Association between Neighborhood Social Deprivation and Stage at Diagnosis among Breast Cancer Patients in South Carolina
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
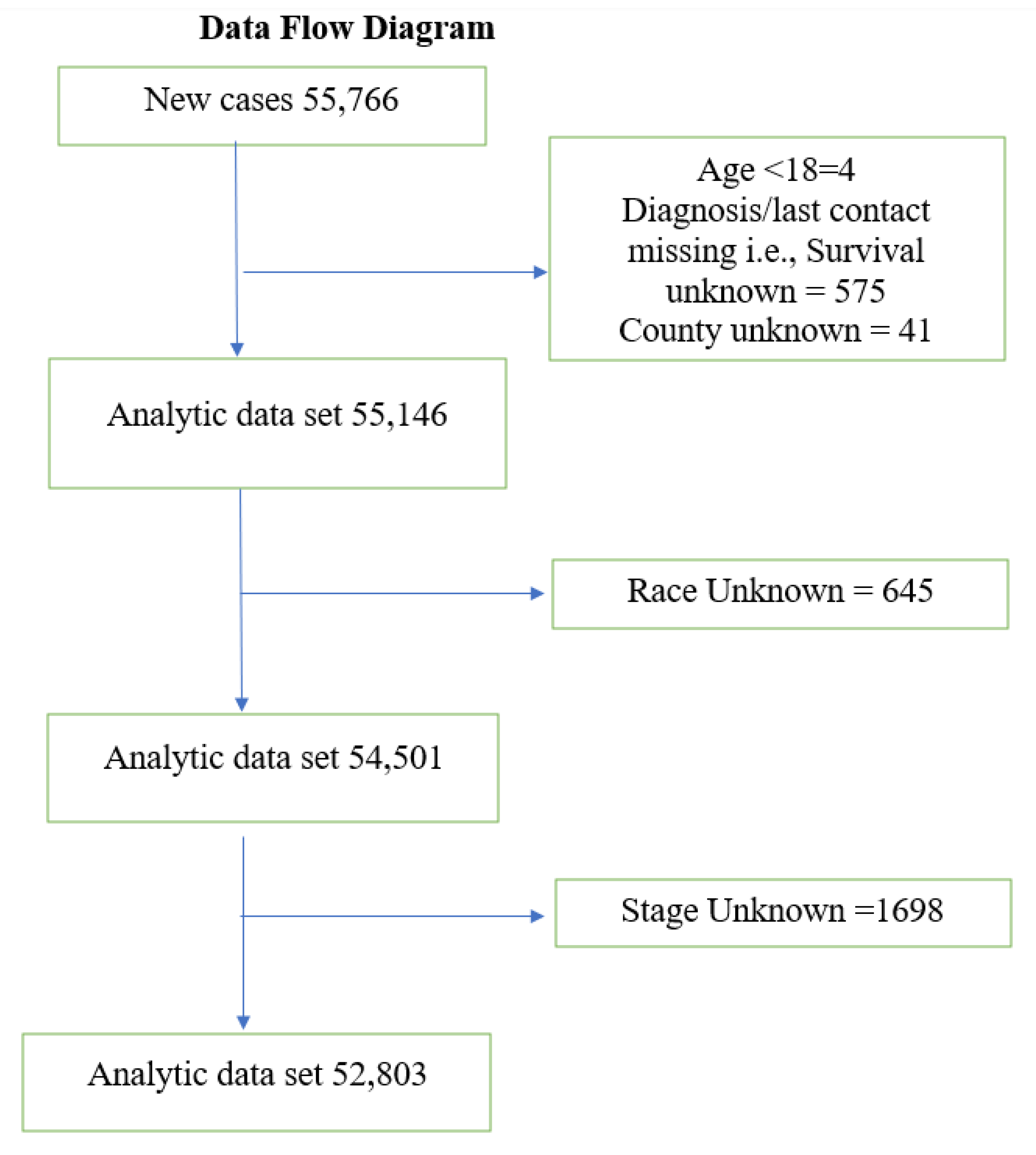
2.2. Inclusion and Exclusion Criteria
2.3. Predictor Variables
2.4. Outcome Variable
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Brill, J.V. Screening for cancer: The economic, medical, and psychosocial issues. Am. J. Manag. Care 2020, 26 (Suppl. 14), S300–S306. [Google Scholar]
- Zahnd, W.E.; Sherman, R.L.; Klonoff-Cohen, H.; McLafferty, S.L.; Farner, S.; Rosenblatt, K.A. Breast cancer staging by subtype in the Lower Mississippi Delta region States. Cancer Epidemiol. 2019, 63, 101624. [Google Scholar] [CrossRef]
- Markossian, T.W.; Hines, R.B. Disparities in late stage diagnosis, treatment, and breast cancer-related death by race, age, and rural residence among women in Georgia. Women Health 2012, 52, 317–335. [Google Scholar] [CrossRef] [PubMed]
- Williams, F.; Thompson, E. Disparity in Breast Cancer Late Stage at Diagnosis in Missouri: Does Rural Versus Urban Residence Matter? J. Racial Ethn. Health Disparities 2016, 3, 233–239. [Google Scholar] [CrossRef]
- Akinyemiju, T.; Moore, J.X.; Ojesina, A.I.; Waterbor, J.W.; Altekruse, S.F. Racial disparities in individual breast cancer outcomes by hormone-receptor subtype, area-level socio-economic status and healthcare resources. Breast Cancer Res. Treat. 2016, 157, 575–586. [Google Scholar] [CrossRef] [PubMed]
- Klassen, A.C.; Pankiewicz, A.; Hsieh, S.; Ward, A.; Curriero, F.C. The association of area-level social class and tobacco use with adverse breast cancer characteristics among white and black women: Evidence from Maryland, 1992–2003. Int. J. Health Geogr. 2015, 14, 13. [Google Scholar] [CrossRef] [Green Version]
- Spada, N.G.; Geramita, E.M.; Zamanian, M.; van Londen, G.J.; Sun, Z.; Sabik, L.M. Changes in Disparities in Stage of Breast Cancer Diagnosis in Pennsylvania After the Affordable Care Act. J. Womens Health 2020, 30, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Weis, K.E.; Liese, A.D.; Hussey, J.; Gibson, J.J.; Duffus, W.A. Associations of rural residence with timing of HIV diagnosis and stage of disease at diagnosis, South Carolina 2001–2005. J. Rural Health 2010, 26, 105–112. [Google Scholar] [CrossRef]
- Butler, D.C.; Petterson, S.; Phillips, R.L.; Bazemore, A.W. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv. Res. 2013, 48 Pt 1, 539–559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, B.P.; Madak-Erdogan, Z. Urban Neighborhood and Residential Factors Associated with Breast Cancer in African American Women: A Systematic Review. Horm. Cancer 2018, 9, 71–81. [Google Scholar] [CrossRef]
- Lian, M.; Pérez, M.; Liu, Y.; Schootman, M.; Frisse, A.; Foldes, E.; Jeffe, D.B. Neighborhood socioeconomic deprivation, tumor subtypes, and causes of death after non-metastatic invasive breast cancer diagnosis: A multilevel competing-risk analysis. Breast Cancer Res. Treat. 2014, 147, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Babatunde, O.A.; Eberth, J.M.; Felder, T.; Moran, R.; Truman, S.; Hebert, J.R.; Zhang, J.; Adams, S.A. Social Determinants of Racial Disparities in Breast Cancer Mortality Among Black and White Women. J. Racial Ethn. Health Disparities 2020, 8, 147–156. [Google Scholar] [CrossRef]
- Moriceau, G.; Bourmaud, A.; Tinquaut, F.; Oriol, M.; Jacquin, J.P.; Fournel, P.; Magne, N.; Chauvin, F. Social inequalities and cancer: Can the European deprivation index predict patients’ difficulties in health care access? A pilot study. Oncotarget 2016, 7, 1055–1065. [Google Scholar] [CrossRef] [Green Version]
- Robert Graham Center. Social Deprivation Index: Background, Definition, Methodology 2020. Available online: https://www.graham-center.org/rgc/maps-data-tools/sdi/social-deprivation-index.html (accessed on 3 October 2020).
- Roseland, M.E.; Schwartz, K.; Ruterbusch, J.J.; Lamerato, L.; Krajenta, R.; Booza, J.; Simon, M.S. Influence of clinical, societal, and treatment variables on racial differences in ER-/PR- breast cancer survival. Breast Cancer Res. Treat. 2017, 165, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Surveillance, Epidemiology, and End Results (SEER). SEER Summary Staging Manual-2000: Codes and Coding Instructions. Available online: https://seer.cancer.gov/tools/ssm/SSM2018-BREAST.pdf (accessed on 12 June 2020).
- Stafford, M.; Marmot, M. Neighbourhood deprivation and health: Does it affect us all equally? Int. J. Epidemiol. 2003, 32, 357–366. [Google Scholar] [CrossRef] [Green Version]
- Diez Roux, A.V.; Mair, C. Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef] [Green Version]
- Celaya, M.O.; Rees, J.R.; Gibson, J.J.; Riddle, B.L.; Greenberg, E.R. Travel distance and season of diagnosis affect treatment choices for women with early-stage breast cancer in a predominantly rural population (United States). Cancer Causes Control 2006, 17, 851–856. [Google Scholar] [CrossRef]
- Gentil, J.; Dabakuyo, T.S.; Ouedraogo, S.; Poillot, M.L.; Dejardin, O.; Arveux, P. For patients with breast cancer, geographic and social disparities are independent determinants of access to specialized surgeons. A eleven-year population-based multilevel analysis. BMC Cancer 2012, 12, 351. [Google Scholar] [CrossRef]
- Osborne, C.; Ostir, G.V.; Du, X.; Peek, M.K.; Goodwin, J.S. The influence of marital status on the stage at diagnosis, treatment, and survival of older women with breast cancer. Breast Cancer Res. Treat. 2005, 93, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Babatunde, O.A.; Eberth, J.M.; Felder, T.M.; Moran, R.; Hughes-Halbert, C.; Truman, S.; Hebert, J.R.; Heiney, S.; Adams, S.A. Racial Disparities and Diagnosis-to-Treatment Time Among Patients Diagnosed with Breast Cancer in South Carolina. J. Racial Ethn. Health Disparities 2021. [Google Scholar] [CrossRef]
- Leung, J.; Smith, M.D.; McLaughlin, D. Inequalities in long term health-related quality of life between partnered and not partnered breast cancer survivors through the mediation effect of social support. Psychooncology 2016, 25, 1222–1228. [Google Scholar] [CrossRef] [PubMed]
- Babatunde, O.A.; Adams, S.A.; Wirth, M.D.; Eberth, J.M.; Sofge, J.; Choi, S.K.; Harmon, B.E.; Davis, L.; Drayton, R.; Hurley, T.G.; et al. Predictors of Retention among African Americans in a Randomized Controlled Trial to Test the Healthy Eating and Active Living in the Spirit (HEALS) Intervention. Ethn. Dis. 2017, 27, 265–272. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Health and Human Services. Healthy People 2030. Building a Healthier Future for All. Available online: https://health.gov/healthypeople (accessed on 18 August 2021).
- Dillon, E.C.; Kim, P.; Li, M.; Huang, Q.; Colocci, N.; Cantril, C.; Hung, D.Y. Breast Cancer Navigation: Using Physician and Patient Surveys to Explore Nurse Navigator Program Experiences. Clin. J. Oncol. Nurs. 2021, 25, 579–586. [Google Scholar] [CrossRef]
- Glassman, B. The Multidimensional Deprivation Index Using Different Neighborhood Quality Definitions. Poverty Statistics Branch. Social, Economic, and Housing Statistics Division. U.S. Census Bureau. SEHSD Working Paper Number 2020-08. Available online: https://www.census.gov/content/dam/Census/library/working-papers/2020/demo/SEHSD-WP2020-08.pdf (accessed on 31 October 2021).
- Hofferkamp, J. Standards for Cancer Registries Volume III. Standards for Completeness, Quality, Analysis, Management, Security and Confidentiallity of Data. 2008. Available online: https://www.naaccr.org/wp-content/uploads/2016/11/Standards-for-Completeness-Quality-Analysis-Management-Security-and-Confidentiality-of-Data-August-2008PDF.pdf (accessed on 18 August 2021).
| Stage at Cancer Diagnosis | |||||
|---|---|---|---|---|---|
| Overall (n = 52,803) | Localized (n = 32,739) | Regional (n = 17,201) | Distant (n = 2863) | p-Value 1 | |
| Age, mean (SD) | 60.9 (13.6) | 62.2 (13.4) | 58.6 (13.8) | 61.2 (14.3) | <0.01 |
| Race | |||||
| African American | 13,013 (24.6) | 6889 (52.9) | 5107 (39.2) | 1017 (7.8) | <0.01 |
| White | 39,790 (75.4) | 25,850 (65.0) | 12,094 (30.4) | 1846 (4.6) | |
| Married | |||||
| No | 19,620 (36.2) | 11,770 (60.0) | 6528 (33.3) | 1322 (6.7) | <0.01 |
| Yes | 26,831 (50.8) | 17,039 (63.5) | 8695 (32.4) | 1097 (4.1) | |
| Unknown | 6352 (12.0) | 3930 (61.9) | 1978 (31.1) | 444 (7.0) | |
| Tumor grade | |||||
| Well differentiated | 10,183 (19.3) | 8069 (79.2) | 1960 (19.3) | 154 (1.5) | <0.01 |
| Moderately differentiated | 19,683 (37.3) | 12,494 (63.5) | 6403 (32.5) | 786 (4.0) | |
| Poorly differentiated | 17,643 (33.4) | 9172 (52.0) | 7320 (41.5) | 1151 (6.5) | |
| Undifferentiated/Anaplastic | 656 (1.2) | 316 (48.2) | 290 (44.2) | 50 (7.6) | |
| Unknown | 4638 (8.8) | 2688 (58.0) | 1228 (26.5) | 722 (15.6) | |
| BCN participation | |||||
| Yes | 1196 (2.3) | 635 (53.1) | 503 (42.1) | 58 (4.9) | <0.01 |
| No | 51,607 (97.7) | 32,104 (62.2) | 16,698 (32.4) | 2805 (5.4) | |
| Composite SDI score, mean (SD) | 54.2 (18.0) | 53.7 (17.9) | 54.9 (18.2) | 55.1 (18.4) | <0.01 |
| 2 Composite SDI score category | |||||
| Lower deprivation | 29,377 (55.6) | 18,590 (63.3) | 9261 (31.5) | 1526 (5.2) | <0.01 |
| Higher deprivation | 23,426 (44.4) | 14,149 (60.4) | 7940 (33.9) | 1337 (5.7) | |
| 3 Healthcare Professional Shortage Area status mean (SD) | 14.4 (3.0) | 14.4 (3.0) | 14.5 (3.0) | 14.5 (3.0) | <0.01 |
| Healthcare Professional Shortage Area status category | |||||
| Lower shortage | 28,892 (54.7) | 18,245 (63.2) | 9124 (31.6) | 1523 (5.3) | <0.01 |
| Higher shortage | 23,911 (45.3) | 14,494 (60.6) | 8077 (33.8) | 1340 (5.6) | |
| Urban–rural designation | |||||
| Urban | 39,752 (75.3) | 24,776 (62.3) | 12,885 (32.4) | 2091 (5.2) | <0.01 |
| Rural | 13,051 (24.7) | 7963 (61.0) | 4316 (33.1) | 772 (5.9) | |
| Year of diagnosis | |||||
| 1996–2002 | 15,902 (30.1) | 9998 (30.5) | 5155 (30.0) | 749 (26.2) | <0.01 |
| 2003–2009 | 18,439 (34.9) | 11,269 (34.4) | 6168 (36.0) | 987 (34.5) | |
| 2010–2015 | 18,462 (35.0) | 11,472 (35.0) | 5863 (34.1) | 1127 (40.0) | |
| Distant | ||
|---|---|---|
| n = 2863 n (%) | Odds Ratio (95% Confidence Interval) | |
| Age | ||
| >60 | 1428 (49.9) | Reference |
| 41–60 | 1251 (43.7) | 1.35 (1.30–1.40) |
| 18–40 | 184 (6.4) | 1.52 (1.41–1.63) |
| Race | ||
| White | 1846 (4.6) | Reference |
| African American | 1017 (7.8) | 1.35 (1.29–1.41) |
| Married | ||
| Yes | 1097 (4.1) | Reference |
| No | 1322 (6.7) | 1.17 (1.13–1.22) |
| Tumor grade | ||
| Well differentiated | 154 (1.5) | Reference |
| Moderately differentiated | 786 (4.0) | 2.13 (2.02–2.26) |
| Poorly differentiated | 1151 (6.5) | 3.16 (2.98–3.34) |
| Undifferentiated/anaplastic | 50 (7.6) | 3.83 (3.27–4.49) |
| BCN participation | ||
| No | 2805 (5.4) | Reference |
| Yes | 58 (4.9) | 1.07 (0.96–1.20) |
| 2 Composite SDI score category | ||
| Lower deprivation | 1526 (5.2) | Reference |
| Higher deprivation | 1337 (5.7) | 1.06 (1.02–1.10) |
| Year of diagnosis | ||
| 1996–2002 | 749 (26.2) | Reference |
| 2003–2009 | 987 (34.5) | 1.15 (1.10–1.20) |
| 2010–2015 | 1127 (40.0) | 1.17 (1.13–1.22) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babatunde, O.A.; Zahnd, W.E.; Eberth, J.M.; Lawson, A.B.; Adams, S.A.; Boakye, E.A.; Jefferson, M.S.; Allen, C.G.; Pearce, J.L.; Li, H.; et al. Association between Neighborhood Social Deprivation and Stage at Diagnosis among Breast Cancer Patients in South Carolina. Int. J. Environ. Res. Public Health 2021, 18, 11824. https://doi.org/10.3390/ijerph182211824
Babatunde OA, Zahnd WE, Eberth JM, Lawson AB, Adams SA, Boakye EA, Jefferson MS, Allen CG, Pearce JL, Li H, et al. Association between Neighborhood Social Deprivation and Stage at Diagnosis among Breast Cancer Patients in South Carolina. International Journal of Environmental Research and Public Health. 2021; 18(22):11824. https://doi.org/10.3390/ijerph182211824
Chicago/Turabian StyleBabatunde, Oluwole Adeyemi, Whitney E. Zahnd, Jan M. Eberth, Andrew B. Lawson, Swann Arp Adams, Eric Adjei Boakye, Melanie S. Jefferson, Caitlin G. Allen, John L. Pearce, Hong Li, and et al. 2021. "Association between Neighborhood Social Deprivation and Stage at Diagnosis among Breast Cancer Patients in South Carolina" International Journal of Environmental Research and Public Health 18, no. 22: 11824. https://doi.org/10.3390/ijerph182211824
APA StyleBabatunde, O. A., Zahnd, W. E., Eberth, J. M., Lawson, A. B., Adams, S. A., Boakye, E. A., Jefferson, M. S., Allen, C. G., Pearce, J. L., Li, H., & Halbert, C. H. (2021). Association between Neighborhood Social Deprivation and Stage at Diagnosis among Breast Cancer Patients in South Carolina. International Journal of Environmental Research and Public Health, 18(22), 11824. https://doi.org/10.3390/ijerph182211824






