Abstract
Dentists’ perceptions about the stressfulness of clinical practice are well-documented, but literature on perceived stress and psychological distress experienced during the COVID-19 pandemic is scarce. This study aims to explore the emotions and attitudes, and the socio-demographic, dental, and COVID-related factors that are associated with the emergence of perceived stress and psychological distress that have been experienced by dentists during the COVID-19 pandemic. General demographic and dental-related data, and specific questions measuring the potential factors regarding dental professionals’ concerns and opinions about their professional circumstances during the pandemic, were electronically collected from 182 dental practitioners. Exploratory and confirmatory factor analyses were used to assess whether dentists’ emotions and attitudes during the pandemic measure the same construct: psychological distress, while linear regression models were built on the exploration of the effects of COVID-related factors on perceived stress and psychological distress. Facets of impulsiveness, lack of interest in social connections, emotional disengagement, mood swings, and acknowledgment of emotional exhaustion due to the pandemic, were measurements of the same construct and manifested in a singular factor: psychological distress. Two aspects, the fear of aerosol propagation and insecurities of financial status, increased the likelihood of the emergence of heightened levels of perceived stress and distress, while years spent in dental practice and age seemed to be protective factors against perceived stress and distress.
1. Introduction
At the end of 2019, in the Wuhan province of China, the spread of a new virus of the family Coronaviridae was detected. By March 2020, the rapid, global spread of SARS-CoV-2 (COVID-19) caused the World Health Organization (WHO) to categorize the pandemic as a public health emergency [1,2] during which, in contrast with public health guidance for previous pandemics [3,4], governments mandated dentists to postpone elective dental procedures and to concentrate solely on emergency patient care.
In general, dentists are known to function under stressful conditions [5,6], hence the need to identify risk factors that could impact upon the levels of psychological symptoms, such as the levels of perceived stress and distress experienced by dentists due to the unprecedented challenge of the COVID-19 pandemic, is in high demand. Dentists have already been shown to have elevated levels of subjective overload and psychological distress, which differed among countries due to social, cultural, and environment issues [7]. However, despite these differences, the assessment of psychological aspects, such as stress, in dental professionals is of high interest. The spread of the COVID-19 pandemic recently highlighted those major concerns and stressors that influence the different aspects of the professional and personal lives of dentists [8,9]. Complications for the dentistry profession may also have further, unknown, long-term impacts on clinical practice, dental education, and dental research [10,11].
Perceived stress represents the feelings or thoughts that an individual has about the level of stress they are under at a given point in time or over a given time period [12], while psychological distress can be regarded as a mental health condition characterized by a complex set of emotional/psychological symptoms, i.e., various somatic and psychological symptoms, such as the elevated levels of anxiety, depression or the feeling of burnout, and is accompanied with several stress-related, socio-demographic, and work-related risk factors [13].
Dentists are habitually at high risk of contagion and transmission of infection because of direct and indirect contact with blood, saliva and other biologic fluids in the oral cavity and airways [14], as well as the presence of bacteria and viruses in the aerosols created by dental procedures [15]. The instruments used in dental procedures produce significant aerosol dispersion [16,17]; therefore, direct and indirect contact transmission from particulate matter (PM), droplet inhalation, and fluid transfer would put dentists, team members and, indirectly, their families, at high risk of contagion [18,19].
Alterations to the dental facility are essential to remove PM dispersion. High levels of PM are shown to occur with the use of natural ventilation, as dental treatment rooms are typically of an open design. High-volume evacuation filters (HVE) and high-efficiency particulate-absorbing filtration (HEPA) are effective at removing PM; however, HVE requires the presence of auxiliary personnel and HEPA filters require constant maintenance to ensure that the unit does not become a source of pathogens [20,21]. The professional must continually strive to minimize the impact of aerosol-generating procedures and mitigate the possibility of bidirectional disease transmission [22].
As an occupational hazard, the risk of exposure to sources of infection, such as the human immune deficiency virus (HIV), tuberculosis (TB), and the hepatitis B virus (HBV), invariably heighten anxiety and work stressors [23]. Elevated levels of perceived risk are a function of the uncertainty of infection regardless of patient triage as the SARS-CoV-2 virus can spread from asymptomatic, symptomatic, and pre-symptomatic patients [24]. The use of a rubber dam, social distancing in treatment areas, and structural changes to a facility were essential in reducing contagion among dentists and patients. The use of teledentistry and online triage prior to appointments were shown to be of significant value in managing risk factors of infection. Despite these modifications and the use of improved personal protective equipment (PPE), dentists remained fearful of infection during treatment procedures [25].
Psychological variables, such as poor social support and a lack of self-efficacy, were reported as significant risk and contributory factors for the emergence of perceived stress and psychological distress in healthcare workers [26]. Based on the economic consequences of past pandemics, a global recessionary trend is to be expected as a result of travel restrictions, social distancing, and quarantine [27]. The career-related uncertainty posed by the novel virus could heighten levels of perceived stress and psychological distress [28,29] among dentists, who are in a profession identified as one of the most significant for stress, burnout, anxiety, and depression [30].
The literature on dentists and perceived stress primarily addresses those in training [31,32,33]. Furthermore, the literature on perceived stress and distress connected to the pandemic is scarce among licensed dental professionals [34]. The aim of the present study was to comprehensively assess the phenomenon of stress among dental professionals: to identify the possible risk factors behind the emergence of perceived stress and psychological distress, and to assess the contribution of these factors to them in dentists during the COVID-19 pandemic.
2. Materials and Methods
2.1. Participants and Procedure
Licensed dentists who are members of the Hungarian Dental Association were invited to answer an electronic test battery, to gather information about dentists’ attitudes, emotions, and information about their opinions regarding their practice after severe acute respiratory syndrome-Coronavirus-2 (SARS-CoV-2) lockdown. A total of 208 dentist replied. A total of 26 participants were excluded from final analysis; thus, 182 participants’ data were evaluated. The study was conducted in accordance with the Declaration of Helsinki, and it was approved by the Human Investigation Review Board, University of Szeged (ethical approval number: 27-XXVII-061-1/2021). Informed consent from each participant was also acquired online prior to participation in the survey.
2.2. Measures
The first section of the survey is composed of questions regarding demographic information: age, gender, residence, years of being a dental practitioner, place of practice, marital status, number of children, and financial status. In the second section, dentists filled out the Perceived Stress Scale, which is a self-assessment questionnaire including 14 questions to be rated on a 5-point Likert scale that reflected on stressful experiences in the past months [35]. The Hungarian adaptation proved to be valid and reliable [36]; internal consistency of the PSS on our sample was excellent (Cronbach’s α = 0.926).
Additionally, four specific questions were formed to measure potential factors regarding dental professionals’ concerns and opinions about the likelihood of infection and their professional futures in relation to COVID-19 and its potential consequences (see Table 1). Questions could be rated on a 5-point Likert scale ranging from 1—I disagree completely, 2—I disagree, 3—I neither agree nor disagree, 4—I agree to 5—I agree completely. Moreover, 12 questions regarding dentists’ emotions and attitude towards the SARS-CoV-2 pandemic were included. Items were rated on a 5-point Likert scale ranging from 1—never, 2—rarely, 3—sometimes, 4—often to 5—always (for the complete list of questions, see Table 2).

Table 1.
Demographic characteristics of the study sample of dental practitioners.

Table 2.
Descriptive statistics of survey questions.
2.3. Data Analysis
To explore whether the questions posed to dentists, regarding their emotions and attitude during the pandemic, measure the same construct (psychological distress). An exploratory factor analysis (EFA) with principal component analysis was used to test the structure of the presupposed Distress Factor; varimax rotation was selected to determine the factors under which each item loads. To identify the number of factors to be retained in the final model, the Kaiser method of factor retention, the evaluation of eigenvalues above 1, and a screen test were utilized. Item factor loadings were also evaluated, where a cutoff of 0.40 was applied for item inclusion. The goodness of fit of the components of the Distress Factor was tested with confirmatory factor analysis. The models were estimated through covariance matrices with the use of maximum likelihood estimation. Model fitness was evaluated by the following fit indices: chi-square (χ2), absolute, and incremental fit indices (RMSEA, TFI and CFI, respectively) and a parsimonious fit index (AIC). Since the χ2 value is sensitive to sample size, i.e., in case of larger samples, it is likely that reasonable models also result in statistically significant χ2 and p values [37,38,39,40], and thus previously mentioned fit indices were also considered (Byrne, 2005). The determination of a good fit is based on the following recommendation: CFI is above 0.95 and for RMSEA, above 0.06 [41]. The result of the factor analyses was used to create a new variable that measures dentists’ distress during the COVID-19 pandemic. To examine the effects of demographic variables, dental-specific questions on the likelihood that dentists experience perceived stress, and the hypothesized distress factor, linear logistic regressions were used with the stepwise regression method. Analyses were conducted with IBM SPSS v24 [42] and IBM AMOS v23 [43].
Dentists experienced psychological symptoms connected to the pandemic, which were predominantly restlessness, annoyance, sleep disturbance, and mood swings. The complete list of survey questions and descriptive statistical data are listed in Table 2.
3. Results
A total of 182 licensed dentists completed the survey and their data were further analyzed. Participants were between 24 and 81 years (mean: 50.93; SD: 13.67) with an average of almost 26 years spent working in a dental practice. Table 1 indicates detailed descriptive demographic characteristics of the sample.
The first 12 items were explored to see whether they measure the same a priori construct: psychological distress connected to the pandemic. Thus, to test whether these measured constructs fit the hypothesized measurement model, both an exploratory factor analysis (EFA) and a confirmatory factor analysis (CFA) were used.
3.1. Exploratory Factor Analysis
The sample size of the present study was sufficient for the analyses, since 182 participants filled out the 12-item survey, which fulfils the recommended 10:1, participant:item ratio [39]. Evaluation of the correlation matrix was significant in each case between item correlations of 0.113 to 0.710, Kaiser–Meyer–Olkin Measure of Sampling Adequacy (KMO = 0.909) and, the Bartlett’s test of sphericity (χ2(66) = 834.092, p ≤ 0.001) suggested that these items are connected but show enough variability to proceed with the principal component analysis. The Kaiser method of factor retention identified two factors with eigenvalues above 1, and a scree test for factor retention suggested a one-factor model; thus, the final model included one factor [44] (see Table 3).

Table 3.
Eigenvalues, extraction loadings and variances of one-factor and two-factor models.
The final model included one factor with all 12 items loading on one factor, with at least 0.441 loadings; communalities for each item were all moderate to high (see Table 4).

Table 4.
Final factor loadings and communalities.
3.2. Confirmatory Factor Analysis
The model was re-estimated with confirmatory factor analysis to assess model fitness. The fit indices of the one-factor model proved to be acceptable: Χ2 = 92.447, df = 54, Χ2/df = 1.712, p ≤ 0.001, CFI = 0.952, TLI = 0.931, RMSEA = 0.063, AIC = 164.447 (see Figure 1).
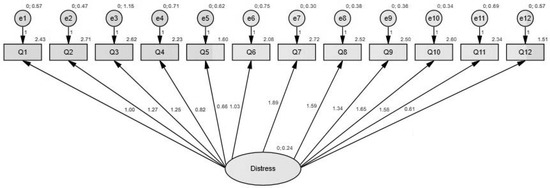
Figure 1.
Confirmatory factor analysis representing the latent variable (distress factor). The ellipse represents the latent variable (distress factor), boxes depict observed variables as follows: Q1: I am preoccupied by things that are not at all or slightly worrying; Q2: I get annoyed easily; Q3: I have trouble sleeping; Q4: I am indifferent towards various activities; Q5: I have barely any or no appetite; Q6: I feel emotionally distant from others; Q7: I feel restless; Q8: I feel sad; Q9: I feel angry; Q10: I have mood swings; Q11: I am noticing the signs of burnout; Q12: I employ addictive behaviour (smoking, drugs, alcohol) to cope with stress. Arrows pointing towards each observed variable represent factor loadings, while the values above each observed variable depict the explained variance.
Based on this, we created a new variable representing the standardized values of the psychological distress factor, where 0 refers to the convergence to the sample mean, negative values stand for lower level of distress, and positive values represent a higher level of experienced distress. Internal consistency on our sample was great (Cronbach’s α = 0.876).
3.3. Effects of COVID-Related Variables on Perceived Stress and Psychological Distress
Two stepwise linear regression models were built on exploring the effects of COVID-related factors on perceived stress and the result of the factor analyses: psychological distress. The first linear regression was carried out to evaluate whether the following predicted perceived stress: age, gender, residence, place of practice, marital status, number of children, financial status compared to national average, whether they felt that the COVID-19 pandemic will have long-lasting consequences on the financial situation of their practice, whether they felt that phone or online consultations would remain an integral part of their practice even after the COVID-19 pandemic would be under control, whether they felt that not even the strict compliance with professional rules can fully resolve the issues caused by aerosol propagation, and whether they felt that their personal professional development is facilitated by online education until the pandemic is significantly under control. The results of the regression model indicated that the final model explained 22.9% of the variance and was significant (F (1162) = 15.149, p ≤ 0.001). It was found that the following significantly predicted the level of perceived stress: financial status, number of years in practice, and the feeling that not even strict compliance with professional rules can fully resolve the issues caused by aerosol propagation.
The second linear regression was carried out to evaluate whether the following significantly predicted perceived psychological distress: age, gender, residence, place of practice, marital status, number of children, financial status compared to national average, whether they felt that the COVID-19 pandemic will have long-lasting consequences on the financial situation of their practice, whether they felt that phone or online consultations would remain an integral part of their practice even after the COVID-19 pandemic would be under control, whether they felt that not even the strict compliance with professional rules can fully resolve the issues caused by aerosol propagation, and whether they felt that their personal professional development would be facilitated by online education until the pandemic is under control. The results of the regression model indicated that the final model explained 14.9% of the variance and was significant (F (1163) = 7.496, p = 0.007. It was found that the following significantly predicted the level of psychological distress: age, financial status, and the feeling that not even the strict compliance with professional rules can fully resolve the issues caused by aerosol propagation (see Table 5).

Table 5.
Effects of COVID-related factors on perceived stress and psychological distress.
4. Discussion
The aim of this study was to reveal the background and potential risk factors of the level of perceived stress and psychological distress associated with the impact of COVID-19 among dentists. This work investigated the role of socio-demographic variables (gender, age, residence, years in practice, place of dental practice, marital status, number of children, and financial status) to ascertain which factors contribute to the appearance of elevated levels of perceived stress and psychological distress in connection with the COVID-19 lockdown.
Factor analysis was used to ascertain whether questions regarding dentists’ emotions and attitude during the pandemic measured the same construct: psychological distress. The present work points out that the psychological distress manifested in one factor, consisting of features of impulsiveness, lack of interest in social connections, emotional disengagement, mood swings, and acknowledgment of emotional exhaustion because of the pandemic. There are ample studies showing that dentists are prone to significant psychological distress due to the intense mental health stressors of clinical practice [45,46]. There is a paucity of the current literature addressing perceived stress (the lack of control and unpredictability in response to stressors) because of the pandemic [47,48].
The results indicated that aerosol propagation during dental procedures significantly promoted psychological symptoms, such as the elevated level of perceived stress and distress among dentists. In line with this, an in vitro study showed that the SARS-CoV-2 virus remained viable in aerosols for a minimum of 3 h with median estimates of half-life between 1.1 to 1.2 h [49]. Moreover, the virus persistently adheres and remains infectious from 2 h up to 9 days on various surfaces [50]. New infection control protocols are needed to mitigate the possibility of cross-contamination during and after the COVID-19 pandemic.
At the time of the present study, there were a lack of data about the SARS-CoV-2 virus transmission vectors in the dental office. Infection control measures were in a state of flux [51]: shortfalls in personal protective equipment (PPE) resulted in an anxiety regarding the heightened perceived stress of risk and consequence. This was further exacerbated by guidelines from government agencies regarding the nature and the mitigation of the virus [52].
It has been reported in the literature that acute COVID-19 infection could contribute to adverse outcomes concerning oral health due to impairment of the immune system. As shown by Dziedic and Wojtyczka, this could lead to xerostomia, opportunistic fungal infections, dysgeusia, unspecific oral ulcerations, recurrent oral herpes simplex (HSV-1), and ulcerative gingivitis due to the increase in susceptibility of the oral mucosa [53]. To date, while there is no scientific evidence that certifies which oral symptoms SARS-CoV-2 can cause, it is reasonable to assume that the oral manifestations described could be a warning sign of the presence of viral load [54].
The study found that uncertainty regarding income disruption was a significant contributing factor to perceived stress and psychological distress. Financial stress and anxiety are contributory factors to cognitive dysfunction, which could amplify levels of perceived stress [55]. While dentists did feel a moral and professional obligation to care for their patients, the financial consequences of practice closure in the short- and long-term were seen as an a priori source of psychological distress [56].
In countries throughout the world, diminished production and lost income due to government-mandated stoppage of elective treatment caused high levels of distress, due to the costs to restructure a practice physical facility, the need to replace PPE after each patient, and stringent infection controls that reduced the number of available appointment times [57]. The pandemic has irrevocably altered the practice of dentistry. Opportunities are available for dental researchers to focus on the cost/benefit ratio of expanded PPE use and other changes in workflows that could be of significance in the mitigation of perceived stress and distress in a workplace environment in the future. Those in solo private practice [58] experienced higher levels of distress than those dentists in governmental hospitals or institutions [59,60] as their earning potential, while greater, is not contractual [61].
Regarding age and years spent in clinical practice, results of this work conformed to the previous literature [62], since these factors have been shown to be protective against perceived stress and psychological distress. Regarding time in practice as a function of perceived stress and distress, the biologic and economic problems associated with the current pandemic were not evident in previous pandemics, particularly among healthcare providers [63,64].
Dental professionals with more work experience were less likely to report fear of changes in the work environment, fear of being infected and infecting others [65]. Less work-related distress could be explained by increased self-confidence among dentists with more work experience [66]. Given the fluctuating dynamics of a dental career, younger clinicians are particularly susceptible to perceived stress [67] and psychological distress, due to concerns regarding fewer job prospects. As repeated lockdowns have been necessary through 2020 and 2021 due to surges in case numbers and variants of the virus, the continued effect on the global economy could sustain increasing levels of anxiety, perceived stress, and distress amongst dentists of any age and gender as to their future vision of their careers [68].
This study has several limitations. The data were self-reported during the early months of the pandemic. As the dynamic nature of the pandemic was associated with repeated modifications of infection controls, it is important to consider the knowledge level of participants in this study within the time frame of response to the questionnaire. Another limitation is that the present study did not incorporate gender disaggregation, for which further studies with increased sample sizes would be necessary to underscore the robustness of the identified distress factor by gender disaggregated analysis. Additionally, further research will be necessary to determine the perceived stress and distress associated with the long-term impact of the financial, psychological, and professional outcomes of the pandemic, especially as the pandemic continues unabated. It is reasonable to assume that this could be of concern to dentists both currently and after the control of the spread and contagion of the pandemic. [69,70].
5. Conclusions
This study provided an understanding of two aspects of stress, perceived stress and psychological distress, among dentists during the COVID-19 pandemic. Psychological distress was operationalized by features reflecting on impulsiveness, lack of interest in social connection, emotional disengagement, mood swings, and acknowledgment of emotional exhaustion. Two major risk factors were identified in both aspects of stress: the fear of aerosol propagation and concerns about financial status. Fear of aerosol propagation and insecurities of financial status both increased the likelihood of the emergence of heightened levels of perceived stress and distress. Years spent in dental practice and age seemed to be protective factors against perceived stress and distress. Since dental professionals are proven to be highly prone to distress and perceived stress, measures should be taken that ascertain the factors that are likely to elevate the level of these psychological symptoms.
The increasing frequency of global pandemics since the turn of the century warrants aggressive iterations of PPE equipment and modified treatment protocols to minimize aerosol propagation. It is advisable for the dentistry profession to provide mental health support systems for clinicians to mitigate the effects of perceived stress and psychological distress in the long term.
Author Contributions
Conceptualization, K.S.S., K.N., B.A. and I.K.; Methodology, I.K. and B.A.; Software, I.K.; Validation, I.K.; Formal Analysis, I.K.; Investigation, K.S.S., and K.N.; Resources, I.K.; Data Curation, I.K.; Writing—Original Draft Preparation, K.S.S., I.K., B.A. and K.N.; Writing—Review & Editing, K.S.S., I.K., B.A. and K.N.; Visualization, I.K. and K.S.S.; Supervision, B.A., K.N. and I.K.; Project Administration, K.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Human Investigation Review Board, University of Szeged (ethical approval number: 27-XXVII-061-1/2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflict of interest.
References
- She, J.; Jiang, J.; Ye, L.; Hu, L.; Bai, C.; Song, Y. 2019 novel coronavirus of pneumonia in Wuhan, China: Emerging attack and management strategies. Clin. Transl. Med. 2020, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. COVID19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ 2020, 368, m1036. [Google Scholar] [CrossRef] [Green Version]
- Ayers, K.M.; Thomson, W.M.; Newton, J.T.; Rich, A.M. Job stressors of New Zealand dentists and their coping strategies. Occup. Med. 2008, 58, 275–281. [Google Scholar] [PubMed] [Green Version]
- Rada, R.E.; Johnson-Leong, C. Stress, burnout, anxiety, and depression among dentists. J. Am. Dent. Assoc. 2004, 135, 788–794. [Google Scholar] [CrossRef] [Green Version]
- Maunder, R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: Lessons learned. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2004, 359, 1117–1125. [Google Scholar] [CrossRef] [Green Version]
- Maunder, R.G.; Lancee, W.J.; Rourke, S.; Hunter, J.J.; Goldbloom, D.; Balderson, K.; Petryshen, P.; Steinberg, R.; Wasylenski, D.; Koh, D.; et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004, 66, 938–942. [Google Scholar] [CrossRef] [PubMed]
- Mijiritsky, E.; Hamama-Raz, Y.; Liu, F.; Datarkar, A.N.; Mangani, L.; Caplan, J.; Shacham, A.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; et al. Subjective Overload and Psychological Distress among Dentists during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5074. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Y.; Ye, J.; Wei, W. Study on the public psychological states and its related factors during the outbreak of the coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2021, 26, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Bhumireddy, J.; Mallineni, S.K.; Nuvvula, S. Challenges and possible solutions in dental practice during and post COVID-19. Environ. Sci. Pollut. Res. Int. 2021, 28, 1275–1277. [Google Scholar] [CrossRef] [PubMed]
- Barabari, P.; Moharamzadeh, K. Novel Coronavirus (COVID-19) and Dentistry-A Comprehensive Review of the Literature. Dent. J. 2020, 8, 53. [Google Scholar] [CrossRef]
- Mazur, M.; Duś-Ilnicka, I.; Jedliński, M.; Ndokaj, A.; Janiszewska-Olszowska, J.; Ardan, R.; Radwan-Oczko, M.; Guerra, F.; Luzzi, V.; Vozza, I.; et al. Facial and Oral Manifestations Following COVID-19 Vaccination: A Survey-Based Study and a First Perspective. Int. J. Environ. Res. Public Health 2021, 18, 4965. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, E.; Wachholtz, A. The effect of perceived stress on life satisfaction: The mediating effect of self-efficacy. Chongsonyonhak Yongu 2016, 23, 29–47. [Google Scholar] [PubMed] [Green Version]
- Arvidsdotter, T.; Marklund, B.; Kylén, S.; Taft, C.; Ekman, I. Understanding persons with psychological distress in primary health care. Scand. J. Caring Sci. 2016, 30, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Özarlsan, M.; Caliskan, S. Attitudes and predictive factors of psychological distress and occupational burnout among dentists during the COVID-19 pandemic in Turkey. Curr. Psychol. 2021, 40, 3113–3124. [Google Scholar]
- Hage-El, W.; Hingray, C.; Lemogne, C.; Yrondi, A.; Brunault, P.; Bienvenu, T.; Etain, B.; Paquet, C.; Gohier, B.; Dennabi, D.; et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks? Encéphale 2020, 46, S73–S80. [Google Scholar]
- Amato, A.; Caggiano, M.; Amato, M.; Moccia, G.; Capunzo, M.; De Caro, F. Infection Control in Dental Practice during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 4769. [Google Scholar] [CrossRef]
- Patel, M. Infection control in dentistry during COVID–19 pandemic: What has changed? Heliyon 2020, 30, e05402. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef]
- Narayana, T.V.; Mohanty, L.; Sreenath, G.; Vidhyadhari, P. Role of preprocedural rinse and high-volume evacuator in reducing bacterial contamination in bioaerosols. J. Oral Maxillofac. Pathol. 2016, 20, 59–65. [Google Scholar]
- Chuaybamrong, P.; Chotigawin, R.; Supothina, S.; Sribenjalux, P.; Larpkiattaworn, S.; Wu, C.Y. Efficacy of photocatalytic HEPA filter on microorganism removal. Indoor Air 2010, 20, 246–254. [Google Scholar] [CrossRef]
- Rexhepi, I.; Mangifesta, R.; Santilli, M.; Guri, S.; Di Carlo, P.; D’Addazio, G.; Caputi, S.; Sinjari, B. Effects of Natural Ventilation and Saliva Standard Ejectors during the COVID-19 Pandemic. A Quantitative Analysis of Aerosol Produced during Dental Procedures. Int. J. Environ. Res. Public Health 2021, 18, 7472. [Google Scholar] [CrossRef]
- Dave, M.; Seoudi, N.; Coulthard, P. Urgent dental care for patients during the COVID-19 pandemic. Lancet 2020, 395, 1257. [Google Scholar] [CrossRef]
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020, 99, 1030–1038. [Google Scholar] [CrossRef]
- Sinjari, B.; Rexhepi, I.; Santilli, M.; D’Addazio, G.; Chiacchiaretta, P.; Di Carlo, P.; Caputi, S. The Impact of COVID-19 Related Lockdown on Dental Practice in Central Italy-Outcomes of A Survey. Int. J. Environ. Res. Public Health 2020, 17, 5780. [Google Scholar] [CrossRef] [PubMed]
- Spoorthy, M.S.; Pratapa, S.K.; Mahani, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic: A review. Asian J. Psychiatry 2020, 51, 102119. [Google Scholar] [CrossRef]
- Ibn-Mohammed, T.; Mustapha, K.B.; Godsell, J.; Adamu, Z.; Babatunde, K.A.; Akintade, D.D.; Acquaye, A.; Ndiaye, M.M.; Yamoah, F.A.; Koh, S.C.L. A critical analysis of the impacts of COVID-19 on the global economy and ecosystems and opportunities for circular economy strategies. Resour. Conserv. Recycl. 2021, 164, 105169. [Google Scholar] [CrossRef]
- Uhlen, M.M.; Ansteinsson, V.E.; Stangvaltaite-Mouhat, L.; Korzeniewska, L.; Skudutyte-Rysstad, R.; Shabestari, M.; Mdala, I.; Hovden, E.A.S. Psychological impact of the COVID-19 pandemic on dental health personnel in Norway. BMC Health Serv. Res. 2021, 21, 420. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Noreen, S.; Farooq, I.; Bugshan, A.; Vohra, F. Risk assessment of healthcare workers at the frontline against COVID-19. Pak. J. Med. Sci. 2020, 36, S99–S103. [Google Scholar] [CrossRef]
- Kulkarni, S.; Dagli, N.; Duraiswamy, P.; Desai, H.; Vyas, H.; Baroudi, K. Stress and professional burnout among newly graduated dentists. J. Int. Soc. Prev. Community Dent. 2016, 6, 535–541. [Google Scholar]
- Al-Sowygh, Z.H. Academic distress, perceived stress, and coping strategies among dental students in Saudi Arabia. Saudi Dent. J. 2013, 25, 97–105. [Google Scholar] [CrossRef] [Green Version]
- Murphy, R.J.; Gray, S.A.; Sterling, G.; Reeves, K.; DuCette, J. A Comparative Study of Professional Student Stress. J. Dent. Educ. 2009, 73, 328–337. [Google Scholar] [CrossRef]
- Cohen, S.; Kamar, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Singh, S.; Tiwari, V.; Vanza, B.; Khare, N.; Bharadwaj, P. Assessment of Level of Perceived Stress and Sources of Stress Among Dental Professionals Before and During the COVID-19 Outbreak. J. Int. Soc. Prev. Community Dent. 2020, 10, 794–802. [Google Scholar] [PubMed]
- Stauder, A.; Konkoly, T.B. Az Észlelt Stressz Kérdőív (PSS) Magyar verziójának jellemzői. Mentálhigiéné és Pszichoszomatika 7 2006, 3, 203–216. [Google Scholar] [CrossRef] [Green Version]
- Flesia, F.; Monaro, M.; Mazza, C.; Fietta, V.; Colicino, E.; Segatto, B.; Roma, P. Predicting Perceived Stress Related to the COVID-19 Outbreak through Stable Psychological Traits and Machine Learning Models. J. Clin. Med. 2020, 9, 3350. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Bryant, F.B.; Yarnold, P.R. Principal-components analysis and exploratory and confirmatory factor analysis. In Reading and Understanding Multivariate Statistics; Grimm, L.G., Yarnold, P.R., Eds.; American Psychological Association: Washington, DC, USA, 1995; pp. 99–136. [Google Scholar]
- Jöreskog, K.G.; Sörbom, D. LISREL VI: Analysis of Linear Structural Relationships by Maximum Likelihood and Least Squares Methods; Scientific Software: Mooresville, IN, USA, 1986. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, Version 24.0; IBM Corp: Armonk, NY, USA, 2016. [Google Scholar]
- Arbuckle, J.L. Amos (Version 23.0); Computer Program; IBM SPSS: Chicago, IL, USA, 2014. [Google Scholar]
- Costello, A.B.; Osborne, J.W. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2005, 10, 7. [Google Scholar]
- DiMatteo, M.R.; Shugars, D.A.; Hays, R.D. Occupational stress, life stress and mental health among dentists. J. Occup. Orang. Psychol. 1993, 66, 153–162. [Google Scholar] [CrossRef]
- Puriene, A.; Janulyte, V.; Musteikyte, M.; Bendinskaite, R. General Health of Dentists. Literature review. Stomatologija 2007, 9, 10–20. [Google Scholar]
- León-Manco, R.A.; Agudelo-Suárez, A.A.; Armas-Vega, A.; Figueiredo, M.C.; Verdugo-Paiva, F.; Santana-Pérez, Y.; Viteri-García, A. Perceived Stress in Dentists and Dental Students of Latin America and the Caribbean during the Mandatory Social Isolation Measures for the COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 5889. [Google Scholar] [CrossRef]
- Meira, T.M.; Paiva, S.M.; Antelo, O.M.; Guimarães, L.M.; Bastos, S.Q.; Tanaka, O.M. Perceived stress and quality of life among graduate dental faculty. J. Dent. Educ. 2020, 84, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Bardellini, E.; Amadori, F.; Veneri, F.; Conti, G.; Majorana, A. Coronavirus Disease-2019 and dental practice: A project on the use of ozonized water in the water circuit of the dental armchair. Stomatologija 2020, 22, 35–38. [Google Scholar]
- Meng, L.; Hua, F.; Bian, Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [Green Version]
- Badru, O.A.; Oloko, K.O.; Hassan, A.O.; Yusuf, O.B.; Abdur-Razaq, U.A.; Yakub, S.S. Prevalence and correlates of psychological distress amongst healthcare workers during the COVID-19 pandemic: An online survey. S. Afr. J. Psychiatry 2021, 27, 1617. [Google Scholar] [CrossRef]
- Dziedzic, A.; Wojtyczka, R. The impact of coronavirus infectious disease 19 (COVID-19) on oral health. Oral Dis. 2021, 27, 703–706. [Google Scholar] [CrossRef]
- Sinjari, B.; D’Ardes, D.; Santilli, M.; Rexhepi, I.; D’Addazio, G.; Di Carlo, P.; Chiacchiaretta, P.; Caputi, S.; Cipollone, F. SARS-CoV-2 and Oral Manifestation: An Observational, Human Study. J. Clin. Med. 2020, 9, 3218. [Google Scholar] [CrossRef]
- Cooper, C.L.; Watts, J.; Baglioni, A.J.; Kelly, M. Job satisfaction, mental health, and job stressors among general dental practitioners in the UK. Br. Dent. J. 1987, 162, 77–81. [Google Scholar] [CrossRef]
- Coulthard, P. Dentistry and coronavirus (COVID-19)—Moral decision-making. Br. Dent. J. 2020, 228, 503–505. [Google Scholar] [CrossRef]
- Archuleta, K.L.; Scott, D.A. College students and financial distress: Exploring debt, financial satisfaction, and financial anxiety. J. Financ. Couns. Plan. 2013, 24, 50–62. [Google Scholar]
- Ferneini, E.M. The Financial Impact of COVID-19 on Our Practice. J. Oral Maxillofac. Surg. 2020, 78, 1046–1048. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, H.; Atteya, S.; Ihab, M.; Nyan, M.; Maharani, D.A.; Rahardjo, A.; Shaath, M.; Aboalshamat, K.; Butool, S.; Shamala, A.; et al. Dental practice closure during the frst wave of COVID-19 and associated professional, practice and structural determinants: A multi-country survey. BMC Oral Health 2021, 21, 243. [Google Scholar] [CrossRef]
- Farooq, I.; Ali, S. COVID-19 outbreak and its monetary implications for dental practices, hospitals, and healthcare workers. Postgrad. Med. J. 2020, 96, 791–792. [Google Scholar] [CrossRef] [PubMed]
- Humphris, G.M.; Cooper, C.L. New Stressors for GDPs in the past ten years: A qualitative study. BMJ 1998, 185, 404–406. [Google Scholar] [CrossRef] [PubMed]
- Mak, I.W.; Chu, C.M.; Pan, P.C.; Yiu, M.G.; Chan, V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 2009, 31, 318–326. [Google Scholar] [CrossRef]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef]
- Yap, A.U.; Bhole, S.; Teo, C.S. A cross-cultural comparison of perceived sources of stress in the dental school environment. J. Dent. Educ. 1996, 60, 459–464. [Google Scholar] [CrossRef]
- Mahendran, K.; Patel, S.; Sproat, C. Psychosocial effects of the COVID-19 pandemic on staff in a dental teaching hospital. Br. Dent. J. 2020, 229, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Pouradeli, S.; Shahravan, A.; Eskandarizden, A.; Rafie, F.; Hashemipour, M.A. Occupational Stress and Coping Behaviours Among Dentists in Kerman, Iran. Sultan Qaboos Univ. Med. J. 2016, 16, e341–e346. [Google Scholar] [CrossRef]
- Mahdee, A.F.; Gul, S.S.; Abdulkareem, A.A.; Qasim, S.S.B. Anxiety, Practice Modification, and Economic Impact Among Iraqi Dentists During the COVID-19 Outbreak. Front. Med. 2020, 7, 595028. [Google Scholar] [CrossRef] [PubMed]
- Allan, S.M.; Bealey, R.T.; Birch, J.; Cushing, T.; Parke, S.; Sergi, G.; Bloomfield, M.; Meiser-Stedman, R. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: A rapid systematic review and meta-analysis. Eur. J. Psychotraumatol. 2020, 11, 1810903. [Google Scholar] [CrossRef] [PubMed]
- Lung, F.-W.; Lu, Y.-C.; Chang, Y.-Y.; Shu, B.-C. Mental Symptoms in Different Health Professionals During the SARS Attack: A Follow-up Study. Psychiatry Q. 2009, 80, 107–116. [Google Scholar] [CrossRef]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The Psychological Impact of the SARS Epidemic on Hospital Employees in China: Exposure, Risk Perception, and Altruistic Acceptance of Risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).