1. Introduction
The word dissection originates from the Latin words “dis” and “secare”, namely, “to separate” and “to cut”. Dissection can, therefore, be understood as the practice of dissecting an organism to analyze its internal structures, which does not include its meaning in the medical field, as the study of a human corpse for the purpose of teaching anatomy.
Human body dissection was already widely practiced in ancient Greece, while in Roman times, it was forbidden, so, as reported by Galen’s writings, anatomical studies continued on animals, assuming their anatomical similarity [
1]. Remaining in the European context, the progressive awareness of the usefulness of human dissection as an irreplaceable cognitive and didactic method of understanding anatomy resulted in the legalization of this practice in around the fourteenth century. In the present time, anatomical dissection plays a key role in the study of anatomy, being present in many of the major medical schools worldwide [
2,
3]. The study of anatomical preparation represents not only an important didactic opportunity for students and neophytes, but it is useful in many medical and surgical disciplines, to better understand the anatomical reasons for certain biological traits [
4,
5].
Even in the dental field, especially in oral surgery, questions may arise from daily clinical practice, which can be answered thanks to the study of anatomy.
2. Materials and Methods
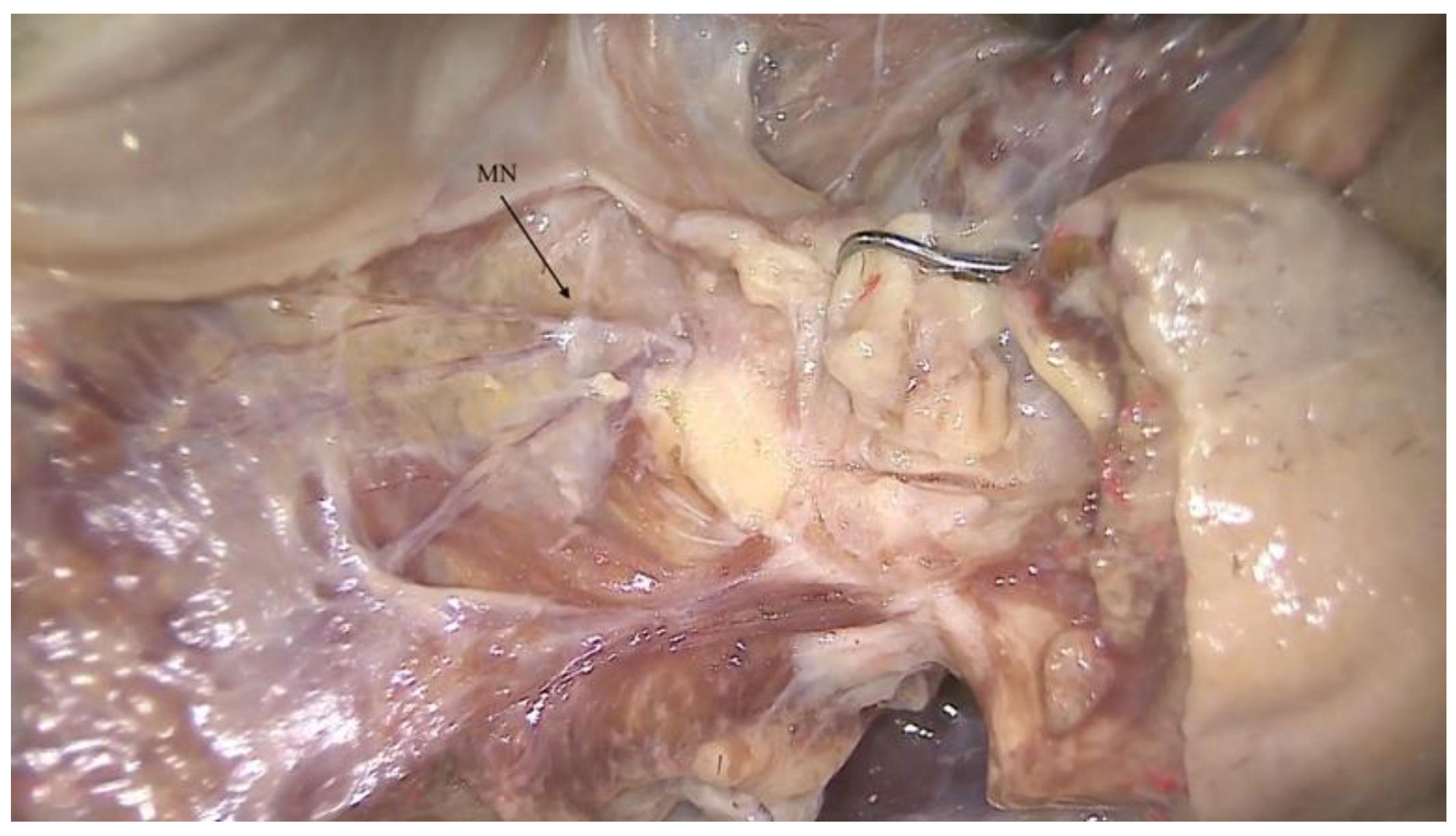
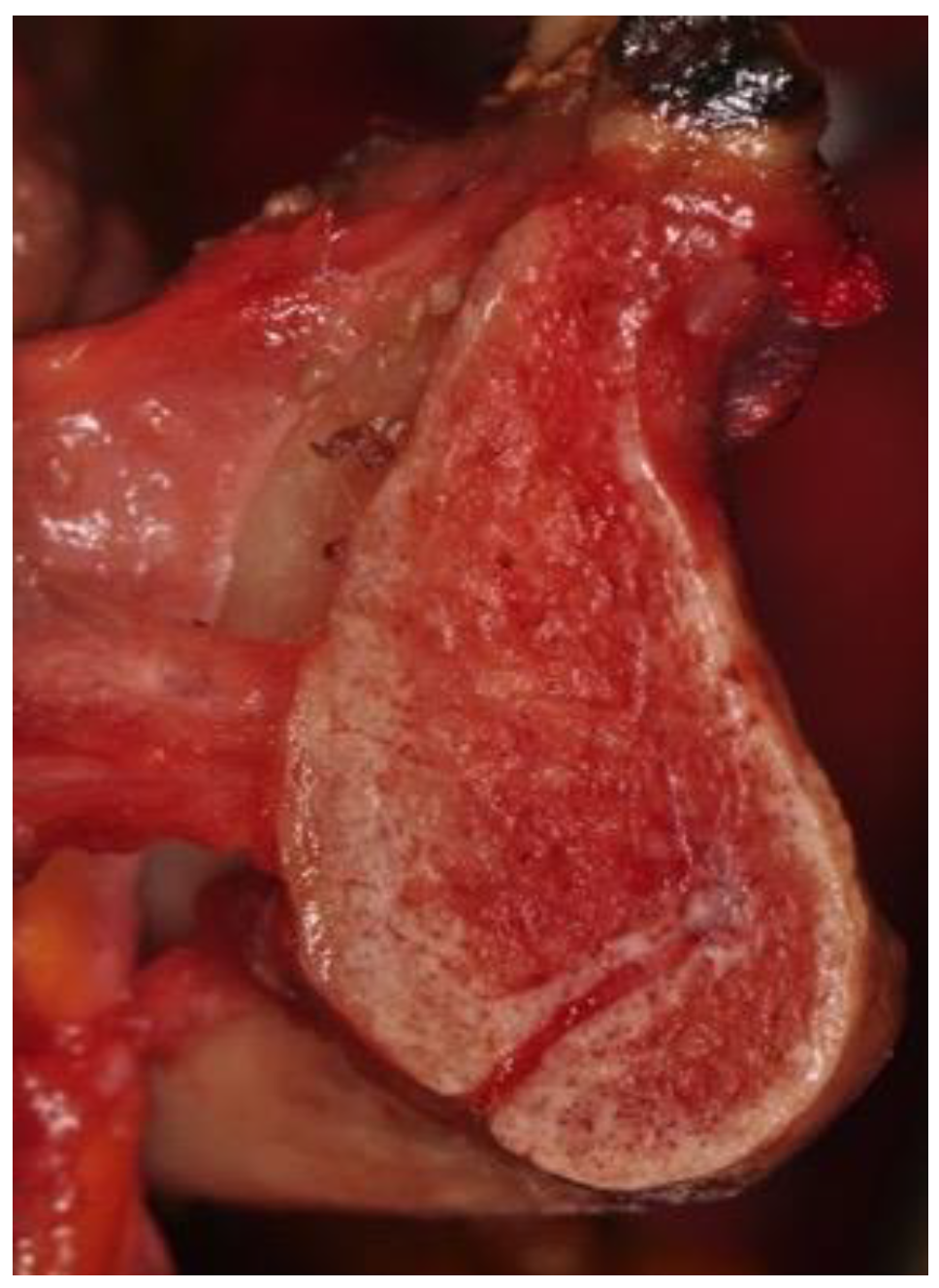
An example of a clinical question is the possible lack of anesthesia of the mandibular symphysis during oral surgery. The mandibular symphysis is a common surgery site for the extraction or exposure of impacted lower canines, the removal of cystic lesions, the realization of mentoplasty, or for the grafting of large amounts of intraoral bone. On such occasions it is necessary to obtain complete anesthesia of the surgical area, which is classically pursued through the bilateral block of the mental nerves and possible reinforcements with local infiltrations at the symphysis (
Figure 1). Sometimes, however, given that the operation is performed under local anesthesia, it is possible that the patient reports intraoperative pain despite the correct execution of the anesthetic techniques described above [
6]. This possibility can trigger doubts about the success of the nerve block. These doubts, however, can be discarded thanks to an in-depth anatomical study through anatomical dissection of the lower jaw (
Figure 2).
3. Results
3.1. The Nerve to the Mylohyoid
The mandibular symphysis receives terminal innervation from the third trigeminal branch (V3), via the inferior alveolar nerve. The inferior alveolar nerve then divides into the mental nerve, which emerges from the homonymous foramen at the level of the apexes of the first and second lower premolar, and in the incisor nerve, which continues its intra-bony course until it anastomoses medially with the contralateral nerve. The nerve to the mylohyoid is also found in the symphyseal area. It is a motor nerve that detaches from V3 before the mandibular nerve enters the mandible. It can originate from different distances that refer to the entrance into the mandibular foramen, between 13.4 and 14.7 mm, as reported in the literature. Once detached, the nerve runs anteriorly along the mandibular lingual surface in the mylohyoid groove. This groove can also be found in the form of an intra-bony canal, enclosing the neurovascular bundle. At the end of the mylohyoid groove, the motor fibers of the mylohyoid nerve end in the homonymous muscle, and in the anterior belly of the digastric muscle. Normally, this nerve is only responsible for muscle motility, which should not create any problems for symphysis anesthesia [
7].
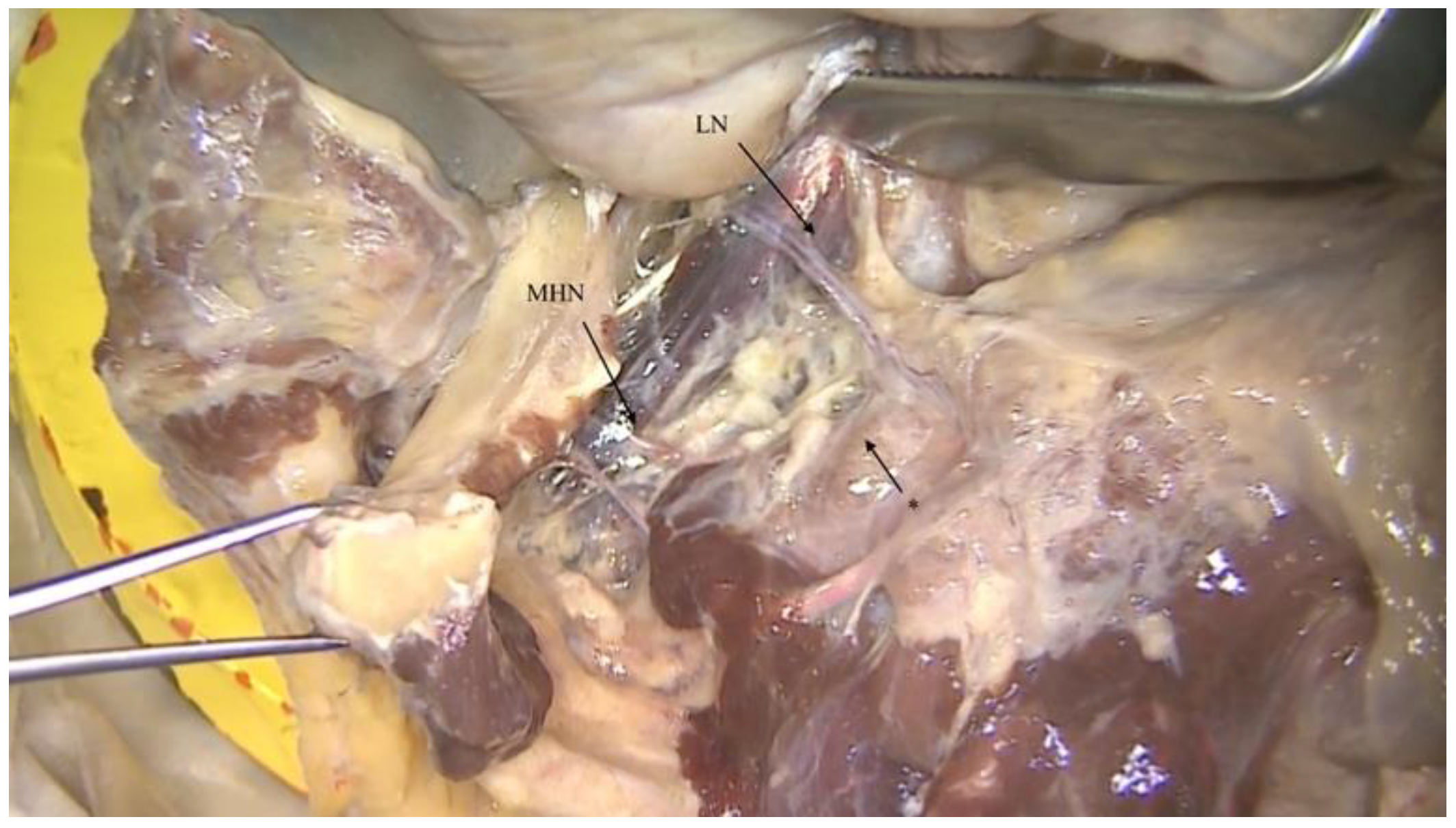
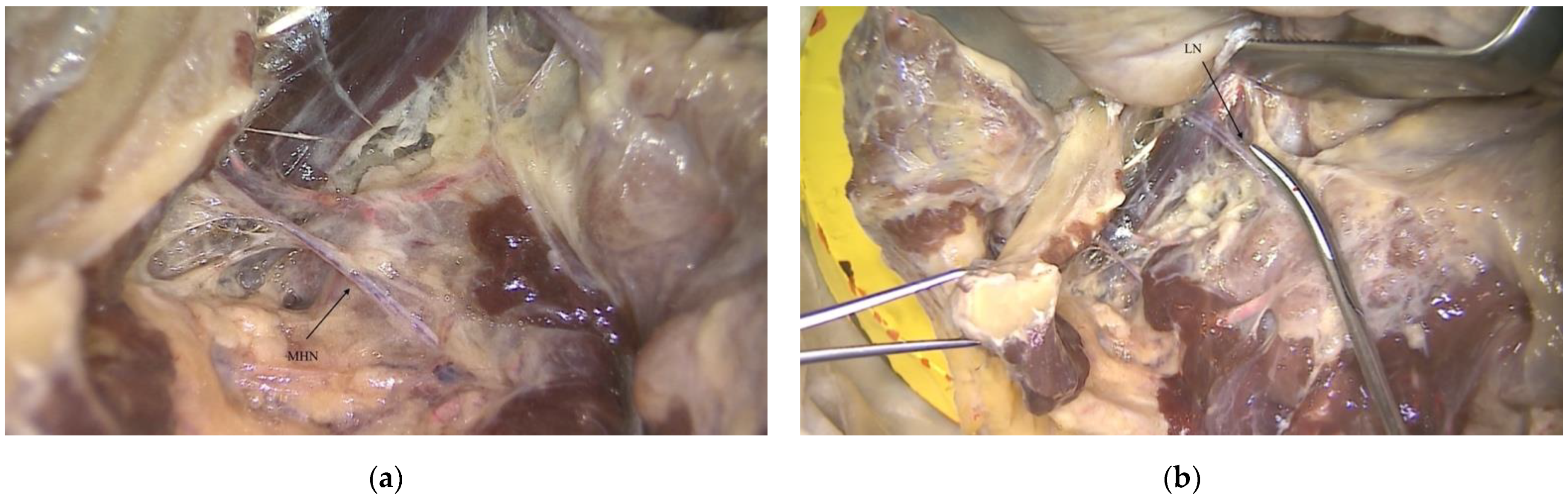
However, it is not uncommon to find an anastomosis between the nerve to the mylohyoid and the terminations of the lingual nerve [
8] (
Figure 3 and
Figure 4).
3.2. The Lingual Nerve
The lingual nerve is also a posterior branch that detaches from the mandibular nerve, and then exits the infratemporal fossa, and passes between the tensor of the veli palatini and the lateral pterygoid muscle. After descending into the plane between the medial and lateral pterygoid muscles, it enters the pterygomandibular space between the lateral pterygoid and the mandibular branch, running more anteriorly and medially than the course of the inferior alveolar nerve. The lingual nerve continues to run along the mandibular body, in which it forms an imprint on its medial aspect below the third molar and immediately above the posterior margin of the mylohyoid line. This precise position is well known to dentists due to the risk of injury it causes during third molar surgery. The lingual nerve lies on the lateral side of the tongue, crossing the styloglossus muscle, and then traveling with the hyoglossus above the submandibular gland and its duct, with which it has an intimate relationship. The lingual nerve then passes through the mylohyoid muscle and rests on the genioglossus muscle. From here, the lingual nerve divides into several terminal branches below the tongue mucosa, providing sensory innervation of the anterior 2/3 of the tongue, the lingual floor, and the lingual gingiva of the molar and premolar area [
9,
10].
Crossing the duct of the submandibular gland, the lingual nerve can give rise to an unusual lateral branch that anastomoses with the nerve to the mylohyoid, usually below it, as it passes through the mylohyoid muscle [
11].
In patients who have the described anastomosis, an anesthetic injection at only the level of the mental foramina may not be sufficient to obtain total anesthesia, causing painful perception during surgery. The nerve to the mylohyoid, in fact, in such cases, collects the sensitivity of the symphyseal area. The clinical solution derives from the knowledge of this anatomical variant, which is easily understood if highlighted during a cadaver dissection (
Figure 5). The clinician must, therefore, proceed, in the event of sensory perception during surgery in the symphyseal area, with a bilateral anesthetic block of the lingual nerves.
The lingual nerve block has an injection point that is distal to the second molar and 6–8 mm lower than the lingual gingival margin. The insertion axis of the needle originates from the contralateral canine region and turns to the second molar. The 5–8 mm penetration of the needle will allow one to reach the target area for lingual nerve anesthesia. This procedure must be performed bilaterally to ensure adequate anesthesia of the symphysis in the above-described cases of anastomosis of the lingual nerve and the nerve to the mylohyoid [
12].
4. Discussion
There is no doubt that this anesthetic procedure primarily involves knowledge of the possible anastomosis, the course of the lingual nerve, and the point where the lingual nerve meets the nerve to the mylohyoid. As a result, anatomical study of this region may be crucial [
13].
Thus, from the clinical example of the lack of anesthesia to the mental symphysis, the importance of anatomical study, particularly through dissection, can be better understood. The knowledge deriving from anatomical dissection plays a key role, not least because of its usefulness for the patient. In the described case, in fact, the patient can benefit greatly from being able to safely receive surgery of the symphyseal area under complete analgesia, thanks to the knowledge acquired by the surgeon.
5. Conclusions
The study of anatomy through dissection is an ancient practice that can still be a useful tool for clinicians today, to find answers to their daily practice questions, raising their level of preparation and the quality of their work. Human body dissection is crucial not only in medical school, providing the student with a solid foundation of anatomy, but also for expert surgeons, to grant their patient a safe and high-quality clinical procedure.
Author Contributions
Conceptualization, R.P. and P.F.; methodology, R.P.; validation, P.F., M.K. and A.R.; writing—original draft preparation, L.B.; writing—review and editing, C.B.; visualization, R.P. and M.C.; supervision, P.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Nutton, V. The Unknown Galen; Institute of Classical Studies: London, UK, 2002; p. 89. [Google Scholar]
- Macchi, V.; Porzionato, A.; Stecco, C.; Tiengo, C.; Parenti, A.; Cestrone, A.; De Caro, R. Body parts removed during surgery: A useful training source. Anat. Sci. Educ. 2011, 4, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.C.H.; Chan, S.O.; Wong, A.L.Y.; Ng, P.K.L. Understanding family involvement in body donation in Hong Kong: A qualitative study of registered donors and bereaved family members. Health Soc. Care Community 2020, 28, 270–278. [Google Scholar] [CrossRef] [PubMed]
- De Caro, R.; Boscolo-Berto, R.; Artico, M.; Bertelli, E.; Cannas, M.; Cappello, F.; Carpino, G.; Castorina, S.; Cataldi, A.; Cavaletti, G.A.; et al. The Italian law on body donation: A position paper of the Italian College of Anatomists. Ann. Anat. Anat. Anz. 2021, 238, 151761. [Google Scholar] [CrossRef] [PubMed]
- Orsini, E.; Quaranta, M.; Ratti, S.; Mariani, G.A.; Mongiorgi, S.; Billi, A.M.; Manzoli, L. The whole body donation program at the university of Bologna: A report based on the experience of one of the oldest university in Western world. Ann. Anat. Anat. Anz. 2021, 234, 151660. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.; Reader, A.; Beck, M.; Meyers, W.J. Anesthetic efficacy of the mylohyoid nerve block and combination inferior alveolar nerve block/mylohyoid nerve block. Oral. Surg. Oral. Med. Oral. Pathol. 1999, 87, 557–563. [Google Scholar] [CrossRef]
- Stein, P.; Brueckner, J.; Milline, M. Sensory Innervation of Mandibular Teeth by the Nerve to the Mylohyoid: Implications in Local Anesthesia. Clin. Anat. 2007, 20, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Iwanaga, J.; Kikuta, S.; Oskouian, R.J.; Tubbs, R.S. Nerve to mylohyoid branched from the lingual nerve: Previously undescribed case. Anat. Sci. Int. 2019, 94, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Ghabriel, M.; Takezawa, K.; Townsend, G. The lingual nerve: Overview and new insights into anatomical variability based on fine dissection using human cadavers. Odontology 2019, 107, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Shimotakahara, R.; Lee, H.; Mine, K.; Ogata, S.; Tamatsu, Y. Anatomy of the lingual nerve: Application to oral surgery. Clin. Anat. 2019, 32, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Zhan, C.; Yuan, Z.; Qu, R.; Zou, L.; He, S.; Li, Z.; Liu, C.; Xiao, Z.; Ouyang, J.; Dai, J. Should we pay attention to the aberrant nerve communication between the lingual and mylohyoid nerves? Br. J. Oral. Maxillofac. Surg. 2019, 57, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, S.; Paneerselvam, E.; Guruprasad, T.; Pathumai, M.; Abraham, S.; Krishnakumar Raja, V.B. Efficacy of Exclusive Lingual Nerve Block versus Conventional Inferior Alveolar Nerve Block in Achieving Lingual Soft-tissue Anesthesia. Ann. Maxillofac. Surg. 2017, 7, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Potu, B.K.; Pulakunta, T.; Ray, B.; Rao, M.S.; Bhat, K.M.; D’Silva, S.S.; Nayak, S.R. Unusual communication between the lingual nerve and mylohyoid nerves in a South Indian male cadaver: Its clinical significance. Rom. J. Morphol. Embryol. 2009, 50, 145–146. [Google Scholar] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).