Placement of Posterior Composite Restorations: A Cross-Sectional Study of Dental Practitioners in Al-Kharj, Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Questionnaire Description
2.3. Sampling and Data Collection
2.4. Statistical Analysis
3. Results
3.1. Response Rate
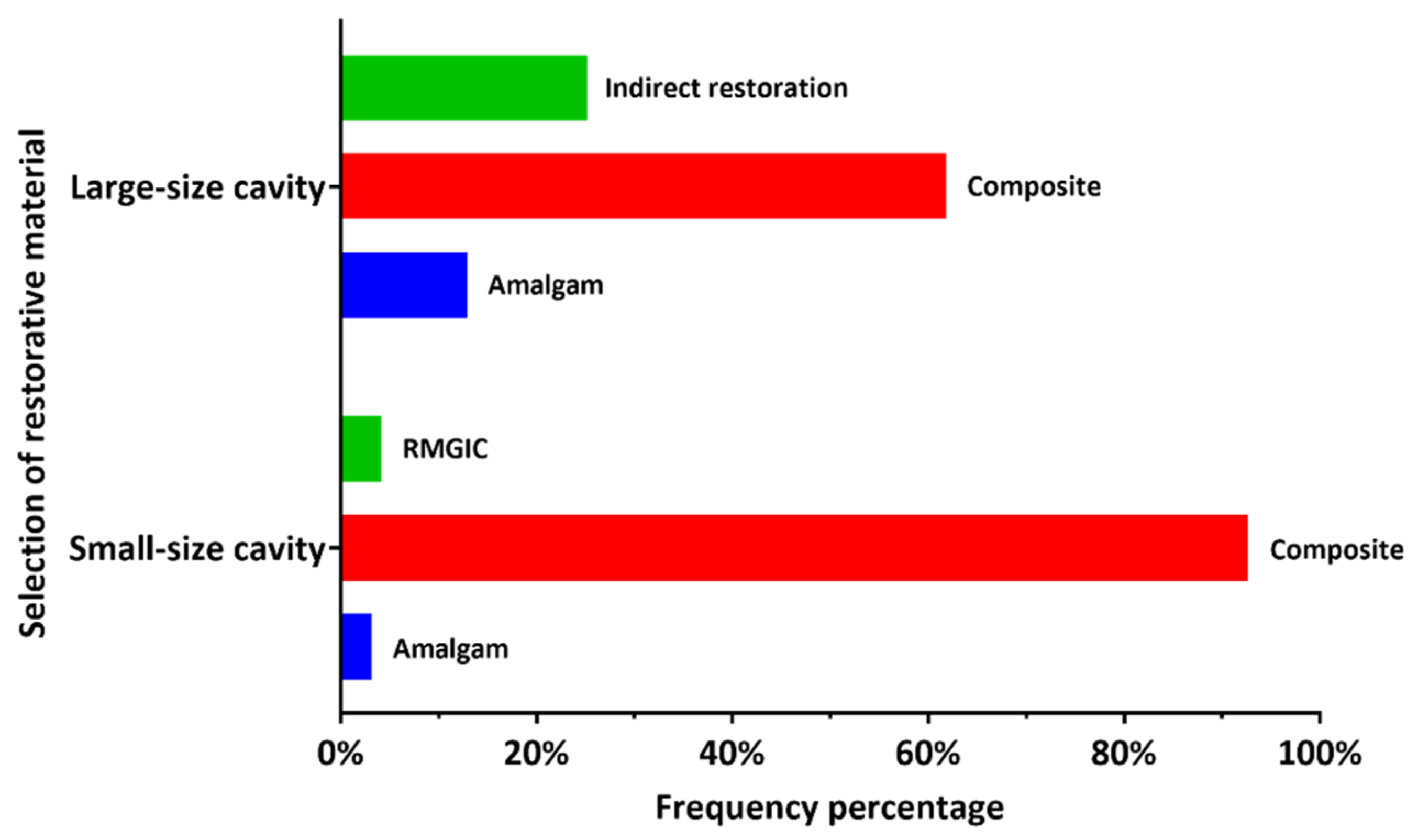
3.2. Selection of the Restorative Material
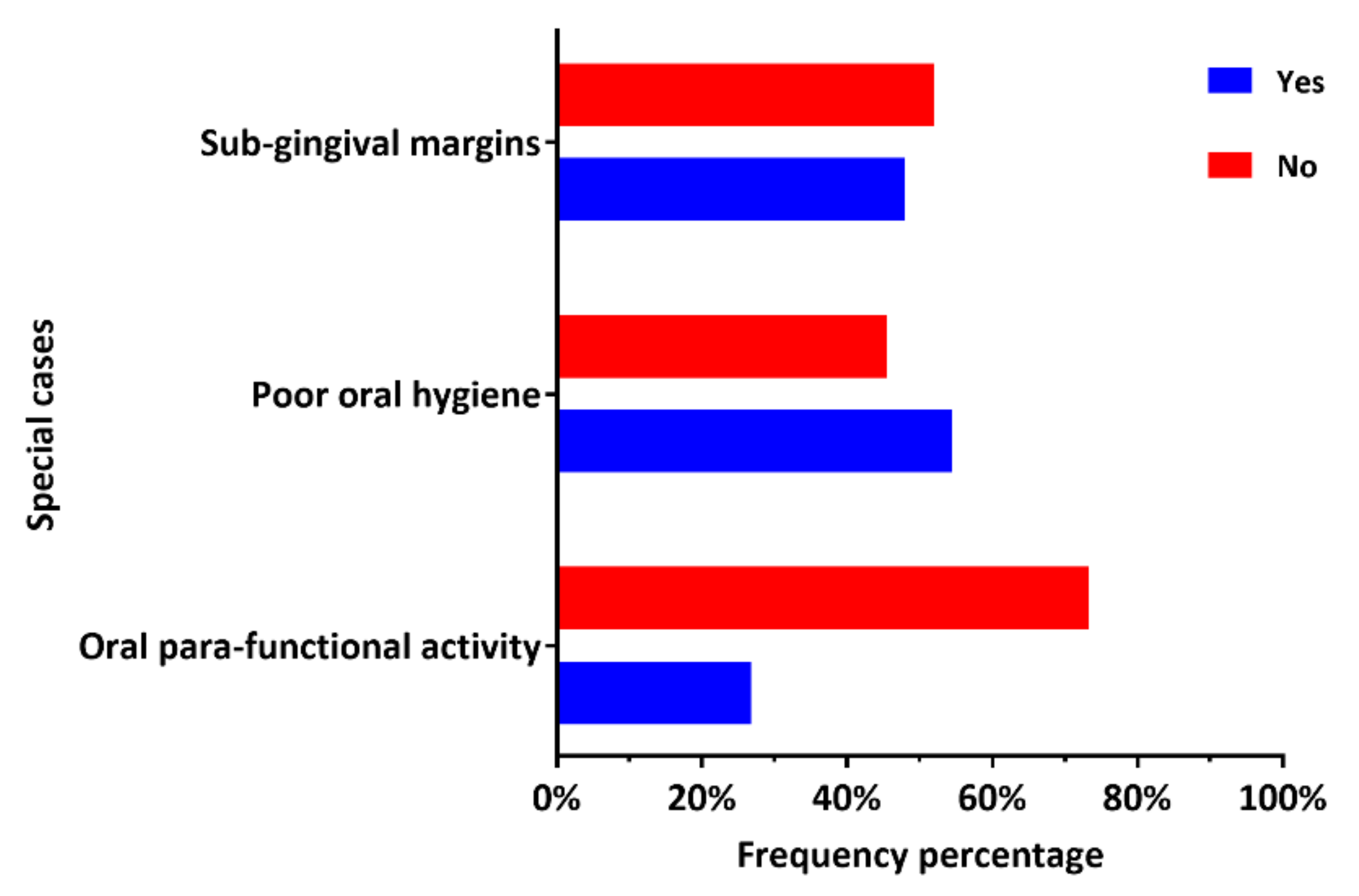
3.3. Placement of Posterior Composite Restorations in Patients with Certain Clinical Conditions
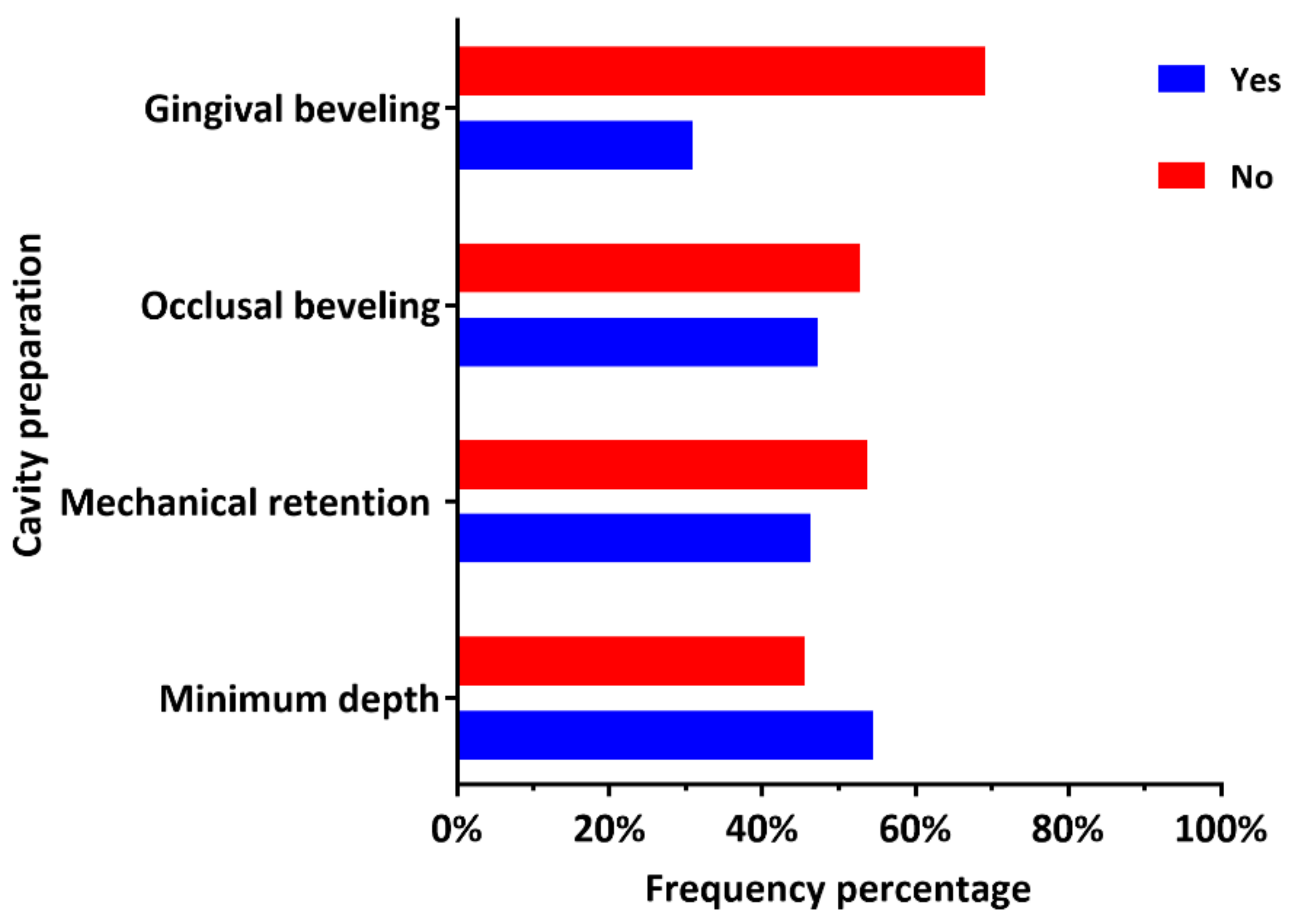
3.4. Specifications of the Cavity Preparation
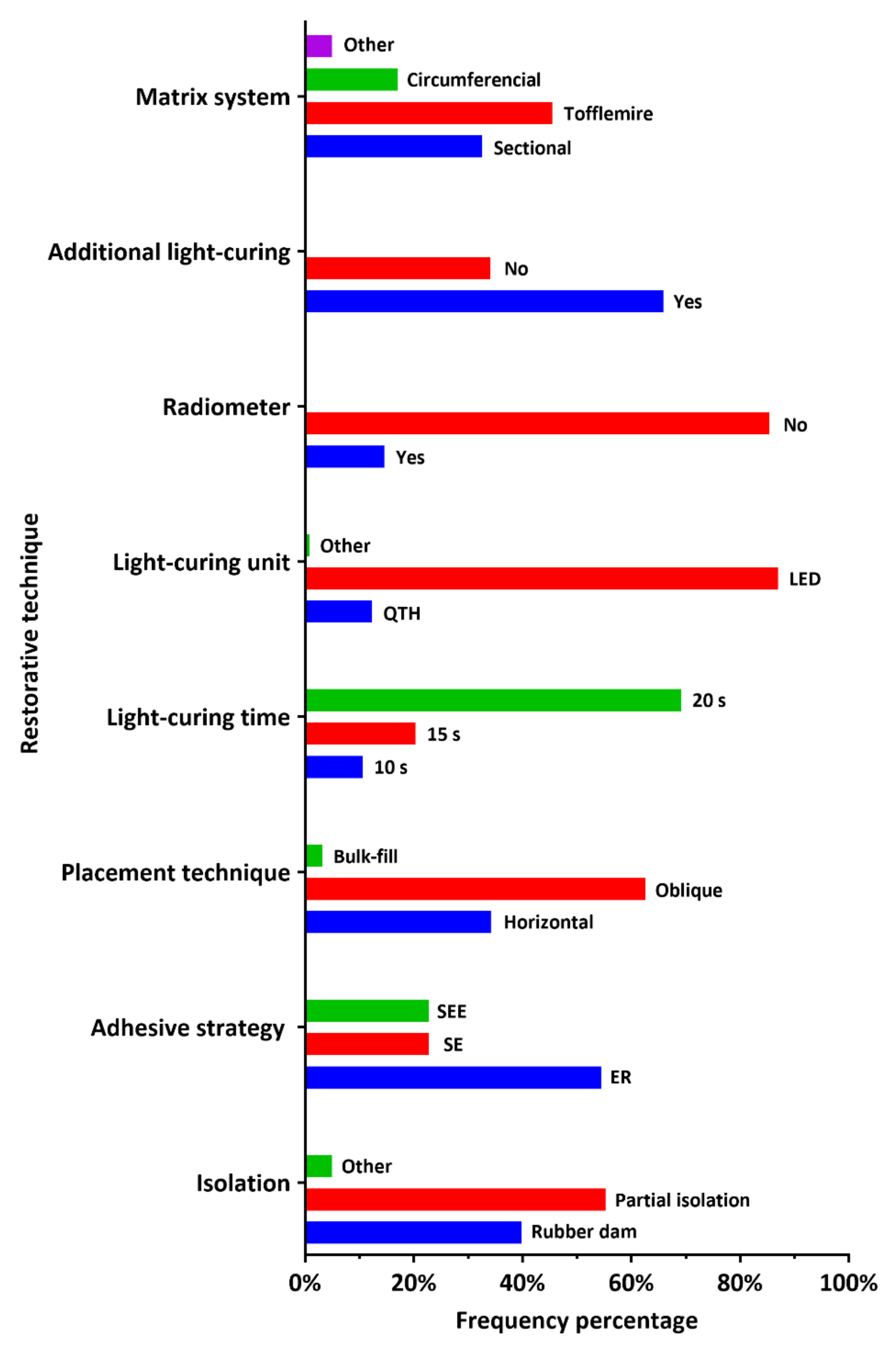
3.5. Restorative Technique
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burke, F.J.; Mackenzie, L.; Sands, P. Dental materials—What goes where? Class I and II cavities. Dent. Update 2013, 40, 260–274. [Google Scholar] [CrossRef] [PubMed]
- Sunnegardh-Gronberg, K.; van Dijken, J.W.; Funegard, U.; Lindberg, A.; Nilsson, M. Selection of dental materials and longevity of replaced restorations in Public Dental Health clinics in northern Sweden. J. Dent. 2009, 37, 673–678. [Google Scholar] [CrossRef]
- Fuks, A. The use of amalgam in pediatric dentistry. Pediatr. Dent. 2001, 24, 448–455. [Google Scholar]
- Khalaf, M.E.; Alomari, Q.D.; Omar, R. Factors relating to usage patterns of amalgam and resin composite for posterior restorations—A prospective analysis. J. Dent. 2014, 42, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Ritter, A.V. Posterior composites revisited. J. Esthet. Restor. Dent. 2008, 20, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Roeters, J.J.; Shortall, A.C.; Opdam, N.J. Can a single composite resin serve all purposes? Br. Dent. J. 2005, 199, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Gilmour, A.S.; Latif, M.; Addy, L.D.; Lynch, C.D. Placement of posterior composite restorations in United Kingdom dental practices: Techniques, problems, and attitudes. Int. Dent. J. 2009, 59, 148–154. [Google Scholar] [PubMed]
- Lynch, C.D.; Opdam, N.J.; Hickel, R.; Brunton, P.A.; Gurgan, S.; Kakaboura, A.; Shearer, A.C.; Vanherle, G.; Wilson, N.H.; Academy of Operative Dentistry European Section. Guidance on posterior resin composites: Academy of Operative Dentistry—European Section. J. Dent. 2014, 42, 377–383. [Google Scholar] [CrossRef]
- Watts, D.C.; el Mowafy, O.M.; Grant, A.A. Fracture resistance of lower molars with Class 1 composite and amalgam restorations. Dent. Mater. 1987, 3, 261–264. [Google Scholar] [CrossRef]
- Lynch, C.D.; McConnell, R.J. The cracked tooth syndrome. J. Can. Dent. Assoc. 2002, 68, 470–475. [Google Scholar]
- Pink, F.E.; Minden, N.J.; Simmonds, S. Decisions of practitioners regarding placement of amalgam and composite restorations in general practice settings. Oper. Dent. 1994, 19, 127–132. [Google Scholar]
- Friedl, K.H.; Hiller, K.A.; Schmalz, G. Placement and replacement of composite restorations in Germany. Oper. Dent. 1995, 20, 34–38. [Google Scholar]
- Mjor, I.A.; Dahl, J.E.; Moorhead, J.E. Age of restorations at replacement in permanent teeth in general dental practice. Acta Odontol. Scand. 2000, 58, 97–101. [Google Scholar] [CrossRef]
- Forss, H.; Widstrom, E. Reasons for restorative therapy and the longevity of restorations in adults. Acta Odontol. Scand. 2004, 62, 82–86. [Google Scholar] [CrossRef]
- Hayashi, M.; Seow, L.L.; Lynch, C.D.; Wilson, N.H. Teaching of posterior composites in dental schools in Japan. J. Oral. Rehabil. 2009, 36, 292–298. [Google Scholar] [CrossRef]
- Opdam, N.J.; Bronkhorst, E.M.; Roeters, J.M.; Loomans, B.A. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent. Mater. 2007, 23, 2–8. [Google Scholar] [CrossRef]
- Opdam, N.J.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Gaengler, P.; Lindberg, A.; Huysmans, M.C.; van Dijken, J.W. Longevity of posterior composite restorations: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef]
- Sabbagh, J.; McConnell, R.J.; McConnell, M.C. Posterior composites: Update on cavities and filling techniques. J. Dent. 2017, 57, 86–90. [Google Scholar] [CrossRef]
- Demarco, F.F.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef]
- Lucarotti, P.S.; Holder, R.L.; Burke, F.J. Outcome of direct restorations placed within the general dental services in England and Wales (Part 3): Variation by dentist factors. J. Dent. 2005, 33, 827–835. [Google Scholar] [CrossRef]
- Burke, F.J.; McHugh, S.; Randall, R.C.; Meyers, I.A.; Pitt, J.; Hall, A.C. Direct restorative materials use in Australia in 2002. Aust. Dent. J. 2004, 49, 185–191. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Akbar, I. Knowledge and attitudes of general dental practitioners towards posterior composite restorations in Northern Saudi Arabia. J. Clin. Diagn. Res. 2015, 9, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F. Attitudes of dentists and interns in Riyadh to the use of dental amalgam. BMC. Res. Notes 2016, 9, 488. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, J.M.; Murray, C.M.; Schwass, D.R.; Brosnan, M.; Brunton, P.A.; Lyons, K.S.; Thomson, W.M. The Dental Amalgam Phasedown in New Zealand: A 20-year Trend. Oper. Dent. 2020, 45, 255–264. [Google Scholar] [CrossRef]
- Bailey, O.; Vernazza, C.R.; Stone, S.; Ternent, L.; Roche, A.G.; Lynch, C. Amalgam Phase-Down Part 1: UK-Based Posterior Restorative Material and Technique Use. JDR Clin. Trans. Res. 2020, in press. [Google Scholar] [CrossRef]
- STROBE Statement Guidelines. Available online: https://www.strobe-statement.org/download/strobe-checklist-cohort-case-control-and-cross-sectional-studies-combined (accessed on 30 April 2021).
- Geisen, E.; Romano Bergstrom, J. Chapter 6—Think aloud and verbal-probing techniques. In Usability Testing for Survey Research; Geisen, E., Romano Bergstrom, J., Eds.; Morgan Kaufmann: Boston, MA, USA, 2017; pp. 131–161. [Google Scholar] [CrossRef]
- The Statistical Yearbook (2020), Ministry of Health, Saudi Arabia. Available online: https://www.moh.gov.sa/en/Ministry/Statistics/book/Pages/default.aspx (accessed on 22 April 2021).
- Ozdemir, M.H.; Saracoglu, A.; Ozdemir, A.U.; Ergonen, A.T. Dental malpractice cases in Turkey during 1991–2000. J. Clin. Forensic Med. 2005, 12, 137–142. [Google Scholar] [CrossRef]
- Borgia, E.; Baron, R.; Borgia, J.L. Quality and Survival of Direct Light-Activated Composite Resin Restorations in Posterior Teeth: A 5- to 20-Year Retrospective Longitudinal Study. J. Prosthodont. 2019, 28, e195–e203. [Google Scholar] [CrossRef]
- Bohaty, B.S.; Ye, Q.; Misra, A.; Sene, F.; Spencer, P. Posterior composite restoration update: Focus on factors influencing form and function. Clin. Cosmet. Investig. Dent. 2013, 5, 33–42. [Google Scholar] [CrossRef]
- Palotie, U.; Eronen, A.K.; Vehkalahti, K.; Vehkalahti, M.M. Longevity of 2- and 3-surface restorations in posterior teeth of 25- to 30-year-olds attending Public Dental Service—A 13-year observation. J. Dent. 2017, 62, 13–17. [Google Scholar] [CrossRef]
- Kopperud, S.E.; Tveit, A.B.; Gaarden, T.; Sandvik, L.; Espelid, I. Longevity of posterior dental restorations and reasons for failure. Eur. J. Oral. Sci. 2012, 120, 539–548. [Google Scholar] [CrossRef]
- Pallesen, U.; van Dijken, J.W. A randomized controlled 27 years follow up of three resin composites in Class II restorations. J. Dent. 2015, 43, 1547–1558. [Google Scholar] [CrossRef]
- Dablanca-Blanco, A.B.; Blanco-Carrión, J.; Martín-Biedma, B.; Varela-Patiño, P.; Bello-Castro, A.; Castelo-Baz, P. Management of large class II lesions in molars: How to restore and when to perform surgical crown lengthening? Restor. Dent. Endod. 2017, 42, 240–252. [Google Scholar] [CrossRef]
- Veneziani, M. Adhesive restorations in the posterior area with subgingival cervical margins: New classification and differentiated treatment approach. Eur. J. Esthet. Dent. 2010, 5, 50–76. [Google Scholar]
- Bailey, O.; O’Connor, C. Papilla management in sub-gingival, interproximal, direct composite restoration: A key step to success. Br. Dent. J. 2019, 226, 933–937. [Google Scholar] [CrossRef]
- Bertoldi, C.; Monari, E.; Cortellini, P.; Generali, L.; Lucchi, A.; Spinato, S.; Zaffe, D. Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin. Oral. Investing. 2020, 24, 1001–1011. [Google Scholar] [CrossRef]
- Peumans, M.; Politano, G.; Van Meerbeek, B. Effective Protocol for Daily High-quality Direct Posterior Composite Restorations. Cavity Preparation and Design. J. Adhes. Dent. 2020, 22, 581–596. [Google Scholar] [CrossRef]
- Zabrovsky, A.; Neeman Levy, T.; Bar-On, H.; Beyth, N.; Ben-Gal, G. Next generation of dentists moving to amalgam-free dentistry: Survey of posterior restorations teaching in North America. Eur. J. Dent. Educ. 2019, 23, 355–363. [Google Scholar] [CrossRef]
- Awad, M.M.; Salem, W.S.; Almuhaizaa, M.; Aljeaidi, Z. Contemporary teaching of direct posterior composite restorations in Saudi dental schools. Saudi J. Dent. Res. 2017, 8, 42–51. [Google Scholar] [CrossRef]
- Lynch, C.D.; Shortall, A.C.; Stewardson, D.; Tomson, P.L.; Burke, F.J. Teaching posterior composite resin restorations in the United Kingdom and Ireland: Consensus views of teachers. Br. Dent. J. 2007, 203, 183–187. [Google Scholar] [CrossRef]
- Lynch, C.D.; Frazier, K.B.; McConnell, R.J.; Blum, I.R.; Wilson, N.H. State-of-the-art techniques in operative dentistry: Contemporary teaching of posterior composites in UK and Irish dental schools. Br. Dent. J. 2010, 209, 129–136. [Google Scholar] [CrossRef]
- Lynch, C.D.; O’Sullivan, V.R.; Dockery, P.; McGillycuddy, C.T.; Rees, J.S.; Sloan, A.J. Hunter-Schreger Band patterns and their implications for clinical dentistry. J. Oral. Rehabil. 2011, 38, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Rousson, V. Clinical effectiveness of direct class II restorations—A meta-analysis. J. Adhes. Dent. 2012, 14, 407–431. [Google Scholar] [CrossRef]
- Cajazeira, M.R.; De Saboia, T.M.; Maia, L.C. Influence of the operatory field isolation technique on tooth-colored direct dental restorations. Am. J. Dent. 2014, 27, 155–159. [Google Scholar] [PubMed]
- Raskin, A.; Setcos, J.C.; Vreven, J.; Wilson, N.H. Influence of the isolation method on the 10-year clinical behaviour of posterior resin composite restorations. Clin. Oral. Investing. 2000, 4, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Van Meerbeek, B. Editorial: Rubber-dam—A blessing not only in the Covid-19 era. J. Adhes. Dent. 2021, 23, 3. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Yoshihara, K.; Van Landuyt, K.; Yoshida, Y.; Peumans, M. From Buonocore’s Pioneering Acid-Etch Technique to Self-Adhering Restoratives. A Status Perspective of Rapidly Advancing Dental Adhesive Technology. J. Adhes. Dent. 2020, 22, 7–34. [Google Scholar] [CrossRef]
- Mazzoni, A.; Nascimento, F.D.; Carrilho, M.; Tersariol, I.; Papa, V.; Tjäderhane, L.; Di Lenarda, R.; Tay, F.R.; Pashley, D.H.; Breschi, L. MMP activity in the hybrid layer detected with in situ zymography. J. Dent. Res. 2012, 91, 467–472. [Google Scholar] [CrossRef]
- Liu, Y.; Tjäderhane, L.; Breschi, L.; Mazzoni, A.; Li, N.; Mao, J.; Pashley, D.H.; Tay, F.R. Limitations in bonding to dentin and experimental strategies to prevent bond degradation. J. Dent. Res. 2011, 90, 953–968. [Google Scholar] [CrossRef]
- Breschi, L.; Maravic, T.; Cunha, S.R.; Comba, A.; Cadenaro, M.; Tjaderhane, L.; Pashley, D.H.; Tay, F.R.; Mazzoni, A. Dentin bonding systems: From dentin collagen structure to bond preservation and clinical applications. Dent. Mater. 2018, 34, 78–96. [Google Scholar] [CrossRef]
- Frankenberger, R.; Lohbauer, U.; Roggendorf, M.J.; Naumann, M.; Taschner, M. Selective enamel etching reconsidered: Better than etch-and-rinse and self-etch. J. Adhes. Dent. 2008, 10, 339–344. [Google Scholar]
- Feltrin Antoniazzi, B.; Ferreira Nicoloso, G.; Larissa Lenzi, T.; Soares, M.; Zovico, F.; de Oliveira Rocha, R. Selective Acid Etching Improves the Bond Strength of Universal Adhesive to Sound and Demineralized Enamel of Primary Teeth. J. Adhes. Dent. 2016, 18, 311–316. [Google Scholar] [CrossRef]
- Cuevas-Suárez, C.E.; da Rosa, W.L.O.; Lund, R.G.; da Silva, A.F.; Piva, E. Bonding Performance of Universal Adhesives: An Updated Systematic Review and Meta-Analysis. J. Adhes. Dent. 2019, 21, 7–26. [Google Scholar] [CrossRef]
- Peumans, M.; Van Meerbeek, B.; Asscherickx, K.; Simon, S.; Abe, Y.; Lambrechts, P.; Vanherle, G. Do condensable composites help to achieve better proximal contacts? Dent. Mater. 2001, 17, 533–541. [Google Scholar] [CrossRef]
- Loomans, B.A.; Opdam, N.J.; Roeters, F.J.; Bronkhorst, E.M.; Burgersdijk, R.C.; Dorfer, C.E. A randomized clinical trial on proximal contacts of posterior composites. J. Dent. 2006, 34, 292–297. [Google Scholar] [CrossRef]
- Loomans, B.A.; Opdam, N.J.; Roeters, J.F.; Bronkhorst, E.M.; Plasschaert, A.J. Influence of composite resin consistency and placement technique on proximal contact tightness of Class II restorations. J. Adhes. Dent. 2006, 8, 305–310. [Google Scholar] [CrossRef]
- Van der Vyver, P.J. Posterior composite resin restorations. Part 3. Matrix systems. S. Afr. Dent. J. 2002, 57, 221–226. [Google Scholar]
- Hancock, E.B.; Mayo, C.V.; Schwab, R.R.; Wirthlin, M.R. Influence of interdental contacts on periodontal status. J. Periodontol. 1980, 51, 445–449. [Google Scholar] [CrossRef]
- Ferracane, J.L. Buonocore Lecture. Placing dental composites—A stressful experience. Oper. Dent. 2008, 33, 247–257. [Google Scholar] [CrossRef]
- Felix, S.A.; Gonzalez-Lopez, S.; Mauricio, P.D.; Aguilar-Mendoza, J.A.; Bolanos-Carmona, M.V. Effects of filling techniques on the regional bond strength to lateral walls in Class I cavities. Oper. Dent. 2007, 32, 602–609. [Google Scholar] [CrossRef]
- Niu, Y.; Ma, X.; Fan, M.; Zhu, S. Effects of layering techniques on the micro-tensile bond strength to dentin in resin composite restorations. Dent. Mater. 2009, 25, 129–134. [Google Scholar] [CrossRef]
- Gonzalez-Lopez, S.; Lucena-Martin, C.; de Haro-Gasquet, F.; Vilchez-Diaz, M.A.; de Haro-Munoz, C. Influence of different composite restoration techniques on cuspal deflection: An in vitro study. Oper. Dent. 2004, 29, 656–660. [Google Scholar] [PubMed]
- Al Shaafi, M.; Maawadh, A.; Al Qahtani, M. Evaluation of Light Intensity Output of QTH and LED Curing Devices in Various Governmental Health Institutions. Oper. Dent. 2011, 36, 356–361. [Google Scholar] [CrossRef]
- Rueggeberg, F.A. State-of-the-art: Dental photocuring--a review. Dent. Mater. 2011, 27, 39–52. [Google Scholar] [CrossRef] [PubMed]
- Roulet, J.F.; Price, R. Light curing—Guidelines for practitioners—A consensus statement from the 2014 symposium on light curing in dentistry held at Dalhousie University, Halifax, Canada. J. Adhes. Dent. 2014, 16, 303–304. [Google Scholar] [CrossRef] [PubMed]
- Alqabbaa, L.M.; Alsenani, M.S.; Alsaif, N.S.; Alsaif, R.A.; Binalrimal, S.R. Light intensity output of visible light communication units and clinicians’ knowledge and attitude among Riyadh private clinics. J. Conserv. Dent. 2018, 21, 667–670. [Google Scholar] [CrossRef] [PubMed]
- Davidson, D.F.; Suzuki, M. A prescription for the successful use of heavy filled composites in the posterior dentition. J. Can. Dent. Assoc. 1999, 65, 256–260. [Google Scholar] [PubMed]
- Jackson, R.D. Class II composite resin restorations: Faster, easier, predictable. Br. Dent. J. 2016, 221, 623–631. [Google Scholar] [CrossRef] [PubMed]
| DPs’ Information | Total n = 123 (100%) | Governmental n = 37 (30%) | Private n = 86 (70%) |
|---|---|---|---|
| Professional registration | |||
| General Practitioner (GP) | 76 (61.8) | 16 (13) | 60 (48.8) |
| Resident | 5 (4.1) | 0 | 5 (4.1) |
| Registrar | 10 (8.1) | 7 (5.7) | 3 (2.4) |
| Senior registrar | 11 (9) | 7 (5.7) | 4 (3.3) |
| Consultant | 21 (17.1) | 7 (5.7) | 14 (11.4) |
| Years of clinical experience | |||
| 0–2 years | 12 (9.8) | 5 (4.1) | 7 (5.7) |
| 2–5 years | 27 (22) | 8 (6.5) | 19 (15.4) |
| More than 5 years | 84 (68.3) | 24 (19.5) | 60 (48.8) |
| Question | Governmental n = 37 (30%) | Private n = 86 (70%) | p-Value |
|---|---|---|---|
| Q1. Which material do often you use in posterior small cavity (1 or 2 surfaces)? | 0.452 | ||
| Amalgam | 0 | 4 (3.3) | |
| Composite | 35 (28.4) | 79 (64.2) | |
| Resin modified glass ionomer | 2 (1.7) | 3 (2.4) | |
| Q2. Which material do you often use in posterior large cavity (3 or more surfaces)? | 0.746 | ||
| Amalgam | 4 (3.2) | 12 (9.8) | |
| Composite | 22 (17.9) | 54 (43.9) | |
| Other (Indirect restoration) | 11 (9) | 20 (16.2) | |
| Q3. Do you often place direct posterior composite restorations in patients with oral para-functional activity? | 1.000 | ||
| Yes | 10 (8.1) | 23 (18.7) | |
| No | 27 (22) | 63 (51.2) | |
| Q4. Do you often place direct posterior composite restorations in patients with poor oral hygiene? | 0.066 | ||
| Yes | 15 (12.2) | 52 (42.3) | |
| No | 22 (17.9) | 34 (27.6) | |
| Q5. Do you often place direct posterior composite restorations in posterior cavities with 1–2 mm Sub-gingival margins | 0.201 | ||
| Yes | 14 (11.4) | 45 (36.6) | |
| No | 23 (18.7) | 41 (33.3) |
| Question | Governmental n = 37 (30%) | Private n = 86 (70%) | p-Value |
|---|---|---|---|
| Q6. Do you prepare a minimum pulpal depth of 2 mm for occlusal cavities? | 0.001 * | ||
| Yes | 11 (9) | 56 (45.5) | |
| No | 26 (21.1) | 30 (24.4) | |
| Q7. Do you prepare mechanical means of retention for composite restorations? | 0.003 * | ||
| Yes | 9 (7.4) | 48 (38.9) | |
| No | 28 (22.8) | 38 (30.9) | |
| Q8. Do you bevel the occlusal margins of the cavity? | 0.120 | ||
| Yes | 13 (10.6) | 45 (36.6) | |
| No | 24 (19.5) | 41 (33.3) | |
| Q9. Do you bevel the gingival margin of the cavity? | 0.212 | ||
| Yes | 8 (6.5) | 30 (24.4) | |
| No | 29 (23.6) | 56 (45.5) |
| Question | Governmental n = 37 (30%) | Private n = 86 (70%) | p-Value |
|---|---|---|---|
| Q10. How often do you achieve the operative field isolation? | 0.004 # | ||
| Rubber dam | 23 (18.7) | 26 (21.1) | |
| Cotton rolls and intraoral suction (Partial isolation) | 13 (10.6) | 55 (44.7) | |
| Other | 1 (0.8) | 5 (4.1) | |
| Q11. Which adhesive strategy do you use more often? | <0.001 # | ||
| Etch-and-rinse (total etch) | 30 (24.4) | 37 (30.1) | |
| Self-etching (no acid etching) | 2 (1.7) | 26 (21.1) | |
| Selective enamel etching | 5 (4.1) | 23 (18.7) | |
| Q12. Which placement technique do you often apply for the placement of composite restorations? | 0.472 | ||
| Horizontal layering | 12 (9.8) | 30 (24.4) | |
| Oblique layering | 25 (20.3) | 52 (42.3) | |
| Bulk-fill | 0 | 4 (3.2) | |
| Q13. Which light-curing unit do you often use to light-cure posterior restorations? | 0.013 # | ||
| Quartz tungsten halogen (QTH) | 9 (7.3) | 6 (4.9) | |
| Light emitting diodes (LED) | 28 (22.8) | 79 (64.2) | |
| Other | 0 | 1 (0.8) | |
| Q14. Do you regularly monitor the output of light-curing unit with a radiometer? | 0.023 * | ||
| Yes | 10 (8.1) | 8 (6.5) | |
| No | 27 (22) | 78 (63.4) | |
| Q15. How long do you light-cure composite increment of 2 mm thickness? | 0.784 | ||
| 10s | 4 (3.3) | 9 (7.3) | |
| 15s | 7 (5.7) | 18 (14.6) | |
| 20s | 26 (21.1) | 59 (48) | |
| Q16. For class II composite restorations, after removal of the matrix band, do you often perform additional light-curing from the buccal and lingual directions? | 0.087 | ||
| Yes | 29 (23.6) | 52 (42.3) | |
| No | 8 (6.5) | 34 (27.6) | |
| Q17. Which matrix system do you often use to restore the proximal contact with composite restoration? | <0.001 # | ||
| Sectional matrix | 19 (15.4) | 21 (17.1) | |
| Tofflemire matrix | 6 (4.9) | 50 (40.6) | |
| Circumferential matrix | 10 (8.1) | 11 (9) | |
| Other | 2 (1.7) | 4 (3.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Awad, M.M.; Alradan, M.; Alshalan, N.; Alqahtani, A.; Alhalabi, F.; Salem, M.A.; Rabah, A.; Alrahlah, A. Placement of Posterior Composite Restorations: A Cross-Sectional Study of Dental Practitioners in Al-Kharj, Saudi Arabia. Int. J. Environ. Res. Public Health 2021, 18, 12408. https://doi.org/10.3390/ijerph182312408
Awad MM, Alradan M, Alshalan N, Alqahtani A, Alhalabi F, Salem MA, Rabah A, Alrahlah A. Placement of Posterior Composite Restorations: A Cross-Sectional Study of Dental Practitioners in Al-Kharj, Saudi Arabia. International Journal of Environmental Research and Public Health. 2021; 18(23):12408. https://doi.org/10.3390/ijerph182312408
Chicago/Turabian StyleAwad, Mohamed M., Mansour Alradan, Nawaf Alshalan, Ali Alqahtani, Feras Alhalabi, Mohammed Ali Salem, Ahmed Rabah, and Ali Alrahlah. 2021. "Placement of Posterior Composite Restorations: A Cross-Sectional Study of Dental Practitioners in Al-Kharj, Saudi Arabia" International Journal of Environmental Research and Public Health 18, no. 23: 12408. https://doi.org/10.3390/ijerph182312408
APA StyleAwad, M. M., Alradan, M., Alshalan, N., Alqahtani, A., Alhalabi, F., Salem, M. A., Rabah, A., & Alrahlah, A. (2021). Placement of Posterior Composite Restorations: A Cross-Sectional Study of Dental Practitioners in Al-Kharj, Saudi Arabia. International Journal of Environmental Research and Public Health, 18(23), 12408. https://doi.org/10.3390/ijerph182312408







