Breast Cancer Screening in Semi-Rural Malaysia: Utilisation and Barriers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Participants and Sample
2.3. Data Collection
2.3.1. Socio-Demographic Variables
2.3.2. Breast Self-Examination and Cancer Screening Practices
- BSE: Data on awareness, frequency and timing of BSE, the level of confidence and the perceived benefit of BSE were collected. Women who performed BSE at least once in their lifetime were considered ‘having ever done BSE’, while women who performed BSE at least once every month were regarded as ‘having regular BSE’.
- CBE: Information on CBE awareness was assessed by asking, “Have you heard of Clinical Breast Examination?” and utilisation of CBE was captured by asking, “Has a health care provider ever examined your breasts?” The participants were also asked if they had a CBE in the past year and the number of times they had a CBE in the past five years. At least once a year for the past five years was considered as regular CBE. Access to CBE among women who were aware of a facility was assessed as the reported time in minutes it would take the woman to travel one way to the nearest health clinic.
- Mammogram: Information on the awareness of mammograms was assessed by asking, “Have you heard of mammograms?” and utilisation of mammograms was captured by asking, “Have you ever undergone breast imaging or mammogram?” The participants were also asked if they had undergone a mammogram in the past two years. Women who had a mammogram at least once in their life were categorised as ‘having ever had a mammogram’. Those who had a mammogram in the past two years were regarded as ‘having done a recent mammogram’ [13]. Access to mammograms was assessed as the time in minutes it would take for a woman to travel one way to the nearest health clinic with a mammogram facility (among women who were aware of such a facility).
2.3.3. Perceived Benefit and Barriers
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. Socio-Demographic Characteristics
3.2. Knowledge and Attitude towards BC and Breast Help-Seeking
3.3. Awareness, Access and Utilisation of Breast Self-Examination BC Screening Practices
- BSE: As shown in Table 2, 72% of women have had BSE at least once, but only 23.2% performed BSE regularly. More than half of the women (56%) reported needing more training to perform BSE. Among women who were aware of BSE (n = 195), 86.2% perceived BSE to be beneficial.
- CBE: Among the 250 women, 133 (53.2%) were aware of CBE as a BC screening method, while only 36% had ever undergone a CBE (Table 2), and 4.4% performed CBE regularly. CBEs were conducted by doctors (72.2%) and community health nurses (27.8%). Most of the recent CBEs were completed to screen for BC (80.6%) and the remaining CBEs were related to pregnancy or other breast health issues. Only 46% of women were aware of the nearest health facility that offered CBE. The median travel time (IQR) to reach the facility was reported as 15 (20) min, and more than 25% of the women had a travel time of ≥30 min. Among the women aware of CBE, 126 (94.7%) believed that CBE was beneficial.
- Mammogram: Only 47.6% (n = 119) of women had heard of mammograms as a BC screening method, and 22.4% of women received a mammogram at least once in their lifetime (Table 2). Few participants (10.8%) received a mammogram recently. Out of these mammograms, 88.9% were done to screen for BC, and 48.1% had their mammogram in a private facility. Among women who were aware of mammograms, 95.8% reported that they believed mammogram was beneficial. Only 21.2% of the participants knew the nearest health facility that offered a mammogram. These women reported a median (IQR) time of 70 (72.5) minutes to reach the mammogram facility.
- Breast cancer screening programmes: Among all interviewed women, only 15.6% were aware of the existing mammogram subsidy offered by LPPKN and only 8% used this subsidy. Only 11.2% of women utilised any form of BC screening programme offered by NGOs.
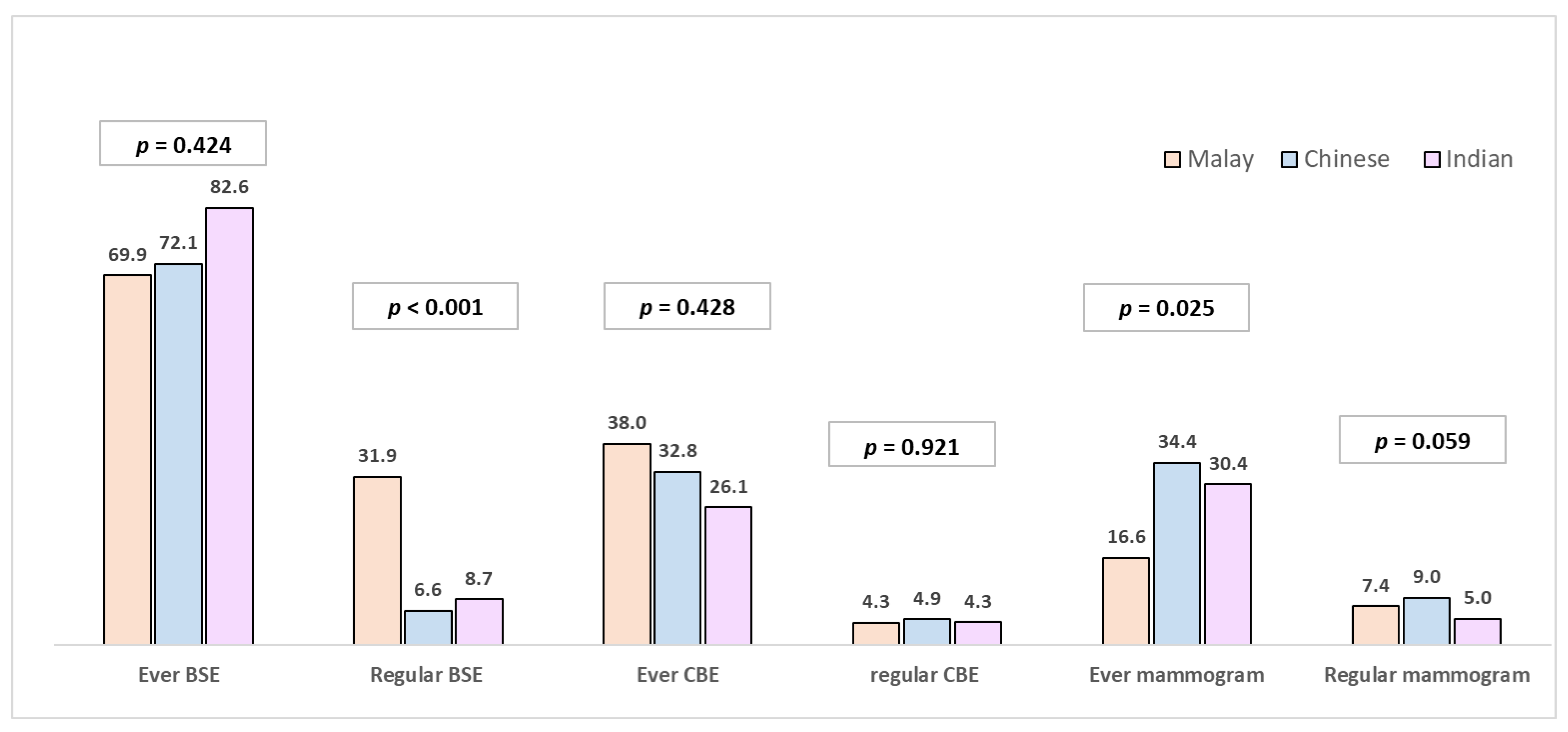
3.4. Ethnic Difference in Screening Practices
3.5. Socio-Demographic Factors Associated with Screening Practice
3.6. Barriers to BC Screening and Health-Seeking
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Institute NC. Summary of Malaysian National Cancer Registry Report (2007–2011); National Cancer Institute, National Cancer Registry Report MoH: Putrajaya, Malaysia, 2017.
- National Cancer Registry; National Cancer Institute; Ministry of Health Malaysia. Malaysian Study on Cancer Survival (MySCan); Ministry of Health Malaysia: Putrajaya, Malaysia, 2018.
- Cheng, M.L.; Ling, D.; Nanu, P.K.; Nording, H.; Lim, C.H. Factors influencing late stage of breast cancer at presentation in a district Hospital-Segamat Hospital, Johor. Med. J. Malaysia 2015, 70, 148–152. [Google Scholar] [PubMed]
- Aziah, A.; Hashimah, B.; Nirmal, K.; Siti Zubaidah, A.; Puteri, N.; Nabihah, A.; Sukumaran, R.; Balqis, B.; Nadia, S.; Sharifah, S. Malaysia National Cancer Registry Report (MNCR) 2012–2016. Natl. Cancer Regist. NCI 2019, 3, 34–37. [Google Scholar]
- Anderson, B.O.; Yip, C.H.; Smith, R.A.; Shyyan, R.; Sener, S.F.; Eniu, A.; Carlson, R.W.; Azavedo, E.; Harford, J. Guideline implementation for breast healthcare in low-income and middle-income countries: Overview of the Breast Health Global Initiative Global Summit 2007. Cancer 2008, 113, 2221–2243. [Google Scholar] [CrossRef] [PubMed]
- Mittra, I.; Mishra, G.A.; Dikshit, R.P.; Gupta, S.; Kulkarni, V.Y.; Shaikh, H.K.A.; Shastri, S.S.; Hawaldar, R.; Gupta, S.; Pramesh, C. Effect of screening by clinical breast examination on breast cancer incidence and mortality after 20 years: Prospective, cluster randomised controlled trial in Mumbai. BMJ 2021, 372, n256. [Google Scholar] [CrossRef] [PubMed]
- Board, P.A.T.E. Breast Cancer Screening (PDQ®). In PDQ Cancer Information Summaries; National Cancer Institute: Bethesda, MD, USA, 2021. [Google Scholar]
- Institute for Public Health (IPH), National Institutes of Health, Ministry of Health Malaysia. National Health and Morbidity Survey (NHMS) 2019: Vol. I: NCDs—Non-Communicable Diseases: Risk Factors and other Health Problems; Ministry of Health Malaysia: Selangor, Malaysia, 2020.
- Subramanian, P.; Oranye, N.O.; Masri, A.M.; Taib, N.A.; Ahmad, N. Breast cancer knowledge and screening behaviour among women with a positive family history: A cross sectional study. Asian Pac. J. Cancer Prev. 2013, 14, 6783–6790. [Google Scholar] [CrossRef] [PubMed]
- Nik Farid, N.D.; Abdul Aziz, N.; Al-Sadat, N.; Jamaludin, M.; Dahlui, M. Clinical breast examination as the recommended breast cancer screening modality in a rural community in Malaysia; what are the factors that could enhance its uptake? PLoS ONE 2014, 9, e106469. [Google Scholar]
- Partap, U.; Young, E.H.; Allotey, P.; Soyiri, I.N.; Jahan, N.; Komahan, K.; Devarajan, N.; Sandhu, M.S.; Reidpath, D.D. HDSS profile: The South East Asia community observatory health and demographic surveillance system (SEACO HDSS). Int. J. Epidemiol. 2017, 46, 1370g–1371g. [Google Scholar] [CrossRef] [PubMed]
- Malaysia MoH. Clinical Practice Guideline. In Management of Breast Cancer, 3rd ed.; Malaysia MoH: Putrajaya, Malaysia, 2009. [Google Scholar]
- Su, T.T.; Azzani, M.; Donnelly, M.; Majid, H.A. Seeking medical help for cancer among urban dwellers in Malaysia—Emotional barriers and awareness of cancer symptoms. Eur. J. Cancer Care 2020, 29, e13232. [Google Scholar] [CrossRef] [PubMed]
- Karim, N.K.A.; Sooi, L.K.; Mangantig, E. Factors Associated with Breast-self Examination Practice and Mammogram Breast Density among Malaysian Women. Malays. J. Med. Health Sci. 2019, 15, 96–101. [Google Scholar]
- Bhoo-Pathy, N.; Hartman, M.; Yip, C.-H.; Saxena, N.; Taib, N.A.; Lim, S.-E.; Iau, P.; Adami, H.-O.; Bulgiba, A.M.; Lee, S.-C. Ethnic differences in survival after breast cancer in South East Asia. PLoS ONE 2012, 7, e30995. [Google Scholar] [CrossRef] [PubMed]
- Family Health Development Division. Guidelines to National Breast Cancer Early Detection Program; Family Health Development Division: Selangor, Malaysia, 2011. Contract No.: MOH/K/ASA/44.11 (GU). (In Malay)
- Health MO. Annual Report, Ministry of Health Division FHD; Ministry of Health: Selangor, Malaysia, 2019. (In Malay)
- Taib, N.A.; Yip, C.H.; Low, W.Y. A grounded explanation of why women present with advanced breast cancer. World J. Surg. 2014, 38, 1676–1684. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, A.; Aljunid, S.M. Availability and accessibility of subsidised mammogram screening program in peninsular Malaysia: A preliminary study using travel impedance approach. PLoS ONE 2018, 13, e0191764. [Google Scholar] [CrossRef] [PubMed]
- Tumin, M.; Kana, G.; Ahmad Zaki, A. Financing and provision of primary health care in Malaysia. J. Adm. Sci. 2016, 13, 1–15. [Google Scholar]
- Brustrom, J.E.; Hunter, D.C. Going the distance: How far will women travel to undergo free mammography? Mil. Med. 2001, 166, 347–349. [Google Scholar] [CrossRef] [PubMed]
- Norlaili, A.A.; Fatihah, M.A.; Daliana, N.F.N.; Maznah, D. Breast cancer awareness of rural women in Malaysia: Is it the same as in the cities? Asian Pac. J. Cancer Prev. 2013, 14, 7161–7164. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Khan, T.M.; Leong, J.P.Y.; Ming, L.C.; Khan, A.H. Association of knowledge and cultural perceptions of Malaysian women with delay in diagnosis and treatment of breast cancer: A systematic review. Asian Pac. J. Cancer Prev. 2015, 16, 5349–5357. [Google Scholar] [CrossRef] [PubMed]
- Aidalina, M.; ASJ, S.M. The uptake of Mammogram screening in Malaysia and its associated factors: A systematic review. Med. J. Malaysia 2018, 73, 202–211. [Google Scholar] [PubMed]

| Characteristics | Frequency (%) |
|---|---|
| Age (in years), mean (SD) Below 60 60 and above | 59.4 (10.9) 128 (51.2) 122 (48.8) |
| Education | |
| No schooling | 24 (9.6) |
| Primary | 121 (48.4) |
| Secondary | 98 (39.2) |
| Pre-university/university | 7 (2.8) |
| Ethnicity | |
| Malay | 163 (65.2) |
| Chinese | 61 (24.4) |
| Indian | 23 (9.2) |
| Others | 3 (1.2) |
| Marital status | |
| Currently married | 170 (68) |
| Widow Separated/divorced Unmarried | 80 (32) 6 (2.4) 9 (3.6) |
| Employment status | |
| Currently working Homemaker | 36 (19.6) 188 (75.2) |
| Unemployed Retired | 13 (5.2) 13 (5.2) |
| Household income (monthly, RM) Median (IQR) (n = 221) | 1200 (875) |
| At least minimum wage # (≥RM 1000) Below minimum wage (<RM 1000) | 141 (56.4) 80 (32) |
| Family history of breast cancer | 27 (10.8) |
| A previous breast cancer diagnosis | 2 (0.8) |
| Awareness, Utilisation and Access Measures | Breast Self-Examination | Clinical Breast Examination | Mammogram |
|---|---|---|---|
| Frequency (%) | Frequency (%) | Frequency (%) | |
| Have heard about this screening | 195 (78) | 133 (53.2) | 119 (47.6) |
| Have ever had this screening | 180 (72) | 90 (36) | 56 (22.4) |
| Have undergone this screening regularly | 58 (23.2) | 11 (4.4) | 27 (10.8) a |
| Perceived benefit of this screening method b | 168 (86.2) | 126 (94.7) | 114 (95.8) |
| One-way trip length to the health facility c | (n = 115) | (n = 53) | |
| <30 min | NA | 86 (74.8) | 14 (26.4) |
| 30 min to 60 min | 24 (20.9) | 20 (37.7) | |
| >60 min | 5 (4.3) | 19 (35.8) |
| Socio-Demographic Variables | Regular BSE | CBE | Mammogram | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (Freq,%) | No (Freq,%) | p Value a | p value b Adjusted OR (95% CI) | Ever (Freq, %) | Never (Freq, %) | p value a | p value c Adjusted OR (95% CI) | Ever (Freq, %) | Never (Freq, %) | p value a | p value d Adjusted OR (95% CI) | |
| Age | 0.013 | 0.342 | 0.002 | 0.148 | ||||||||
| Below 60 | 38 (65.5) | 90 (46.9) | 58 (64.4) | 70 (43.8) | 33 (58.9) | 95 (49) | 0.189 | 0.560 | ||||
| 60+ (Ref) | 20 (34.5) | 102 (53.1) | 32 (35.6) | 90 (56.3) | 23 (41.1) | 99 (51) | ||||||
| Education | <0.001 | 0.137 | 0.003 | 0.114 | 0.009 | 0.005 0.36 (0.17, 0.74) | ||||||
| Primary and below | 21 (36.2) | 124 (64.6) | 41 (45.6) | 104 (65) | 24 (42.9) | 121 (62.4) | ||||||
| Secondary and above (Ref) | 37 (63.8) | 68 (35.4) | 49 (54.4) | 56 (35) | 32 (57.1) | 73 (37.6) | ||||||
| Ethnicity | <0.001 | 0.001 5.26 (2.05, 13.50) | 0.358 | NA | 0.002 | <0.001 0.30 (0.15–0.57) | ||||||
| Malay | 52 (89.7) | 111 (57.8) | 62 (68.9) | 101 (63.1) | 27 (48.2) | 136 (70.1) | ||||||
| Non-Malay (Ref) | 6 (10.3) | 81 (42.2) | 28 (31.1) | 59 (36.9) | 29 (51.8) | 58 (29.9) | ||||||
| Marital status | 0.143 | 0.571 | 0.001 | 0.012 2.28 (1.20, 4.31) | 0.024 | 0.031 2.33 (1.08, 5.03) | ||||||
| Currently married | 44 (75.9) | 126 (65.6) | 73 (81.1) | 97 (60.6) | 45 (80.4) | 125 (64.4) | ||||||
| Unmarried/widowed (Ref) | 14 (24.1) | 66 (34.4) | 17 (18.9) | 63 (39.4) | 11 (19.6) | 69 (35.6) | ||||||
| Household income | 0.001 | 0.008 2.91 (1.31, 6.44) | 0.369 | NA | 0.627 | NA | ||||||
| At least minimum wage | 47 (81) | 94 (57.7) | 58 (67.4) | 83 (61.5) | 34 (66.7) | 107 (62.9) | ||||||
| Below minimum wage | 11 (19) | 69 (42.3) | 28 (32.6) | 52 (38.5) | 17 (33.3) | 63 (37.1) | ||||||
| Type of Barriers | Perceived Barriers | Total (n = 250) Frequency (Percentage) * | Malay (n = 163) Frequency (Percentage) * | Chinese (n = 61) Frequency (Percentage) * | Indians (n = 23) Frequency (Percentage) * | p Value # |
|---|---|---|---|---|---|---|
| Emotional | Fear of diagnosis | 187 (74.8) | 130 (79.8) | 41 (67.2) | 13 (56.5) | 0.018 |
| Fear of losing breast | 166 (66.4) | 112 (68.7) | 38 (62.3) | 13 (56.5) | 0.401 | |
| Embarrassment | 128 (51.2) | 91 (55.8) | 24 (39.3) | 11 (47.8) | 0.085 | |
| Socio-cultural | Stigma on breast health seeking | 111 (44.4) | 76 (46.6) | 26 (42.6) | 7 (30.4) | 0.330 |
| Lack of family support | 54 (21.6) | 47 (28.8) | 5 (8.2) | 2 (8.7) | 0.001 | |
| Health system related | Uncomfortable with male doctors | 124 (49.6) | 96 (58.9) | 19 (31.1) | 7 (30.4) | <0.001 |
| Doctors might consider symptoms as negligible | 31 (12.4) | 28 (17.2) | 3 (4.9) | 0 | 0.008 | |
| Delay in getting appointment | 58 (23.2) | 47 (28.8) | 9 (14.8) | 2 (8.7) | 0.018 | |
| Doctors do not understand the language and culture | 77 (30.8) | 47 (28.8) | 24 (39.3) | 5 (21.7) | 0.195 | |
| Practical/ financial | Other things to worry about | 92 (36.8) | 62 (38.0) | 23 (37.7) | 6 (26.1) | 0.532 |
| Lack of time | 48 (19.2) | 44 (27.0) | 2 (3.3) | 1 (4.3) | <0.001 | |
| Cost | 174 (69.6) | 124 (76.1) | 34 (55.7) | 13 (56.5) | 0.005 | |
| Distance to health care facility | 118 (47.2) | 88 (54.0) | 20 (32.8) | 8 (34.8) | 0.009 | |
| Screening-related | Lack of trust in screening | 28 (11.2) | 24 (14.7) | 3 (4.9) | 1 (4.3) | 0.065 |
| Pain and discomfort | 132 (52.8) | 102 (62.6) | 21 (34.4) | 7 (30.4) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohan, D.; Su, T.T.; Donnelly, M.; Hoe, W.M.K.; Schliemann, D.; Tan, M.M.; Reidpath, D.; Taib, N.A.; Allotey, P. Breast Cancer Screening in Semi-Rural Malaysia: Utilisation and Barriers. Int. J. Environ. Res. Public Health 2021, 18, 12293. https://doi.org/10.3390/ijerph182312293
Mohan D, Su TT, Donnelly M, Hoe WMK, Schliemann D, Tan MM, Reidpath D, Taib NA, Allotey P. Breast Cancer Screening in Semi-Rural Malaysia: Utilisation and Barriers. International Journal of Environmental Research and Public Health. 2021; 18(23):12293. https://doi.org/10.3390/ijerph182312293
Chicago/Turabian StyleMohan, Devi, Tin Tin Su, Michael Donnelly, Wilfred Mok Kok Hoe, Désirée Schliemann, Min Min Tan, Daniel Reidpath, Nur Aishah Taib, and Pascale Allotey. 2021. "Breast Cancer Screening in Semi-Rural Malaysia: Utilisation and Barriers" International Journal of Environmental Research and Public Health 18, no. 23: 12293. https://doi.org/10.3390/ijerph182312293
APA StyleMohan, D., Su, T. T., Donnelly, M., Hoe, W. M. K., Schliemann, D., Tan, M. M., Reidpath, D., Taib, N. A., & Allotey, P. (2021). Breast Cancer Screening in Semi-Rural Malaysia: Utilisation and Barriers. International Journal of Environmental Research and Public Health, 18(23), 12293. https://doi.org/10.3390/ijerph182312293






