The Prevalence of Myopia in Children in Spain: An Updated Study in 2020
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Inclusion and Exclusion Criteria
2.4. Clinical Procedure
- (1)
- Best corrected and uncorrected visual acuity.
- (2)
- Objective refraction: non-cycloplegic retinoscopy (differences of ±0.5D were estimated in the spherical equivalent compared to the non-cycloplegic refraction) [16].
- (3)
- Subjective refraction.
- (4)
- Binocular vision and accommodation tests: Cover–uncover alternating cover, ocular motility, Hirschberg test, Worth test, near point of convergence, amplitude of accommodation, stereopsis, and colour vision.
- (5)
- Finally, the anterior segment (eyelid, eyelashes, lid margin, cornea, conjunctiva, and lens) was reviewed using a slit lamp.
2.5. Definition of Variables
2.6. Statistical Analysis
3. Results
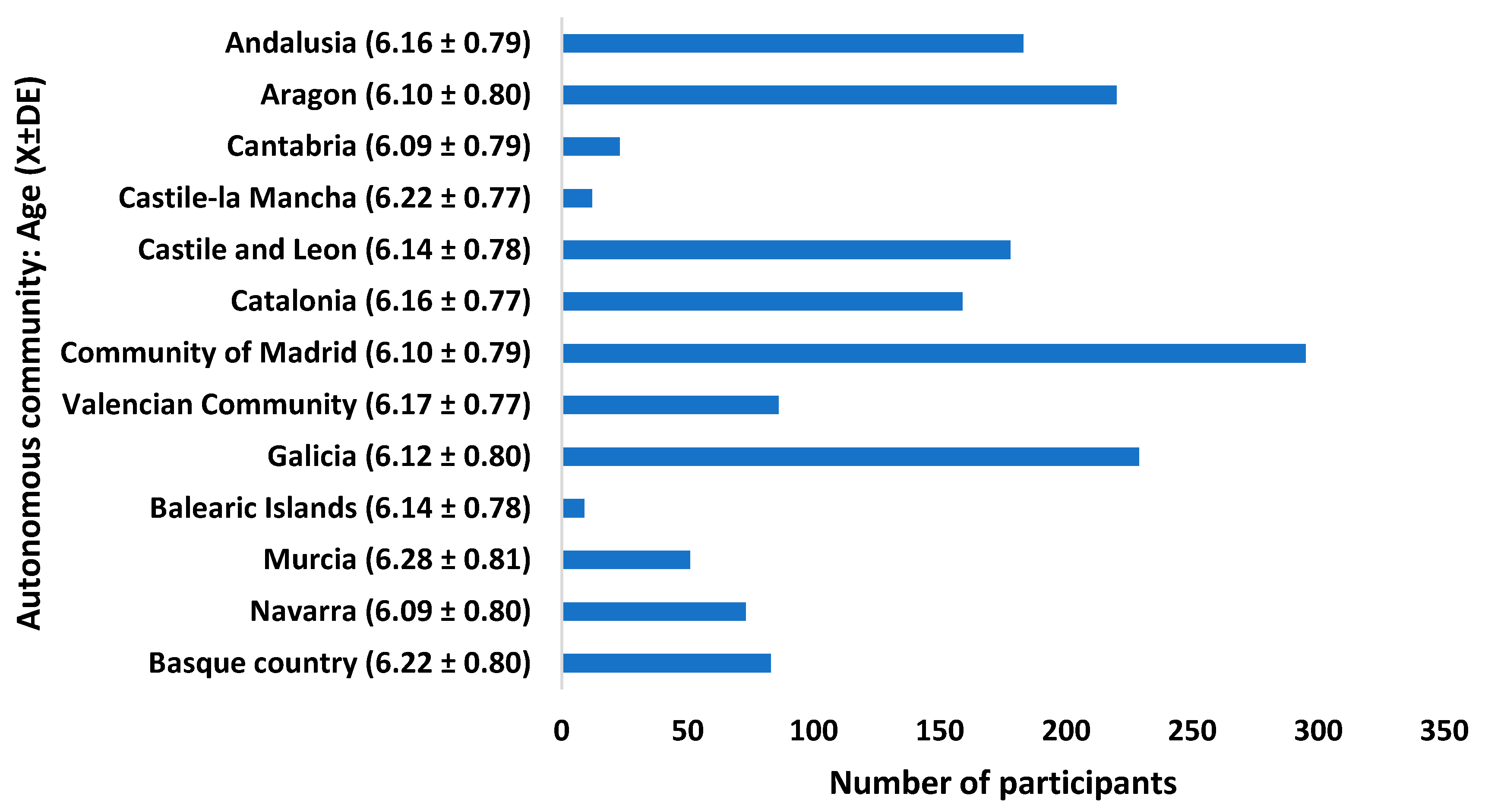
3.1. Demography
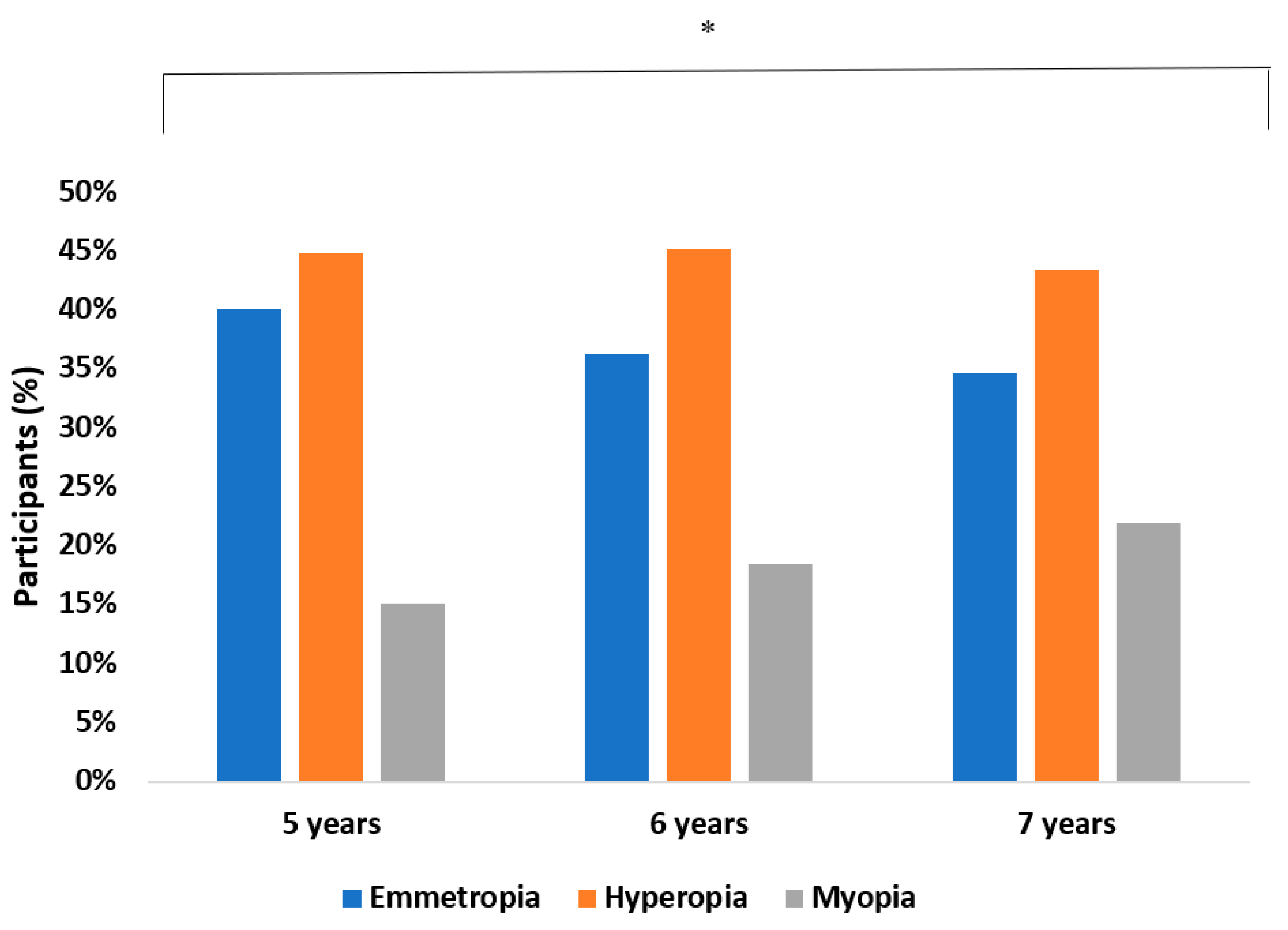
3.2. Prevalence Results
3.2.1. Distribution of the Mean Value of the Spherical Equivalent
3.2.2. Degree of Myopia
3.3. Risk Factor Results
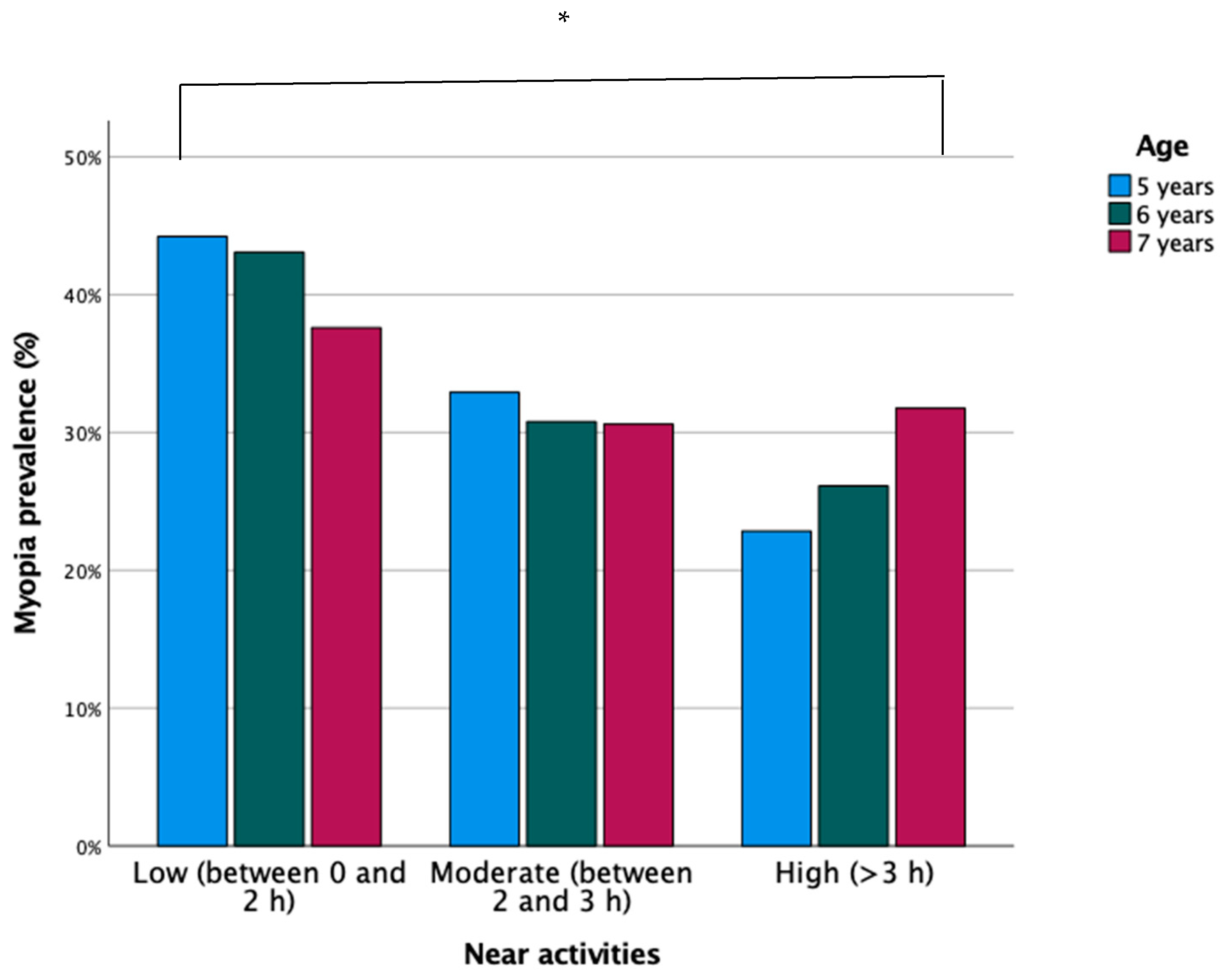
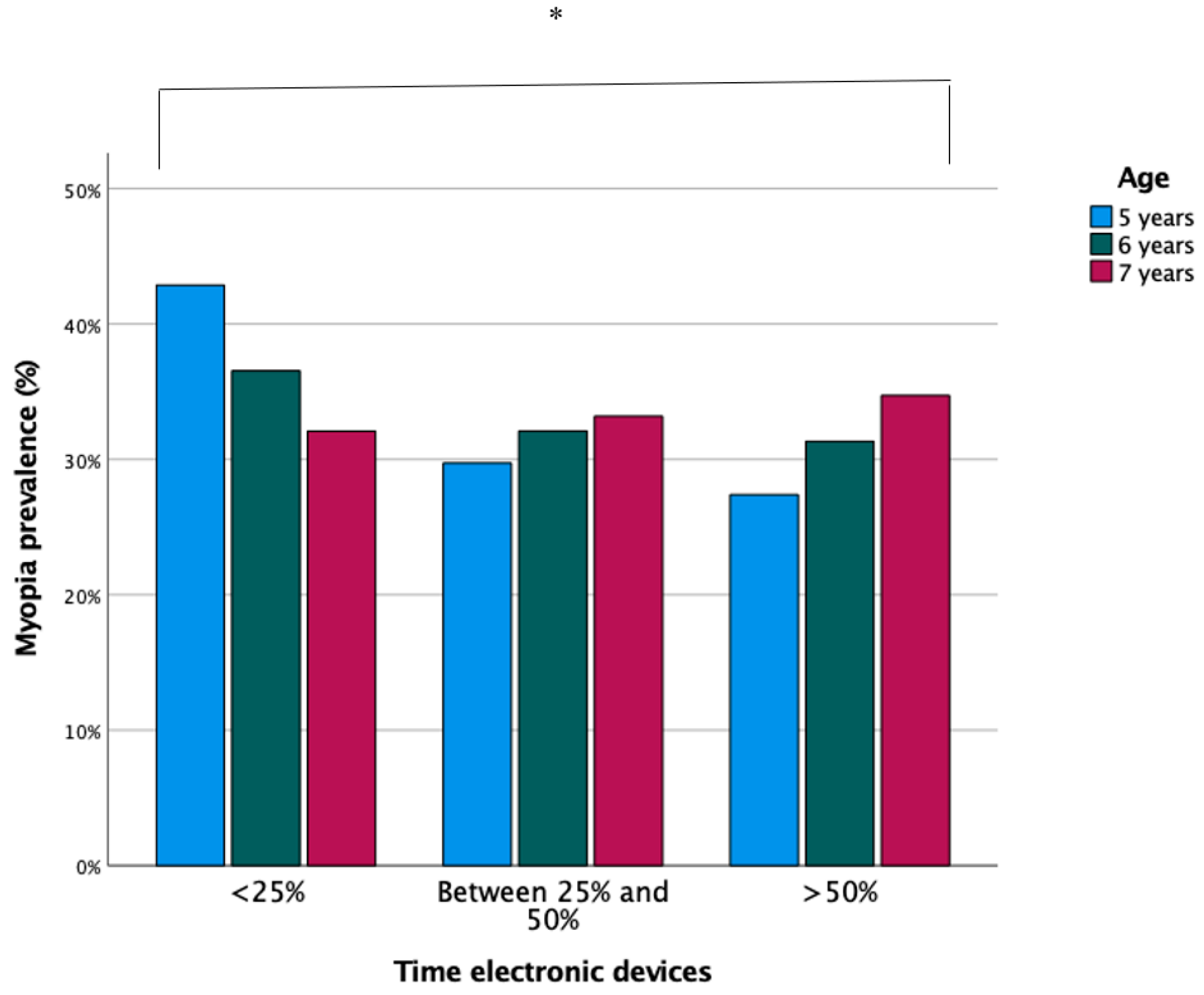
3.3.1. Near-Vision Activities and the Use of Digital Devices
3.3.2. Family Background
3.4. Protection Factor Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chua, J.; Wong, T.Y. Myopia-the silent epidemic that should not be ignored. JAMA Ophthalmol. 2016, 134, 1363–1364. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rudnicka, A.R.; Kapetanakis, V.V.; Wathern, A.K.; Logan, N.S.; Gilmartin, B.; Whincup, P.H.; Cook, D.G.; Owen, C.G. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: Implications for aetiology and early prevention. Br. J. Ophthalmol. 2016, 100, 882–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bourne, R.R.; Stevens, G.A.; White, R.A.; Smith, J.L.; Flaxman, S.R.; Price, H.; Jonas, J.B.; Keeffe, J.; Leasher, J.; Naidoo, K.; et al. Causes of vision loss worldwide, 1990-2010: A systematic analysis. Lancet Glob. Health 2013, 1, e339–e349. [Google Scholar] [CrossRef] [Green Version]
- Tricard, D.; Marillet, S.; Ingrand, P.; Bullimore, M.A.; Bourne, R.R.A.; Leveziel, N. Progression of myopia in children and teenagers: A nationwide longitudinal study. Br. J. Ophthalmol. 2021. [Google Scholar] [CrossRef]
- Wang, J.; Li, Y.; Musch, D.C.; Wei, N.; Qi, X.; Ding, G.; Li, X.; Li, J.; Song, L.; Zhang, Y.; et al. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA Ophthalmol. 2021, 139, 293–300. [Google Scholar] [CrossRef]
- Choy, B.N.K.; You, Q.; Zhu, M.M.; Lai, J.S.M.; Ng, A.L.K.; Wong, I.Y.H. Prevalence and associations of myopia in Hong Kong primary school students. Jpn. J. Ophthalmol. 2020, 64, 437–449. [Google Scholar] [CrossRef]
- Jan, C.; Li, S.M.; Kang, M.T.; Liu, L.; Li, H.; Jin, L.; Qin, X.; Congdon, N.; Wang, N. Association of visual acuity with educational outcomes: A prospective cohort study. Br. J. Ophthalmol. 2019, 103, 1666–1671. [Google Scholar] [CrossRef] [Green Version]
- Varma, R.; Tarczy-Hornoch, K.; Jiang, X. Visual impairment in preschool children in the United States: Demographic and geographic variations from 2015 to 2060. JAMA Ophthalmol. 2017, 135, 610–616. [Google Scholar] [CrossRef]
- Hashemi, H.; Fotouhi, A.; Yekta, A.; Pakzad, R.; Ostadimoghaddam, H.; Khabazkhoob, M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J. Curr. Ophthalmol. 2017, 30, 3–22. [Google Scholar] [CrossRef]
- Logan, N.S.; Shah, P.; Rudnicka, A.R.; Gilmartin, B.; Owen, C.G. Childhood ethnic differences in ametropia and ocular biometry: The Aston Eye Study. Ophthalmic Physiol. Opt. 2011, 31, 550–558. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, L.; Kapetanankis, V.V.; McClelland, J.F.; Logan, N.S.; Owen, C.G.; Saunders, K.J.; Rudnicka, A.R. Risk Factors for Childhood Myopia: Findings From the NICER Study. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1524–1530. [Google Scholar] [CrossRef] [PubMed]
- Tideman, J.W.L.; Polling, J.R.; Hofman, A.; Jaddoe, V.W.; Mackenbach, J.P.; Klaver, C.C. Environmental factors explain socioeconomic prevalence differences in myopia in 6-year-old children. Br. J. Ophthalmol. 2018, 102, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Czepita, D.; Zejmo, M.; Mojsa, A. Prevalence of myopia and hyperopia in a population of polish school children. Ophthalmic Physiol. Opt. 2007, 27, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Peregrina, C.; Sanchez-Tena, M.A.; Martinez-Perez, C.; Villa-Collar, C. Prevalence and Risk Factors of Myopia in Spain. J. Ophthalmol. 2019, 2019, 3419576. [Google Scholar] [CrossRef] [PubMed]
- Khurana, R.; Tibrewal, S.; Ganesh, S.; Tarkar, R.; Nguyen, P.T.T.; Siddiqui, Z.; Dasgupta, S. Accuracy of noncycloplegic refraction performed at school screening camps. Indian J. Ophthalmol. 2018, 66, 806–811. [Google Scholar] [CrossRef] [PubMed]
- American Optometric Association. Care of the Patient with Myopia; American Optometric Association: St. Louis, MO, USA, 2018. [Google Scholar]
- Myopia Profile: An Information Resource for Optometrists. Available online: https://www.myopiaprofile.com/store/ (accessed on 5 February 2021).
- Montés-Micó, R.; Ferrer-Blasco, T. Distribution of refractive errors in Spain. Doc. Ophthalmol. 2000, 101, 25–33. [Google Scholar] [CrossRef]
- Antón, A.; Andrada, M.T.; Mayo, A.; Portela, J.; Merayo, J. Epidemiology of refractive errors in an adult European population: The Segovia study. Ophthalmic Epidemiol. 2009, 16, 231–237. [Google Scholar] [CrossRef]
- French, A.N.; Morgan, I.G.; Mitchell, P.; Rose, K.A. Risk factors for incident myopia in Australian schoolchildren: The Sydney adolescent vascular and eye study. Ophthalmology 2013, 120, 2100–2108. [Google Scholar] [CrossRef]
- Theophanous, C.; Modjtahedi, B.S.; Batech, M.; Marlin, D.S.; Luong, T.Q.; Fong, D.S. Myopia prevalence and risk factors in children. Clin. Ophthalmol. 2018, 12, 1581–1587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matamoros, E.; Ingrand, P.; Pelen, F.; Bentaleb, Y.; Weber, M.; Korobelnik, J.F.; Souied, E.; Leveziel, N. Prevalence of Myopia in France: A Cross-Sectional Analysis. Medicine 2015, 94, e1976. [Google Scholar] [CrossRef] [PubMed]
- Kumah, B.D.; Ebri, A.; Abdul-Kabir, M.; Ahmed, A.S.; Koomson, N.Y.; Aikins, S.; Aikins, A.; Amedo, A.; Lartey, S.; Naidoo, K. Refractive error and visual impairment in private school children in Ghana. Optom. Vis. Sci. 2013, 90, 1456–1461. [Google Scholar] [CrossRef] [Green Version]
- Lira, R.P.; Arieta, C.E.; Passos, T.H.; Maziero, D.; Astur, G.L.; do Espírito Santo, Í.F.; Bertolani, A.C.; Pozzi, L.F.; de Castro, R.S.; Ferraz, Á.A. Distribution of Ocular Component Measures and Refraction in Brazilian School Children. Ophthalmic Epidemiol. 2017, 24, 29–35. [Google Scholar] [CrossRef]
- Galvis, V.; Tello, A.; Otero, J.; Serrano, A.A.; Gómez, L.M.; Castellanos, Y. Refractive errors in children and adolescents in Bucaramanga (Colombia). Arq. Bras. Oftalmol. 2017, 80, 359–363. [Google Scholar] [CrossRef]
- Fredrick, D.R. Myopia. BMJ 2002, 324, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Németh, J.; Tapasztó, B.; Aclimandos, W.A.; Kestelyn, P.; Jonas, J.B.; De Faber, J.H.N.; Januleviciene, I.; Grzybowski, A.; Nagy, Z.Z.; Pärssinen, O.; et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur. J. Ophthalmol. 2021, 31, 853–883. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Calossi, A.; Cho, P.; Gifford, K.; Jones, L.; Jones, D.; Guthrie, S.; Li, M.; Lipener, C.; Logan, N.S.; et al. Global trends in myopia management attitudes and strategies in clinical practice—2019 Update. Cont. Lens Anterior Eye 2020, 43, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.; Ellwein, L.; Cotch, M.F.; Ferris, F.L., 3rd; Sperduto, R. Prevalence of refractive error in the United States, 1999–2004. Arch. Ophthalmol. 2008, 126, 1111–1119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fledelius, H.C. Myopia profile in Copenhagen medical students 1996-98. Refractive stability over a century is suggested. Acta Ophthalmol. Scand. 2000, 78, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Otawa, U.C.; Munsamy, A.J.; Wajuihian, S.O. Prevalence and risk factors for myopia among school children in Aba, Nigeria. Afr. Vis. Eye Health 2017, 76, a369. [Google Scholar]
- COMET Group. Myopia stabilization and associated factors among participants in the correction of myopia evaluation trial (COMET). Investig. Ophthalmol. Vis. Sci. 2013, 54, 7871–7884. [Google Scholar] [CrossRef] [Green Version]
- Lin, Z.; Vasudevan, B.; Jhanji, V.; Mao, G.Y.; Gao, T.Y.; Wang, F.H.; Rong, S.S.; Ciuffreda, K.J.; Liang, Y.B. Near work, outdoor activity, and their association with refractive error. Optom. Vis. Sci. 2014, 91, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Enthoven, C.A.; Tideman, J.W.L.; Polling, J.R.; Yang-Huang, J.; Raat, H.; Klaver, C.C.W. The impact of computer use on myopia development in childhood: The Generation R study. Prev. Med. 2020, 132, 105988. [Google Scholar] [CrossRef] [PubMed]
- Grzybowski, A.; Kanclerz, P.; Tsubota, K.; Lanca, C.; Saw, S.M. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020, 20, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.M.; Li, S.Y.; Kang, M.T.; Zhou, Y.; Liu, L.R.; Li, H.; Wang, Y.P.; Zhan, S.Y.; Gopinath, B.; Mitchell, P.; et al. Near Work Related Parameters and Myopia in Chinese Children: The Anyang Childhood Eye Study. PLoS ONE 2015, 10, e0134514. [Google Scholar] [CrossRef]
- Lu, B.; Congdon, N.; Liu, X.; Choi, K.; Lam, D.S.; Zhang, M.; Zheng, M.; Zhou, Z.; Li, L.; Liu, X.; et al. Associations between near work, outdoor activity, and myopia among adolescent students in rural China: The Xichang Pediatric Refractive Error Study report no. 2. Arch. Ophthalmol. 2009, 127, 769–775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones-Jordan, L.A.; Mitchell, G.L.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Mutti, D.O.; Twelker, J.D.; Sims, J.R.; Zadnik, K.; CLEERE Study Group. Visual activity before and after the onset of juvenile myopia. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1841–1850. [Google Scholar] [CrossRef] [PubMed]
- Yam, J.C.; Tang, S.M.; Kam, K.W.; Chen, L.J.; Yu, M.; Law, A.K.; Yip, B.H.; Wang, Y.M.; Cheung, C.Y.L.; Ng, D.S.C.; et al. High prevalence of myopia in children and their parents in Hong Kong Chinese Population: The Hong Kong Children Eye Study. Acta Ophthalmol. 2020, 98, e639–e648. [Google Scholar] [CrossRef] [PubMed]
- Jiang, D.; Lin, H.; Li, C.; Liu, L.; Xiao, H.; Lin, Y.; Huang, X.; Chen, Y. Longitudinal association between myopia and parental myopia and outdoor time among students in Wenzhou: A 2.5-year longitudinal cohort study. BMC Ophthalmol. 2021, 21, 11. [Google Scholar] [CrossRef]
- Deng, L.; Pang, Y. Effect of Outdoor Activities in Myopia Control: Meta-analysis of Clinical Studies. Optom. Vis. Sci. 2019, 96, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Lingham, G.; Yazar, S.; Lucas, R.M.; Milne, E.; Hewitt, A.W.; Hammond, C.J.; MacGregor, S.; Rose, K.A.; Chen, F.K.; He, M.; et al. Time spent outdoors in childhood is associated with reduced risk of myopia as an adult. Sci. Rep. 2021, 11, 6337. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Yang, L.; Lu, B.; Wang, H.; Xu, T.; Du, D.; Wu, S.; Li, X.; Lu, M. Association between parents’ attitudes and behaviors toward children’s visual care and myopia risk in school-aged children. Medicine 2017, 96, e9270. [Google Scholar] [CrossRef] [PubMed]

| Gender | Age | Degree of Myopia | ||
|---|---|---|---|---|
| Low n (%) | Moderate n (%) | High n (%) | ||
| Female | 5 | 21 (16.2) | 4 (33.3) | 0 (0.0) |
| 6 | 49 (37.7) | 4 (33.3) | 1 (50.0) | |
| 7 | 60 (46.2) | 4 (33.3) | 1 (50.0) | |
| Total | 130 (100.0) | 12 (100.0) | 2 (100.0) | |
| Masculine | 5 | 25 (17.1) | 4 (25.0) | 2 (40.0) |
| 6 | 60 (41.1) | 2 (12.5) | 0 (0.0) | |
| 7 | 61 (41.8) | 10 (62.5) | 3 (60.0) | |
| Total | 146 (100.0) | 16 (100.0) | 5 (100.0) | |
| Total | 5 | 46 (16.7) | 8 (28.6) | 2 (28.6) |
| 6 | 109 (39.5) | 6 (21.4) | 1 (14.3) | |
| 7 | 121 (43.8) | 14 (50.0) | 4 (57.1) | |
| Total | 276 (100.0) | 28 (100.0) | 7 (100.0) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alvarez-Peregrina, C.; Martinez-Perez, C.; Villa-Collar, C.; González-Pérez, M.; González-Abad, A.; Sánchez-Tena, M.Á.; on behalf of Grupo de Investigación Alain Afflelou. The Prevalence of Myopia in Children in Spain: An Updated Study in 2020. Int. J. Environ. Res. Public Health 2021, 18, 12375. https://doi.org/10.3390/ijerph182312375
Alvarez-Peregrina C, Martinez-Perez C, Villa-Collar C, González-Pérez M, González-Abad A, Sánchez-Tena MÁ, on behalf of Grupo de Investigación Alain Afflelou. The Prevalence of Myopia in Children in Spain: An Updated Study in 2020. International Journal of Environmental Research and Public Health. 2021; 18(23):12375. https://doi.org/10.3390/ijerph182312375
Chicago/Turabian StyleAlvarez-Peregrina, Cristina, Clara Martinez-Perez, Cesar Villa-Collar, Mariano González-Pérez, Ana González-Abad, Miguel Ángel Sánchez-Tena, and on behalf of Grupo de Investigación Alain Afflelou. 2021. "The Prevalence of Myopia in Children in Spain: An Updated Study in 2020" International Journal of Environmental Research and Public Health 18, no. 23: 12375. https://doi.org/10.3390/ijerph182312375
APA StyleAlvarez-Peregrina, C., Martinez-Perez, C., Villa-Collar, C., González-Pérez, M., González-Abad, A., Sánchez-Tena, M. Á., & on behalf of Grupo de Investigación Alain Afflelou. (2021). The Prevalence of Myopia in Children in Spain: An Updated Study in 2020. International Journal of Environmental Research and Public Health, 18(23), 12375. https://doi.org/10.3390/ijerph182312375










