Naturalistic Topography Assessment in a Randomized Clinical Trial of Smoking Unfiltered Cigarettes: Challenges, Opportunities, and Recommendations
Abstract
:1. Introduction
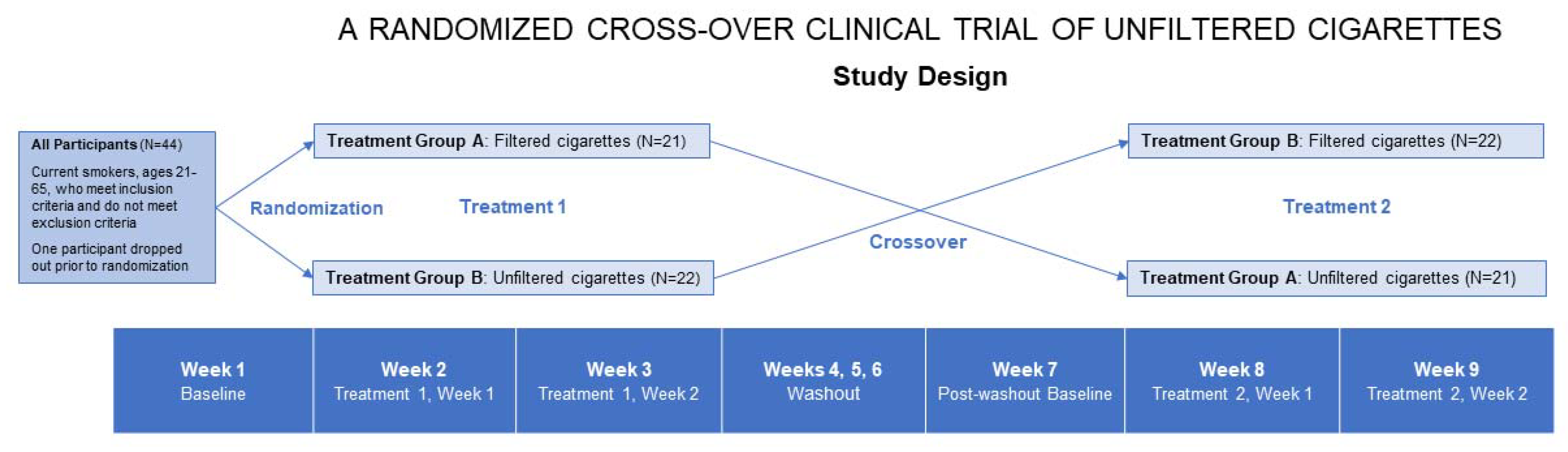
2. Experimental Section
Methods
3. Results
3.1. Calibration and Standardization of CReSS Settings
3.2. Compliance Rates
3.3. Other CReSS Device Issues
3.4. Overheating and Clogging
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blank, M.D.; Disharoon, S.; Eissenberg, T. Comparison of methods for measurement of smoking behavior: Mouthpiece-based computerized devices versus direct observation. Nicotine Tob. Res. 2009, 11, 896–903. [Google Scholar] [CrossRef]
- Pickworth, W.B.; Lee, E.M.; Malson, J.L.; Moolchan, E.T.; Waters, A.J. Smoking topography: Reliability and validity in dependent smokers. Nicotine Tob. Res. 2003, 5, 673–679. [Google Scholar] [CrossRef]
- Oldham, M.J.; Plunkett, S.E.; Fisher, M.T.; Shafer, K.H.; Morton, M.J. Laboratory evaluation of the CReSSmicro™ portable topography device: Implications for clinical research. Contrib. Tob. Res. 2014, 26, 19–25. [Google Scholar] [CrossRef] [Green Version]
- McClure, E.A.; Stitzer, M.L.; Vandrey, R. Characterizing smoking topography of cannabis in heavy users. Psychopharmacology 2012, 220, 309–318. [Google Scholar] [CrossRef] [Green Version]
- De Jesus, S.; Hsin, A.; Faulkner, G.; Prapavessis, H. A systematic review and analysis of data reduction techniques for the CReSS smoking topography device. J. Smok. Cessat. 2015, 10, 12–28. [Google Scholar] [CrossRef]
- Borgwaldt-Hauni: Korber Solutions. CReSS Pocket & CReSS Desktop FAQ Handbook. (n.d.) pp. 1–68, CReSS Pocket & CReSS Desktop_FAQ_Handbook. Available online: https://www.borgwaldt.com/en/products/smoking-vaping-machines/smoking-topography-devices/cress-pocket.html (accessed on 7 November 2021).
- Shahab, L.; West, R.; McNeill, A. The feasibility of measuring puffing behaviour in roll-your-own cigarette smokers. Tob. Control 2008, 17 (Suppl. 1), i17–i23. [Google Scholar] [CrossRef] [PubMed]
- June, K.M.; Norton, K.J.; Rees, V.W.; O’Connor, R.J. Influence of measurement setting and home smoking policy on smoking topography. Addict. Behav. 2012, 37, 42–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Jesus, S.; Prapavessis, H. Smoking behaviour and sensations during the pre-quit period of an exercise-aided smoking cessation intervention. Addict. Behav. 2018, 81, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Ross, K.C.; Juliano, L.M. Smoking Through a Topography Device Diminishes Some of the Acute Rewarding Effects of Smoking. Nicotine Tob. Res. 2016, 18, 564–571. [Google Scholar] [CrossRef]
- Hammond, D.; Fong, G.T.; Cummings, K.M.; Hyland, A. Smoking Topography, Brand Switching, and Nicotine Delivery: Results from an In vivo Study. Cancer Epidemiol. Biomark. Prev. 2005, 14, 1370–1375. [Google Scholar] [CrossRef] [Green Version]
- Wood, T.; Wewers, M.E.; Groner, J.; Ahijevych, K. Smoke constituent exposure and smoking topography of adolescent daily cigarette smokers. Nicotine Tob. Res. 2004, 6, 853–862. [Google Scholar] [CrossRef] [PubMed]
- Mikheev, V.B.; Buehler, S.S.; Brinkman, M.C.; Granville, C.A.; Lane, T.E.; Ivanov, A.; Cross, K.M.; Clark, P.I. The Application of Commercially Available Mobile Cigarette Topography Devices for E-cigarette Vaping Behavior Measurements. Nicotine Tob. Res. 2020, 22, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Appleton, S.; Liu, J.; Lipowicz, P.J.; Sarkar, M. Effect of cigarette design on biomarkers of exposure, puffing topography and respiratory parameters. Inhal. Toxicol. 2015, 27, 174–180. [Google Scholar] [CrossRef] [Green Version]
- Watson, C.V.; Richter, P.; de Castro, B.R.; Sosnoff, C.; Potts, J.; Clark, P.; McCraw, J.; Yan, X.; Chambers, D.; Watson, C. Smoking Behavior and Exposure: Results of a Menthol Cigarette Cross-over Study. Am. J. Health Behav. 2017, 41, 309–319. [Google Scholar] [CrossRef] [Green Version]
- Chen, A.; Krebs, N.; Zhu, J.; Muscat, J.E. Nicotine metabolite ratio predicts smoking topography: The Pennsylvania Adult Smoking Study. Drug Alcohol Depend. 2018, 190, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Denlinger-Apte, R.L.; Donny, E.C.; Lindgren, B.R.; Rubin, N.; Goodwin, C.; DeAtley, T.; Colby, S.M.; Cioe, P.A.; Hatsukami, D.K.; Tidey, J.W. Smoking Topography Characteristics During a 6-Week Trial of Very Low Nicotine Content Cigarettes in Smokers With Serious Mental Illness. Nicotine Tob. Res. 2020, 22, 1414–1418. [Google Scholar] [CrossRef] [PubMed]
- Gass, J.C.; Germeroth, L.J.; Wray, J.M.; Tiffany, S.T. The Reliability and Stability of Puff Topography Variables in Non-Daily Smokers Assessed in the Laboratory. Nicotine Tob. Res. 2016, 18, 484–490. [Google Scholar] [CrossRef]
- Caraway, J.W.; Ashley, M.; Bowman, S.A.; Chen, P.; Errington, G.; Prasad, K.; Nelson, P.R.; Shepperd, C.J.; Fearon, I.M. Influence of cigarette filter ventilation on smokers’ mouth level exposure to tar and nicotine. Regul. Toxicol. Pharmacol. 2017, 91, 235–239. [Google Scholar] [CrossRef]
- Eissenberg, T.; Adams, C.; Riggins, E.C.; Likness, M. Smokers’ sex and the effects of tobacco cigarettes: Subject-rated and physiological measures. Nicotine Tob. Res. 1999, 1, 317–324. [Google Scholar] [CrossRef]
- Benowitz, N.L.; Bernert, J.T.; Foulds, J.; Hecht, S.S.; Jacob, P.; Jarvis, M.J.; Joseph, A.; Oncken, C.; Piper, M.E. Biochemical Verification of Tobacco Use and Abstinence: 2019 Update. Nicotine Tob. Res. 2020, 22, 1086–1097. [Google Scholar] [CrossRef] [PubMed]
- Oren, E.; Pulvers, K.; Romero, D.R.; Barber, C.; Carter, E.; Tracy, L.A.; Novotny, T.E. Effects of Unfiltered Cigarettes on Smoking Behavior and Toxicant Exposure: Protocol for a Randomized Crossover Clinical Trial. JMIR Res. Protoc. 2020, 9, e19603. [Google Scholar] [CrossRef] [PubMed]
- Evans-Reeves, K.; Lauber, K.; Hiscock, R. The ‘filter fraud’ persists: The tobacco industry is still using filters to suggest lower health risks while destroying the environment. Tob. Control 2021, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Novotny, T.E.; Slaughter, E. Tobacco Product Waste: An Environmental Approach to Reduce Tobacco Consumption. Curr. Environ. Health Rep. 2014, 1, 208–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Demographic/Characteristic | Total n = 43 |
|---|---|
| n (%) | |
| Age, Mean (SD) | 36.7 (9.9) |
| Sex | |
| Female | 18 (41.9) |
| Male | 25 (58.1) |
| Ethnicity | |
| Not Hispanic/Latino | 35 (81.4) |
| Hispanic/Latino | 8 (18.6) |
| Mexican | 5 (11.6) |
| Puerto Rican | 2 (4.7) |
| Another Hispanic/Latino origin | 1 (2.3) |
| Race | |
| White | 30 (69.8) |
| Multiple races | 5 (11.6) |
| Asian American | 3 (7.0) |
| African American | 2 (4.7) |
| Native Hawaiian or Other Pacific Islander | 0 |
| American Indian or Alaska Native | 0 |
| Unknown | 3 (7.0) |
| Education | |
| High school or below | 11 (25.6) |
| Some college or technical school | 21 (48.8) |
| College graduate or above | 11 (25.6) |
| Income (in $1000s), Mean (SD) | 38.7 (35.4) |
| # years smoked cigarettes, Mean (SD) | 17.2 (9.6) |
| # days smoked in past 30 days, Mean (SD) | 30.0 (0.0) |
| # cigarettes smoked per day, past 30 days, Mean (SD) | 14.5 (6.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero, D.R.; Pulvers, K.; Carter, E.; Barber, C.; Satybaldiyeva, N.; Novotny, T.E.; Oren, E. Naturalistic Topography Assessment in a Randomized Clinical Trial of Smoking Unfiltered Cigarettes: Challenges, Opportunities, and Recommendations. Int. J. Environ. Res. Public Health 2021, 18, 11857. https://doi.org/10.3390/ijerph182211857
Romero DR, Pulvers K, Carter E, Barber C, Satybaldiyeva N, Novotny TE, Oren E. Naturalistic Topography Assessment in a Randomized Clinical Trial of Smoking Unfiltered Cigarettes: Challenges, Opportunities, and Recommendations. International Journal of Environmental Research and Public Health. 2021; 18(22):11857. https://doi.org/10.3390/ijerph182211857
Chicago/Turabian StyleRomero, Devan R., Kim Pulvers, Erika Carter, Casey Barber, Nora Satybaldiyeva, Thomas E. Novotny, and Eyal Oren. 2021. "Naturalistic Topography Assessment in a Randomized Clinical Trial of Smoking Unfiltered Cigarettes: Challenges, Opportunities, and Recommendations" International Journal of Environmental Research and Public Health 18, no. 22: 11857. https://doi.org/10.3390/ijerph182211857
APA StyleRomero, D. R., Pulvers, K., Carter, E., Barber, C., Satybaldiyeva, N., Novotny, T. E., & Oren, E. (2021). Naturalistic Topography Assessment in a Randomized Clinical Trial of Smoking Unfiltered Cigarettes: Challenges, Opportunities, and Recommendations. International Journal of Environmental Research and Public Health, 18(22), 11857. https://doi.org/10.3390/ijerph182211857






