med. 2019, 112, 261–267. [Google Scholar] [CrossRef]
- Azarpazhooh, M.R.; Morovatdar, N.; Avan, A.; Phan, T.G.; Divani, A.A.; Yassi, N.; Stranges, S.; Silver, B.; Biller, J.; Tokazebani Belasi, M.; et al. COVID-19 Pandemic and Burden of Non-Communicable Diseases: An Ecological Study on Data of 185 Countries. J Stroke Cerebrovasc. Dis. 2020, 29, 105089. [Google Scholar] [CrossRef]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, Y.S.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar]
- Lopez, A.D.; Mathers, C.D.; Ezzati, M.; Jamison, D.T.; Murray, C.J. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 2006, 367, 1747–1757. [Google Scholar]
- World Health Organization. Global Health Observatory (GHO) Data. 2020. Available online: https://www.who.int/gho/ncd/mortality_morbidity/en/ (accessed on 7 July 2020).
- World Health Organization. Non-Communicable Diseases Fact Sheet. 2020. Available online: http://www.who.int/mediacentre/factsheets/fs355/en/ (accessed on 13 November 2013).
- Alwan, A.; Maclean, D.R.; Riley, L.M.; d’Espaignet, E.T.; Mathers, C.D.; Stevens, G.A.; Bettcher, D. Monitoring and surveillance of chronic non-communicable diseases: Progress and capacity in high-burden countries. Lancet 2010, 376, 1861–1868. [Google Scholar]
- Parkin, D.M.; Bray, F.; Ferlay, J.; Jemal, A. Cancer in Africa 2012. Cancer Epidemiol. Biomarkers Prev. 2014, 23, 953–966. [Google Scholar]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar]
- World Health Organization. Under Five Mortalities. 2010. Available online: http://www.who.int/whosis/en/index.html (accessed on 22 September 2020).
- Kumar, A.; Mohanty, S.K. Rich-Poor Gap in Infant and Under Five Mortalities in Urban India, 1992–05; International Institute for Population Sciences: Mumbai, India, 2009. [Google Scholar]
- Stevens, A.G.; Mathers, D.C.; Beard, R.J. Global mortality trends and patterns in older women. Bull. World Health Organ. 2013, 91, 630–639. [Google Scholar] [CrossRef]
- National Centre for Health Statistics. Health, United States, 1986 and Prevention Profile; Public Health Service; US Department of Health and Human Services: Hyattsville, MA, USA, 1989; DHHS publication no. (PHS) 87-1232.
- Herzallah, H.K.; Antonisamy, B.R.; Shafee, M.H.; Al-Otaibi, S.T. Temporal trends in the incidence and demographics of cancers, communicable diseases, and non-communicable diseases in Saudi Arabia over the last decade. Saudi Med. J. 2019, 40, 277–286. [Google Scholar] [CrossRef]
- Central Department of Statistics & Information. Highlights Demographic Survey 1428H (2007). In Riyadh (KSA): National e-Government Portal; 2007. Available online: www.cdsi.gov.sa (accessed on 29 August 2020).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems; the 10th Revision; World Health Organization: Geneve, Switzerland, 1992; Volume 1. [Google Scholar]
- Ahmad, O.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.; Lozano, R.; Inoue, M. Age Standardization of Rates: A New WHO Standard; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Mathers, C.D.; Lopez, A.D.; Murray, C.J.L. The Burden of Disease and Mortality by Condition: Data, Methods and Results for 2001. In Global Burden of Disease and Risk Factors; Lopez, A.D., Mathers, C.D., Ezzati, M., Jamison, D.T., Murray, C.J.L., Eds.; Oxford University Press: New York, NY, USA, 2006; pp. 45–240. [Google Scholar]
- Osypuk, T.L.; Joshi, P.; Geronimo, K.; Acevedo-Garcia, D. Do Social and Economic Policies Influence Health? A Review. Curr. Epidemiol. Rep. 2014, 1, 149–164. [Google Scholar] [CrossRef]
- The Global Burden of Disease (2004): 2004 Update; World Health Organization: Geneva, Switzerland, 2008.
- Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef] [Green Version]
- Janati, A.; Hosseiny, M.; Gouya, M.M.; Moradi, G.; Ghaderi, E. Communicable Disease Reporting Systems in the World: A Systematic Review Article. Iran. J. Public Health 2015, 44, 1453–1465. [Google Scholar]
- Sahal, N.; Reintjes, R.; Mahgoub, A.E.; Aro, A.R. Staff views about the quality of the communicable diseases surveillance system in Khartoum state, Sudan, 2005–2007: A qualitative study. East. Mediterr. Health J. 2011, 17, 565–569. [Google Scholar]
- Shinde, R.R.; Kembhavi, R.S.; Kuwatada, J.S.; Khandednath, T.S. To develop a public private partnership model of disease notification as a part of integrated disease surveillance project (IDSP) for private medical practitioners in Mumbai City, India. Glob. J. Med. Public Health 2012, 1, 1–11. [Google Scholar]
- Bino, S.; Cavaljuga, S.; Kunchev, A.; Lausevic, D.; Kaic, B.; Pistol, A.; Kon, P.; Karadjovski, Z.; Georghita, S.; Cicevalieva, S. South-eastern European Health Network (SEEHN) communicable diseases surveillance: A decade of bridging trust and collaboration. Emerg. Health Threats J. 2013, 6, 1–7. [Google Scholar]
- Cheng, Z.J.; Shan, J. 2019 Novel coronavirus: Where we are and what we know. Infection 2020, 48, 155–163. [Google Scholar]
- Nethan, S.; Sinha, D.; Mehrotra, R. Non-Communicable Disease Risk Factors and their Trends in India. Asian Pac. J. Cancer Prev. APJCP 2017, 18, 2005–2010. [Google Scholar]
- World Health Organisation. Global Status Report on Non-Communicable Diseases. 2014. Available online: http://www.who.int/nmh/publications/ncd-status-report-2014/en/ (accessed on 11 January 2018).
- Rawal, L.B.; Biswas, T.; Khandker, N.N.; Saha, S.R.; Bidat Chowdhury, M.M.; Khan, A.N.S.; Hasib Chowdhury, E.; Renzaho, A. Non-communicable disease (NCD) risk factors and diabetes among adults living in slum areas of Dhaka, Bangladesh. PLoS ONE 2017, 12, e0184967. [Google Scholar]
- World Health Organization Regional office for Eastern Mediterranean Cairo Egypt. Country Cooperation Strategy for Saudi Arabia 2006–2011. Available online: http://www.who.int/countryfocus/cooperation_strategy/ccs_sau_en.pdf.EM/ARD/014/E/R (accessed on 13 September 2020).
- Saudi Vision (2030). National Transformation Program: Strategic objectives. Available online: https://vision2030.gov.sa/sites/default/files/attachments/NTP%20English%20Public%20Document_2810.pdf (accessed on 30 March 2019).
- GBD Compare. World Bank 2018, Saudi Arabia; Population Reference Bureau: Washington, DC, USA, 2018. [Google Scholar]
- Memish, Z.A.; El Bcheraoui, C.; Tuffaha, M.; Robinson, M.; Daoud, F.; Jaber, S. Obesity and Associated Factors Kingdom of Saudi Arabia. Prev. Chronic Dis. 2014, 11, 140236. [Google Scholar]
- Memish, Z.A.; Jaber, S.; Mokdad, A.H.; AlMazroa, M.A.; Murray, C.J.L.; Al Rabeeah, A.A. Burden of Disease, Injuries, and Risk Factors in the Kingdom of Saudi Arabia, 1990–2010. Prev. Chronic. Dis. 2014, 11, 140176. [Google Scholar]
- Pan American Health Organization. NCDs at a Glance: NCD Mortality and Risk Factor Prevalence in the Americas; Paho: Washington, DC, USA, 2019. [Google Scholar]
- Liu, K.; Yang, J.; Zou, H. Cultural heterogeneity, social policy, and economic growth in China. China Econ. Review. 2020, 62, 101501. [Google Scholar] [CrossRef]
- Abebe, S.M.; Andargie, G.; Shimeka, A.; Alemu, K.; Kebede, Y.; Wubeshet, M.; Tariku, A.; Gebeyehu, A.; Bayisa, M.; Yitayal, M.; et al. The prevalence of non-communicable diseases in Northwest Ethiopia: Survey of Dabat health and demographic surveillance system. BMJ Open 2017, 7, e015496. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, G.; Wu, H.; Jian, W.; Wild, S.H.; Gasevic, D. Sex differences in non-communicable disease prevalence in China: A cross-sectional analysis of the China health and retirement longitudinal study in 2011. BMJ Open 2017, 7, e017450. [Google Scholar] [CrossRef]
- Melingheri, M.; Paladino, M.E.; Piacenti, S.; Riva, M.A. Effects of COVID-19 lockdown on epidemic diseases of childhood. J. Med. Virol. 2020, 93, 153–154. [Google Scholar] [CrossRef]
- Deputy Director for Public Health Science and Surveillance, Center for Surveillance, Epidemiology, and Laboratory Services, Division of Scientific Education and Professional Development (2012). Available online: https://www.cdc.gov/ddphss/index.html (accessed on 22 May 2020).
- David, M.M.; Fauci, A.S. Emerging Infectious Diseases: Threats to Human Health and Global Stability. PLoS Pathog. 2013, 9, e1003467. [Google Scholar] [CrossRef] [Green Version]
- Van Boheemen, S.; de Graaf, M.; Lauber, C.; Bestebroer, T.M.; Raj, V.S.; Zaki, A.M.; Osterhaus, A.D.; Haagmans, B.L.; Gorbalenya, A.E.; Snijder, E.J.; et al. Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. mBio 2012, 3, e00473-12. [Google Scholar] [CrossRef] [Green Version]
- Sahal, N.; Reintjes, R.; Eltayeb, E.M.; Aro, A.R. Assessment of core activities and supportive functions for the communicable diseases surveillance system in Khartoum state, Sudan, 2005–2007. East Mediterr. Health J. 2010, 16, 1204–1210. [Google Scholar]
- Boehmer, T.K.; Patnaik, J.L.; Burnite, S.J.; Ghosh, T.S.; Gershman, K.; Vogt, R.L. Use of Hospital Discharge Data to Evaluate Notifiable Disease Reporting to Colorado’s Electronic Disease Reporting System. Public Health Rep. 2011, 126, 100–106. [Google Scholar]
- Kebede, S.; Gatabazi, J.B.; Rugimbanya, P.; Mukankwiro, T.; Perry, H.N.; Alemu, W.; Ndihokubwayo, B.J.; Kramer, H.M.; Mukabayire, O. Strengthening systems for communicable disease surveillance: Creating a laboratory network in Rwanda. Health Res. Policy Syst. 2011, 9, 1–8. [Google Scholar]
- Wang, K.; Xiang, L.; Kang, L.; Miao, L.; Li, Q.; Li, X.; Jun Zhu, J.; Wang, Y.; Huang, Y.; He, C. Communicable disease mortality trends and characteristics of infants in rural China, 1996–2015. BMC Public Health 2020, 20, 455. [Google Scholar] [CrossRef]
- World Health Organization. Newborns: Improving Survival and Well-Being. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortaliy (accessed on 19 September 2020).
- Masquelier, B.; Hug, L.; Sharrow, D. Global, regional and national mortality trends in older children and young adolescents (5–14 years) from 1990 to 2016: An analysis of empirical data. Lancet Glob. Health 2018, 6, e1087–e1099. [Google Scholar]
- Saudi Ministry of Health. Guidelines on the Date of Death as it’s Continuously Updated on the National and International Basis; Saudi Ministry of Health: Riyadh, Saudi Arabia, 2020.
- Baud, D.; Qi, X.; Nielsen-Saines, K.; Musso, D.; Pomar, L.; Favre, G. Real estimates of mortality following COVID-19 infection. Lancet Infect. Dis. 2020, 20, 773. Available online: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30195-X/abstract (accessed on 27 March 2020).
- Quick Interim Guide to COVID-19 Surveillance Case Definitions and Disposition. Available online: https//covid19.cdc.gov.sa (accessed on 18 October 2020).
- Jin, J.M.; Bai, P.; He, W.; Liu, S.; Wu, F.; Liu, X.F.; Han, D.M.; Liu, S.; Yang, J.K. Gender Differences in Patients with COVID-19: Focus on Severity and Mortality. Front. Public Health 2020, 8, 152. [Google Scholar] [CrossRef]
- Ng, J.; Bakrania, K.; Russell, R.; Falkous, R. Why Is the Disease Killing More Men than Women? COVID-19 Mortality Rates by Age and Gender. 2020. Available online: https//www.rgare.com/docs/defaultsource/knowledge-center-articles/covid-19_mortality_age_gender.pdf?sfvrsn=5806a7ea_4/ (accessed on 3 July 2020).
- Bellan, M.; Gavelli, F.; Hayden, E.; Patrucco, F.; Soddu, D.; Pedrinelli, A.R.; Cittone, M.G.; Rizzi, E.; Casciaro, G.F.; Vassia, V.; et al. Pattern of emergency department referral during the COVID-19 outbreak in Italy. Panminerva Med. 2020. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Ioannidis, J.P.A.; Axfors, C.; Contopoulos-Ioannidis, D.G. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicentres. Environ. Res. 2020, 188, 109890. [Google Scholar]
- Guilmoto, C.Z. COVID-19 Death Rates by Age and Sex and the Resulting Mortality Vulnerability of Countries and Regions in the World. 2020. Available online: https://www.medrxiv.org/content/10.1101/2020.05.17.20097410v1.full.pdf (accessed on 9 July 2020).
- Boretti, A. COVID-19 fatality rate for Saudi Arabia, updated 3 June 2020. J. Glob. Antimicrob. Resist. 2020, 22, 845–846. [Google Scholar] [CrossRef]
- World Health Organization. Health Profile of Saudi Arabia. 2015. Available online: http://apps.who.int/iris/handle/10665/253771 (accessed on 28 December 2020).
- World Health Organization. Global Status Report on Road Safety 2013; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Available online. Available online: https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html (accessed on 3 November 2020).
- Mansuri, F.A.; Al-Zalabani, A.H.; Zalat, M.M.; Qabshawi, R.I. Road safety and road traffic accidents in Saudi Arabia. Saudi Med. J. 2015, 36, 418–424. [Google Scholar] [CrossRef]
- Al-Naami, M.Y.; Arafah, M.A.; Al-Ibrahim, F.S. Trauma care systems in Saudi Arabia: An agenda for action. Ann. Saudi Med. 2010, 30, 50–58. [Google Scholar]
- Roy, D.; Tripathy, S.; Kar, S.K.; Sharma, N.; Verma, S.K.; Kaushal, V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian populatio during COVID-19 pandemic. Asian J. Psychiatry 2020, 51, 102083. [Google Scholar]
- Khan, Z.U.; Al Asiri, K.M.; Iqbal, J. Injury patterns from road traffic accidents. Pak. J. Med Sci. 2010, 26, 394–397. [Google Scholar]
- Center of Disease Control (CDC). New ICD Code Introduced for COVID-19 Deaths. Available online: https://www.cdc.gov/nchs/data/nvss/coronavirus/Alert-2-New-ICD-code-introduced-for-COVID-19-deaths.pdf (accessed on 9 July 2010).
- World Meter. COVID-19 Coronavirus Pandemic. 2020. Available online: https://www.worldometers.info/coronavirus/ (accessed on 4 July 2020).
- Lipsitch, M.; Swerdlow, D.L.; Finelli, L. Defining the Epidemiology of COVID-19—Studies Needed. N. Engl. J. Med. 2020, 382, 1194–1196. [Google Scholar]
- Our World in Data. 2020. Available online: covid.ourworldindata.org/data/owid-covid-data.csv (accessed on 3 June 2020).
- Global Burden of Disease. Study Published. 2010. Available online: https://www.who.int/pmnch/media/news/2012/who_burdenofdisease/en/ (accessed on 29 April 2020).
| Diseases and Injury Categories and ICD-10 Codes | Underlying Causes F (%) | F % |
|---|---|---|
| I-Communicable diseases (CDs), maternal, and neonatal conditions | ||
| A-Infectious, parasitic diseases | 2438 (8.3) | 5141 (17.6) |
| B-Acute Respiratory Infections | 864 (2.9) | |
| C-Maternal Conditions | 177 (0.6) | |
| D-Neonatal Causes | 351 (1.2) | |
| E-Nutritional deficiencies | 13 (0.0) | |
| 1298 (4.4) | |
| II-Non Communicable diseases (NCDs) | ||
| F-Malignant + other neoplasms | 1199 (4.1) | 11,862 (40.5) |
| G-Diabetes Mellitus | 658 (2.2) | |
| H-Endocrine and metabolic disorders | 232 (0.8) | |
| I-Mental disorders | 38 (0.1) | |
| J-Nervous System, Sense organ disorders | 640 (2.2) | |
| K-Cardiovascular Diseases (CVD) | 6864 (23.4) | |
| L-Chronic Respiratory diseases | 1153 (3.9) | |
| M-Diseases of the digestive system + Oral health | 255 (0.9) | |
| N-Genitourinary diseases | 483 (1.6) | |
| O-Skin diseases | 29 (0.1) | |
| P-Musculoskeletal disease | 96 (0.3) | |
| Q-Congenital anomalies | 189 (0.6) | |
| R-Ill -defined conditions | 26 (0.1) | |
| III-Injuries | ||
| S-Unintentional injuries T = 2773 (9.4) | 10,213 (34.9) | |
| 994 (3.4) | |
| 184 (0.6) | |
| 1421 (4.9) | |
| T-Intentional injuries | ||
| 174 (0.6) | ||
| U-Codes allocated or redistributed to other codes | ||
| T = 3071 (10.5) | ||
| 146 (0.5) | |
| 48 (0.2) | |
| 22 (0.1) | |
| 2768 (9.5) | |
| 87 (0.3) | |
| Ill-defined conditions; T = 4369 (14.9%) | ||
| 192 (0.7) | |
| 399 (1.4) | |
| 114 (0.4) | |
| 469 (1.6) | |
| 253 (0.9) | |
| 1083 (3.7) | |
| 949 (3.2) | |
| 471 (1.6) | |
| 439 (1.6) | |
| IV-Codes of special Conditions | ||
| 15 (0.1) | 473 (1.6) |
| 390 (1.3) | |
| 51 (0.2) | |
| 17 (0.1) | |
| V-Factors that influence the health status | 117 (0.4) | 117 (0.4) |
| Null | 1485 (5.0) | 1485 (5.0) |
| Total | 29,291 | 100.0 |
| WHO Classification of Main Causes of Deaths | The First Half of 2020 Underlying Causes of Mortality F(%) |
|---|---|
| Communicable, maternal, perinatal, and nutritional conditions | 5546 (18.9) |
| (including SARS, and COVID-19 confirmed cases by special codes) | |
| Diabetes Mellitus | 658 (2.2) |
| Chronic Respiratory diseases | 1053 (3.9) |
| Cardio-vascular diseases | |
| {ICD-10, heart Failure-ill-defined and unspecific Cardiovascular conditions+ heart failure + abnormal heart rhythm+ abnormal blood pressure} | 10,103 (34.5) |
| Cancer | |
| (Malignant+ other neoplasm + Ill-defined malignant neoplasm + Unspecified uterine cancer) | 1345 (4.6) |
| Other Non-communicable diseases (NCDs) | 2181 (7.4) |
| Injuries | |
| 1866 (6.4) |
| 994 (3.4) | |
| T = 2860 (9.8%) | |
| Ill-defined injury conditions /unknown/risk factors | 4060 (13.9) |
| Null | 1485 (5.0) |
| No of deaths | 29,291 |
| Total no of the population (1440 h, 2019 G) | 34,218,168 |
| Age Groups (y) | Total Number (f) | Proportional Mortality (%) | NCDs Mortality F (%) | NCDs-Age Specific ASMR * | CDs ** Mortality F (%) | CDs-ASMR * | COVID-19 Mortality F (%) | COVID-19 ASMR * |
|---|---|---|---|---|---|---|---|---|
| Abortion | ------ | -------- | ----- | |||||
| 47 | 0.2 | 0 | 0 (0.0) | 0 (0.0) | |||
| 236 | 0.8 | 23 (0.1) | 3 (0.1) | 0 (0.0) | |||
| 1 m | 645 | 2.2 | 314 (2.0) | 744 26.4 | 101 (3.04) | 236 8.4 | 1 (0.1) | 3 0.01 |
| 1 m–12 m | 225 | 0.9 | 69 (0.4) | 14 (0.4) | ---- | |||
| 1–4 | 776 | 2.6 | 361 (2.3) | 121 (3.6) | 2 (0.1) | |||
| 5–9 | 225 | 0.8 | 115 (0.7) | 3.8 | 19 (8.4) | 0.64 | 0 | --- |
| 10–14 | 227 | 0.8 | 97 (0.6) | 3.7 | 21 (0.6) | 0.8 | 0 | ---- |
| 15–19 | 514 | 1.8 | 163 (1.1) | 6.9 | 34 (1.0) | 1.4 | 3 (0.2) | 0.13 |
| 20–24 | 850 | 2.9 | 216 (1.4) | 8.2 | 49 (1.5) | 1.9 | 9 (0.5) | 0.34 |
| 25–29 | 1049 | 3.6 | 343 (2.2) | 10.5 | 75 (2.3) | 2.3 | 20 (1.2) | 0.61 |
| 30–34 | 1107 | 3.8 | 424 (2.7) | 12.9 | 78 (2.4) | 2.4 | 49 (2.9) | 1.48 |
| 35–39 | 1119 | 3.8 | 481 (3.1) | 12.97 | 82 (2.5) | 2.2 | 84 (4.9) | 2.27 |
| 40–44 | 1361 | 4.6 | 666 (4.3) | 20.1 | 96 (2.9) | 2.9 | 146 (8.6) | 4.49 |
| 45–49 | 1504 | 5.1 | 723 (4.7) | 29.3 | 131 (3.9) | 5.3 | 150 (8.8) | 6.9 |
| 50–54 | 2019 | 6.9 | 1067 (6.9) | 62.23 | 173 (5.2) | 10.1 | 245 (14.5) | 14.28 |
| 55–59 | 2177 | 7.4 | 1195 (7.7) | 100.9 | 210 (6.3) | 17.7 | 209 (12.4) | 17.66 |
| 60–64 | 2689 | 9.2 | 1505 (9.8) | 193.2 | 286 (8.6) | 36.7 | 229 (13.6) | 29.39 |
| 65–69 | 2222 | 7.6 | 1296 (8.3) | 298.7 | 254 (7.7) | 58.6 | 177 (10.5) | 40.87 |
| 70–74 | 2225 | 7.6 | 1364 (8.8) | 473.5 | 292 (8.8) | 101.4 | 108 (6.4) | 37.5 |
| 75–79 | 2375 | 8.1 | 1451 (9.4) | 839.5 | 353 (10.6) | 204.2 | 103 (6.1) | 59.6 |
| 80–84 | 2148 | 7.3 | 1338 (8.7) | 3267 1597.7 | 333 (10.04) | 1104 529.5 | 69 (4.1) | 153 74.8 |
| 85–89 | 1692 | 5.8 | 1033 (6.6) | 267 (8.0) | 48 (2.8) | |||
| 90–94 | 1054 | 3.6 | 629 (4.1) | 176 (5.3) | 25 (1.5) | |||
| 95–99 | 447 | 1.5 | 77 (0.4) | 273 (8.2) | 8 (0.5) | |||
| 100–104 | 208 | 0.7 | 128 (0.8) | 35 (1.1) | 2 (0.1) | |||
| 105–109 | 82 | 0.3 | 41 (0.3) | 16 (0.5) | 1 (0.1) | |||
| 110 or more | 38 | 0.1 | 21 (0.1) | 4 (0.1) | ---- | |||
| Total | 29,291 | 100.0 | 15,430 | 3317 | 1688 |
| Health Province | No of Deaths | Proportional Mortality (PM) | Province Specific MR% * 10,000 | NCDs Proportional Mortality F (%) | NCDs-Province Specific MR * 10,000 | RTTA Proportional Mortality F (%) | RTTA Region-Specific MR * 100,000 |
|---|---|---|---|---|---|---|---|
| Makkah | 4270 | 14.6 | 17.4 | 1936 (12.6) | 8.2 | 92 (9.3) | 3.7 |
| Riyadh | 5271 | 18.0 | 6.1 | 2021 (13.2) | 5.5 | 232 (23.3) | 2.7 |
| Jeddah | 3616 | 12.3 | 7.3 | 2620 (17.1) | 5.3 | 78 (7.8) | 1.6 |
| Al Madinah-Al Monawarah | 2355 | 8.0 | 10.5 | 976 (6.4) | 4.3 | 57 (5.7) | 2.5 |
| Aseer | 1856 | 6.2 | 9.76 | 1010 (6.6) | 5.3 | 74 (7.4) | 3.9 |
| Jazan | 2151 | 7.3 | 13.1 | 1257 (8.8) | 7.6 | 57 (5.7) | 3.4 |
| Al-Qassem | 1280 | 4.4 | 8.6 | 573 (3.7) | 3.9 | 18 (1.8) | 1.2 |
| Al Taif | 1290 | 4.4 | 9.48 | 683 (4.5) | 5.2 | 44 (4.4) | 3.3 |
| Eastern Region | 1760 | 6.0 | 5.17 | 896 (5.8) | 2.6 | 66 (6.6) | 1.9 |
| Tabouk | 714 | 2.4 | 7.5 | 314 (2.0) | 3.3 | 52 (5.2) | 5.4 |
| Hail | 673 | 2.3 | 9.2 | --- | 65 (6.5) | 8.8 | |
| Al-Qunfudah | 386 | 1.3 | 11.9 | 270 (1.8) | 8.3 | 10 (1.0) | 3.1 |
| Najran | 552 | 1.9 | 9.07 | 308 (2.0) | 9.1 | 30 (3.0) | 4.9 |
| Al-Jouf | 471 | 1.6 | 13.3 | 317 (1.8) | 8.9 | 4 (0.4) | 1.1 |
| Al-Ahsa | 784 | 2.7 | 6.1 | 553 (70.5) | 4.3 | 27 (2.7) | 2.1 |
| Al-Bahaa | 486 | 1.7 | 9.8 | 309 (2.0) | 6.2 | 2 (0.2) | 0.4 |
| Bisha | 399 | 1.4 | 9.8 | 290 (1.9) | 7.1 | 6 (0.6) | 1.5 |
| Northern Border | 435 | 1.5 | 11.3 | 270 (1.8) | 7.0 | 6 (0.6) | 1.6 |
| Hafr -Al Baten | 385 | 1.3 | 8.2 | 224 (1.5) | 4.7 | 24 (2.4) | 5.1 |
| Al-Qurayyat | 157 | 0.5 | 8.8 | 92 (0.6) | 5.2 | 10 (1.0 | 5.6 |
| Sex-Specific Mortality Rate (MR) * 100,000 | Proportional NCDs Mortality Per Sex F (%) | NCDs Sex-Specific MR(SSMR) * 100,000 | CDs Proportional MR Per Sex | CDs SSMR * 100,000 | Proportional COVID-19 Mortality Per Sex F(%) | COVID-19 SSMR * 100,000 | |
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Males (19,212) | 97.9 | 9424 (49.1) | 47.7 | 1899 (9.8) | 9.8 | 1361 (7.1) | 6.9 |
| Females(10,079) | 95.8 | 5916 (58.7) | 40.8 | 1418 (14.1) | 100.1 | 327 (3.2) | 2.5 |
| Sex | Nationality | |||
|---|---|---|---|---|
| Males N = 19,212 F (%) | Females N = 10,079 F (%) | Saudi N = 18,110 F (%) | Non-Saudi N= 11,181 F (%) | |
| Null (N = 1485) | 938 (4.9) | 547 (5.4) | 793 (4.4) | 692 (6.2) |
| RTTA (N = 994) | 867 (4.5) | 127 (1.3) | 640 (3.5) | 354 (3.2) |
| CDs ***(N = 3317) | 1899 (9.9) | 1418 (14.0) | 2409 (13.3) | 908 (8.1)) |
| NCDs (N = 15,340) | 9424 (49.1) | 5916 (58.7) | 10,394 (57.4) | 4946 (44.2) |
| COVID-19 (N = 1688) | 1361 (7.1) | 327 (3.2) | 463 (2.6) | 1225 (11.0) |
| Other causes ** | 4723 (24.7) | 1744 (17.3) | 3411 (18.8) | 3056 (27.3) |
| p | 0.01 * | 0.00 * | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asiri, A.M.; Alomary, S.A.; Alqahtani, S.A.; Adam, I.F.; Amer, S.A. Determinants of the Underlying Causes of Mortality during the First Wave of COVID-19 Pandemic in Saudi Arabia: A Descriptive National Study. Int. J. Environ. Res. Public Health 2021, 18, 12647. https://doi.org/10.3390/ijerph182312647
Asiri AM, Alomary SA, Alqahtani SA, Adam IF, Amer SA. Determinants of the Underlying Causes of Mortality during the First Wave of COVID-19 Pandemic in Saudi Arabia: A Descriptive National Study. International Journal of Environmental Research and Public Health. 2021; 18(23):12647. https://doi.org/10.3390/ijerph182312647
Chicago/Turabian StyleAsiri, Abdullah M., Shaker A. Alomary, Saeed A. Alqahtani, Izzeldin F. Adam, and Samar A. Amer. 2021. "Determinants of the Underlying Causes of Mortality during the First Wave of COVID-19 Pandemic in Saudi Arabia: A Descriptive National Study" International Journal of Environmental Research and Public Health 18, no. 23: 12647. https://doi.org/10.3390/ijerph182312647
APA StyleAsiri, A. M., Alomary, S. A., Alqahtani, S. A., Adam, I. F., & Amer, S. A. (2021). Determinants of the Underlying Causes of Mortality during the First Wave of COVID-19 Pandemic in Saudi Arabia: A Descriptive National Study. International Journal of Environmental Research and Public Health, 18(23), 12647. https://doi.org/10.3390/ijerph182312647







