Who Is Suffering from the “Corona Blues”? An Analysis of the Impacts of the COVID-19 Pandemic on Depression and Its Implications for Health Policy
Abstract
:1. Introduction, Theoretical Issues and Hypothesis
1.1. Why Do Corona Blues Matter?
1.2. Theoretical Issues: Impact of COVID-19 on Mental Health
1.3. Sociodemographic Factors
1.3.1. Gender
1.3.2. Age
1.3.3. Education Level
1.3.4. Income
1.3.5. Marital Status
1.3.6. Children
1.4. Non-Pandemic Factors
1.4.1. Social Support
1.4.2. Health Status
1.4.3. Optimism
1.4.4. Self-Efficacy
1.5. Pandemic Factors
1.5.1. Concerns about Infection and Threats to One’s Life
1.5.2. Financial Instability
1.5.3. Employment Instability
1.5.4. Lifestyle Changes
1.5.5. Health Status Changes after COVID-19 Infections
1.5.6. Knowledge
1.5.7. Preventive Actions
2. Sample and Measurements
2.1. Sample
2.2. Measurements
2.3. Analysis Method
3. Analysis
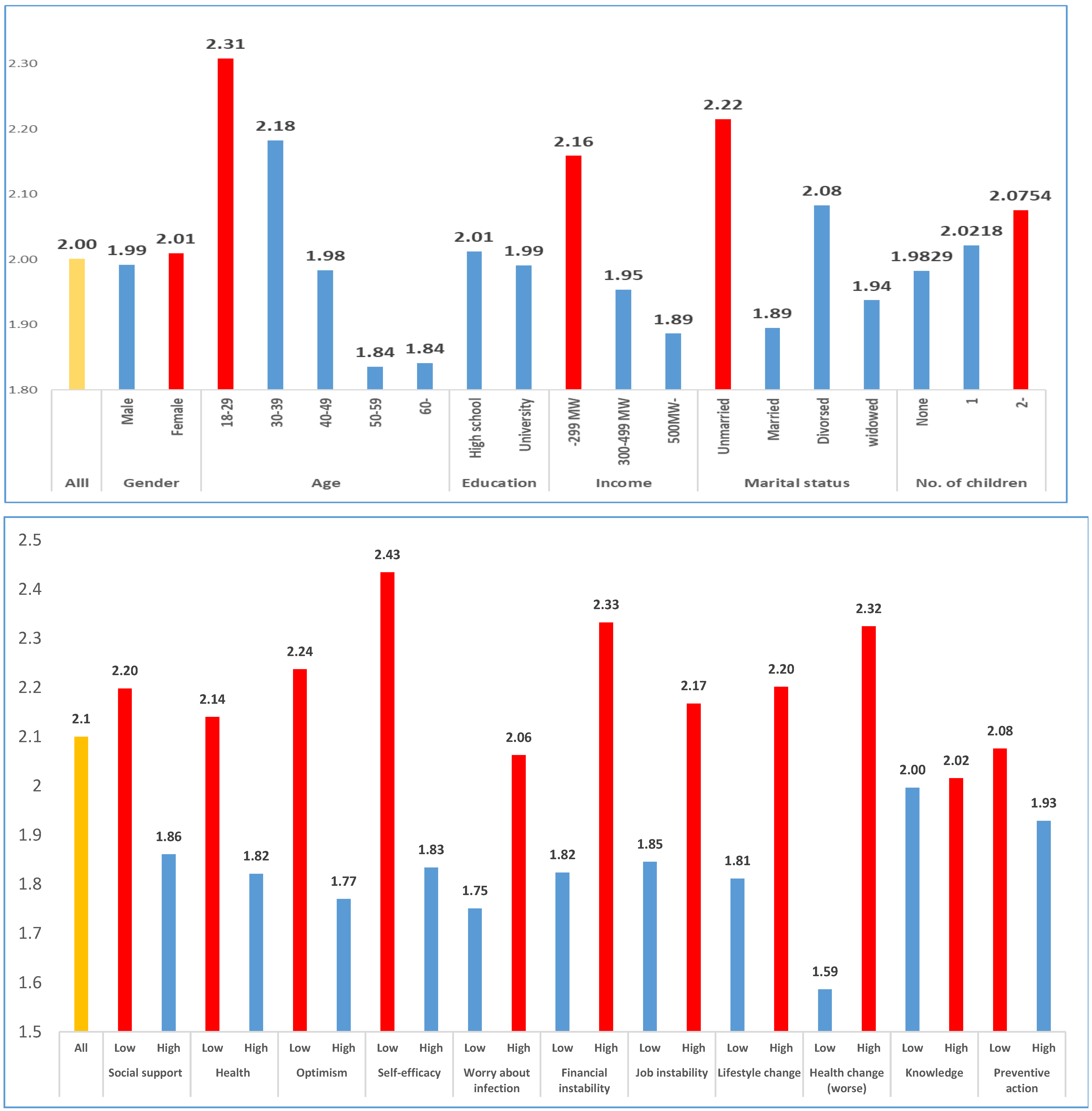
3.1. Descriptive Analysis
3.2. Regression Analysis
4. Discussion and Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard. 2021. Available online: https://covid19.who.int/ (accessed on 10 July 2020).
- Solomou, L.; Constantinidou, F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter. Int. J. Environ. Res. Public Health 2020, 17, 4924. [Google Scholar] [CrossRef]
- Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 2020, 51, 102092. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.M.; Wong, J.G.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, C.M.; Wong, P.C.; Tsang, K.W.T.; Chua, S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J. Psychiatry 2007, 52, 233–240. [Google Scholar] [CrossRef] [Green Version]
- Jeong, H.; Yim, H.W.; Song, Y.J. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health 2016, 38, e2016048. [Google Scholar] [CrossRef]
- Bueno-Notivol, J.; Gracia-García, P.; Olaya, B.; Lasheras, I.; López-Antón, R.; Santabárbara, J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021, 21, 100196. [Google Scholar] [CrossRef]
- Stein, D.J.; Scott, K.M.; de Jonge, P.; Kessler, R.C. Epidemiology of anxiety disorders: From surveys to nosology and back. Dialogues Clin. Neurosci. 2017, 19, 127–136. [Google Scholar]
- Santabárbara, J.; Lasheras, I.; Lipnicki Darren, M.; Bueno-Notivol, J.; Pére z-Moreno, M.; López-Antón, R.; De la Cámara, C.; Lobo, A.; Gracia-García, P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 109, 110207. [Google Scholar] [CrossRef]
- Lei, L.; Huang, X.; Zhang, S.; Yang, J.; Yang, L.; Xu, M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med. Sci. Monit. 2020, 26, e924609-1. [Google Scholar] [CrossRef] [Green Version]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Ahmed Khan, F.; Napolean Shanmugam, G.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef]
- Al Maqbali, M.; Al Sinani, M.; Al-Lenjawi, B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J. Psychosom. Res. 2020, 141, 110343. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.J.G.; Taylor, S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020, 71, 102211. [Google Scholar] [CrossRef]
- APA (American Psychiatry Association). What Is Depression? 2020. Available online: https://www.psychiatry.org/patients-families/depression/what-is-depression (accessed on 1 May 2020).
- Huremović, D. Mental Health of Quarantine and Isolation, Psychiatry of Pandemics; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Seligman, M.E.P. Learned Helplessness. Annu. Rev. Med. 1972, 23, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Ni, M.Y.; Yang, L.; Leung, C.M.; Li, N.; Yao, X.I.; Wang, Y.; Leung, G.M.; Cowling, B.J.; Liao, Q. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China. JMIR Public Health Surveill 2020, 7, e19009. [Google Scholar] [CrossRef] [PubMed]
- Al Banna, M.H.; Sayeed, A.; Kundu, S.; Christopher, E.; Hasan, M.T.; Begum, M.R.; Kormoker, T.; Dola, S.T.I.; Hassan, M.M.; Chowdhury, S.; et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: A nationwide cross-sectional study. Int. J. Environ. Health Res. 2020, 1–12. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Porter, C.; Favara, M.; Hittmeyer, A.; Scott, D.; Jiménez, A.S.; Ellanki, R.; Woldehanna, T.; Duc, L.T.; Craske, M.G.; Stein, A. Impact of the COVID-19 pandemic on anxiety and depression symptoms of young people in the global south: Evidence from a fourcountry cohort study. BMJ Open 2021, 11, e049653. [Google Scholar] [CrossRef]
- Kazmi, S.S.H.; Hasan, K.; Talib, S.; Saxena, S. COVID-19 and Lockdwon: A study on the impact on mental health. SSRN Electron. J. 2020, 13. [Google Scholar] [CrossRef]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef]
- Guo, Y.; Cheng, C.; Zeng, Y.; Li, Y.; Zhu, M.; Yang, W.; Xu, H.; Li, X.; Leng, J.; Monroe-Wise, A.; et al. Mental health Disorders and associated risk factors in quarantined adults during the COVID-19 outbreak in China: Cross-sectional study. J. Med. Internet Res. 2020, 22, e20328. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Nguyen, H.C.; Nguyen, M.H.; Do, B.N.; Tran, C.Q.; Nguyen, T.T.P.; Pham, K.M.; Pham, L.V.; Tran, K.V.; Duong, T.T.; Tran, T.V.; et al. People with Suspected COVID-19 Symptoms Were More Likely Depressed and Had Lower Health-Related Quality of Life: The Potential Benefit of Health Literacy. J. Clin. Med. 2020, 9, 965. [Google Scholar] [CrossRef] [Green Version]
- Sønderskov, K.M.; Dinesen, P.T.; Santini, Z.I.; Østergaard, S.D. The depressive state of Denmark during the COVID-19 pandemic Acta. Neuropsychiatrica 2020, 32, 226–228. [Google Scholar] [CrossRef] [Green Version]
- Fu, W.; Wang, C.; Zou, L.; Guo, Y.; Lu, Z.; Yan, S.; Mao, J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry 2020, 10, 225. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 2020, 11, 1540. [Google Scholar] [CrossRef]
- Liu, X.; Zhu, M.; Zhang, R.; Zhang, J.; Zhang, C.; Liu, P.; Feng, Z.; Chen, Z. Public mental health problems during COVID-19 pandemic: A large-scale meta-analysis of the evidence. Transl. Psychiatry 2021, 11, 384. [Google Scholar] [CrossRef] [PubMed]
- MHW (Ministry of Health and Welfare). Corona 19 National Mental Health Survey. 2020. Available online: http://www.mohw.go.kr (accessed on 1 June 2020).
- Zhang, Y.; Ma, Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, 2381. [Google Scholar] [CrossRef] [Green Version]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Shevlin, M.; McBride, O.; Murphy, J.; Miller, J.G.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.P.; McKay, R.; Stocks, T.V.; et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 2020, 6, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.M.A.; Mohammad, D.; Qureshi, M.F.H.; Abbas, M.Z.; Aleem, S. Prevalence, Psychological Responses and Associated Correlates of Depression, Anxiety and Stress in a Global Population, During the Coronavirus Disease (COVID-19) Pandemic. Community Ment. Health J. 2021, 57, 101–110. [Google Scholar] [CrossRef]
- Sigdel, A.; Bista, A.; Bhattarai, N.; Poon, B.C.; Giri, G.; Marqusee, H. Depression, Anxiety and Depression-anxiety comorbidity amid COVID-19 Pandemic: An online survey conducted during lockdown in Nepal. MedRxiv 2020. [Google Scholar] [CrossRef]
- Arafa, A.; Mohamed, A.; Saleh, L.; Senosy, S. Psychological impacts of the COVID-19 pandemic on the public in Egypt. Community Ment. Health J. 2020, 57, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Horesh, D.; Kapel Lev-Ari, R.; Hasson-Ohayon, I. Risk factors for psychological distress during the COVID-19 pandemic in Israel: Loneliness, age, gender, and health status play an important role. Br. J. Health Psychol. 2020, 25, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef] [PubMed]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Palgi, Y.; Shrira, A.; Ring, L.; Bodner, E.; Avidor, S.; Bergman, Y.; Cohen-Fridel, S.; Keisari, S.; Hoffman, Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020, 275, 109–111. [Google Scholar] [CrossRef]
- Kotov, R.; Gamez, W.; Schmidt, F.; Watson, D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychol. Bull. 2010, 136, 768–821. [Google Scholar] [CrossRef]
- Conversano, C.; Rotondo, A.; Lensi, E.; Della Vista, O.; Arpone, F.; Reda, M.A. Optimism and its impact on mental and physical well-being. Clin. Pract. Epidemiol. Ment. Health 2010, 6, 25–29. [Google Scholar] [CrossRef]
- Zhou, S.J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Biber, D.D.; Melton, B.; Czech, D.R. The impact of COVID-19 on college anxiety, optimism, gratitude, and course satisfaction. J. Am. Coll. Health 2020. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy. In Encyclopedia of Human Behavior; Ramachaudran, V.S., Ed.; Academic Press: New York, NY, USA, 1994; Volume 4, pp. 71–81. [Google Scholar]
- Mumtaz, A.; Manzoor, F.; Jiang, S.; Anisur Rahaman, M. COVID-19 and Mental Health: A Study of Stress, Resilience, and Depression among the Older Population in Pakistan. Healthcare 2021, 9, 424. [Google Scholar] [CrossRef]
- Arima, M.; Takamiya, Y.; Furuta, A.; Siriratsivawong, K.; Tsuchiya, S.; Izumi, M. Factors associated with the mental health status of medical students during the COVID-19 pandemic: A cross-sectional study in Japan. BMJ Open 2020, 10, e043728. [Google Scholar] [CrossRef] [PubMed]
- Bressington, D.T.; Cheung, T.C.; Lam, S.C.; Suen, L.; Kwai, P.; Fong, T.K.H.; Ho, H.S.W. Association Between Depression, Health Beliefs, and Face Mask Use During the COVID-19 Pandemic. Front. Psychiatry 2020, 11, 571179. [Google Scholar] [CrossRef]
- Sun, Y.; Song, H.; Liu, H.; Mao, F.; Sun, X.; Cao, F. Occupational stress, mental health, and self-efficacy among community mental health workers: A cross-sectional study during COVID-19 pandemic. Int. J. Soc. Psychiatry 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Hyland, P.; Shevlin, M.; McBride, O.; Murphy, J.; Karatzias, T.; Bentall, R.P.; Martinez, A.; Vallières, F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020, 142, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and anxiety in Hong Kong during covid-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef]
- Hertz-Palmor, N.; Moore, T.M.; Gothelf, D.; Di Domenico, G.E.; Dekel, I.; Greenberg, D.M.; Barzilay, R. Association among income loss, financial strain and depressive symptoms during COVID-19: Evidence from two longitudinal studies. MedRxiv 2020. [Google Scholar] [CrossRef]
- Ueda, M.; Stickley, A.; Sueki, H.; Matsubayashi, T. Mental health status of the general population during the Covid-19 pandemic: A cross-sectional national survey in Japan. MedRxiv. 2020. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef]
- Shi, L.; Lu, Z.A.; Que, J.Y.; Huang, X.L.; Liu, L.; Ran, M.S.; Gong, Y.M.; Yuan, K.; Yan, W.; Sun, Y.K.; et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 2020, 3, e2014053. [Google Scholar] [CrossRef]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Malmborg, J.S.; Bremander, A.; Olsson, M.C.; Bergman, A.C.; Brorsson, A.S.; Bergman, S. Worse health status, sleeping problems, and anxiety in 16-year-old students are associated with chronic musculoskeletal pain at three-year follow-up. BMC Public Health 2019, 19, 1565. [Google Scholar] [CrossRef]
- Seong, K.; Kim, S.J.; Moon, J.H. Effects of Life Changes Due to COVID-19 on Depression in the Elderly. Soc. Work. Pract. Res. 2021, 18, 99–129. [Google Scholar] [CrossRef]
- Aldhmadi, B.K.; Kumar, R.; Itumalla, R.; Perera, B. Depressive Symptomatology and Practice of Safety Measures among Undergraduate Students during COVID-19: Impact of Gender. Int. J. Environ. Res. Public Health 2021, 18, 4924. [Google Scholar] [CrossRef] [PubMed]
- Sakib, N.; Akter, T.; Zohra, F.; Bhuiyan, A.I.; Mamun, M.A.; Griffiths, M.D. Fear of COVID-19 and Depression: A Comparative Study Among the General Population and Healthcare Professionals During COVID-19 Pandemic Crisis in Bangladesh. Int. J. Ment. Health Addict. 2021, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Rubin, G.J.; Wessely, S. The psychological effects of quarantining a city. BMJ Clin. Res. Ed. 2020, 368, m313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO (World Health Organization). Survey Tool and Guidance. 2020. Available online: https://www.euro.who.int/_data/assets/pdf_file/0007/436705/COVID-19-survey-tool-and-guidance.pdf (accessed on 1 July 2020).
- ABS (Australian Bureau of Statistics). Household Impacts of COVID-19 Survey. Available online: https://www.abs.gov.au/ (accessed on 1 July 2020).
- Beck, A.T.; Steer, R.A.; Brown, G.K. Manual for the Beck Depression Inventory-II; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [Green Version]
- Zhao, H.; He, X.; Fan, G.; Li, L.; Huang, Q.; Qiu, Q.; Kang, Z.; Du, T.; Han, L.; Ding, L.; et al. COVID-19 infection outbreak increases anxiety level of general public in China: Involved mechanisms and influencing factors. J. Affect. Disord. 2020, 276, 446–452. [Google Scholar] [CrossRef]
- Ciarambino, T.; Palmiero, L.; Bottone, R.; Schettini, F.; Adinolfi, L.E.; Giordano, M. Female relatives of Covid-19 patients have an unsatisfactory perception of emergency room performance by clinical staff. Aging Pathobiol. Ther. 2021, 3, 37–38. [Google Scholar] [CrossRef]
- Ciarambino, T.; Ilardi, A.; Giannico, O.; Maffettone, A.; Ciaburri, F.; Paoli, V.; Fontanella, A.; Tirelli, P.; Bologna, C.; Gallucci, F.; et al. Gender differences in COVID-19 patients: A regional survey among physicians of Internal Medicine Wards. Ital. J. Med. 2021, 15, 160–163. [Google Scholar] [CrossRef]
- Biegler, P. Autonomy, stress, and treatment of depression. BMJ 2008, 336, 1046–1048. [Google Scholar] [CrossRef] [Green Version]
- Sherwood, P.R.; Given, C.W.; Given, B.A.; von Eye, A. Caregiver burden and depressive symptoms: Analysis of common outcomes in caregivers of elderly patients. J. Aging Health 2005, 17, 125–147. [Google Scholar] [CrossRef]
- Shalini, M.; Tushar, S. Gender-Based Violence During COVID-19 Pandemic: A Mini-Review. Front. Glob. Women’s Health 2020, 1, 4. [Google Scholar]
- Seney, M.L.; Ekong, K.I.; Ding, Y.; Tseng, G.C.; Sibille, E. Sex chromosome complement regulates expression of mood-related genes. Biol Sex Differ. 2013, 4, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pařízek, A.; Mikešová, M.; Jirák, R.; Hill, M.; Koucký, M.; Pašková, A.; Velíková, M.; Adamcová, K.; Šrámková, M.; Jandíková, H.; et al. Steroid hormones in the development of postpartum depression. Physiol. Res. 2014, 63 (Suppl. 2), S277–S282. [Google Scholar] [CrossRef] [PubMed]

| Concept | Measurement | Scale | Mean (S.D.) | Cronbach’s α |
|---|---|---|---|---|
| Social support | -I have many good social relationships with people. -When I am in trouble, I can get help from others. | Five-point scale (1 = strongly disagree, 5 = strongly agree). | 3.49 (0.690) | 0.800 |
| Health status | -I am healthy. -I am in good health compared to other people. | Five-point scale (1 = strongly disagree, 5 = strongly agree). | 3.24 (0.808) | 0.901 |
| Optimism | -I am an optimist who thinks the future will be bright. -I think many of the current problems will be resolved. | Five-point scale (1 = strongly disagree, 5 = strongly agree). | 3.33 (0.771) | 0.828 |
| Self-efficacy | -If I make an effort, I can fully practice preventive actions. -I have sufficient ability to practice coronavirus prevention actions. | Five-point scale (1 = strongly, 5 = strongly agree). | 3.95 (0.719) | 0.868 |
| Worry about infection and life-threating | -How do you rate the probability of being infected with the coronavirus on a scale from 1 to 10, where 1 point means “very low’ and 10 points means “very high” -How do you rate the probability of your life being threatened by the coronavirus on a scale from 1 to 10, where 1 point means “very low” and 10 points means “very high” | Ten-point scale (1 = very low, 10 = very high)? | 4.30 (2.188) | 0.833 |
| Financial instability | -What do you think about the impact of COVID-19? I will personally go bankrupt. | Five-point scale (1 = strongly disagree, 5 = strongly agree). | 3.08 (1.108) | - |
| Occupational instability | - I may be personally out of work or lose my job. | Five-point scale (1 = strongly disagree, 5 = strongly agree). | 3.36 (1.129) | - |
| Lifestyle changes | -How much did your participation in the following activities increase compared to before the outbreak of the coronavirus: (1) time spent using a smartphone, (2) time spent watching TV, (3) time exercising, and (4) time for self-development? Responses: ① decreased, ② the same, ③ slightly increased, ④ increased a lot. | Four-point scale (1 = decreased. 2 = no change, 3= increased a little, 4 = increased a lot) | 2.64 (0.610) | 0.628 |
| Health status changes | -Physical health deteriorated after the COVID-19 pandemic. -Health become worse after the COVID-19 pandemic. | Five-point scale (1 = strongly disagree, 5 = strongly agree). | 2.78 (0.840) | 0.771 |
| Knowledge | -I am well aware of the COVID-19 pandemic. -I know more about the COVID-19 pandemic. | Five-point scale (1 = strongly disagree, 5 = strongly agree). | 3.02 (0.650) | 0.840 |
| Preventive actions | -Have you taken the following preventive actions to prevent coronavirus infection: (1) covering your mouth with your sleeve when coughing, (2) ventilating the room at least twice a day, and (3) wearing a mask? | Five-point scale (1 = did not comply at all, 5 = thoroughly complied) | 4.17 (0.635) | 0.769 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depression | −0.16 ** | −0.217 ** | −0.289 ** | −0.229 ** | 0.306 ** | 0.318 ** | 0.239 ** | 0.251 ** | 0.43 ** | −0.003 | −0.125 ** | |
| 2. Social support | −0.164 ** | 0.254 ** | 0.335 ** | 0.267 ** | −0.097 ** | −0.056 * | −0.024 | 0.069 ** | −0.038 | 0.257 ** | 0.299 ** | |
| 3. Health status | −0.219 ** | 0.290 ** | 0.337 ** | 0.197 ** | −0.262 ** | −0.1 ** | −0.083 ** | 0.074 ** | −0.15 ** | 0.185 ** | 0.171 ** | |
| 4. Optimism | −0.311 ** | 0.346 ** | 0.353 ** | 0.243 ** | −0.165 ** | −0.129 ** | −0.116 ** | 0.037 | −0.117 ** | 0.152 ** | 0.15 ** | |
| 5. Self−efficacy | −0.239 ** | 0.274 ** | 0.210 ** | 0.257 ** | −0.178 ** | −0.06 * | 0.06 * | −0.01 | −0.177 ** | 0.135 ** | 0.433 ** | |
| 6. Concern about infection and threat to life | 0.309 ** | −0.104 ** | −0.265 ** | −0.169 ** | −0.175 ** | 0.202 ** | 0.149 ** | 0.131 ** | 0.296 ** | 0.008 | −0.06 * | |
| 7. Financial instability | 0.326 ** | −0.097 ** | −0.131 ** | −0.147 ** | −0.066 ** | 0.216 ** | 0.741 ** | 0.121 ** | 0.262 ** | 0.054 * | 0.015 | |
| 8. Occupational instability | 0.260 ** | −0.070 ** | −0.119 ** | −0.145 ** | 0.044 † | 0.165 ** | 0.753 ** | 0.100 ** | 0.235 ** | 0.017 | 0.106 ** | |
| 9. Lifestyle change | 0.253 ** | 0.076 ** | 0.079 ** | 0.029 | −0.01 | 0.129 ** | 0.111 ** | 0.093 ** | 0.163 ** | 0.093 ** | 0.043 † | |
| 10. Health status change | 0.420 ** | −0.041 | −0.146 ** | −0.110 ** | −0.170 ** | 0.296 ** | 0.265 ** | 0.239 ** | 0.160 ** | 0.08 ** | −0.033 | |
| 11. Knowledge | −0.013 | 0.275 ** | 0.202 ** | 0.175** | 0.142 ** | 0.005 | 0.032 | −0.010 | 0.090 ** | 0.077 ** | 0.161 ** | |
| 12. Preventive actions | −0.131 ** | 0.292 ** | 0.176 ** | 0.146 ** | 0.439 ** | −0.046 † | 0.018 | 0.098 ** | 0.045 † | −0.018 | 0.152 ** |
| Factor | Variable | B | S.E. | Beta | T-Value | Sig |
|---|---|---|---|---|---|---|
| Constant | 1.902 | 0.232 | 8.194 | 0.000 | ||
| Factor 1: Sociodemographic factors | Gender | −0.036 | 0.043 | −0.018 | −0.839 | 0.401 |
| Age | −0.007 | 0.002 | −0.111 | −3.332 | 0.001 | |
| Education level | −0.003 | 0.045 | −0.002 | −0.077 | 0.939 | |
| Income | −0.021 | 0.048 | −0.009 | −0.433 | 0.665 | |
| Married | −0.095 | 0.071 | −0.046 | −1.344 | 0.179 | |
| Divorced | −0.038 | 0.111 | −0.008 | −0.341 | 0.733 | |
| Widowed | −0.029 | 0.157 | −0.004 | −0.188 | 0.851 | |
| Number of children | 0.017 | 0.032 | 0.013 | 0.530 | 0.596 | |
| Factor 2: Non-pandemic factors | Social support | −0.064 | 0.034 | −0.045 | −1.864 | 0.062 |
| Health status | −0.072 | 0.029 | −0.059 | −2.483 | 0.013 | |
| Optimism | −0.220 | 0.031 | −0.171 | −7.205 | 0.000 | |
| Self-efficacy | −0.090 | 0.034 | −0.065 | −2.688 | 0.007 | |
| Factor 3: Pandemic related factors | Concern about infection and threats to life | 0.046 | 0.010 | 0.101 | 4.474 | 0.000 |
| Financial instability | 0.154 | 0.029 | 0.172 | 5.366 | 0.000 | |
| Employment instability | −0.002 | 0.028 | −0.002 | −0.074 | 0.941 | |
| Lifestyle changes | 0.296 | 0.035 | 0.182 | 8.541 | 0.000 | |
| Health changes (worse) | 0.327 | 0.027 | 0.276 | 12.142 | 0.000 | |
| Knowledge | 0.016 | 0.034 | 0.010 | 0.467 | 0.641 | |
| Preventive actions | −0.071 | 0.038 | −0.045 | −1.857 | 0.064 | |
| F-value | 46.203 *** | |||||
| R2/adjusted R2 | 0.369/0.361 | |||||
| F1: R2/adjusted R2 | 0.041/0.036 | |||||
| F2: R2/adjusted R2 | 0.131/0.133 | |||||
| F3: R2/adjusted R2 | 0.295/0.272 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Kim, S. Who Is Suffering from the “Corona Blues”? An Analysis of the Impacts of the COVID-19 Pandemic on Depression and Its Implications for Health Policy. Int. J. Environ. Res. Public Health 2021, 18, 12273. https://doi.org/10.3390/ijerph182312273
Kim S, Kim S. Who Is Suffering from the “Corona Blues”? An Analysis of the Impacts of the COVID-19 Pandemic on Depression and Its Implications for Health Policy. International Journal of Environmental Research and Public Health. 2021; 18(23):12273. https://doi.org/10.3390/ijerph182312273
Chicago/Turabian StyleKim, Sunhee, and Seoyong Kim. 2021. "Who Is Suffering from the “Corona Blues”? An Analysis of the Impacts of the COVID-19 Pandemic on Depression and Its Implications for Health Policy" International Journal of Environmental Research and Public Health 18, no. 23: 12273. https://doi.org/10.3390/ijerph182312273
APA StyleKim, S., & Kim, S. (2021). Who Is Suffering from the “Corona Blues”? An Analysis of the Impacts of the COVID-19 Pandemic on Depression and Its Implications for Health Policy. International Journal of Environmental Research and Public Health, 18(23), 12273. https://doi.org/10.3390/ijerph182312273







