Development of Policy-Relevant Indicators for Injury Prevention in British Columbia by the Key Decision-Makers
Abstract
1. Introduction
2. Methods
2.1. Context
2.2. Priority Setting Process
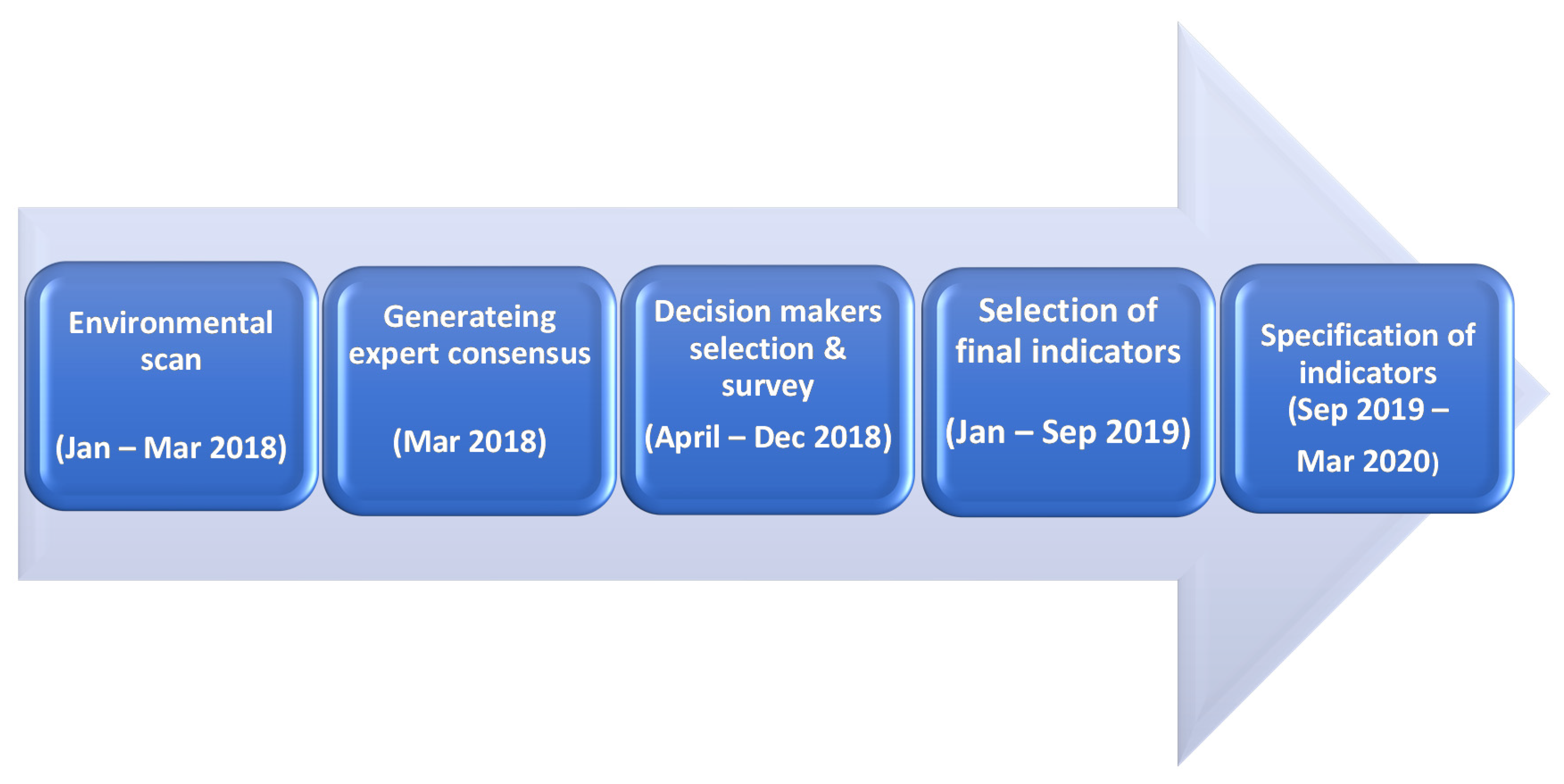
2.3. Indicator Development Process
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Haagsma, J.A.; Graetz, N.; Bolliger, I.; Naghavi, M.; Higashi, H.; Mullany, E.C.; Abera, S.F.; Abraham, J.P.; Adofo, K.; Alsharif, U. The global burden of injury: Incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj. Prev. 2016, 22, 3–18. [Google Scholar] [CrossRef]
- Haagsma, J.A.; James, S.L.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; Lucchesi, L.R.; Roberts, N.L.S.; Sylte, D.O. Burden of injury along the development spectrum: Associations between the Socio-demographic Index and disability-adjusted life year estimates from the Global Burden of Disease Study 2017. Inj. Prev. 2020, 26, i12–i26. [Google Scholar] [CrossRef] [PubMed]
- Yao, X.; Skinner, R.; McFaull, S.; Thompson, W. At-a-glance–2015 injury deaths in Canada. Health Promot. Chronic Dis. Prev. Can. 2019, 39, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Pike, I.; Rajabali, F.; Zheng, A. Potential Lost, Potential for Change. The Cost of Injury in Canada 2021; Parachute Canada: Toronto, ON, Canada, 2021. [Google Scholar]
- Piedt, S.; Rajabali, F.; Turcotte, K.; Barnett, B.; Pike, I. The British Columbia Casebook for Injury Prevention; BC Injury Research and Prevention Unit: Vancouver, BC, Canada, 2015. [Google Scholar]
- Belton, K.; Pike, I.; Heatley, J.; Cloutier, E.; Skinner, R. The Cost of Injury in Canada; Parachute: Toronto, ON, Canada, 2015. [Google Scholar]
- Rajabali, F.; Beaulieu, E.; Smith, J.; Pike, I. The economic burden of injuries in British Columbia: Applying evidence to practice. BC Med. J. 2018, 60, 358–364. [Google Scholar]
- Ministry of Health British Columbia. Promote, Protect, Prevent: Our Health Begins Here. BC’s Guiding Framework for Public Health. Available online: www.health.gov.bc.ca/library/publications/year/2017/BC-guiding-framework-for-public-health-2017-update.pdf (accessed on 15 July 2021).
- Scott, V.; Lockhart, S.; Gallagher, E.; Smith, D.; Asselin, G.; Belton, K. Canadian Falls Prevention Curriculum (CFPC); BC Injury Research and Prevention Unit: Vancouver, BC, Canada, 2007. [Google Scholar]
- Smith, J.; Zheng, X.; Lafreniere, K.; Pike, I. Social marketing to address attitudes and behaviours related to preventable injuries in British Columbia, Canada. Inj. Prev. 2018, 24, i52–i59. [Google Scholar] [CrossRef]
- Pike, I.; Piedt, S.; Lafreniere, K. 337 Social marketing to reduce preventable injuries in BC, Canada. Inj. Prev. 2016, 22, A123–A124. [Google Scholar] [CrossRef]
- Karbakhsh, M.; Beaulieu, E.; Smith, J.; Zheng, A.; Turcotte, K.; Pike, I. Public attitudes towards the preventability of transport and non-transport related injuries: Can a social marketing campaign make a difference? Prev. Med. Rep. 2019, 13, 179–182. [Google Scholar] [CrossRef]
- Lacombe, C.; Arason, N. British Columbia Road Safety Strategy 2015 and Beyond. Victoria: BC Ministry of Justice and Office of the Superintendent of Motor Vehicles. 2013. Available online: https://www2.gov.bc.ca/assets/gov/driving-and-transportation/driving/roadsafetybc/strategy/road-safety-strategy.pdf (accessed on 14 October 2021).
- Babul, S.; Turcotte, K.; Lambert, M.; Hadly, G.; Sadler, K. Delivering Evidence-Based Online Concussion Education to Medical and Healthcare Professionals: The Concussion Awareness Training Tool (CATT). J. Sports Med. 2020, 2020, 8896601. [Google Scholar] [CrossRef]
- Babul, S. Addressing the need for standardized concussion care in Canada: Concussion Awareness Training Tool. Can. Fam. Physician 2015, 61, 660–662. [Google Scholar]
- Richmond, S.A.; Bruin, S.; Black, A.M.; Pike, I.; Babul, S. Active & Safe Central: Using a mixed-methods design and the RE-AIM framework to evaluate a sport and recreational injury prevention resource for practitioners in Canada. BMJ Open 2021, 11, e039070. [Google Scholar] [PubMed]
- Frieden, T.R. Six components necessary for effective public health program implementation. Am. J. Public Health 2014, 104, 17–22. [Google Scholar] [CrossRef]
- Hanson, D.W.; Finch, C.F.; Allegrante, J.P.; Sleet, D. Closing the gap between injury prevention research and community safety promotion practice: Revisiting the public health model. Public Health Rep. 2012, 127, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, A.; Lloyd, D.G.; Gabbe, B.J.; Cook, J.; Finch, C.F. We have the programme, what next? Planning the implementation of an injury prevention programme. Inj. Prev. 2017, 23, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.S.; Wilkins, N. Mind the gap: Approaches to addressing the research-to-practice, practice-to-research chasm. J. Public Health Manag. Pract. 2018, 24, S6. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.S.; Wilkins, N.; Marshall, S.W.; Dellapenna Jr, A.; Pressley, J.C.; Bauer, M.; South, E.C.; Green, K. The power of academic-practitioner collaboration to enhance science and practice integration: Injury and violence prevention case studies. J. Public Health Manag. Pract. 2018, 24, S67. [Google Scholar] [CrossRef]
- Green, L.W. Closing the chasm between research and practice: Evidence of and for change. Health Promot. J. Austr. 2014, 25, 25–29. [Google Scholar] [CrossRef]
- BC Injury Prevention Committee (BCIPC). Provincial Injury Prevention Priorities. Available online: http://www.bccdc.ca/pop-public-health/Documents/bcipc-provincial-injury-prevention-priorities-2017.pdf (accessed on 14 October 2021).
- Rajabali, F.; Ibrahimova, A.; Barnett, B.; Pike, I. Economic Burden of Injury in British Columbia; BC Injury Research and Prevention Unit: Vancouver, BC, Canada, 2015. [Google Scholar]
- Freebairn, L.; Atkinson, J.-A.; Kelly, P.M.; McDonnell, G.; Rychetnik, L. Decision makers’ experience of participatory dynamic simulation modelling: Methods for public health policy. BMC Med. Inform. Decis. Mak. 2018, 18, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Armstead, T.L.; Wilkins, N.; Doreson, A. Indicators for evaluating community-and societal-level risk and protective factors for violence prevention: Findings from a review of the literature. J. Public Health Manag. Pract. 2018, 24, S42. [Google Scholar] [CrossRef]
- Pan American Health Organization. Health Indicators. Conceptual and Operational Considerations. Available online: https://iris.paho.org/handle/10665.2/49056 (accessed on 14 October 2021).
- Hanley, J. Edwin Chadwick and the poverty of statistics. Med. Hist. 2002, 46, 21–40. [Google Scholar] [CrossRef][Green Version]
- Szreter, S. The population health approach in historical perspective. Am. J. Public Health 2003, 93, 421–431. [Google Scholar] [CrossRef]
- Etches, V.; Frank, J.; Ruggiero, E.D.; Manuel, D. Measuring population health: A review of indicators. Annu. Rev. Public Health 2006, 27, 29–55. [Google Scholar] [CrossRef] [PubMed]
- Von Schirnding, Y. Health in Sustainable Development Planning: The Role of Indicators. Available online: https://apps.who.int/iris/handle/10665/67391 (accessed on 14 October 2021).
- Cryer, C. ICE Injury Indicator Group (ICEIInG)-progress report, aspirations, goals and strategy development. In International Collaborative Effort on Injury Statistics; NCHS, CDC, US Department of Health and Human Services: Washington, DC, USA, 2003. [Google Scholar]
- Cryer, C.; Langley, J.D.; Jarvis, S.N.; Mackenzie, S.G.; Stephenson, S.C.R.; Heywood, P. Injury outcome indicators: The development of a validation tool. Inj. Prev. 2005, 11, 53–57. [Google Scholar] [CrossRef]
- Lyons, R.A.; Brophy, S.; Pockett, R.; John, G. Purpose, development and use of injury indicators. Int. J. Inj. Contr. Saf. Promot. 2005, 12, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Pike, I.; Smith, J.; Al-Hajj, S.; Fuselli, P.; Macpherson, A. The Canadian atlas of child and youth injury: Mobilizing injury surveillance data to launch a national knowledge translation tool. Int. J. Environ. Res. Public Health 2017, 14, 982. [Google Scholar] [CrossRef] [PubMed]
- MacKay, J.M.; Macpherson, A.K.; Pike, I.; Vincenten, J.; McClure, R. Action indicators for injury prevention. Inj. Prev. 2010, 16, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.E.; Johnson, R.L. State Injury Indicators Report: Instructions for Preparing 2019 Data; Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta, GA, USA, 2021.
- McClure, R.J.; Mack, K.; Wilkins, N.; Davey, T.M. Injury prevention as social change. Inj. Prev. 2016, 22, 226–229. [Google Scholar] [CrossRef]
- Gozt, A.; Licari, M.; Halstrom, A.; Milbourn, H.; Lydiard, S.; Black, A.; Arendts, G.; Macdonald, S.; Song, S.; MacDonald, E. Towards the development of an integrative, evidence-based suite of indicators for the prediction of outcome following mild traumatic brain injury: Results from a pilot study. Brain Sci. 2020, 10, 23. [Google Scholar] [CrossRef]
- McClure, R.J.; Peel, N.; Kassulke, D.; Neale, R. Appropriate indicators for injury control? Public Health 2002, 116, 252–256. [Google Scholar] [CrossRef]
- Lindsay, P.; Schull, M.; Bronskill, S.; Anderson, G. The development of indicators to measure the quality of clinical care in emergency departments following a modified-Delphi approach. Acad. Emerg. Med. 2002, 9, 1131–1139. [Google Scholar] [CrossRef] [PubMed]
- Pike, I.; Piedt, S.; Warda, L.; Yanchar, N.; Macarthur, C.; Babul, S.; Macpherson, A.K. Developing injury indicators for Canadian children and youth: A modified-delphi approach. Inj. Prev. 2010, 16, 154–160. [Google Scholar] [CrossRef]
- Pike, I.; McDonald, R.J.; Piedt, S.; Macpherson, A.K. Developing injury indicators for First Nations and Inuit children and youth in Canada: A modified Delphi approach. Chronic Dis. Inj. Can. 2014, 34, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.; Samarakkody, D.; Oakey, M.; Fyfe, M.; Turcotte, K.; Pike, I. Provincial priority setting approach to injury prevention in British Columbia, Canada. Inj. Prev. 2018, 24, A3. [Google Scholar]
- Cryer, C.; Langley, J.D. Developing valid indicators of injury incidence for “all injury”. Inj. Prev. 2006, 12, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Cryer, C.; Davie, G.S.; Gulliver, P.J.; Petridou, E.T.; Dessypris, N.; Lauritsen, J.; Macpherson, A.K.; Miller, T.R.; De Graaf, B. Empirical validation of the New Zealand serious non-fatal injury outcome indicator for ‘all injury’. Inj. Prev. 2018, 24, 300–304. [Google Scholar] [CrossRef]
- Rigby, M.J.; Köhler, L.I.; Blair, M.E.; Metchler, R. Child health indicators for Europe: A priority for a caring society. Eur. J. Public Health 2003, 13, 38–46. [Google Scholar] [CrossRef]
- Pike, I.; Macpherson, A.; Warda, L.; Yanchar, N.; Hewitt, A.; Fuselli, P.; Babul, S.; Desapriya, E.; Macarthur, C.; Hameed, S.M.; et al. Measuring Injury Matters: Injury Indicators for Children and Youth in Canada. Vol1. Can. Inj. Indic. Dev. Team 2010. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Khan, Y.; Brown, A.D.; Gagliardi, A.R.; O’Sullivan, T.; Lacarte, S.; Henry, B.; Schwartz, B. Are we prepared? The development of performance indicators for public health emergency preparedness using a modified Delphi approach. PLoS ONE 2019, 14, e0226489. [Google Scholar] [CrossRef]
- World Health Organization. Global Reference List of 100 Core Health Indicators. Available online: https://apps.who.int/iris/bitstream/handle/10665/173589/WHO_HIS_HSI_2015.3_eng.pdf (accessed on 14 October 2021).
- Government of Australia. National Road Safety Strategy—The Safe System Principles. Available online: https://www.roadsafety.gov.au/nrss/safe-system.aspx (accessed on 14 October 2021).
- Australian Transport Counsil. National Road Safety Strategy 2011–2020. Available online: https://apo.org.au/sites/default/files/resource-files/2011-05/apo-nid55370.pdf (accessed on 14 October 2021).
- Naumann, R.B.; Sandt, L.; Kumfer, W.; LaJeunesse, S.; Heiny, S.; Lich, K.H. Systems Thinking in the Context of Road Safety: Can Systems Tools Help us Realize a True “Safe Systems” Approach? Curr. Epidemiol. Rep. 2020, 7, 343–351. [Google Scholar] [CrossRef]
- Arason, N. Canada and the Safe Systems Approach to Road Safety. Inst. Transp. Eng. ITE J. 2019, 89, 26–30. [Google Scholar]
- McClure, R.J.; Cameron, C.M.; Purdie, D.M.; Kliewer, E. V Indicators of injury burden: Which types are the most important? Int. J. Inj. Contr. Saf. Promot. 2005, 12, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Mitton, C.; Macnab, Y.C.; Smith, N.; Foster, L. Injury data in British Columbia: Policy maker perspectives on knowledge transfer. Chronic Dis. Can. 2009, 29, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Cryer, C.; Langley, J.D.; Stephenson, S.C.R.; Jarvis, S.N.; Edwards, P. Measure for measure: The quest for valid indicators of non-fatal injury incidence. Public Health 2002, 116, 257–262. [Google Scholar] [CrossRef]
- McClure, R. Catalyzing state public health agency actions to prevent injuries and violence: Introductory remarks. J. Public Health Manag. Pract. 2018, 24, S1. [Google Scholar] [CrossRef]
- Turner, S.L.; Lyons, J.; Lyons, R.A. Development of an Injury Indicator Tool to Support Policy and Practice across Wales. Int. J. Popul. Data Sci. 2019, 4, 108. [Google Scholar] [CrossRef]
- Brownson, R.C.; Royer, C.; Ewing, R.; McBride, T.D. Researchers and policymakers: Travelers in parallel universes. Am. J. Prev. Med. 2006, 30, 164–172. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
| Criteria | Description |
|---|---|
| Importance | The indicator measures an injury issue that is large; is trending; has a major life impact affecting a B.C. population; is urgent; and has ethical/social justice/equity impacts |
| Modifiability | The indicator will measure evidence-informed injury interventions or sets of evidence-informed injury prevention interventions and the extent to which we are changing the conditions that contribute to final health and safety outcomes |
| Acceptance | The indicator measures an evidence-informed injury prevention intervention supported by and understood by public, government municipality, and other relevant stakeholders |
| Practicality | The indicator measures an intervention (current or potential) that is practical and feasible to implement in the B.C. context |
| Grouped (‘Like’) Indicators | Included Indicators * |
|---|---|
| 1. Access to timely and appropriate care | O1,2 |
| 2. Road-related fatalities | O3-5 |
| 3. Road-related serious injuries | O6,7 |
| 4. Road-related ED visits | O11 |
| 5. Automated Speed enforcement | SS1,2; SRU2-4 |
| 6. Speed compliance | SS5-8 |
| 7. Signalised intersection safety | SRU5,6 |
| 8. Designated heavy truck traffic route | SR8 |
| 9. Pedestrian safety in school zones | SR1 |
| 10. Pedestrian safety | SR2, SR3 |
| 11. Enhanced road designs | SR4, SR5 |
| 12. Passive safety technology | SV1 |
| 13. Traffic enforcement | SRU1 |
| 14. Traffic legislative initiatives to enhance traffic safety | SRU7-9 |
| 15. Traffic violations | SRU10-14 |
| 16. Safe and unsafe driving behaviours | SRU15-17 |
| 17. Active transportation | SRU18,19 |
| 18. Unsafe speed and traffic crashes | O8-10 |
| 19. Speeding related vehicle impoundments | SS3 |
| 20. Evidence-based speed limit approach | SS4 |
| 21. Unprotected and protected on-road bike lanes | SR6 |
| 22. Multi-use pathway | SR7 |
| 23. Road-related injury costs | HS18-20 # |
| 1. Fall-related fatalities | HS1 |
| 2. Fall-related injury hospitalization | HS2,3 |
| 3. Fall-related ED visits and repeat visits | HS4,5 |
| 4. Fall-related costs | HS6-8 |
| 5. Wait time for surgery | HS9 |
| 6. Health service coverage | HSC1-3 |
| 7. Fall prevention designated staff | PLC1 |
| 8. Availability of fall prevention resources and plans | PLC2-6 |
| 9. Number and rate of unintentional injury fatalities | HS1-3 |
| 10. Number and rate of unintentional injury hospitalizations | HS4,5; HS10-12 |
| 11. ED visits for unintentional injuries | HS13-15 |
| 12. PYLL, DALY, and cost of injury | HS17-20 |
| 13. Poisoning helpline utilization | AI11 |
| 1. Self-reported unintentional injuries | HS16 |
| 2. Treatment coverage for substance use | HS21 |
| 3. Percentage of adult binge drinking | AI1 |
| 4. Communities with access to water safety programs | AI3,4 |
| 5. Injury prevention legislation and policy 1 | AI5-8 |
| 6. Injury prevention legislation and policy 2 | AI9 |
| 7. Percentage of bicycle helmet use | AI10 |
| 8. Availability of fire and ambulance services | AI12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oakey, M.; Evans, D.C.; Copley, T.T.; Karbakhsh, M.; Samarakkody, D.; Brubacher, J.R.; Pawer, S.; Zheng, A.; Rajabali, F.; Fyfe, M.; et al. Development of Policy-Relevant Indicators for Injury Prevention in British Columbia by the Key Decision-Makers. Int. J. Environ. Res. Public Health 2021, 18, 11837. https://doi.org/10.3390/ijerph182211837
Oakey M, Evans DC, Copley TT, Karbakhsh M, Samarakkody D, Brubacher JR, Pawer S, Zheng A, Rajabali F, Fyfe M, et al. Development of Policy-Relevant Indicators for Injury Prevention in British Columbia by the Key Decision-Makers. International Journal of Environmental Research and Public Health. 2021; 18(22):11837. https://doi.org/10.3390/ijerph182211837
Chicago/Turabian StyleOakey, Megan, David C. Evans, Tobin T. Copley, Mojgan Karbakhsh, Diana Samarakkody, Jeff R. Brubacher, Samantha Pawer, Alex Zheng, Fahra Rajabali, Murray Fyfe, and et al. 2021. "Development of Policy-Relevant Indicators for Injury Prevention in British Columbia by the Key Decision-Makers" International Journal of Environmental Research and Public Health 18, no. 22: 11837. https://doi.org/10.3390/ijerph182211837
APA StyleOakey, M., Evans, D. C., Copley, T. T., Karbakhsh, M., Samarakkody, D., Brubacher, J. R., Pawer, S., Zheng, A., Rajabali, F., Fyfe, M., & Pike, I. (2021). Development of Policy-Relevant Indicators for Injury Prevention in British Columbia by the Key Decision-Makers. International Journal of Environmental Research and Public Health, 18(22), 11837. https://doi.org/10.3390/ijerph182211837






