Associations of Dietary Patterns and Risk of Hypertension in Southwest China: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Recruitment and Study Population
2.2. Assessment of Dietary Patterns
2.3. Assessment of Outcome and Covariates
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Subjects
3.2. Distribution of Dietary Patterns
3.3. Associations between Dietary Patterns and Hypertension Incidence
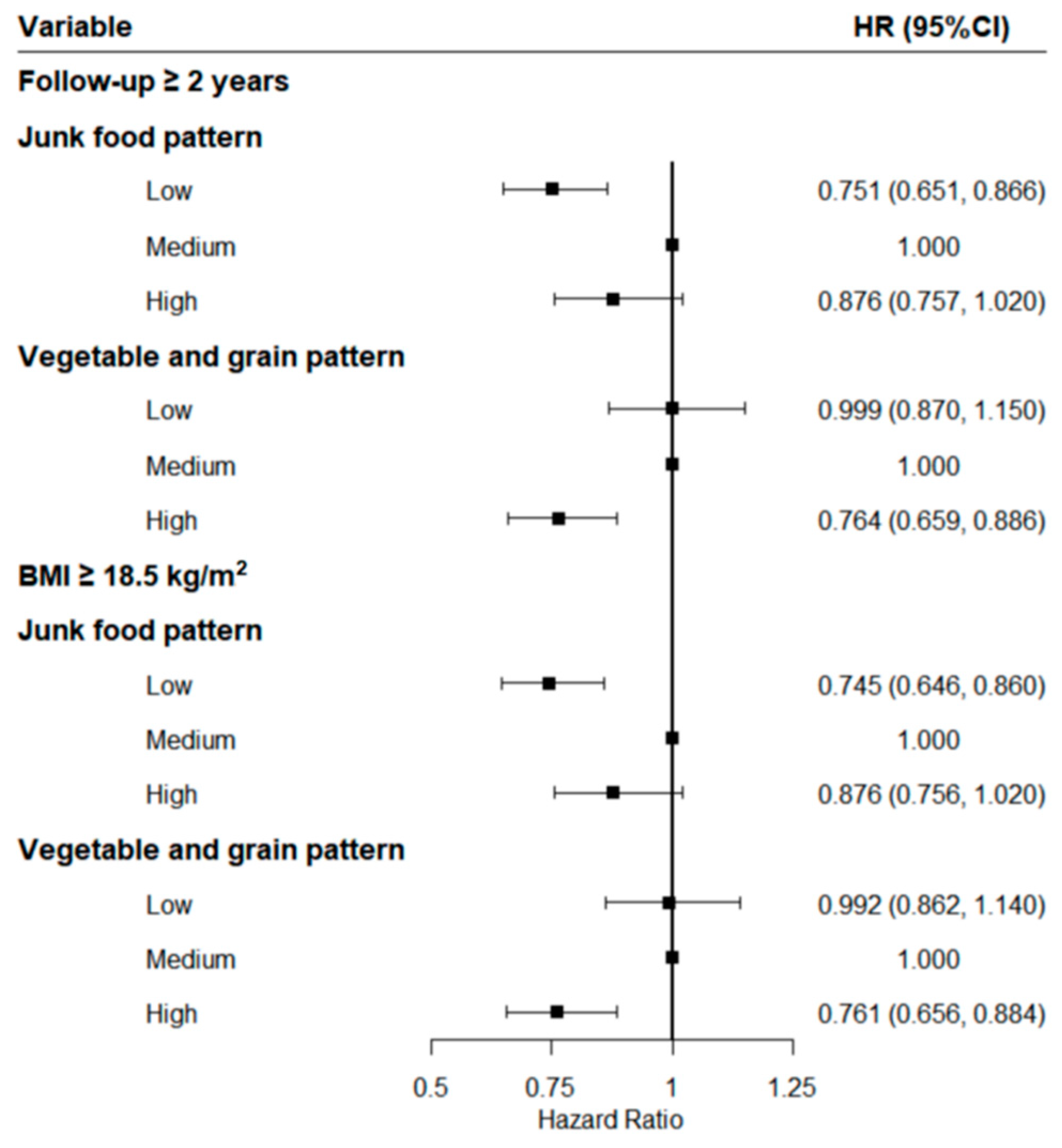
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, B.; Bentham, J.; Di Cesare, M.; Bixby, H.; Danaei, G.; Cowan, M.J.; Paciorele, C.J.; Singh, G.; Hajifathalian, K.; Benett, J.E.; et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, L.; Wang, F.; Liu, L.; Wang, H. Prevalence, awareness, treatment, and control of hypertension in China: Results from a national survey. Am. J. Hypertens. 2014, 27, 1355–1361. [Google Scholar] [CrossRef]
- Shim, J.S.; Oh, K.; Jung, S.J.; Kim, H.C. Self-reported diet management and adherence to dietary guidelines in Korean adults with hypertension. Korean Circ J. 2020, 50, 432–440. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Despres, J.-P.; Fullerton, H.J.; Howard, V.J.; et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef]
- Song, S.; Kim, J.; Kim, J. Gender differences in the association between dietary pattern and the incidence of hypertension in middle-aged and older adults. Nutrients 2018, 10, 252. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Campos, H. Dietary therapy in hypertension. N. Engl. J. Med. 2010, 362, 2102–2112. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Curhan, G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation 2007, 116, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.M.; Huang, Y.Q.; Zhang, X.Y.; Tong, X.Q.; Zheng, P.F.; Shu, L. Association between dietary patterns and prediabetes risk in a middle-aged Chinese population. Nutr. J. 2020, 19, 77. [Google Scholar] [CrossRef]
- Park, S.Y.; Murphy, S.P.; Wilkens, L.R.; Yamamoto, J.F.; Sharma, S.; Hankin, J.H.; Henderson, B.E.; Kolonel, L.N. Dietary patterns using the Food Guide Pyramid groups are associated with sociodemographic and lifestyle factors: The multiethnic cohort study. J. Nutr. 2005, 135, 843–849. [Google Scholar] [CrossRef]
- Zheng, P.F.; Shu, L.; Zhang, X.Y.; Si, C.J.; Yu, X.L.; Gao, W.; Tong, X.-Q.; Zhang, L. Association between dietary patterns and the risk of hypertension among Chinese: A cross-sectional study. Nutrients 2016, 8, 239. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; He, Y.; Li, Y.; Luan, D.; Yang, X.; Zhai, F.; Ma, G. Dietary patterns and hypertension among Chinese adults: A nationally representative cross-sectional study. BMC Public Health 2011, 11, 925. [Google Scholar] [CrossRef]
- Ruan, Y.; Huang, Y.; Zhang, Q.; Qin, S.; Du, X.; Sun, Y. Association between dietary patterns and hypertension among Han and multi-ethnic population in southwest China. BMC Public Health 2018, 18, 1106. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.H.; Ning, G. Contents and methods of chronic disease surveillance project in China in 2010. Chin. J. Prev. Med. 2012, 46, 477–479. [Google Scholar]
- China Obesity Working Group. Prevention and control of overweight and obesity in Chinese adults. Preparation guide (excerpt). J. Nutr. 2004, 26, 1–4. [Google Scholar]
- Hu, F.B.; Rimm, E.; Smith-Warner, S.A.; Feskanich, D.; Stampfer, M.J.; Ascherio, A.; Sampson, L.; Willett, W.C. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am. J. Clin. Nutr. 1999, 69, 243–249. [Google Scholar] [CrossRef]
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Blanco Mejia, S.; Rahelić, D.; Kahleová, H.; Salas-Salvado, J.; Kendall, C.W.; Sievenpiper, J.L. DASH dietary pattern and cardiometabolic outcomes: An umbrella review of systematic reviews and meta-analyses. Nutrients 2019, 11, 338. [Google Scholar] [CrossRef]
- Chen, P.; He, G.; Zou, X.; Zhang, X.; Li, J.; Wang, Z.; Gao, H.; Luo, L.; Zhang, Z.; Yu, J.; et al. Genetic diversities and phylogenetic analyses of three Chinese main ethnic groups in southwest China: A Y-Chromosomal STR study. Sci. Rep. 2018, 8. [Google Scholar] [CrossRef]
- Wang, X.; Liu, A.; Du, M.; Wu, J.; Wang, W.; Qian, Y.; Zheng, H.; Liu, D.; Nan, X.; Jia, L.; et al. Diet quality is associated with reduced risk of hypertension among Inner Mongolia adults in northern China. Public Health Nutr. 2020, 23, 1543–1554. [Google Scholar] [CrossRef]
- Du, S.F.; Wang, H.J.; Zhang, B.; Zhai, F.Y.; Popkin, B.M. China in the period of transition from scarcity and extensive undernutrition to emerging nutrition-related non-communicable diseases, 1949–1992. Obes. Rev. 2014, 15, 8–15. [Google Scholar] [CrossRef]
- Zhai, F.; Fu, D.; Du, S.; Ge, K.; Chen, C.; Popkin, B.M. What is China doing in policy-making to push back the negative aspects of the nutrition transition? Public Health Nutr. 2002, 5, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Xue, B.; Yu, Y.; Zhang, Z.; Guo, F.; Beltz, T.G.; Thunhorst, R.L.; Felder, R.B.; Johnson, A.K. Leptin mediates high-fat diet sensitization of angiotensin II-elicited hypertension by upregulating the brain renin-angiotensin system and inflammation. Hypertension 2016, 67, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.Y.; Kim, M.K.; Lee, M.; Kim, Y.O. Macronutrient composition and sodium intake of diet are associated with risk of metabolic syndrome and hypertension in Korean women. PLoS ONE 2013, 8, e78088. [Google Scholar] [CrossRef] [PubMed]
- Majane, O.H.; Vengethasamy, L.; du Toit, E.F.; Makaula, S.; Woodiwiss, A.J.; Norton, G.R. Dietary-induced obesity hastens the progression from concentric cardiac hypertrophy to pump dysfunction in spontaneously hypertensive rats. Hypertension 2009, 54, 1376–1383. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stanley, W.C.; Shah, K.B.; Essop, M.F. Does junk food lead to heart failure? Importance of dietary macronutrient composition in hypertension. Hypertension 2009, 54, 1209–1210. [Google Scholar] [CrossRef]
- Tovar, J.; Nilsson, A.; Johansson, M.; Björck, I. Combining functional features of whole-grain barley and legumes for dietary reduction of cardiometabolic risk: A randomised cross-over intervention in mature women. Br. J. Nutr. 2014, 111, 706–714. [Google Scholar] [CrossRef]
- Borneo, R.; León, A.E. Whole grain cereals: Functional components and health benefits. Food Funct. 2012, 3, 110–119. [Google Scholar] [CrossRef]
- Villegas, R.; Gao, Y.T.; Yang, G.; Li, H.L.; Elasy, T.A.; Zheng, W.; Shu, X.O. Legume and soy food intake and the incidence of type 2 diabetes in the Shanghai Women’s Health Study. Am. J. Clin. Nutr. 2008, 87, 162–167. [Google Scholar] [CrossRef]
- Aleixandre, A.; Miguel, M. Dietary fiber and blood pressure control. Food Funct. 2016, 7, 1864–1871. [Google Scholar] [CrossRef]
- Bain, L.K.; Myint, P.K.; Jennings, A.; Lentjes, M.A.; Luben, R.N.; Khaw, K.T.; Wareham, N.J.; Welch, A.A. The relationship between dietary magnesium intake, stroke and its major risk factors, blood pressure and cholesterol, in the EPIC-Norfolk cohort. Int. J. Cardiol. 2015, 196, 108–114. [Google Scholar] [CrossRef]
- Jenkins, D.J.; Kendall, C.W.; Vuksan, V.; Faulkner, D.; Augustin, L.S.; Mitchell, S.; Ireland, C.; Srichaikul, K.; Mirrahimi, A.; Chiavaroli, L.; et al. Effect of lowering the glycemic load with canola oil on glycemic control and cardiovascular risk factors: A randomized controlled trial. Diabetes Care 2014, 37, 1806–1814. [Google Scholar] [CrossRef] [PubMed]
- Sijtsma, F.P.; Meyer, K.A.; Steffen, L.M.; Van Horn, L.; Shikany, J.M.; Odegaard, A.O.; Gross, M.D.; Kromhout, D.; Jacobs, D.R., Jr. Diet quality and markers of endothelial function: The CARDIA study. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Steffen, L.M.; Jacobs, D.R., Jr.; Murtaugh, M.A.; Moran, A.; Steinberger, J.; Hong, C.P.; Sinaiko, A.R. Whole grain intake is associated with lower body mass and greater insulin sensitivity among adolescents. Am. J. Epidemiol. 2003, 158, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, J. Association between fruit and vegetable consumption and risk of hypertension in middle-aged and older Korean adults. J. Acad. Nutr. Diet. 2018, 118, 1438–1449.e5. [Google Scholar] [CrossRef]
- Tang, O.; Miller, E.R.; Gelber, A.C.; Choi, H.K.; Appel, L.J.; Juraschek, S.P. DASH diet and change in serum uric acid over time. Clin. Rheumatol. 2017, 36, 1413–1417. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total | Non-HTN | New HTN | p-Value |
|---|---|---|---|---|
| Participants, n | 5442 | 4265 | 1177 | |
| Age, years | <0.001 | |||
| 18.0–34.9 | 3267 (60.0) | 2739 (64.2) | 528 (44.9) | |
| 35.0–49.9 | 1542 (28.3) | 1119 (26.2) | 423 (35.9) | |
| ≥50.0 | 633 (11.6) | 407 (9.5) | 226 (19.2) | |
| Women, % | 2970 (54.6) | 2357 (55.3) | 613 (52.1) | 0.056 |
| Han Chinese, % | 3096 (56.9) | 2397 (56.2) | 699 (59.4) | 0.055 |
| Education > 9 years, % | 2453 (45.1) | 2020 (47.4) | 433 (36.8) | <0.001 |
| Married, % | 4380 (80.5) | 3404 (79.8) | 976 (82.9) | 0.019 |
| Farmer, % | 3111 (57.2) | 2373 (55.6) | 738 (62.7) | <0.001 |
| Current smoker, % | 1484 (27.3) | 1128 (26.4) | 356 (30.2) | 0.011 |
| Alcohol use, % | 1691 (31.1) | 1324 (31.0) | 367 (31.2) | 0.956 |
| Physical activity, % | 4717 (86.7) | 3695 (86.6) | 1022 (86.8) | 0.899 |
| HTN family history, % | 522 (9.6) | 421 (9.9) | 101 (8.6) | 0.203 |
| BMI, kg/m2 | 0.001 | |||
| <22.0 | 357 (6.6) | 290 (6.8) | 67 (5.7) | |
| 22.0–23.9 | 3585 (66.0) | 2844 (66.8) | 741 (63.1) | |
| 24.0–27.9 | 1233 (22.7) | 942 (22.1) | 291 (24.8) | |
| ≥28.0 | 257 (4.7) | 181 (4.3) | 76 (6.5) |
| Characteristics | Junk Food Pattern | Vegetable–Grain Pattern | ||||||
|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | p-Value | Low | Medium | High | p-Value | |
| Participants, n | 1814 | 1814 | 1814 | 1814 | 1814 | 1814 | ||
| Age, years | <0.001 | <0.001 | ||||||
| 18.0–34.9 | 1013 (31.0) | 1032 (31.6) | 1222 (37.4) | 985 (30.1) | 1141 (34.9) | 1141 (34.9) | ||
| 35.0–49.9 | 553 (35.9) | 551 (35.7) | 438 (28.4) | 537 (34.8) | 500 (32.4) | 505 (32.7) | ||
| ≥50.0 | 248 (39.2) | 231 (36.5) | 154 (24.3) | 292 (46.1) | 173 (27.3) | 168 (26.5) | ||
| Gender | 0.101 | <0.001 | ||||||
| Women | 953 (32.1) | 1011 (34.0) | 1006 (33.9) | 1096 (36.9) | 980 (33.0) | 894 (30.1) | ||
| Men | 861 (34.8) | 803 (32.5) | 808 (32.7) | 718 (29.0) | 834 (33.7) | 920 (37.2) | ||
| Han Chinese | <0.001 | <0.001 | ||||||
| Yes | 832 (26.9) | 982 (31.7) | 1282 (41.4) | 1206 (39.0) | 1021 (33.0) | 869 (28.1) | ||
| No | 982 (41.9) | 832 (35.5) | 532 (22.7) | 608 (25.9) | 793 (33.8) | 945 (40.3) | ||
| Education years | <0.001 | 0.001 | ||||||
| >9 | 608 (24.8) | 729 (29.7) | 1116 (45.5) | 772 (31.5) | 799 (32.6) | 882 (36.0) | ||
| ≤9 | 1206 (40.3) | 1085 (36.3) | 698 (23.4) | 1042 (34.9) | 1015 (34.0) | 932 (31.2) | ||
| Married | <0.001 | 0.677 | ||||||
| Yes | 1480 (33.8) | 1512 (34.5) | 1388 (31.7) | 1449 (33.1) | 1470 (33.6) | 1461 (33.4) | ||
| No | 334 (31.5) | 302 (28.4) | 426 (40.1) | 365 (34.4) | 344 (32.4) | 353 (33.2) | ||
| Farmers | <0.001 | <0.001 | ||||||
| Yes | 1236 (39.7) | 1082 (34.8) | 793 (25.5) | 974 (31.3) | 1093 (35.1) | 1044 (33.6) | ||
| No | 578 (24.8) | 732 (31.4) | 1021 (43.8) | 840 (36.0) | 721 (30.9) | 770 (33.0) | ||
| Current smoker | <0.001 | <0.001 | ||||||
| Yes | 437 (29.4) | 493 (33.2) | 554 (37.3) | 439 (29.6) | 502 (33.8) | 543 (36.6) | ||
| No | 1377 (34.8) | 1321 (33.4) | 1260 (31.8) | 1375 (34.7) | 1312 (33.1) | 1271 (32.1) | ||
| Alcohol use | <0.001 | <0.001 | ||||||
| Yes | 519 (30.7) | 530 (31.3) | 642 (38.0) | 472 (27.9) | 595 (35.2) | 624 (36.9) | ||
| No | 1295 (34.5) | 1284 (34.2) | 1172 (31.2) | 1342 (35.8) | 1219 (32.5) | 1190 (31.7) | ||
| Physical activity | <0.001 | 0.267 | ||||||
| Yes | 1513 (32.1) | 1552 (32.9) | 1652 (35.0) | 1570 (33.3) | 1557 (33.0) | 1590 (33.7) | ||
| No | 301 (41.5) | 262 (36.1) | 162 (22.3) | 244 (33.7) | 257 (35.4) | 224 (30.9) | ||
| HTN family history, % | <0.001 | 0.629 | ||||||
| Yes | 107 (20.5) | 158 (30.3) | 257 (49.2) | 166 (31.8) | 183 (35.1) | 173 (33.1) | ||
| No | 1707 (34.7) | 1656 (33.7) | 1557 (31.6) | 1648 (33.5) | 1631 (33.2) | 1641 (33.4) | ||
| BMI, kg/m2 | 0.013 | 0.444 | ||||||
| <22.0 | 117 (32.8) | 124 (34.7) | 116 (32.5) | 123 (34.5) | 134 (37.5) | 100 (28.0) | ||
| 22.0–23.9 | 1254 (35.0) | 1169 (32.6) | 1162 (32.4) | 1190 (33.2) | 1181 (32.9) | 1214 (33.9) | ||
| 24.0–27.9 | 370 (30.0) | 428 (34.7) | 435 (35.3) | 410 (33.3) | 414 (33.6) | 409 (33.2) | ||
| ≥28.0 | 70 (27.2) | 87 (33.9) | 100 (38.9) | 87 (33.9) | 82 (31.9) | 88 (34.2) | ||
| Cases, n | Incident Density/1000 PYs | HR (95% CI) | |||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||
| Junk food pattern | |||||
| Low | 376 | 29.52 | 0.783 (0.682, 0.899) *** | 0.771 (0.671, 0.886) *** | 0.772 (0.671, 0.887) *** |
| Medium | 435 | 34.60 | 1.000 | 1.000 | 1.000 |
| High | 366 | 34.00 | 0.865 (0.752, 0.994) * | 0.917 (0.794, 1.060) | 0.895 (0.775, 1.030) |
| Vegetable and grain pattern | |||||
| Low | 416 | 33.11 | 0.964 (0.842, 1.100) | 0.986 (0.860, 1.130) | 0.990 (0.864, 1.140) |
| Medium | 438 | 34.26 | 1.000 | 1.000 | 1.000 |
| High | 323 | 25.67 | 0.762 (0.660, 0.880) *** | 0.775 (0.670, 0.895) *** | 0.774 (0.669, 0.894) *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Wang, Y.; Chen, Y.; Zhou, J.; Xu, L.; Xu, K.; Wang, N.; Fu, C.; Liu, T. Associations of Dietary Patterns and Risk of Hypertension in Southwest China: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 12378. https://doi.org/10.3390/ijerph182312378
Zhang Y, Wang Y, Chen Y, Zhou J, Xu L, Xu K, Wang N, Fu C, Liu T. Associations of Dietary Patterns and Risk of Hypertension in Southwest China: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(23):12378. https://doi.org/10.3390/ijerph182312378
Chicago/Turabian StyleZhang, Yixia, Yanhuan Wang, Yun Chen, Jie Zhou, Lina Xu, Kelin Xu, Na Wang, Chaowei Fu, and Tao Liu. 2021. "Associations of Dietary Patterns and Risk of Hypertension in Southwest China: A Prospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 23: 12378. https://doi.org/10.3390/ijerph182312378
APA StyleZhang, Y., Wang, Y., Chen, Y., Zhou, J., Xu, L., Xu, K., Wang, N., Fu, C., & Liu, T. (2021). Associations of Dietary Patterns and Risk of Hypertension in Southwest China: A Prospective Cohort Study. International Journal of Environmental Research and Public Health, 18(23), 12378. https://doi.org/10.3390/ijerph182312378






