Association of Grip Strength with Quality of Life in the Chinese Oldest Old
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Quality of Life
2.2.2. Grip Strength
2.2.3. Covariates
2.3. Data Analysis
3. Results
3.1. Sample Characteristics
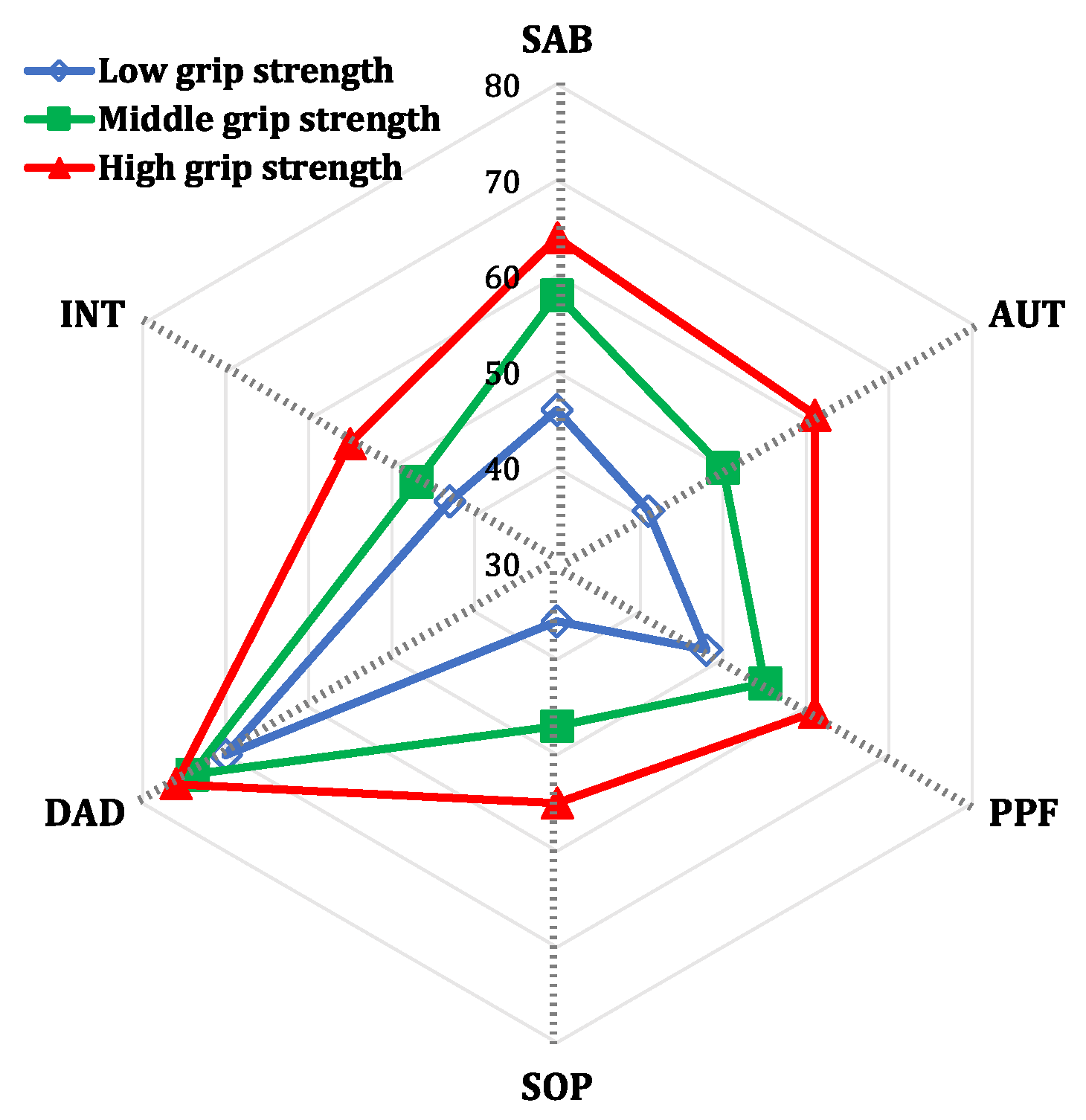
3.2. Association between Grip Strength and Quality of Life
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- United Nations, Department of Economic and Social Affairs. World World Population Aging 2017. Available online: https://www.un.org/en/development/desa/population/theme/ageing/WPA2017.asp (accessed on 10 October 2021).
- Osypuk, T.L.; Joshi, P.; Geronimo, K.; Acevedo-Garcia, D. Do Social and Economic Policies Influence Health? A Review. Curr. Epidemiol. Rep. 2014, 1, 149–164. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Goodkind, D.; Kowal, P. An Aging World: 2015. Available online: https://www.census.gov/content/dam/Census/library/publications/2016/demo/p95-16-1.pdf (accessed on 12 October 2021).
- National Bureau of Statisitcs of China. Tabulation on the 2020 Population Census of the People’s Republic of China; National Bureau of Statisitcs of China: Beijing, China, 2021.
- Salomon, J.A.; Wang, H.; Freeman, M.K.; Vos, T.; Flaxman, A.D.; Lopez, A.D.; Murray, C.J. Healthy life expectancy for 187 countries, 1990–2010: A systematic analysis for the Global Burden Disease Study 2010. Lancet 2012, 380, 2144–2162. [Google Scholar] [CrossRef]
- Costanza, R.; Fisher, B.; Ali, S.; Beer, C.; Bond, L.; Boumans, R.; Danigelis, N.L.; Dickinson, J.; Elliott, C.; Farley, J.; et al. Quality of life: An approach integrating opportunities, human needs, and subjective well-being. Ecol. Econ. 2007, 61, 267–276. [Google Scholar] [CrossRef]
- WHOQOL Group. Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual. Life Res. 1993, 2, 153–159. [Google Scholar] [CrossRef]
- Phyo, A.Z.Z.; Freak-Poli, R.; Craig, H.; Gasevic, D.; Stocks, N.P.; Gonzalez-Chica, D.A.; Ryan, J. Quality of life and mortality in the general population: A systematic review and meta-analysis. BMC Public Health 2020, 20, 1596. [Google Scholar] [CrossRef]
- Lapid, M.I.; Rummans, T.A.; Boeve, B.F.; McCormick, J.K.; Pankratz, V.S.; Cha, R.H.; Smith, G.E.; Ivnik, R.J.; Tangalos, E.G.; Petersen, R.C. What is the quality of life in the oldest old? Int. Psychogeriatr. 2011, 23, 1003–1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bohannon, R.W. Grip Strength: An Indispensable Biomarker For Older Adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef] [Green Version]
- Soysal, P.; Hurst, C.; Demurtas, J.; Firth, J.; Howden, R.; Yang, L.; Tully, M.A.; Koyanagi, A.; Ilie, P.C.; Lopez-Sanchez, G.F.; et al. Handgrip strength and health outcomes: Umbrella review of systematic reviews with meta-analyses of observational studies. J. Sport Health Sci. 2020, 10, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Li, T.; Yang, H.; Wang, J.; Liu, M.; Wang, S.; He, Y.; Jiang, B. Association between muscle strength and health-related quality of life in a Chinese rural elderly population: A cross-sectional study. BMJ Open 2020, 10, e026560. [Google Scholar] [CrossRef] [Green Version]
- Laudisio, A.; Giovannini, S.; Finamore, P.; Loreti, C.; Vannetti, F.; Coraci, D.; Incalzi, R.A.; Zuccal, G.; Macchi, C.; Padua, L.; et al. Muscle strength is related to mental and physical quality of life in the oldest old. Arch. Gerontol. Geriatr. 2020, 89, 104109. [Google Scholar] [CrossRef] [PubMed]
- Sayer, A.A.; Syddall, H.E.; Martin, H.J.; Dennison, E.M.; Roberts, H.C.; Cooper, C. Is grip strength associated with health-related quality of life? Findings from the Hertfordshire Cohort Study. Age Ageing 2006, 35, 409–415. [Google Scholar] [CrossRef] [Green Version]
- Haider, S.; Luger, E.; Kapan, A.; Titze, S.; Lackinger, C.; Schindler, K.E.; Dorner, T.E. Associations between daily physical activity, handgrip strength, muscle mass, physical performance and quality of life in prefrail and frail community-dwelling older adults. Qual. Life Res. 2016, 25, 3129–3138. [Google Scholar] [CrossRef] [Green Version]
- Molzahn, A.; Skevington, S.M.; Kalfoss, M.; Makaroff, K.S. The importance of facets of quality of life to older adults: An international investigation. Qual. Life Res. 2010, 19, 293–298. [Google Scholar] [CrossRef]
- Power, M.; Quinn, K.; Schmidt, S.; Group, W.-O. Development of the WHOQOL-old module. Qual. Life Res. 2005, 14, 2197–2214. [Google Scholar] [CrossRef]
- Liu, R.; Wu, S.; Hao, Y.; Gu, J.; Fang, J.; Cai, N.; Zhang, J. The Chinese version of the world health organization quality of life instrument-older adults module (WHOQOL-OLD): Psychometric evaluation. Health Qual. Life Outcomes 2013, 11, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization European Office. WHOQOL-OLD. Available online: https://www.who.int/mental_health/evidence/WHOQOL_OLD_Manual.pdf (accessed on 10 May 2021).
- Schlüssel, M.M.; dos Anjos, L.A.; de Vasconcellos, M.T.; Kac, G. Reference values of handgrip dynamometry of healthy adults: A population-based study. Clin. Nutr. 2008, 27, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Ge, X.; Hou, S.; Gao, G.; Zhang, X.; Yu, Y. Ability of daily living and its influencing factors among rural elderly in Dabieshan Mountain area. Chin. J. Public Health 2012, 7, 884–886. [Google Scholar]
- Hoyl, M.T.; Alessi, C.A.; Harker, J.O.; Josephson, K.R.; Pietruszka, F.M.; Koelfgen, M.; Mervis, J.R.; Fitten, L.J.; Rubenstein, L.Z. Development and testing of a five-item version of the Geriatric Depression Scale. J. Am. Geriatr. Soc. 1999, 47, 873–878. [Google Scholar] [CrossRef]
- Li, Z. The Evaluation and Application of the Chinese Version of the Short-form UCLA Loneliness Scale. Master’s Thesis, Central South University, Changsha, China, 2012. [Google Scholar]
- Chen, K.L.; Xu, Y.; Chu, A.Q.; Ding, D.; Liang, X.N.; Nasreddine, Z.S.; Dong, Q.; Hong, Z.; Zhao, Q.H.; Guo, Q.H. Validation of the Chinese Version of Montreal Cognitive Assessment Basic for Screening Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2016, 64, e285–e290. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 4th ed.; SAGE Publications Limited: London, UK, 2018. [Google Scholar]
- Baernholdt, M.; Hinton, I.; Yan, G.; Rose, K.; Mattos, M. Factors associated with quality of life in older adults in the United States. Qual. Life Res. 2012, 21, 527–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klompstra, L.; Ekdahl, A.W.; Krevers, B.; Milberg, A.; Eckerblad, J. Factors related to health-related quality of life in older people with multimorbidity and high health care consumption over a two-year period. BMC Geriatr. 2019, 19, 187. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.M.; Titus, A.J.; Bruce, M.L.; Orzechowski, N.M.; Mackenzie, T.A.; Bartels, S.J.; Batsis, J.A. Depression and Handgrip Strength among U.S. Adults Aged 60 Years and Older from NHANES 2011-2014. J. Nutr. Health Aging 2018, 22, 938–943. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.R.; Jung, S.M.; Bang, H.; Kim, H.S.; Kim, Y.B. The association between muscular strength and depression in Korean adults: A cross-sectional analysis of the sixth Korea National Health and Nutrition Examination Survey (KNHANES VI) 2014. BMC Public Health 2018, 18, 1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.-M.; Chen, C.-M. Factors Associated with Quality of Life Among Older Adults with Chronic Disease in Taiwan. Int. J. Gerontol. 2017, 11, 12–15. [Google Scholar] [CrossRef] [Green Version]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Garcia, S.; Garcia-Pena, C.; Ramirez-Garcia, E.; Moreno-Tamayo, K.; Cantu-Quintanilla, G.R. Decreased Autonomy in Community-Dwelling Older Adults. Clin. Interv. Aging 2019, 14, 2041–2053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Xia, R.; Wang, S.; Xue, W.; Yang, J.; Sun, S.; Zhuang, G. Relative Contributions of Different Lifestyle Factors to Health-Related Quality of Life in the Elderly. Int. J. Environ. Res. Public Health 2018, 15, 256. [Google Scholar] [CrossRef] [Green Version]
- Moreno-Tamayo, K.; Manrique-Espinoza, B.; Ramirez-Garcia, E.; Sanchez-Garcia, S. Social isolation undermines quality of life in older adults. Int. Psychogeriatr. 2020, 32, 1283–1292. [Google Scholar] [CrossRef] [PubMed]
- Gobbens, R.J.; van Assen, M.A. Psychometric properties of the Dutch WHOQOL-OLD. Health Qual. Life Outcomes 2016, 14, 103. [Google Scholar] [CrossRef] [Green Version]
- Bilgili, N.; Arpaci, F. Quality of life of older adults in Turkey. Arch. Gerontol. Geriatr. 2014, 59, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Gobbens, R.J.; Remmen, R. The effects of sociodemographic factors on quality of life among people aged 50 years or older are not unequivocal: Comparing SF-12, WHOQOL-BREF, and WHOQOL-OLD. Clin. Interv. Aging 2019, 14, 231–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total (n = 400) | Low QOL (n = 203) | High QOL (n = 197) | p Value | ||
|---|---|---|---|---|---|
| N (%)/Mean (SD)/Median (IQR) | N (%)/Mean (SD)/Median (IQR) | N (%)/Mean (SD)/Median (IQR) | |||
| Age (years) | 85.18 (4.20) | 86.66 (4.31) | 83.70 (3.53) | <0.001 ** | |
| Age group | 80–85 years | 228 (57.00) | 86 (42.36) | 142 (72.08) | <0.001 ** |
| ≥86 years | 172 (43.00) | 117 (57.64) | 55 (27.92) | ||
| Gender | Female | 186 (46.5) | 85 (41.87) | 101 (51.27) | 0.060 |
| Male | 214 (53.50) | 118 (58.13) | 96 (48.73) | ||
| Educated years | ≤9 years | 209 (52.25) | 114 (56.16) | 95 (48.22) | 0.112 |
| >9 years | 191 (47.75) | 89 (43.84) | 102 (51.78) | ||
| Marital status | unmarried | 163 (40.75) | 99 (48.77) | 64 (32.49) | 0.001 * |
| Married | 237 (59.25) | 104 (51.23) | 133 (67.51) | ||
| Living arrangement | Alone | 60 (15.00) | 30 (14.78) | 30 (15.23) | 0.900 |
| With others | 340 (85.00) | 173 (85.22) | 167 (84.77) | ||
| Number of chronic conditions | none or one | 83 (20.75) | 19 (9.36) | 64 (32.49) | <0.001 ** |
| two | 96 (24.00) | 35 (17.24) | 61 (30.96) | ||
| ≥three | 221 (55.25) | 149 (73.40) | 72 (36.55) | ||
| Polypharmacy | No | 243 (60.75) | 83 (40.89) | 160 (81.22) | <0.001 ** |
| Yes | 157 (39.25) | 120 (59.11) | 37 (18.78) | ||
| ADL/IADL limitations | Normal | 217 (54.25) | 46 (22.66) | 171 (86.80) | <0.001 ** |
| Limited | 183 (45.75) | 157 (77.34) | 26 (13.20) | ||
| Depression | Normal | 238 (59.50) | 71 (34.98) | 167 (84.77) | <0.001 ** |
| depressed | 162 (40.50) | 132 (65.02) | 30 (15.23) | ||
| Loneliness (score) a | 7 (4) | 9 (7) | 6 (1) | <0.001 ** | |
| Cognitive function | Normal | 152 (38.00) | 36 (17.73) | 116 (58.88) | <0.001 ** |
| Impaired | 248 (62.00) | 167 (82.27) | 81 (41.12) | ||
| Handgrip strength | 19.82 (6.94) | 17.07 (6.47) | 22.65 (6.25 | <0.001 ** | |
| Main Independent Variable | Crude Model | Adjusted Model1 a | Adjusted Model 2 b | |||
|---|---|---|---|---|---|---|
| β (95%CI) | p | β (95%CI) | p | β (95%CI) | p | |
| Overall QOL | ||||||
| Grip strength | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 7.86 (5.36, 10.37) | <0.001 | 3.26 (1.18, 5.34) | 0.002 | 2.04 (0.23, 3.85) | 0.027 |
| High | 14.82 (12.31, 17.33) | <0.001 | 6.96 (4.69, 9.22) | <0.001 | 4.40 (2.40, 6.40) | <0.001 |
| p for trend | <0.001 | <0.001 | <0.001 | |||
| partial ω2 | 0.336 | 0.104 | 0.053 | |||
| Sensory ability | ||||||
| Grip strength | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 12.42 (8.11, 16.72) | <0.001 | 5.59 (1.41, 9.78) | 0.009 | 4.00 (−0.01, 8.02) | 0.051 |
| High | 18.35 (14.03, 22.66) | <0.001 | 7.44 (2.89, 11.99) | 0.001 | 4.29 (−0.14, 8.73) | 0.058 |
| p for trend | <0.001 | 0.002 | 0.063 | |||
| partial ω2 | 0.219 | 0.038 | 0.004 | |||
| Autonomy | ||||||
| Grip strength | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 9.50 (5.97, 13.03) | <0.001 | 2.84 (−0.09, 5.77) | 0.058 | 1.70 (1.87, 7.70) | 0.231 |
| High | 20.53 (16.99, 24.07) | <0.001 | 9.17 (5.98, 12.36) | <0.001 | 6.74 (3.66,9.81) | <0.001 |
| p for trend | <0.001 | <0.001 | <0.001 | |||
| partial ω2 | 0.307 | 0.079 | 0.044 | |||
| Past, present and future activities | ||||||
| Grip strength | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 6.66 (4.09, 9.22) | <0.001 | 2.81 (0.42, 5.19) | 0.021 | 1.62 (−0.52, 3.76) | 0.136 |
| High | 12.94 (10.37, 15.52) | <0.001 | 6.13 (3.53, 8.72) | <0.001 | 3.52 (1.15, 5.88) | 0.004 |
| p for trend | <0.001 | <0.001 | 0.004 | |||
| partial ω2 | 0.254 | 0.061 | 0.022 | |||
| Social participation | ||||||
| Grip strength | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 11.06 (7.63, 14.49) | <0.001 | 5.08 (2.18, 7.98) | 0.001 | 3.60 (0.91, 6.29) | 0.009 |
| High | 19.72 (16.28, 23.16) | <0.001 | 9.43 (6.28, 12.59) | <0.001 | 6.72 (3.75,9.69) | <0.001 |
| p for trend | <0.001 | <0.001 | <0.001 | |||
| partial ω2 | 0.329 | 0.106 | 0.061 | |||
| Perception of death and dying | ||||||
| Grip strength | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 3.61 (0.29, 6.92) | 0.033 | 2.98 (−0.43, 6.40) | 0.086 | 2.41 (−0.99, 5.82) | 0.164 |
| High | 5.41 (2.09, 8.73) | 0.001 | 4.14 (0.46, 7.85) | 0.029 | 2.85 (−0.91, 6.62) | 0.971 |
| p for trend | 0.001 | 0.530 | 0.970 | |||
| partial ω2 | 0.031 | 0.031 | 0.142 | |||
| Intimacy | ||||||
| Grip strength | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 3.94 (0.42, 7.47) | 0.0281 | 0.24 (−3.22, 3.71) | 0.891 | −1.09 (−4.28, 2.10) | 0.503 |
| High | 11.98 (8.45, 15.51) | <0.001 | 5.44 (1.68, 9.21) | 0.005 | 2.29 (−1.23, 5.82) | 0.202 |
| p for trend | <0.001 | 0.004 | 0.183 | |||
| partial ω2 | 0.107 | 0.015 | 0.0002 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, B.; Ma, C. Association of Grip Strength with Quality of Life in the Chinese Oldest Old. Int. J. Environ. Res. Public Health 2021, 18, 12394. https://doi.org/10.3390/ijerph182312394
Xie B, Ma C. Association of Grip Strength with Quality of Life in the Chinese Oldest Old. International Journal of Environmental Research and Public Health. 2021; 18(23):12394. https://doi.org/10.3390/ijerph182312394
Chicago/Turabian StyleXie, Boqin, and Chenjuan Ma. 2021. "Association of Grip Strength with Quality of Life in the Chinese Oldest Old" International Journal of Environmental Research and Public Health 18, no. 23: 12394. https://doi.org/10.3390/ijerph182312394
APA StyleXie, B., & Ma, C. (2021). Association of Grip Strength with Quality of Life in the Chinese Oldest Old. International Journal of Environmental Research and Public Health, 18(23), 12394. https://doi.org/10.3390/ijerph182312394







