The Role of Health Literacy in Health Behavior, Health Service Use, Health Outcomes, and Empowerment in Pediatric Patients with Chronic Disease: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
- pubmed
- CINAHL
- PsycINFO
- Scopus
2.2. Eligibility Criteria
2.3. Study Selection, Data Extraction and Analysis
2.4. Quality Assessment
3. Results
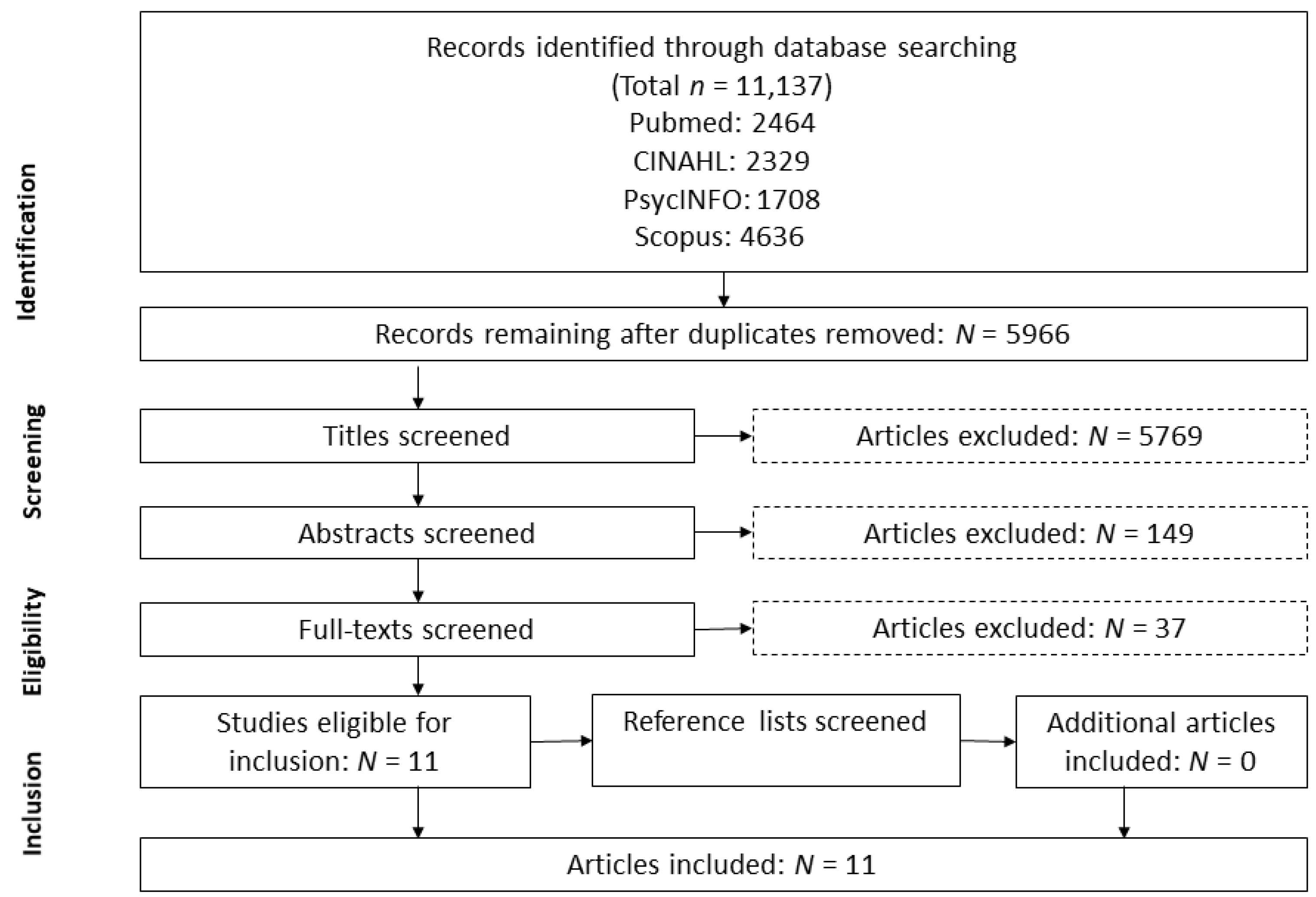
3.1. Literature Search
3.2. Study Characteristics
3.3. Study Quality
3.4. Health Literacy Measures
3.5. Health Literacy and Health Behavior, Health Service Use, Health Outcomes, and Empowerment
4. Discussion
4.1. Health Literacy and Health Behavior
4.2. Health Literacy and Health Service Use
4.3. Health Literacy and Health Outcomes
4.4. Health Literacy and Empowerment
4.5. Study Quality and Instruments Measuring Health Literacy
4.6. Strengths and Limitations
5. Conclusions
Implications for Research and Practice
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Author | Publication Year | Country | Study Design | Sample Size | Median Age of Participants (Range) | Health Issues | Health Literature Measure | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Beukema et al. [50] | 2019 | Netherlands | Prospective cohort study | 390 | 15 (12–18) | Psychosocial/mental diseases | 3-item HL Screening questions | Adherence Learning process (improved understanding) Confidence Psychosocial outcomes (SDQ) |
| Dore-Stites et al. [51] | 2019 | USA | Cross-sectional study | Total: 79 Subgroup: 20 | Total: N/A (N/A) Subgroup: N/A (13–18) | Liver transplant recipients | TOFHLA Newest vital sign | Adherence (tacrolimus blood level) Liver function (AST, ALT, TBili) |
| Jackson et al. [52] | 2019 | Ireland | Retrospective cohort study | 251 | 21.38 (13–30) | Cystic fibrosis | HLS-EU-Q16 | HRQoL (CFQr) BMI, ppFEV1, P. aeruginosa Days of iv/oral antibiotics Outpatient visits Days hospitalized |
| Levine et al. [53] | 2018 | USA | Retrospective cohort study | 49 | N/A (12–18) | Chronic kidney diseases, SLE, kidney transplant, dialysis | Newest vital sign | ED visits Preventable hospitalizations Total hospitalizations Total inpatient days |
| Manegold et al. [54] | 2019 | USA | Cross-sectional study | 65 | 15.03 (13–17) | Diabetes mellitus type 1 | TOFHLA-R | Transition readiness (TRAQ) Glycemic control (Hba1c) |
| Murphy et al. [55] | 2010 | USA | Longitudinal cohort study | 186 | 20.5 (16–24) | HIV | TOFHLA STOFHLA | Viral load, CD4 cells Self-efficacy for adherence to HIV medication regimes/keeping of medical appointments Medical care received (diabetic self-care practice instrument (adopted for HIV+ patients) and Module 1 of the Pediatric Adherence Questionnaire and Self-efficacy for health promotion and risk reduction) ED visits Overnight hospital stays |
| Navarra et al. [56] | 2014 | USA | Cross-sectional study | 50 | 19.7 (13–24) | HIV | TOFHLA REALM-Teen | Adherence to ART (BAMS) |
| Sharif et al. [57] | 2011 | USA | Cross-sectional study | 78 | 11.5 (10–16) | Obesity | STOFHLA | BMI Eating self-efficacy (ESES Questionnaire) |
| Valerio et al. [58] | 2016 | USA | Cross-sectional study | 181 | N/A (15–19) | Asthma | 3-item HL screening questions | HLQoL (MiniPAQLQ) Asthma management: medication use Morbidity (EPRII guidelines) Hospitalization |
| Valerio et al. [59] | 2018 | USA | Cross-sectional study | 327 | 15.8 (13–18) | Asthma | REALM-Teen | Asthma self efficacy Morbidity (symptom days, symptom bother) |
| Zhong et al. [60] | 2020 | USA | Cross-sectional study | Total: 59 Subgroup: 21 | Total: N/A (12–29) Subgroup: N/A (12–18) | Chronic kidney disease, hypertension | Newest vital sign | HCT readiness (STARx Questionnaire) Self-management |
| Criterion | Beukema et al. (2019) | Dore-Stites et al. (2019) | Jackson et al. (2019) | Levine et al. (2018) | Manegold et al. (2019) | Murphy et al. (2010) | Navarra et al. (2014) | Sharif et al. (2011) | Valerio et al. (2016) | Valerio et al. (2018) | Zhong et al. (2020) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Reporting | |||||||||||
| 1: Hypothesis/aim/objective clearly described | 1 | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 1 | 1 |
| 2: Main outcomes in introduction or methods | 1 | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 1 | 1 |
| 3: Patient characteristics clearly described | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 4: Interventions of interest clearly described | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 5: Principal confounders clearly described | 2 | 0 | 0 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 2 |
| 6: Main findings clearly described | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 1 | 1 | 0.5 | 1 |
| 7: Estimates of random variability provided for main outcomes | 1 | 1 | 1 | 0 | 1 | 0.5 | 1 | 1 | 1 | 0.5 | 1 |
| 8: All adverse events of intervention reported | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9: Characteristics of patients lost to follow-up described | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 10: Probability values reported for main outcomes | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| External validity | |||||||||||
| 11: Subjects asked to participate were representative of source population | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0.5 | 0 |
| 12: Subjects prepared to participate were representative of source population | 1 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0 | 0.5 | 1 | 0 | 0.5 |
| 13: Location and delivery of study treatment was representative of source population | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Internal validity—bias and confounding | |||||||||||
| 14: Study participants blinded to treatment | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15: Blinded outcome assessment | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 16: Any data dredging clearly described | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 17: Analyses adjust for differing lengths of follow-up | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 18: Appropriate statistical tests performed | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 19: Compliance with interventions was reliable | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 20: Outcome measures were reliable and valid | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 21: All participants recruited from the same source population | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 22: All participants recruited over the same period | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 23: Participants randomized to treatment(s) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 24: Allocation of treatment concealed from investigators and participants | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 25: Adequate adjustment for confounding | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 |
| 26: Losses to follow-up taken into account | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Power | |||||||||||
| 27: Sufficient power to detect treatment effect at significance | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 17 | 9.5 | 11.5 | 9.5 | 9 | 12 | 12 | 12.5 | 11 | 8.5 | 12.5 |
| Outcome | Regarded in n Studies | Positive Correlation | Reported Estimate | 95% CI | p |
|---|---|---|---|---|---|
| Health behavior | 7 | ||||
| Adherence | 4 | Beukema et al. | 0.43 (β coefficient) | −0.27, 1.14 | 0.23 |
| Dore-Stites et al. | N/A | N/A | N/A | ||
Murphy et al.
| 1.00 (odds ratio) 1.00 (odds ratio) | (0.96–1.05) (0.95–1.04) | 0.98 | ||
Navarra et al.
| −0.011 (correlation coefficient) −0.122 (correlation coefficient) | N/A N/A | 0.94 0.40 | ||
| Self-management/care | 3 | Beukema et al.
| 0.37 (β coefficient) | −0.15, 0.90 | 0.16 |
Valerio et al., 2016
| 1.12 (odds ratio) 1.33 (odds ratio) | 0.53, 2.34 0.64, 2.80 | 0.774 0.447 | ||
Zhong et al.
| N/A | N/A | 0.05 | ||
| Health service use | 4 | ||||
| ED visits/hospitalization/hospital stays | 4 | Jackson et al.
| −0.06 (correlation coefficient) −0.08 (correlation coefficient) | −0.18–0.07 −0.2–0.05 | 0.432 0.329 |
Levine et al.
| N/A | N/A | N/A | ||
Murphy et al.
| 0.98 (odds ratio) 0.97 (odds ratio) | 0.96–1.01 0.93–1.01 | 0.28 0.14 | ||
Valerio et al., 2016
| 1.37 (odds ratio) | 1.11, 1.69 | 0.003 | ||
| Medical care received | 1 | Murphy et al.
| 1.09 (odds ratio) 1.06 (odds ratio) | 1.04–1.15 1.02–1.09 | 0.0002 |
| Health outcomes | 8 | ||||
| Physiological parameters/clinical characteristics | 5 | Dore-Stites et al.
| N/A | N/A | N/A |
Jackson et al.
| −0.02 (correlation coefficient) 0.03 (correlation coefficient) −0.03 (correlation coefficient) −0.08 (correlation coefficient) −0.08 (correlation coefficient) −0.21 (correlation coefficient) −0.23 (correlation coefficient) | −0.14–0.11 −0.09–0.15 −0.16–0.09 −0.2–0.05 −0.21–0.04 −0.33–−0.09 −0.34–−0.11 | 0.763 0.649 0.649 0.329 0.295 0.004 0.004 | ||
Manegold et al.
| −0.05 (correlation coefficient) | N/A | 0.43 | ||
Murphy et al.
| N/A N/A | N/A N/A | 0.15 0.13 | ||
Sharif et al.
| −0.016 (correlation coefficient) −0.43 (β coefficient) | −0.025, −0.008 | <0.0001 | ||
| Morbidity | 3 | Beukema et al.
| −1.70 (β coefficient) | −2.72, −0.69 | 0.001 |
Valerio et al., 2016
| 1.35 (odds ratio) | 0.67, 2.71 | 0.404 | ||
Valerio et al., 2018
| 0.95 (β coefficient) 0.23 (β coefficient) | 0.005, 1.89 −0.09, 0.55 | 0.05 0.16 | ||
| HRQoL | 2 | Jackson et al. | 0.23 (correlation coefficient) | 0.11–0.35 | 0.004 |
| Valerio et al., 2016 | 0.75 (odds ratio) | 0.59, 0.95 | 0.016 | ||
| Empowerment | 5 | ||||
| Self-efficacy | 3 | Murphy et al.
| 0.99 (odds ratio) 1.01 (odds ratio) | 0.95–1.03 0.95–1.06 | 0.55 0.85 |
| Sharif et al. | −0.45 | N/A | <0.0001 | ||
| Valerio et al., 2018 | 1.28 (β coefficient) | 0.23, 2.32 | 0.02 | ||
| Transition readiness | 2 | Manegold et al. | −0.10 (correlation coefficient) | 0.50 | |
Zhong et al.
| N/A | N/A | 0.001 |
References
- Hagen, C.V.; Schwarz, H.P. Psychische Entwicklung bei chronischer Krankheit im Kindes- und Jugendalter, 1st ed.; Kohlhammer Verlag: Stuttgart, Germany, 2009; ISBN 9783170204133. [Google Scholar]
- Perrin, J.M.; Anderson, L.E.; van Cleave, J. The rise in chronic conditions among infants, children, and youth can be met with continued health system innovations. Health Aff. 2014, 33, 2099–2105. [Google Scholar] [CrossRef]
- Newacheck, P.W.; Budetti, P.P.; McManus, P. Trends in childhood disability. Am. J. Public Health 1984, 74, 232–236. [Google Scholar] [CrossRef]
- Torpy, J.M.; Campbell, A.; Glass, R.M. JAMA patient page. Chronic diseases of children. JAMA 2010, 303, 682. [Google Scholar] [CrossRef]
- Bethell, C.D.; Read, D.; Blumberg, S.J.; Newacheck, P.W. What is the prevalence of children with special health care needs? Toward an understanding of variations in findings and methods across three national surveys. Matern. Child Health J. 2008, 12, 1–14. [Google Scholar] [CrossRef]
- Gledhill, J.; Rangel, L.; Garralda, E. Surviving chronic physical illness: Psychosocial outcome in adult life. Arch. Dis. Child. 2000, 83, 104–110. [Google Scholar] [CrossRef]
- Perrin, J.M.; Bloom, S.R.; Gortmaker, S.L. The increase of childhood chronic conditions in the United States. JAMA 2007, 297, 2755–2759. [Google Scholar] [CrossRef]
- Hwu, Y.J. The impact of chronic illness on patients. Rehabil. Nurs. 1995, 20, 221–225. [Google Scholar] [CrossRef]
- Turkel, S.; Pao, M. Late consequences of chronic pediatric illness. Psychiatr. Clin. N. Am. 2007, 30, 819–835. [Google Scholar] [CrossRef] [PubMed]
- Simmons, R.G. At the Threshold: The Developing Adolescent, 7th ed.; Feldman, S.S., Elliott, G.R., Eds.; Harvard University Press: Cambridge, UK, 2001; ISBN 0674050355. [Google Scholar]
- Secinti, E.; Thompson, E.J.; Richards, M.; Gaysina, D. Research Review: Childhood chronic physical illness and adult emotional health—A systematic review and meta-analysis. J. Child Psychol. Psychiatry 2017, 58, 753–769. [Google Scholar] [CrossRef] [PubMed]
- Hoff, A.L.; Mullins, L.L.; Chaney, J.M.; Hartman, V.L.; Domek, D. Illness uncertainty, perceived control, and psychological distress among adolescents with type 1 diabetes. Res. Theory Nurs. Pract. 2002, 16, 223–236. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M. Wenn Kinder und Jugendliche Körperlich Chronisch Krank Sind: Psychische und soziale Entwicklung, Prävention, Intervention; Springer: Berlin/Heidelberg, Germany, 2012; ISBN 9783642312779. [Google Scholar]
- Bai, G.; Herten, M.H.-V.; Landgraf, J.M.; Korfage, I.J.; Raat, H. Childhood chronic conditions and health-related quality of life: Findings from a large population-based study. PLoS ONE 2017, 12, e0178539. [Google Scholar] [CrossRef]
- Ingerski, L.M.; Modi, A.C.; Hood, K.K.; Pai, A.L.; Zeller, M.; Piazza-Waggoner, C.; Driscoll, K.A.; Rothenberg, M.E.; Franciosi, J.; Hommel, K.A. Health-related quality of life across pediatric chronic conditions. J. Pediatr. 2010, 156, 639–644. [Google Scholar] [CrossRef]
- Boice, M.M. Chronic illness in adolescence. Adolescence 1998, 33, 927–939. [Google Scholar] [PubMed]
- Smith, F.J.; Taylor, K.M.G.; Newbould, J.; Keady, S. Medicines for chronic illness at school: Experiences and concerns of young people and their parents. J. Clin. Pharm. Ther. 2008, 33, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Blum, R.W.; Garell, D.; Hodgman, C.H.; Jorissen, T.W.; Okinow, N.A.; Orr, D.P.; Slap, G.B. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. J. Adolesc. Health 1993, 14, 570–576. [Google Scholar] [CrossRef]
- Baker, D.W.; Parker, R.M.; Williams, M.V.; Pitkin, K.; Parikh, N.S.; Coates, W.; Imara, M. The health care experience of patients with low literacy. Arch. Fam. Med. 1996, 5, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Health literacy: Report of the Council on Scientific Affairs. JAMA 1999, 281, 552–557. [Google Scholar] [CrossRef]
- Baur, C.; Harris, L.; Squire, E. The U.S. National Action Plan to Improve Health Literacy: A Model for Positive Organizational Change. Stud. Health Technol. Inform. 2017, 240, 186–202. [Google Scholar] [PubMed]
- Sørensen, K.; van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Rothman, R.L.; Yin, H.S.; Mulvaney, S.; Co, J.P.T.; Homer, C.; Lannon, C. Health literacy and quality: Focus on chronic illness care and patient safety. Pediatrics 2009, 124, S315–S326. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Chesser, A.K.; Keene Woods, N.; Smothers, K.; Rogers, N. Health Literacy and Older Adults: A Systematic Review. Gerontol. Geriatr. Med. 2016, 2, 2333721416630492. [Google Scholar] [CrossRef]
- Miller, T.A. Health literacy and adherence to medical treatment in chronic and acute illness: A meta-analysis. Patient Educ. Couns. 2016, 99, 1079–1086. [Google Scholar] [CrossRef]
- Mackey, L.M.; Doody, C.; Werner, E.L.; Fullen, B. Self-Management Skills in Chronic Disease Management: What Role Does Health Literacy Have? Med. Decis. Mak. 2016, 36, 741–759. [Google Scholar] [CrossRef] [PubMed]
- Papadakos, J.K.; Hasan, S.M.; Barnsley, J.; Berta, W.; Fazelzad, R.; Papadakos, C.J.; Giuliani, M.E.; Howell, D. Health literacy and cancer self-management behaviors: A scoping review. Cancer 2018, 124, 4202–4210. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.M.; Fraser, S.; Dudley, C.; Oniscu, G.C.; Tomson, C.; Ravanan, R.; Roderick, P. Health literacy and patient outcomes in chronic kidney disease: A systematic review. Nephrol. Dial. Transplant. 2018, 33, 1545–1558. [Google Scholar] [CrossRef] [PubMed]
- Manganello, J.A. Health literacy and adolescents: A framework and agenda for future research. Health Educ. Res. 2008, 23, 840–847. [Google Scholar] [CrossRef]
- Martin, A.J.; Steinbeck, K. The role of puberty in students’ academic motivation and achievement. Learn. Individ. Differ. 2017, 53, 37–46. [Google Scholar] [CrossRef]
- Weiss, B.D.; Palmer, R. Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. J. Am. Board Fam. Pract. 2004, 17, 44–47. [Google Scholar] [CrossRef]
- Baker, D.W.; Parker, R.M.; Williams, M.V.; Clark, W.S.; Nurss, J. The relationship of patient reading ability to self-reported health and use of health services. Am. J. Public Health 1997, 1027–1030. [Google Scholar] [CrossRef]
- Baker, D.W.; Gazmararian, J.A.; Williams, M.V.; Scott, T.; Parker, R.M.; Green, D.; Ren, J.; Peel, J. Health literacy and use of outpatient physician services by Medicare managed care enrollees. J. Gen. Intern. Med. 2004, 19, 215–220. [Google Scholar] [CrossRef]
- Schaeffer, D.; Berens, E.-M.; Vogt, D. Health literacy in the German population—Results of a representative survey. Dtsch. Arztebl. Int. 2017, 114, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Gazmararian, J.A.; Curran, J.W.; Parker, R.M.; Bernhardt, J.M.; deBuono, B.A. Public health literacy in America: An ethical imperative. Am. J. Prev. Med. 2005, 28, 317–322. [Google Scholar] [CrossRef]
- Sogie-Thomas, B. Understanding Health Literacy: Implications for Medicine and Public Health. J. Natl. Med. Assoc. 2006, 98, 980–981. [Google Scholar]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Holland, A.; Brasure, M.; Lohr, K.N.; Harden, E.; et al. Health literacy interventions and outcomes: An updated systematic review. Evid. Rep. Technol. Assess. 2011, 199, 1–941. [Google Scholar]
- DeWalt, D.A.; Hink, A. Health literacy and child health outcomes: A systematic review of the literature. Pediatrics 2009, 124, S265–S274. [Google Scholar] [CrossRef] [PubMed]
- Sanders, L.M.; Thompson, V.T.; Wilkinson, J.D. Caregiver health literacy and the use of child health services. Pediatrics 2007, 119, e86–e92. [Google Scholar] [CrossRef] [PubMed]
- Stanton, W.R.; Feehan, M.; McGee, R.; Silva, P.A. The relative value of reading ability and IQ as predictors of teacher-reported behavior problems. J. Learn. Disabil. 1990, 23, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Hassan, K.; Heptulla, R.A. Glycemic control in pediatric type 1 diabetes: Role of caregiver literacy. Pediatrics 2010, 125, e1104–e1108. [Google Scholar] [CrossRef] [PubMed]
- Pulgarón, E.R.; Sanders, L.M.; Patiño-Fernandez, A.M.; Wile, D.; Sanchez, J.; Rothman, R.L.; Delamater, A.M. Glycemic control in young children with diabetes: The role of parental health literacy. Patient Educ. Couns. 2014, 94, 67–70. [Google Scholar] [CrossRef] [PubMed]
- DeWalt, D.A.; Dilling, M.H.; Rosenthal, M.S.; Pignone, M.P. Low parental literacy is associated with worse asthma care measures in children. Ambul. Pediatr. 2007, 7, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Stormacq, C.; Wosinski, J.; Boillat, E.; van den Broucke, S. Effects of health literacy interventions on health-related outcomes in socioeconomically disadvantaged adults living in the community: A systematic review. JBI Evid. Synth. 2020, 18, 1389–1469. [Google Scholar] [CrossRef]
- Pignone, M.; DeWalt, D.A.; Sheridan, S.; Berkman, N.; Lohr, K.N. Interventions to improve health outcomes for patients with low literacy. A systematic review. J. Gen. Intern. Med. 2005, 20, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Visscher, B.B.; Steunenberg, B.; Heijmans, M.; Hofstede, J.M.; Devillé, W.; van der Heide, I.; Rademakers, J. Evidence on the effectiveness of health literacy interventions in the EU: A systematic review. BMC Public Health 2018, 18, 1414. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Beukema, L.; Reijneveld, S.A.; Jager, M.; Metselaar, J.; de Winter, A.F. The role of functional health literacy in long-term treatment outcomes in psychosocial care for adolescents. Eur. Child Adolesc. Psychiatry 2020, 29, 1547–1554. [Google Scholar] [CrossRef]
- Dore-Stites, D.; Lopez, M.J.; Magee, J.C.; Bucuvalas, J.; Campbell, K.; Shieck, V.; Well, A.; Fredericks, E.M. Health literacy and its association with adherence in pediatric liver transplant recipients and their parents. Pediatr. Transplant. 2020, 24, e13726. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.D.; Kirwan, L.; Gibney, S.; Jeleniewska, P.; Fletcher, G.; Doyle, G. Associations between health literacy and patient outcomes in adolescents and young adults with cystic fibrosis. Eur. J. Public Health 2020, 30, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.; Javalkar, K.; Nazareth, M.; Faldowski, R.A.; Ferris, M.D.-G.d.; Cohen, S.; Cuttance, J.; Hooper, S.R.; Rak, E. Disparities in Health Literacy and Healthcare Utilization among Adolescents and Young Adults with Chronic or End-stage Kidney Disease. J. Pediatr. Nurs. 2018, 38, 57–61. [Google Scholar] [CrossRef]
- Manegold, E.M. Health Literacy and Family Factors in the Transition to Adult Care in Adolescents with Type 1 Diabetes. Ph.D. Thesis, West Virginia University, Morgantown, WV, USA, 2020. [Google Scholar]
- Murphy, D.A.; Lam, P.; Naar-King, S.; Robert Harris, D.; Parsons, J.T.; Muenz, L.R. Health literacy and antiretroviral adherence among HIV-infected adolescents. Patient Educ. Couns. 2010, 79, 25–29. [Google Scholar] [CrossRef][Green Version]
- Navarra, A.-M.; Neu, N.; Toussi, S.; Nelson, J.; Larson, E.L. Health literacy and adherence to antiretroviral therapy among HIV-infected youth. J. Assoc. Nurses AIDS Care 2014, 25, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Sharif, I.; Blank, A.E. Relationship between child health literacy and body mass index in overweight children. Patient Educ. Couns. 2010, 79, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Valerio, M.A.; Peterson, E.L.; Wittich, A.R.; Joseph, C.L.M. Examining health literacy among urban African-American adolescents with asthma. J. Asthma 2016, 53, 1041–1047. [Google Scholar] [CrossRef]
- Valerio, M.A.; George, M.; Liu, J.; Osakwe, Z.T.; Bruzzese, J.-M. Health literacy and asthma among Hispanic and African-American urban adolescents with undiagnosed asthma. Ann. Allergy Asthma Immunol. 2018, 121, 499–500. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.; Patel, N.; Ferris, M.; Rak, E. Health literacy, nutrition knowledge, and health care transition readiness in youth with chronic kidney disease or hypertension: A cross-sectional study. J. Child Health Care 2020, 24, 246–259. [Google Scholar] [CrossRef] [PubMed]
- Chisolm, D.J.; Buchanan, L. Measuring adolescent functional health literacy: A pilot validation of the Test of Functional Health Literacy in Adults. J. Adolesc. Health 2007, 41, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.W.; Williams, M.V.; Parker, R.M.; Gazmararian, J.A.; Nurss, J. Development of a brief test to measure functional health literacy. Patient Educ. Couns. 1999, 38, 33–42. [Google Scholar] [CrossRef]
- Weiss, B.D.; Mays, M.Z.; Martz, W.; Castro, K.M.; DeWalt, D.A.; Pignone, M.P.; Mockbee, J.; Hale, F.A. Quick assessment of literacy in primary care: The newest vital sign. Ann. Fam. Med. 2005, 3, 514–522. [Google Scholar] [CrossRef]
- Chew, L.D.; Griffin, J.M.; Partin, M.R.; Noorbaloochi, S.; Grill, J.P.; Snyder, A.; Bradley, K.A.; Nugent, S.M.; Baines, A.D.; Vanryn, M. Validation of screening questions for limited health literacy in a large VA outpatient population. J. Gen. Intern. Med. 2008, 23, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.C.; Michielutte, R.; Askov, E.N.; Williams, M.V.; Weiss, B.D. Practical assessment of adult literacy in health care. Health Educ. Behav. 1998, 25, 613–624. [Google Scholar] [CrossRef] [PubMed]
- Quittner, A.L.; Buu, A.; Messer, M.A.; Modi, A.C.; Watrous, M. Development and validation of The Cystic Fibrosis Questionnaire in the United States: A health-related quality-of-life measure for cystic fibrosis. Chest 2005, 128, 2347–2354. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.C.; Wolf, M.S.; Arnold, C.L.; Byrd, R.S.; Long, S.W.; Springer, T.; Kennen, E.; Bocchini, J.A. Development and validation of the Rapid Estimate of Adolescent Literacy in Medicine (REALM-Teen): A tool to screen adolescents for below-grade reading in health care settings. Pediatrics 2006, 118, e1707–e1714. [Google Scholar] [CrossRef] [PubMed]
- Wallston, K.A.; Cawthon, C.; McNaughton, C.D.; Rothman, R.L.; Osborn, C.Y.; Kripalani, S. Psychometric properties of the brief health literacy screen in clinical practice. J. Gen. Intern. Med. 2014, 29, 119–126. [Google Scholar] [CrossRef]
- Cavanaugh, K.L.; Osborn, C.Y.; Tentori, F.; Rothman, R.L.; Ikizler, T.A.; Wallston, K.A. Performance of a brief survey to assess health literacy in patients receiving hemodialysis. Clin. Kidney J. 2015, 8, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Sansom-Daly, U.M.; Peate, M.; Wakefield, C.E.; Bryant, R.A.; Cohn, R.J. A systematic review of psychological interventions for adolescents and young adults living with chronic illness. Health Psychol. 2012, 31, 380–393. [Google Scholar] [CrossRef] [PubMed]
- Ostini, R.; Kairuz, T. Investigating the association between health literacy and non-adherence. Int. J. Clin. Pharm. 2014, 36, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.; Murphy, F.; Keeley, H.S. All of us? An exploration of the concept of mental health literacy based on young people’s responses to fictional mental health vignettes. Ir. J. Psychol. Med. 2015, 32, 129–136. [Google Scholar] [CrossRef]
- Epstein, R.M.; Street, R.L. The values and value of patient-centered care. Ann. Fam. Med. 2011, 9, 100–103. [Google Scholar] [CrossRef]
- Harrington, K.F.; Zhang, B.; Magruder, T.; Bailey, W.C.; Gerald, L.B. The Impact of Parent’s Health Literacy on Pediatric Asthma Outcomes. Pediatr. Allergy Immunol. Pulmonol. 2015, 28, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Michou, M.; Panagiotakos, D.B.; Costarelli, V. Low health literacy and excess body weight: A systematic review. Cent. Eur. J. Public Health 2018, 26, 234–241. [Google Scholar] [CrossRef]
- Naigaga, M.D.; Guttersrud, O.; Pettersen, K.S. Measuring maternal health literacy in adolescents attending antenatal care in a developing country—The impact of selected demographic characteristics. J. Clin. Nurs. 2015, 24, 2402–2409. [Google Scholar] [CrossRef]
- Zheng, M.; Jin, H.; Shi, N.; Duan, C.; Wang, D.; Yu, X.; Li, X. The relationship between health literacy and quality of life: A systematic review and meta-analysis. Health Qual. Life Outcomes 2018, 16, 201. [Google Scholar] [CrossRef]
- Okan, O.; Lopes, E.; Bollweg, T.M.; Bröder, J.; Messer, M.; Bruland, D.; Bond, E.; Carvalho, G.S.; Sørensen, K.; Saboga-Nunes, L.; et al. Generic health literacy measurement instruments for children and adolescents: A systematic review of the literature. BMC Public Health 2018, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Armstrong, R.; Waters, E.; Sathish, T.; Alif, S.M.; Browne, G.R.; Yu, X. Quality of health literacy instruments used in children and adolescents: A systematic review. BMJ Open 2018, 8, e020080. [Google Scholar] [CrossRef] [PubMed]
- Parker, R.M.; Baker, D.W.; Williams, M.V.; Nurss, J.R. The test of functional health literacy in adults: A new instrument for measuring patients‘ literacy skills. J. Gen. Intern. Med. 1995, 10, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Bröder, J.; Okan, O.; Bauer, U.; Bruland, D.; Schlupp, S.; Bollweg, T.M.; Saboga-Nunes, L.; Bond, E.; Sørensen, K.; Bitzer, E.-M.; et al. Erratum to: Health literacy in childhood and youth: A systematic review of definitions and models. BMC Public Health 2017, 17, 419. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, S.L.; Halpern, D.J.; Viera, A.J.; Berkman, N.D.; Donahue, K.E.; Crotty, K. Interventions for individuals with low health literacy: A systematic review. J. Health Commun. 2011, 16, 30–54. [Google Scholar] [CrossRef]
- Neuhauser, H.; Poethko-Müller, C. Chronische Erkrankungen und impfpräventable Infektionserkrankungen bei Kindern und Jugendlichen in Deutschland: Ergebnisse der KiGGS-Studie—Erste Folgebefragung (KiGGS Welle 1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2014, 57, 779–788. [Google Scholar] [CrossRef]
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Population |
|
|
| Focus/outcomes |
|
|
| Study design |
|
|
| Language |
|
|
| Author | Publication Year | Country | Study Design | Sample Size | Median Age of Participants (Range) | Health Issues |
|---|---|---|---|---|---|---|
| Beukema et al. [50] | 2019 | Netherlands | Prospective cohort study | 390 | 15 (12–18) | Psychosocial/mental diseases |
| Dore-Stites et al. [51] | 2019 | USA | Cross-sectional study | Total: 79 Subgroup: 20 | Total: N/A (N/A) Subgroup: N/A (13–18) | Liver transplant recipients |
| Jackson et al. [52] | 2019 | Ireland | Retrospective cohort study | 251 | 21.38 (13–30) | Cystic fibrosis |
| Levine et al. [53] | 2018 | USA | Retrospective cohort study | 49 | N/A (12–18) | Chronic kidney diseases, SLE, kidney transplant, dialysis |
| Manegold et al. [54] | 2019 | USA | Cross-sectional study | 65 | 15.03 (13–17) | Diabetes mellitus type 1 |
| Murphy et al. [55] | 2010 | USA | Longitudinal cohort study | 186 | 20.5 (16–24) | HIV |
| Navarra et al. [56] | 2014 | USA | Cross-sectional study | 50 | 19.7 (13–24) | HIV |
| Sharif et al. [57] | 2011 | USA | Cross-sectional study | 78 | 11.5 (10–16) | Obesity |
| Valerio et al. [58] | 2016 | USA | Cross-sectional study | 181 | N/A (15–19) | Asthma |
| Valerio et al. [59] | 2018 | USA | Cross-sectional study | 327 | 15.8 (13–18) | Asthma |
| Zhong et al. [60] | 2020 | USA | Cross-sectional study | Total: 59 Subgroup: 21 | Total: N/A (12–29) Subgroup: N/A (12–18) | Chronic kidney disease, hypertension |
| Criterion | Beukema et al. (2019) | Dore-Stites et al. (2019) | Jackson et al. (2019) | Levine et al. (2018) | Manegold et al. (2019) | Murphy et al. (2010) | Navarra et al. (2014) | Sharif et al. (2011) | Valerio et al. (2016) | Valerio et al. (2018) | Zhong et al. (2020) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 17 | 9.5 | 11.5 | 9.5 | 9 | 12 | 12 | 12.5 | 11 | 8.5 | 12.5 |
| Outcome | Regarded in n Studies | Study | Negative Correlation | Positive Correlation (p) |
|---|---|---|---|---|
| Health behavior | 7 | |||
| Adherence | 4 | Beukema et al. | No | Yes (0.23) |
| Dore-Stites et al. | N/A | N/A | ||
| Murphy et al. | No | Yes (0.98) | ||
Navarra et al.
| No No | Yes (0.94) Yes (0.40) | ||
| Self-management/care | 3 | Beukema et al. | No | Yes (0.16) |
Valerio et al., 2016
| No No | Yes (0.774) Yes (0.447) | ||
| Zhong et al. | No | Yes (0.05) | ||
| Health service use | 4 | |||
| Emergency department (ED) visits/hospitalization/hospital stays | 4 | Jackson et al.
| No No | Yes (0.432) Yes (0.329) |
| Levine et al. | N/A | N/A | ||
Murphy et al.
| No No | Yes (0.28) Yes (0.14) | ||
| Valerio et al., 2016 | No | Yes (0.003) | ||
| Medical care received | 1 | Murphy et al. | No | Yes (0.0002) |
| Health outcomes | 8 | |||
| Physiological parameters/clinical characteristics | 5 | Dore-Stites et al. | N/A | N/A |
Jackson et al.
| No No No No No No No | Yes (0.763) Yes (0.649) Yes ((0.649 Yes (0.329 Yes (0.295) Yes (0.004) Yes (0.004) | ||
Manegold et al.
| No | Yes (0.43) | ||
Murphy et al.
| No No | Yes (0.15) Yes (0.13) | ||
| Sharif et al. | No | Yes (<0.0001) | ||
| Morbidity | 3 | Beukema et al. | No | Yes (0.001) |
| Valerio et al., 2016 | No | Yes (0.404) | ||
Valerio et al., 2018
| No No | Yes (0.05) Yes (0.16) | ||
| HRQoL | 2 | Jackson et al. | No | Yes (0.004) |
| Valerio et al., 2016 | No | Yes (0.016) | ||
| Empowerment | 5 | |||
| Self-efficacy | 3 | Murphy et al.
| No No | Yes (0.55) Yes (0.85) |
| Sharif et al. | No | Yes (<0.0001) | ||
| Valerio et al., 2018 | No | Yes (0.02) | ||
| Transition readiness | 2 | Manegold et al. | No | Yes (0.50) |
| Zhong et al. | No | Yes (0.001) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riemann, L.; Lubasch, J.S.; Heep, A.; Ansmann, L. The Role of Health Literacy in Health Behavior, Health Service Use, Health Outcomes, and Empowerment in Pediatric Patients with Chronic Disease: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12464. https://doi.org/10.3390/ijerph182312464
Riemann L, Lubasch JS, Heep A, Ansmann L. The Role of Health Literacy in Health Behavior, Health Service Use, Health Outcomes, and Empowerment in Pediatric Patients with Chronic Disease: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(23):12464. https://doi.org/10.3390/ijerph182312464
Chicago/Turabian StyleRiemann, Lisa, Johanna Sophie Lubasch, Axel Heep, and Lena Ansmann. 2021. "The Role of Health Literacy in Health Behavior, Health Service Use, Health Outcomes, and Empowerment in Pediatric Patients with Chronic Disease: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 23: 12464. https://doi.org/10.3390/ijerph182312464
APA StyleRiemann, L., Lubasch, J. S., Heep, A., & Ansmann, L. (2021). The Role of Health Literacy in Health Behavior, Health Service Use, Health Outcomes, and Empowerment in Pediatric Patients with Chronic Disease: A Systematic Review. International Journal of Environmental Research and Public Health, 18(23), 12464. https://doi.org/10.3390/ijerph182312464






