Reconstruction of a Neglected, Extensor Hallucis Longus Tendon Rupture Using Interposed Scar Tissue: A Case Report and Literature Review
Abstract
:1. Introduction
2. Case Presentation
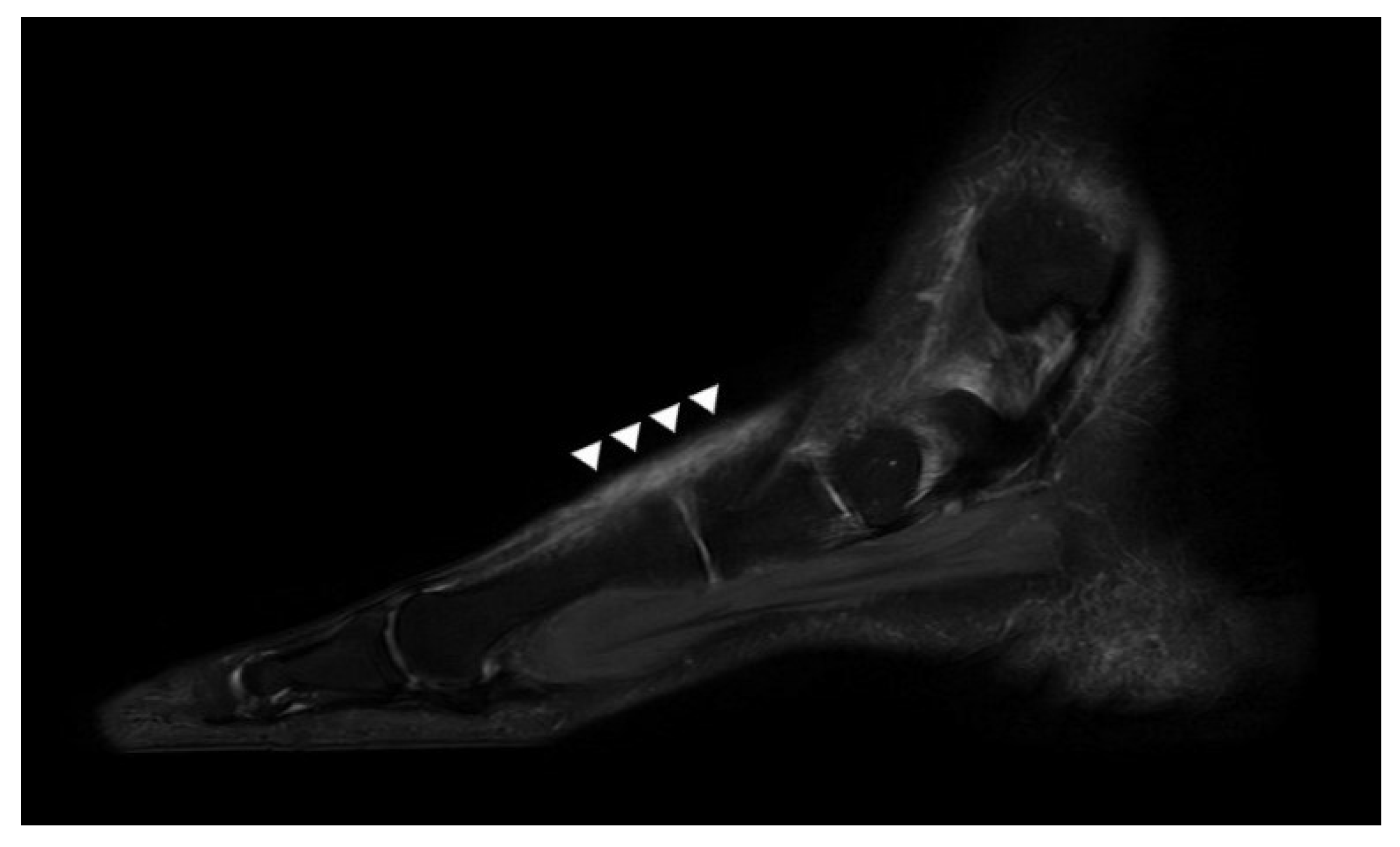
2.1. Preoperative Evaluation
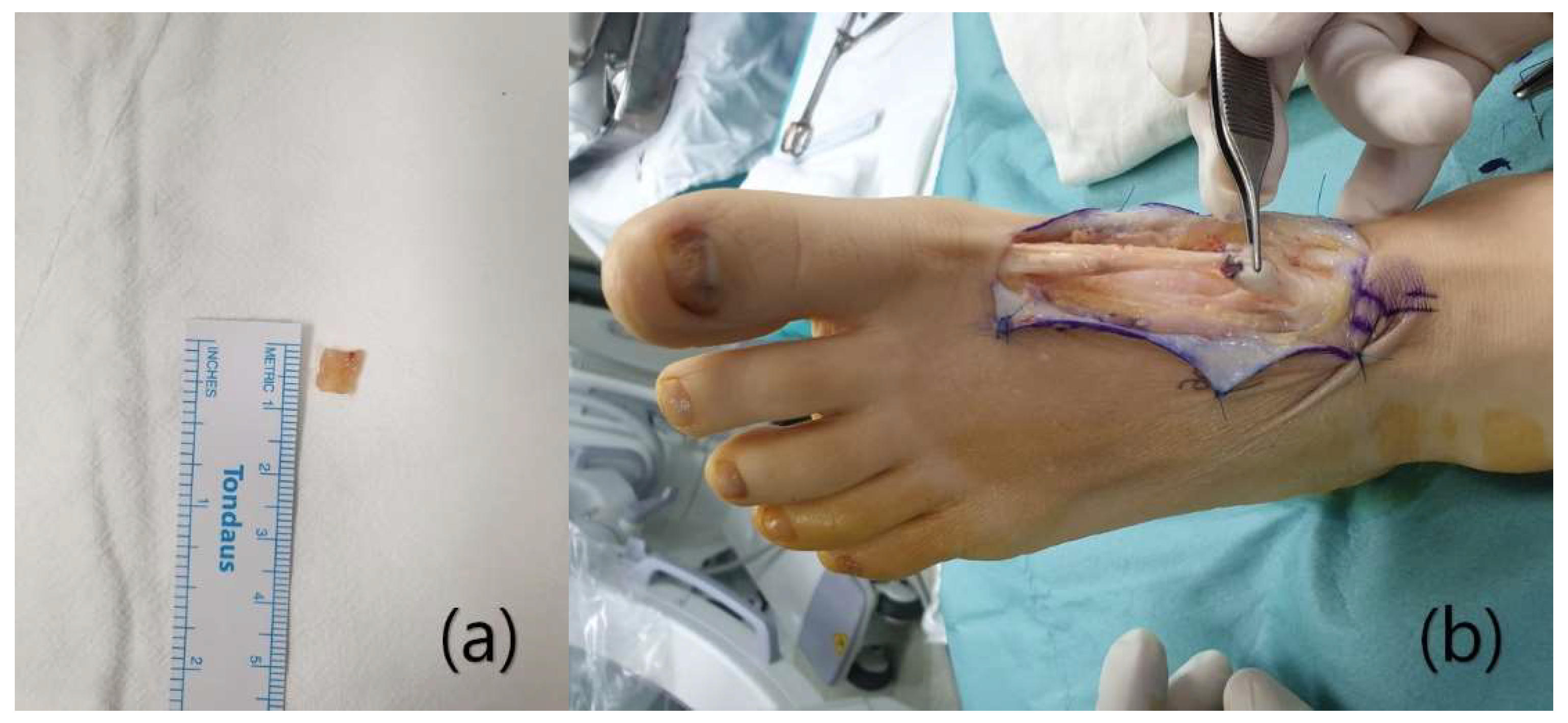
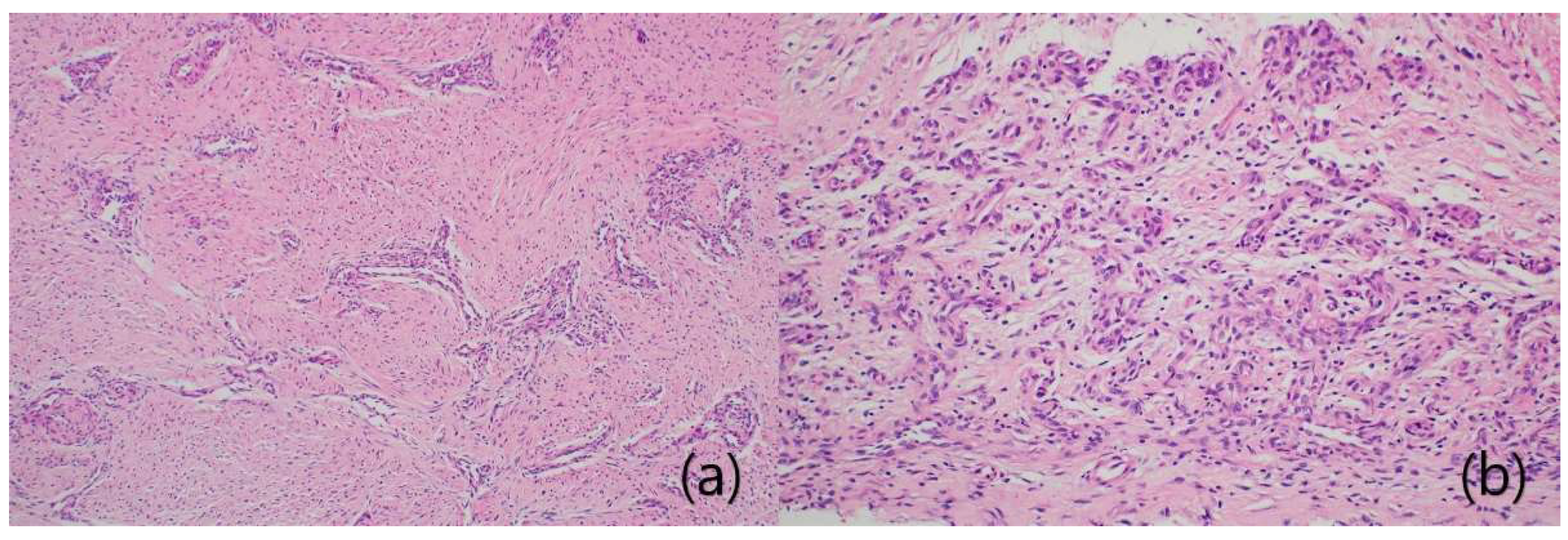
2.2. Surgical Procedure
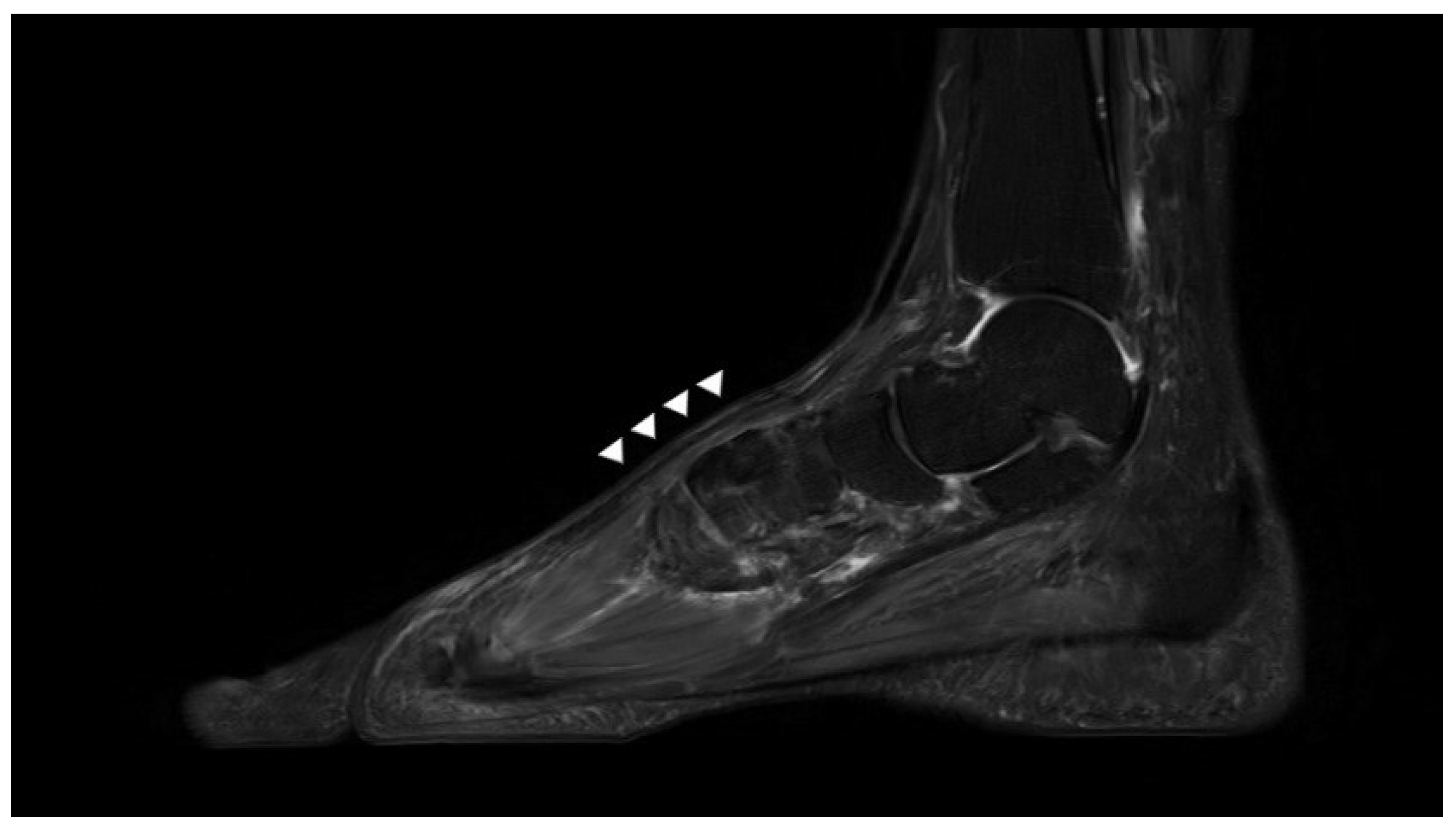
2.3. Postoperative Details
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| EHL | Extensor hallucis longus |
| EDL | Extensor digitorum longus |
| MRI | Magnetic resonance imaging |
References
- Wong, J.C.; Daniel, J.N.; Raikin, S.M. Repair of acute extensor hallucis longus tendon injuries: A retrospective review. Foot Ankle Spec. 2014, 7, 45–51. [Google Scholar] [CrossRef]
- Kass, J.C.; Palumbo, F.; Mehl, S.; Camarinos, N. Extensor hallucis longus tendon injury: An in-depth analysis and treatment protocol. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 1997, 36, 24–27. [Google Scholar] [CrossRef]
- Mulcahy, D.M.; Dolan, A.M.; Stephens, M.M. Spontaneous rupture of extensor hallucis longus tendon. Foot Ankle Int. 1996, 17, 162–163. [Google Scholar] [CrossRef] [PubMed]
- Tuncer, S.; Aksu, N.; Isıklar, U. Delayed rupture of the extensor hallucis longus and extensor digitorum communis tendons after breaching the anterior capsule with a radiofrequency probe during ankle arthroscopy: A case report. J. Foot Ankle Surg. 2010, 49, 490.e1. [Google Scholar] [CrossRef] [PubMed]
- Kurashige, T. Chronic extensor hallucis longus tendon rupture treated with double-bundle autograft of extensor hallucis capsularis: A case report. SAGE Open Med. Case Rep. 2019, 7, 2050313X19841962. [Google Scholar] [CrossRef] [PubMed]
- Tomford, W.W. Transmission of disease through transplantation of musculoskeletal allografts. JBJS 1995, 77, 1742–1754. [Google Scholar] [CrossRef] [PubMed]
- Hirose, K.; Kondo, S.; Choi, H.-R.; Mishima, S.; Iwata, H.; Ishiguro, N. Spontaneous healing process of a supraspinatus tendon tear in rabbits. Arch. Orthop. Trauma Surg. 2004, 124, 374–377. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, T.; Kinoshita, M.; Abe, M.; Shibayama, Y. Unfavorable effect of knee immobilization on Achilles tendon healing in rabbits. Acta Orthop. Scand. 2000, 71, 69–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yasuda, T.; Kinoshita, M.; Okuda, R. Reconstruction of chronic Achilles tendon rupture with the use of interposed tissue between the stumps. Am. J. Sports Med. 2007, 35, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, T.; Shima, H.; Mori, K.; Kizawa, M.; Neo, M. Direct repair of chronic Achilles tendon ruptures using scar tissue located between the tendon stumps. JBJS 2016, 98, 1168–1175. [Google Scholar] [CrossRef] [PubMed]
- Yeo, E.D.; Han, J.K.; Lee, H.S.; Won, S.H.; Jung, K.J.; Chang, H.J.; Cha, J.S.; Ahn, H.; Lee, D.W.; Kang, J.K. Direct reconstruction of chronic extensor digitorum longus tendon rupture using interposed scar tissue in the foot: A case report. Medicine 2020, 99, e22506. [Google Scholar] [CrossRef] [PubMed]
- Lezak, B.; Wehrle, C.J.; Summers, S. Anatomy, bony pelvis and lower limb, posterior tibial artery. [Updated 8 August 2021]. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK536981/ (accessed on 15 September 2021).
- Thordarson, D.B.; Shean, C.J. Nerve and tendon lacerations about the foot and ankle. JAAOS J. Am. Acad. Orthop. Surg. 2005, 13, 186–196. [Google Scholar] [CrossRef] [PubMed]
- Hinsenkamp, M.; Muylle, L.; Eastlund, T.; Fehily, D.; Noël, L.; Strong, D. Adverse reactions and events related to musculoskeletal allografts: Reviewed by the World Health Organisation Project NOTIFY. Int. Orthop. 2012, 36, 633–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zielaskowski, L.A.; Pontious, J. Extensor hallucis longus tendon rupture repair using a fascia lata allograft. J. Am. Podiatr. Med. Assoc. 2002, 92, 467–470. [Google Scholar] [CrossRef] [PubMed]
- Porter, D.A.; Mannarino, F.P.; Snead, D.; Gabel, S.J.; Ostrowski, M. Primary repair without augmentation for early neglected Achilles tendon ruptures in the recreational athlete. Foot Ankle Int. 1997, 18, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Bruns, J.; Kampen, J.; Kahrs, J.; Plitz, W. Achilles tendon rupture: Experimental results on spontaneous repair in a sheep-model. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 364–369. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, W.-J.; Jung, K.-J.; Ahn, H.; Yeo, E.-D.; Lee, H.-S.; Won, S.-H.; Lee, D.-W.; Ji, J.-Y.; Yoon, S.-J.; Hong, Y.-C. Reconstruction of a Neglected, Extensor Hallucis Longus Tendon Rupture Using Interposed Scar Tissue: A Case Report and Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 12157. https://doi.org/10.3390/ijerph182212157
Kim W-J, Jung K-J, Ahn H, Yeo E-D, Lee H-S, Won S-H, Lee D-W, Ji J-Y, Yoon S-J, Hong Y-C. Reconstruction of a Neglected, Extensor Hallucis Longus Tendon Rupture Using Interposed Scar Tissue: A Case Report and Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(22):12157. https://doi.org/10.3390/ijerph182212157
Chicago/Turabian StyleKim, Woo-Jong, Ki-Jin Jung, Hyein Ahn, Eui-Dong Yeo, Hong-Seop Lee, Sung-Hun Won, Dhong-Won Lee, Jae-Young Ji, Sung-Joon Yoon, and Yong-Cheol Hong. 2021. "Reconstruction of a Neglected, Extensor Hallucis Longus Tendon Rupture Using Interposed Scar Tissue: A Case Report and Literature Review" International Journal of Environmental Research and Public Health 18, no. 22: 12157. https://doi.org/10.3390/ijerph182212157
APA StyleKim, W.-J., Jung, K.-J., Ahn, H., Yeo, E.-D., Lee, H.-S., Won, S.-H., Lee, D.-W., Ji, J.-Y., Yoon, S.-J., & Hong, Y.-C. (2021). Reconstruction of a Neglected, Extensor Hallucis Longus Tendon Rupture Using Interposed Scar Tissue: A Case Report and Literature Review. International Journal of Environmental Research and Public Health, 18(22), 12157. https://doi.org/10.3390/ijerph182212157






