Estimating Economic Losses Caused by COVID-19 under Multiple Control Measure Scenarios with a Coupled Infectious Disease—Economic Model: A Case Study in Wuhan, China
Abstract
:1. Introduction
2. Materials and Methods
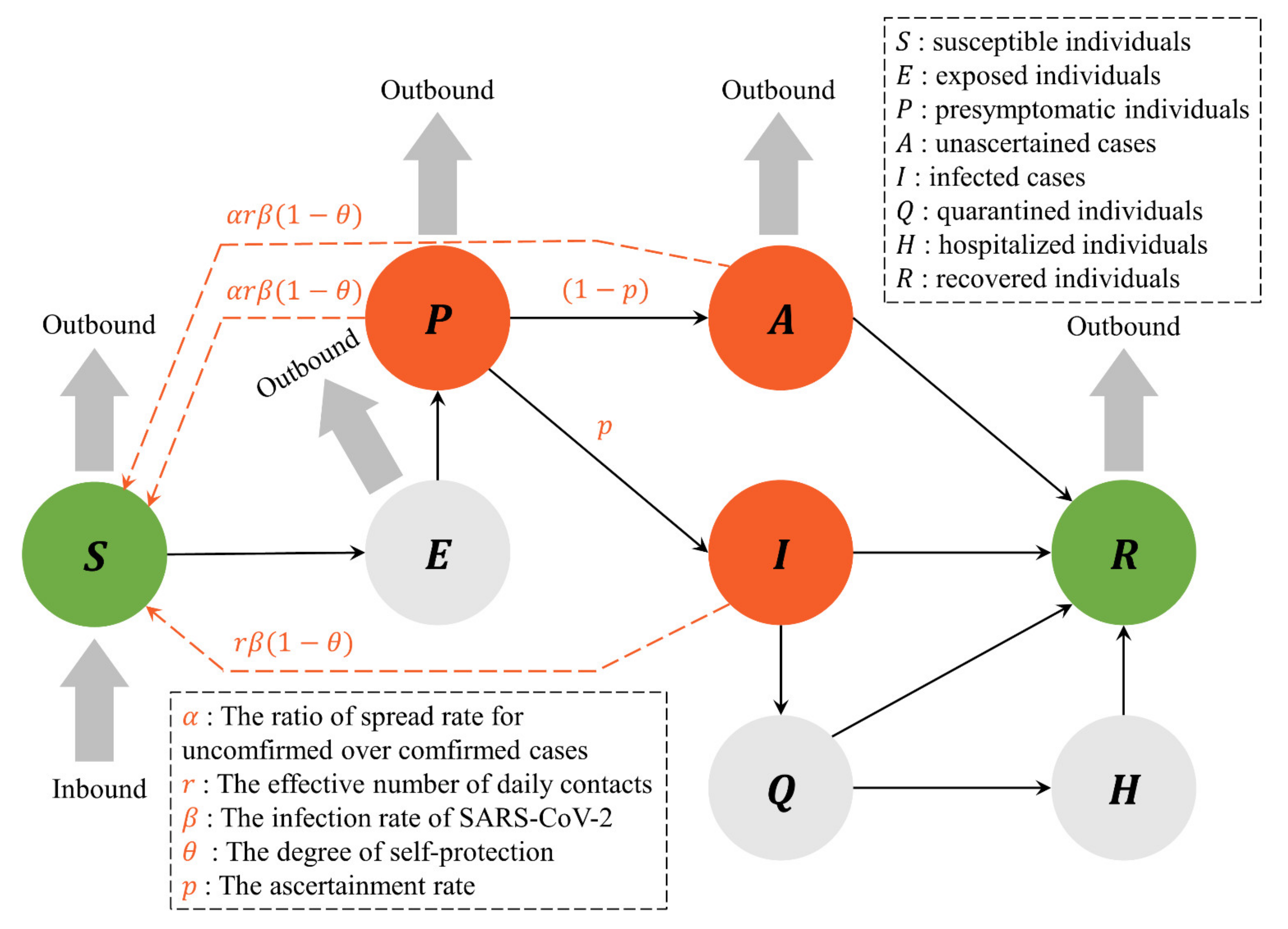
2.1. The Infectious Disease Model
2.1.1. The Framework of the Infectious Disease Model
2.1.2. The Five-Stage Model and its Parameters
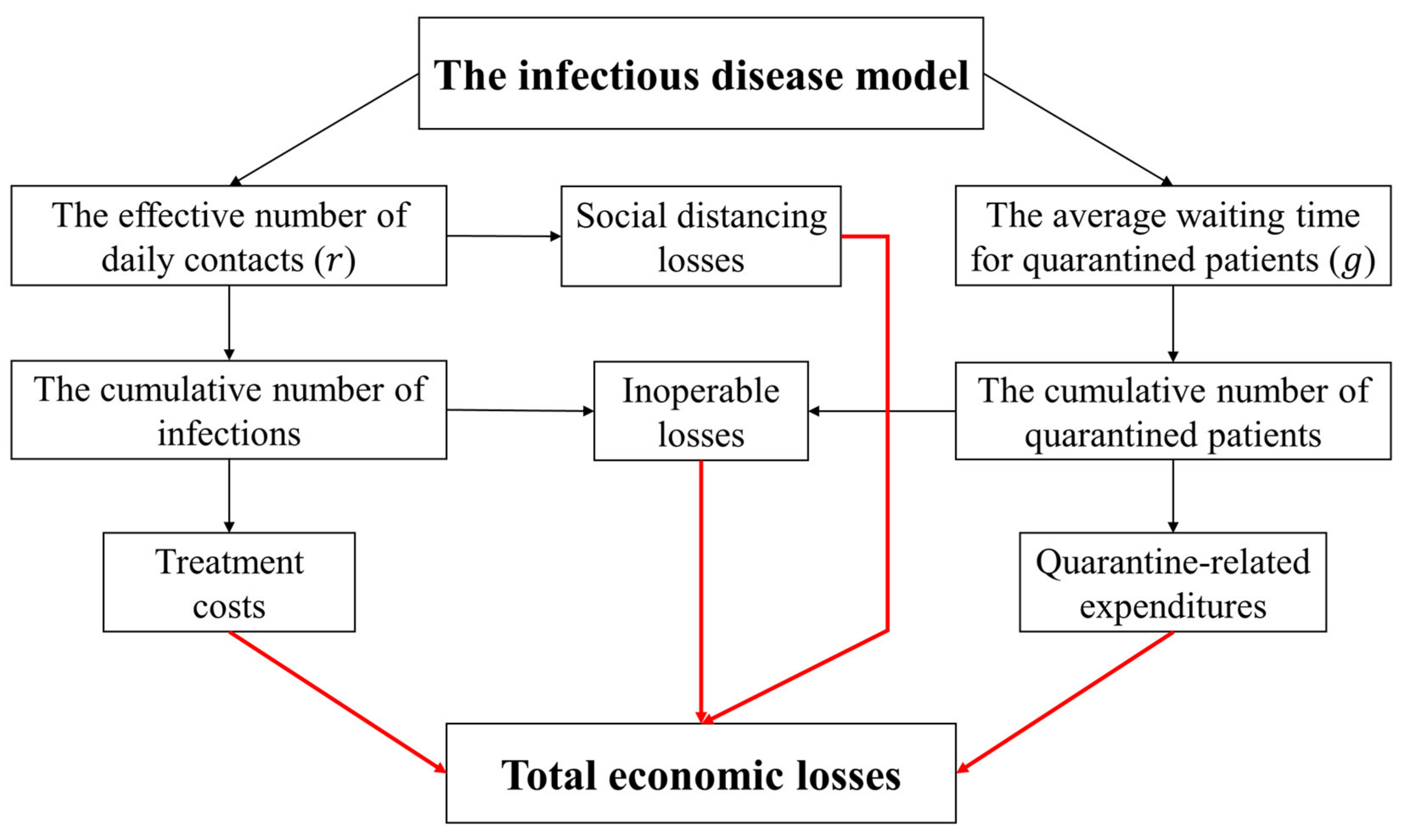
2.2. The Economic Losses Model
2.2.1. Treatment Costs
2.2.2. Quarantine-Related Expenditures
2.2.3. Inoperable Losses
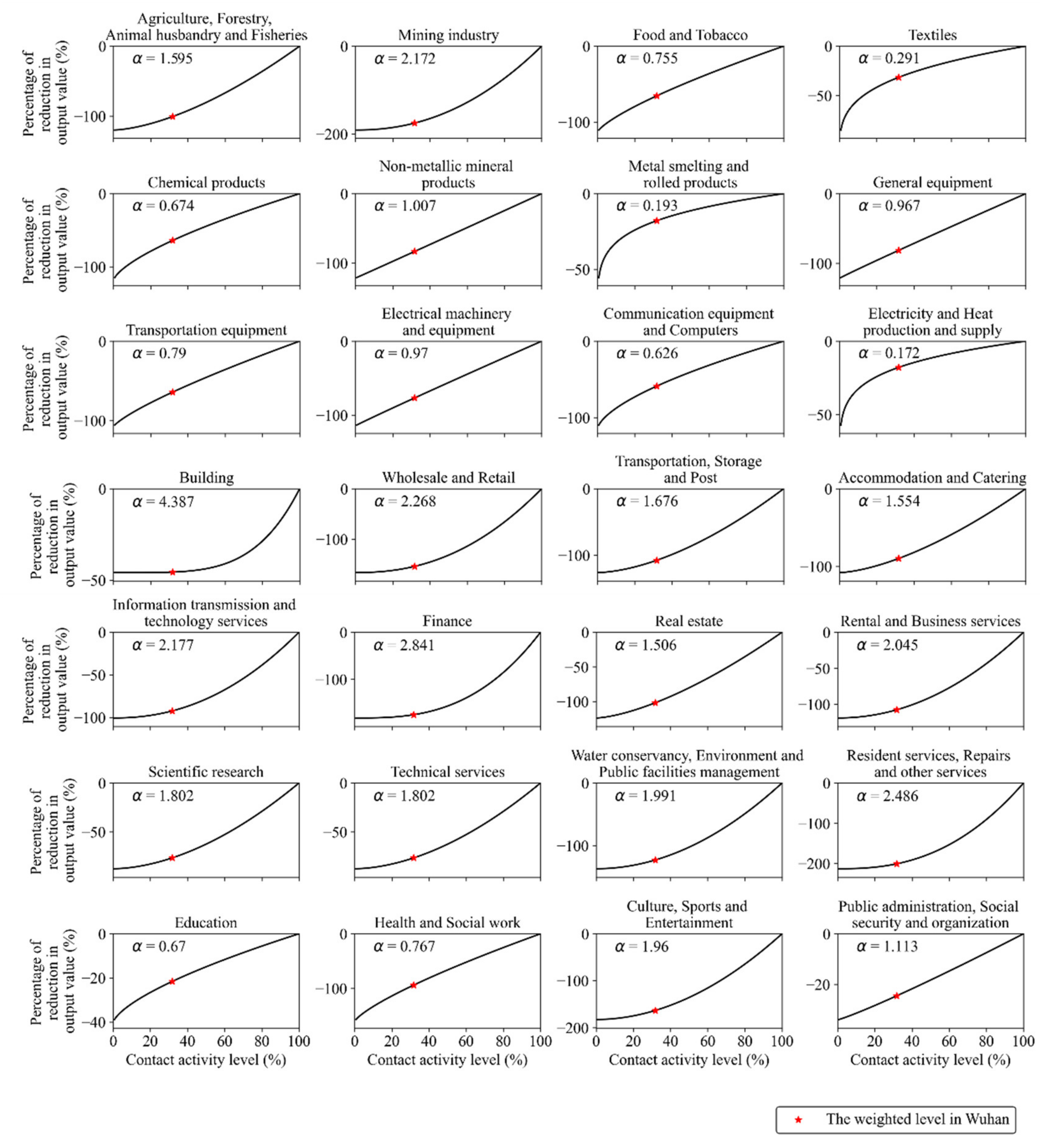
2.2.4. Social Distancing Losses
2.2.5. Total Economic Losses
2.3. Data
3. Results
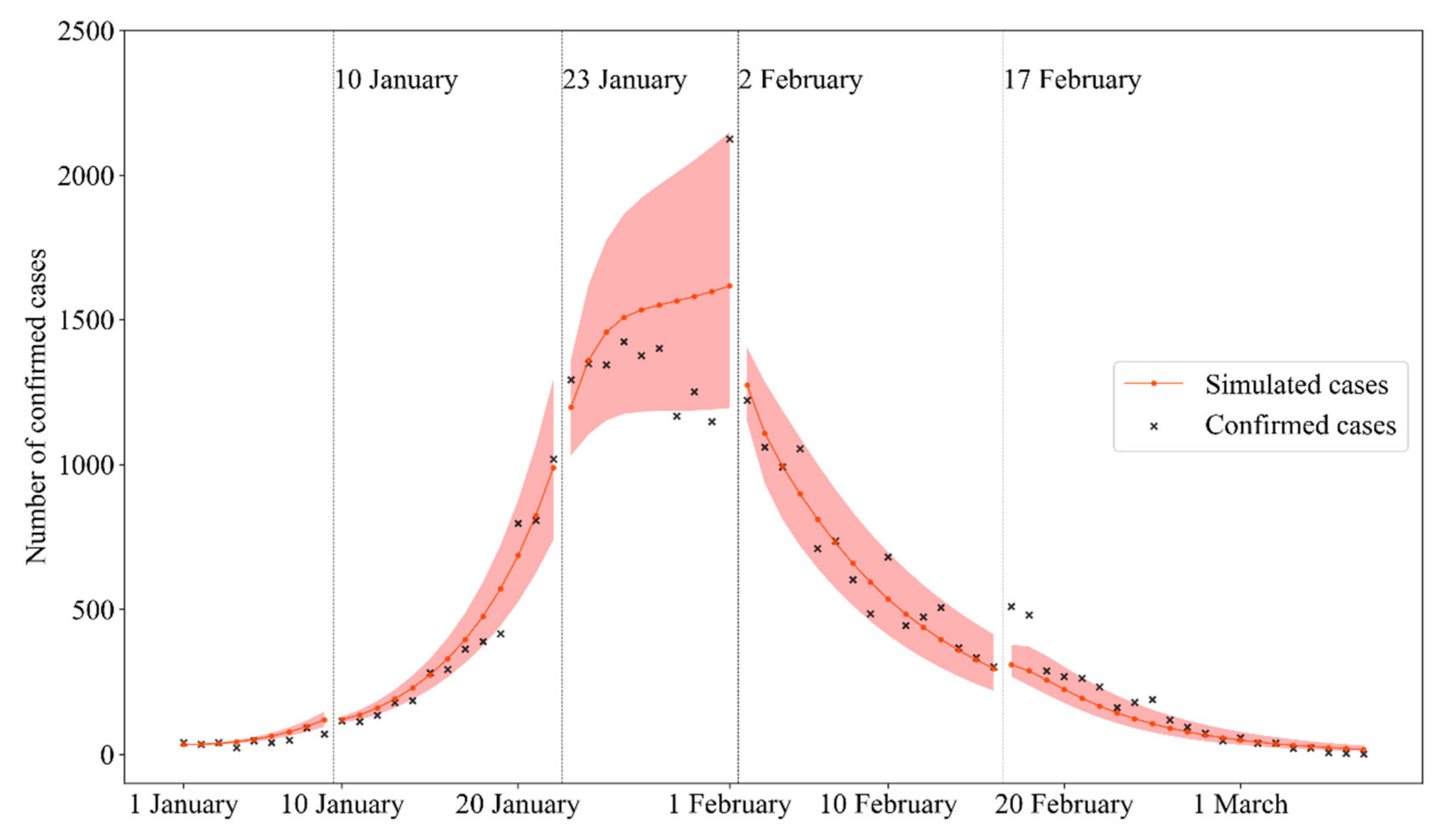
3.1. The Infectious Disease Model Verification
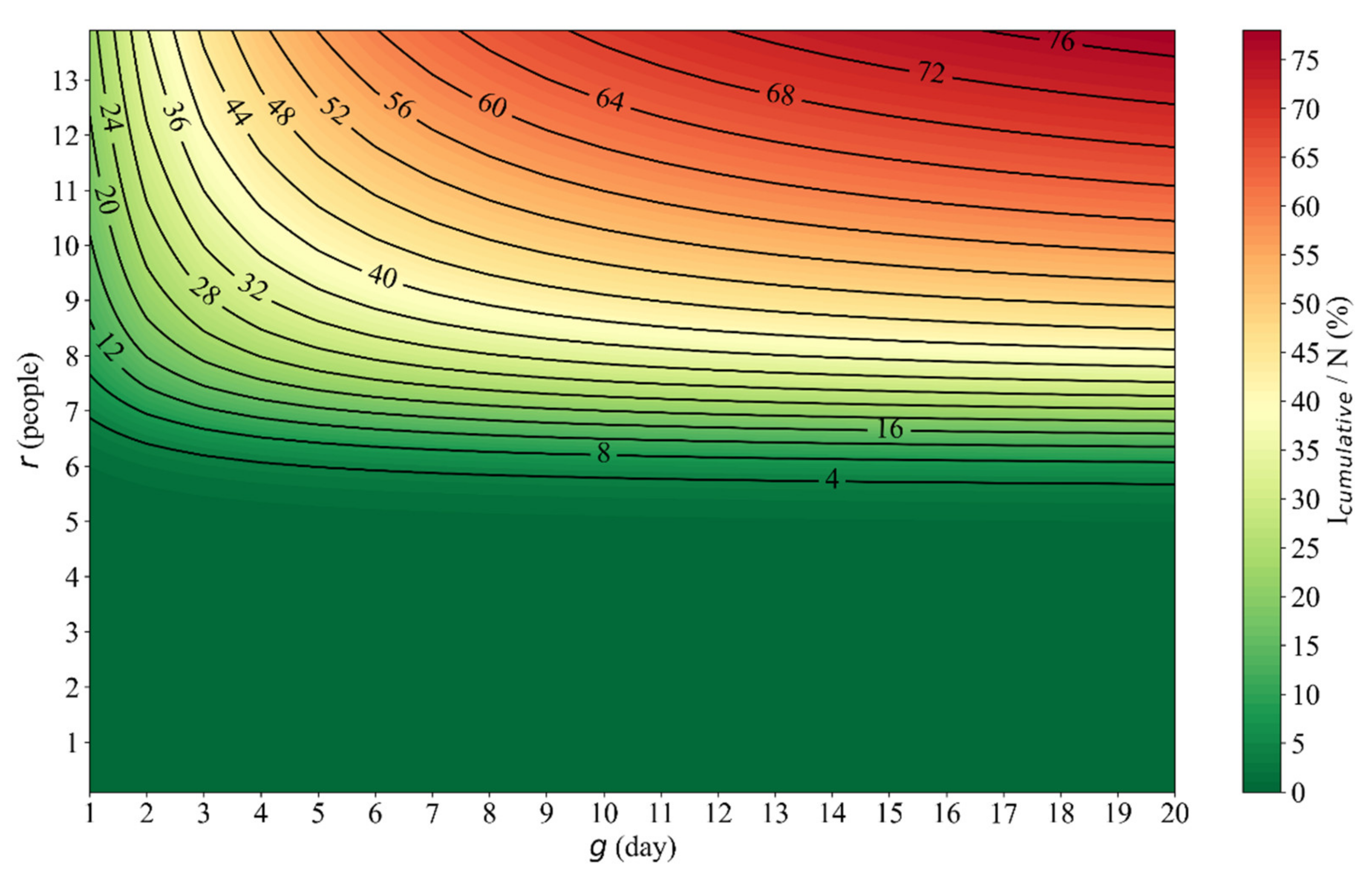
3.2. The Influence of Social Distancing () and Tracking/Quarantining Ability () on Public Health
3.3. The Influence of Social Distancing () and Tracking/Quarantining Ability () on Economic Losses
4. Discussion
4.1. Literature-Based Verification
4.2. Suggestion on Control of COVID-19 Spread
4.3. Contribution and Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A Descriptive Study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061. [Google Scholar] [CrossRef] [PubMed]
- Kucharski, A.J.; Russell, T.W.; Diamond, C.; Liu, Y.; Edmunds, J.; Funk, S.; Eggo, R.M.; Sun, F.; Jit, M.; Munday, J.D.; et al. Early Dynamics of Transmission and Control of COVID-19: A Mathematical Modelling Study. Lancet Infect. Dis. 2020, 20, 553–558. [Google Scholar] [CrossRef] [Green Version]
- Tian, H.; Liu, Y.; Li, Y.; Wu, C.-H.; Chen, B.; Kraemer, M.U.G.; Li, B.; Cai, J.; Xu, B.; Yang, Q.; et al. An Investigation of Transmission Control Measures during the First 50 Days of the COVID-19 Epidemic in China. Science 2020, 368, 638–642. [Google Scholar] [CrossRef] [Green Version]
- Hao, X.; Cheng, S.; Wu, D.; Wu, T.; Lin, X.; Wang, C. Reconstruction of the Full Transmission Dynamics of COVID-19 in Wuhan. Nature 2020, 584, 420–424. [Google Scholar] [CrossRef]
- Pan, A.; Liu, L.; Wang, C.; Guo, H.; Hao, X.; Wang, Q.; Huang, J.; He, N.; Yu, H.; Lin, X.; et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020, 323, 1915–1923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of Non-Pharmaceutical Interventions to Contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef]
- Duhon, J.; Bragazzi, N.; Kong, J.D. The Impact of Non-Pharmaceutical Interventions, Demographic, Social, and Climatic Factors on the Initial Growth Rate of COVID-19: A Cross-Country Study. Sci. Total Environ. 2021, 760, 144325. [Google Scholar] [CrossRef]
- Wu, X.; Yin, J.; Li, C.; Xiang, H.; Lv, M.; Guo, Z. Natural and Human Environment Interactively Drive Spread Pattern of COVID-19: A City-Level Modeling Study in China. Sci. Total Environ. 2021, 756, 143343. [Google Scholar] [CrossRef]
- Zhou, Y.; Xu, R.; Hu, D.; Yue, Y.; Li, Q.; Xia, J. Effects of Human Mobility Restrictions on the Spread of COVID-19 in Shenzhen, China: A Modelling Study Using Mobile Phone Data. Lancet Digit. Health 2020, 2, e417–e424. [Google Scholar] [CrossRef]
- Rowan, N.J.; Moral, R.A. Disposable Face Masks and Reusable Face Coverings as Non-Pharmaceutical Interventions (NPIs) to Prevent Transmission of SARS-CoV-2 Variants That Cause Coronavirus Disease (COVID-19): Role of New Sustainable NPI Design Innovations and Predictive Mathematical Modelling. Sci. Total Environ. 2021, 772, 145530. [Google Scholar] [CrossRef]
- Ferretti, L.; Wymant, C.; Kendall, M.; Zhao, L.; Nurtay, A.; Abeler-Dörner, L.; Parker, M.; Bonsall, D.; Fraser, C. Quantifying SARS-CoV-2 Transmission Suggests Epidemic Control with Digital Contact Tracing. Science 2020, 368, eabb6936. [Google Scholar] [CrossRef] [Green Version]
- Zhou, C.; Su, F.; Pei, T.; Zhang, A.; Du, Y.; Luo, B.; Cao, Z.; Wang, J.; Yuan, W.; Zhu, Y.; et al. COVID-19: Challenges to GIS with Big Data. Geogr. Sustain. 2020, 1, 77–87. [Google Scholar] [CrossRef]
- Li, X.; Zhao, Z.; Liu, F. Big Data Assimilation to Improve the Predictability of COVID-19. Geogr. Sustain. 2020, 1, 317–320. [Google Scholar] [CrossRef]
- Zhao, W.; Zhang, J.; Meadows, M.E.; Liu, Y.; Hua, T.; Fu, B. A Systematic Approach Is Needed to Contain COVID-19 Globally. Sci. Bull. 2020, 65, 876–878. [Google Scholar] [CrossRef] [Green Version]
- Kaim, A.; Gering, T.; Moshaiov, A.; Adini, B. Deciphering the COVID-19 Health Economic Dilemma (HED): A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 9555. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Hu, Q.; Zhu, C.; Wang, H.; Yu, Q.; Sun, H. New Structural Economic Analysis of Anti-COVID-19 Pandemic Model of BEST Region. Int. J. Environ. Res. Public Health 2021, 18, 7822. [Google Scholar] [CrossRef]
- Hubei Provincial Statistics Bureau (HSB). Hubei’s Economic Performance in the First Half of 2020. Available online: http://tjj.hubei.gov.cn/zfxxgk_GK2020/fdzdgknr_GK2020/qtzdgknr_GK2020/hygq_GK2020/202010/t20201030_2986883.shtml (accessed on 20 June 2020). (In Chinese)
- Hubei Provincial Statistics Bureau (HSB). Hubei’s Economic Performance in 2020. Available online: http://tjj.hubei.gov.cn/zfxxgk_GK2020/fdzdgknr_GK2020/qtzdgknr_GK2020/hygq_GK2020/202101/t20210129_3324091.shtml (accessed on 20 January 2021). (In Chinese)
- National Bureau of Statistics of China (NBSC). Stable Recovery of the National Economy in 2020. Available online: http://www.stats.gov.cn/tjsj/zxfb/202101/t20210118_1812423.html (accessed on 18 January 2021). (In Chinese)
- Brodeur, A.; Gray, D.; Islam, A.; Bhuiyan, S. A Literature Review of the Economics of COVID-19. J. Econ. Surv. 2021, 35, 1007–1044. [Google Scholar] [CrossRef]
- Baldwin, R.; Di Mauro, B.W. Economics in the Time of COVID-19; Centre for Economic Policy Research Press: London, UK, 2020; ISBN 978-1-912179-28-2. [Google Scholar]
- Ludvigson, S.C.; Ma, S.; Ng, S. COVID-19 and the Macroeconomic Effects of Costly Disasters; Working Paper 26987; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The Socio-Economic Implications of the Coronavirus Pandemic (COVID-19): A Review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Barro, R.J.; Ursúa, J.F.; Weng, J. The Coronavirus and the Great Influenza Pandemic: Lessons from the “Spanish Flu” for the Coronavirus’s Potential Effects on Mortality and Economic Activity; Working Paper 26866; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]
- International Monetary Fund (IMF). World Economic Outlook: Managing Divergent Recoveries. Available online: https://www.imf.org/en/Publications/WEO/Issues/2021/03/23/world-economic-outlook-april-2021 (accessed on 1 April 2021).
- Guan, D.; Wang, D.; Hallegatte, S.; Davis, S.J.; Huo, J.; Li, S.; Bai, Y.; Lei, T.; Xue, Q.; Coffman, D.; et al. Global Supply-Chain Effects of COVID-19 Control Measures. Nat. Hum. Behav. 2020, 4, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Guan, D.; Zhu, S.; Kinnon, M.M.; Geng, G.; Zhang, Q.; Zheng, H.; Lei, T.; Shao, S.; Gong, P.; et al. Economic Footprint of California Wildfires in 2018. Nat. Sustain. 2021, 4, 252–260. [Google Scholar] [CrossRef]
- You, S.; Wang, H.; Zhang, M.; Song, H.; Xu, X.; Lai, Y. Assessment of Monthly Economic Losses in Wuhan under the Lockdown against COVID-19. Humanit. Soc. Sci. Commun. 2020, 7, 52. [Google Scholar] [CrossRef]
- Jin, H.; Wang, H.; Li, X.; Zheng, W.; Ye, S.; Zhang, S.; Zhou, J.; Pennington, M. Economic Burden of COVID-19, China, January-March, 2020: A Cost-of-Illness Study. Bull. World Health Organ. 2021, 99, 112–124. [Google Scholar] [CrossRef]
- Yu, K.D.S.; Aviso, K.B. Modelling the Economic Impact and Ripple Effects of Disease Outbreaks. Process Integr. Optim. Sustain. 2020, 4, 183–186. [Google Scholar] [CrossRef] [Green Version]
- Xia, J.; Ying, Z.; Li, Z.; Li, F.; Yue, Y.; Cheng, T.; Li, Q. COVID-19 risk assessment driven by urban spatiotemporal big data: A case study of Guangdong-Hong Kong-Macao Greater Bay Area. Acta Geod. Cartogr. Sin. 2020, 49, 671–680. [Google Scholar] [CrossRef]
- Hsiang, S.; Allen, D.; Annan-Phan, S.; Bell, K.; Bolliger, I.; Chong, T.; Druckenmiller, H.; Huang, L.Y.; Hultgren, A.; Krasovich, E.; et al. The Effect of Large-Scale Anti-Contagion Policies on the COVID-19 Pandemic. Nature 2020, 584, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Atkeson, A. What Will Be the Economic Impact of COVID-19 in the US? Rough Estimates of Disease Scenarios; Working Paper 26867; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]
- Alvarez, F.E.; Argente, D.; Lippi, F. A Simple Planning Problem for COVID-19 Lockdown; Working Paper 26981; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]
- Acemoglu, D.; Chernozhukov, V.; Werning, I.; Whinston, M.D. Optimal Targeted Lockdowns in a Multi-Group SIR Model; Working Paper 27102; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]
- Kermack, W.O.; McKendrick, A.G.; Walker, G.T. A Contribution to the Mathematical Theory of Epidemics. Proc. R. Soc. Lond. Ser. Contain. Pap. Math. Phys. Character 1927, 115, 700–721. [Google Scholar] [CrossRef] [Green Version]
- Wu, J.T.; Leung, K.; Leung, G.M. Nowcasting and Forecasting the Potential Domestic and International Spread of the 2019-NCoV Outbreak Originating in Wuhan, China: A Modelling Study. Lancet 2020, 395, 689–697. [Google Scholar] [CrossRef] [Green Version]
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial Undocumented Infection Facilitates the Rapid Dissemination of Novel Coronavirus (SARS-CoV-2). Science 2020, 368, 489–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrot, J.-N.; Grassi, B.; Sauvagnat, J. Sectoral Effects of Social Distancing. AEA Pap. Proc. 2021, 111, 277–281. [Google Scholar] [CrossRef]
- He, X.; Lau, E.H.Y.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X.; et al. Temporal Dynamics in Viral Shedding and Transmissibility of COVID-19. Nat. Med. 2020, 26, 672–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Vullikanti, A.; Hoops, S.; Mortveit, H.; Lewis, B.; Venkatramanan, S.; You, W.; Eubank, S.; Marathe, M.; Barrett, C.; et al. Medical Costs of Keeping the US Economy Open during COVID-19. Sci. Rep. 2020, 10, 18422. [Google Scholar] [CrossRef] [PubMed]
- Hubei Provincial Statistics Bureau (HSB). Hubei Statistical Yearbook 2020. Available online: http://tjj.hubei.gov.cn/tjsj/sjkscx/tjnj/qstjnj/ (accessed on 20 October 2020). (In Chinese)
- National Bureau of Statistics of China (NBSC). China Statistical Yearbook 2019. Available online: http://www.stats.gov.cn/tjsj/ndsj/ (accessed on 1 September 2020). (In Chinese)
- Prem, K.; Cook, A.R.; Jit, M. Projecting Social Contact Matrices in 152 Countries Using Contact Surveys and Demographic Data. PLoS Comput. Biol. 2017, 13, e1005697. [Google Scholar] [CrossRef]
- Hamilton, J.D. Time Series Analysis; Princeton University Press: Princeton, NJ, USA, 1994; ISBN 978-0-691-04289-3. [Google Scholar]
- Prem, K.; Liu, Y.; Russell, T.W.; Kucharski, A.J.; Eggo, R.M.; Davies, N.; Flasche, S.; Clifford, S.; Pearson, C.A.B.; Munday, J.D.; et al. The Effect of Control Strategies to Reduce Social Mixing on Outcomes of the COVID-19 Epidemic in Wuhan, China: A Modelling Study. Lancet Public Health 2020, 5, e261–e270. [Google Scholar] [CrossRef] [Green Version]
- Badr, H.S.; Du, H.; Marshall, M.; Dong, E.; Squire, M.M.; Gardner, L.M. Association between Mobility Patterns and COVID-19 Transmission in the USA: A Mathematical Modelling Study. Lancet Infect. Dis. 2020, 20, 1247–1254. [Google Scholar] [CrossRef]
- Hellewell, J.; Abbott, S.; Gimma, A.; Bosse, N.I.; Jarvis, C.I.; Russell, T.W.; Munday, J.D.; Kucharski, A.J.; Edmunds, W.J.; Sun, F.; et al. Feasibility of Controlling COVID-19 Outbreaks by Isolation of Cases and Contacts. Lancet Glob. Health 2020, 8, e488–e496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flaxman, S.; Mishra, S.; Gandy, A.; Unwin, H.J.T.; Mellan, T.A.; Coupland, H.; Whittaker, C.; Zhu, H.; Berah, T.; Eaton, J.W.; et al. Estimating the Effects of Non-Pharmaceutical Interventions on COVID-19 in Europe. Nature 2020, 584, 257–261. [Google Scholar] [CrossRef]
- Leung, K.; Wu, J.T.; Liu, D.; Leung, G.M. First-Wave COVID-19 Transmissibility and Severity in China Outside Hubei after Control Measures, and Second-Wave Scenario Planning: A Modelling Impact Assessment. Lancet 2020, 395, 1382–1393. [Google Scholar] [CrossRef]
- López, L.; Rodó, X. The End of Social Confinement and COVID-19 Re-Emergence Risk. Nat. Hum. Behav. 2020, 4, 746–755. [Google Scholar] [CrossRef]
- Lee, E.C.; Wada, N.I.; Grabowski, M.K.; Gurley, E.S.; Lessler, J. The Engines of SARS-CoV-2 Spread. Science 2020, 370, 406–407. [Google Scholar] [CrossRef] [PubMed]
- Banga, K. Can the Digital Economy Help Mitigate the Economic Losses from COVID-19 in Kenya? Available online: https://set.odi.org/can-digital-economy-help-mitigate-economic-losses-from-covid-19-in-kenya/ (accessed on 24 October 2021).
- La, V.-P.; Pham, T.-H.; Ho, M.-T.; Nguyen, M.-H.; Nguyen, K.-L.P.; Vuong, T.-T.; Nguyen, H.-K.T.; Tran, T.; Khuc, Q.; Ho, M.-T.; et al. Policy Response, Social Media and Science Journalism for the Sustainability of the Public Health System Amid the COVID-19 Outbreak: The Vietnam Lessons. Sustainability 2020, 12, 2931. [Google Scholar] [CrossRef] [Green Version]
- Cutler, D.M.; Summers, L.H. The COVID-19 Pandemic and the $16 Trillion Virus. JAMA 2020, 324, 1495–1496. [Google Scholar] [CrossRef]
- Walker, P.G.T.; Whittaker, C.; Watson, O.J.; Baguelin, M.; Winskill, P.; Hamlet, A.; Djafaara, B.A.; Cucunubá, Z.; Olivera Mesa, D.; Green, W.; et al. The Impact of COVID-19 and Strategies for Mitigation and Suppression in Low- and Middle-Income Countries. Science 2020, 369, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Vuong, Q.-H.; Ho, T.-M.; Nguyen, H.-K.; Vuong, T.-T. Healthcare Consumers’ Sensitivity to Costs: A Reflection on Behavioural Economics from an Emerging Market. Palgrave Commun. 2018, 4, 70. [Google Scholar] [CrossRef]
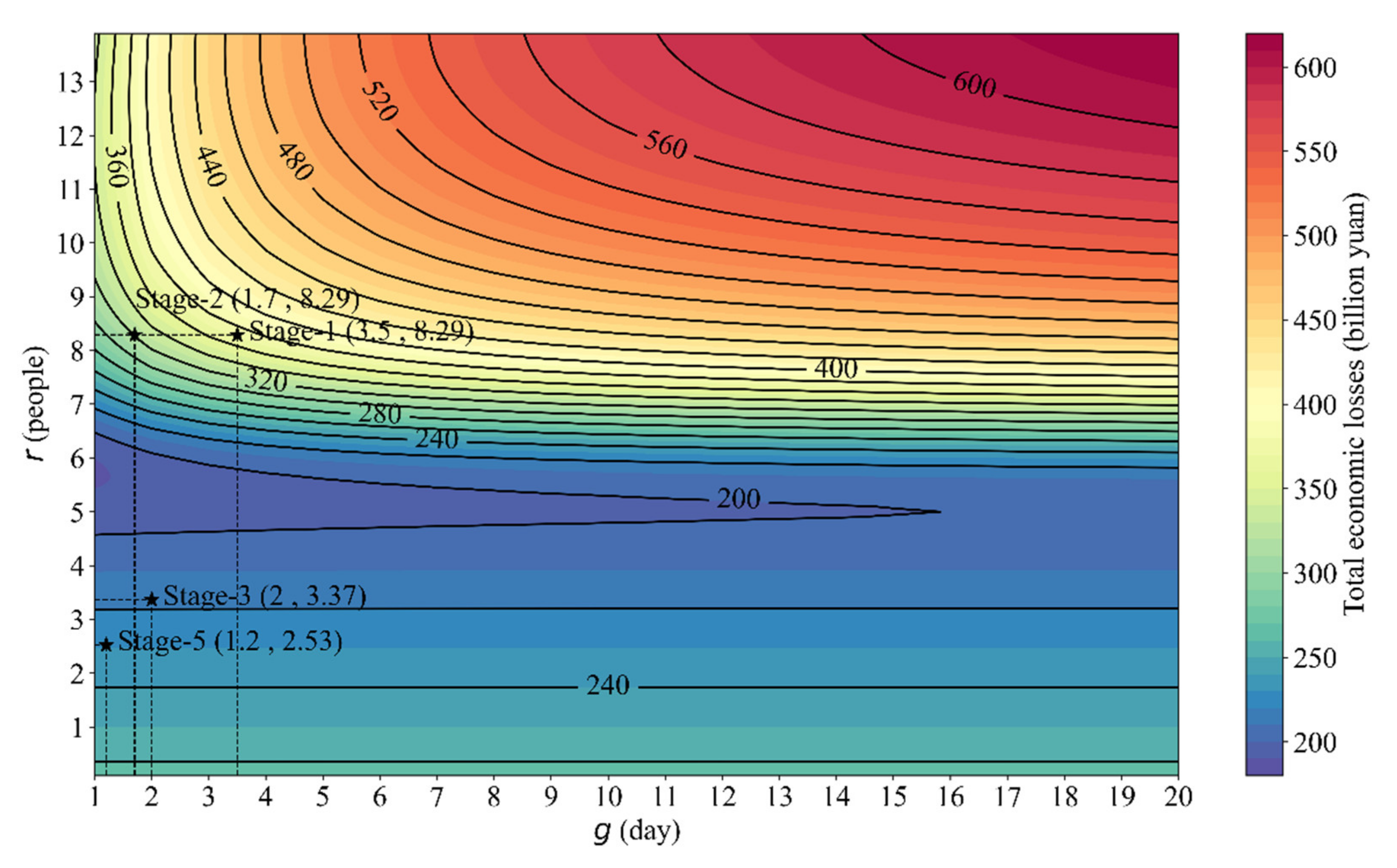
| Meaning | 1.1–1.9 | 1.10–1.22 | 1.23–2.1 | 2.2–2.16 | 2.17–3.8 | Reference | |
|---|---|---|---|---|---|---|---|
| The transmission rate of confirmed cases | 1.31 | 1.31 | 0.40 | 0.17 | 0.10 | [7] | |
| The effective number of daily contacts (people) | 8.29 | 8.29 | 3.37 | 2.15 | 2.53 | Estimated | |
| The SARS-CoV-2 infection rate | 0.395 | 0.395 | 0.395 | 0.395 | 0.395 | [5] | |
| The degree of self-protection | 0.6 | 0.6 | 0.7 | 0.8 | 0.9 | Assumed | |
| The ascertainment rate | 0.15 | 0.15 | 0.14 | 0.10 | 0.16 | [7] | |
| The ratio of spread rate for unconfirmed over confirmed cases | 0.55 | 0.55 | 0.55 | 0.55 | 0.55 | [41] | |
| The presymptomatic infectious period | 2.3 | 2.3 | 2.3 | 2.3 | 2.3 | [7,42] | |
| The latent period | 2.9 | 2.9 | 2.9 | 2.9 | 2.9 | [3,7] | |
| The symptomatic infectious period | 2.9 | 2.9 | 2.9 | 2.9 | 2.9 | [7,14] | |
| The average waiting time for quarantined patients (day) | 3.5 | 1.7 | 2 | 1.7 | 1.2 | Fitted | |
| The average hospitalization period | 10 | 10 | 10 | 10 | 10 | [4] | |
| The total population in Wuhan | 10,000,000 | 10,000,000 | 10,000,000 | 10,000,000 | 10,000,000 | [7,40] | |
| The daily domestic inbound and outbound travelers in Wuhan | 500,000 | 800,000 | 0 | 0 | 0 | [7,40] |
| Meaning | Value | Reference | |
|---|---|---|---|
| (treatment costs) | |||
| The cumulative number of infected patients under various control measures (r and g) | Simulated | ||
| The probability of a COVID-19 infected patient being admitted to the Intensive Care Unit (ICU) | 26.1(%) | [4] | |
| The probability of Acute Respiratory Distress Syndrome (ARDS) after a COVID-19 infected patient is admitted to the Intensive Care Unit (ICU) | 61.1(%) | [4] | |
| The average treatment costs of a COVID-19 infected patient with no complications | 67,360 (yuan) | [44] | |
| The average treatment costs of a COVID-19 infected patient with complications | 94,986 (yuan) | [44] | |
| The average treatment cost of a COVID-19 infected patient with severe complications | 140,006 (yuan) | [44] | |
| (Quarantine-related expenditures) | |||
| The cumulative number of quarantined patients during the COVID-19 outbreak in Wuhan | 26,893 (people) | Equation (1) | |
| The total expenditures for disaster prevention and emergency management in Hubei province in the first quarter of 2020 | 15.68 (billion yuan) | [45] | |
| The cumulative number of quarantined patients under various control measures (r and g) | Simulated | ||
| (Inoperable losses) | |||
| The average time that infected patients received treatment and self-isolation | 8 + 10 + 14 = 32(days) | [4] | |
| The average time that quarantined patients received quarantine and self-isolation | 14 + 14 = 28(days) | Assumed | |
| The per capita daily GDP in 2019 | 198(yuan) | [46] | |
| Meaning | Value | Reference | |
|---|---|---|---|
| The effective number of daily contacts before the COVID-19 outbreak | 13.96 (people) | Equation (5) | |
| The contact’s number matrix with intervals of five years of age in China | [47] | ||
| The proportion of the age structure with intervals of five years of age in China in 2019 | [46] | ||
| The weighted value of the effective number of daily contacts during the COVID-19 outbreak | 4.43 (people) | Equation (6) | |
| The effective number of daily contacts in each stage of the COVID-19 epidemic in Wuhan | Estimated in Table 1 | ||
| The proportion of the duration in each stage of the COVID-19 epidemic in Wuhan | [7] | ||
| The reduction in contact activity caused by the COVID-19 outbreak in Wuhan | 31.73 (%) | Equations (5) and (6) | |
| The degree of nonlinearity of each industry sector’s response to the reduction in contact activity | Equation (8) | ||
| The cumulative output value of each industry sector in the Hubei province in the first quarter of 2020 | [45] | ||
| The actual growth rate of the industry sector in the Hubei province in the first quarter of 2020 | [45] | ||
| The expected growth rate of the industry sector in the Hubei province in the first quarter of 2020 | Estimated with the ARIMA model [48] | ||
| (Social distancing losses) | |||
| The expected growth rate of each industry sector under the different level of contact activity | Equation (9) | ||
| The effective number of daily contacts | ) | Assumed | |
| The different level of contact activity | (0, 1) | Assumed | |
| The percentage of the output value in 2019 Wuhan to the output value in the 2019 Hubei province | 35.37 (%) | [45] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, X.; Gong, W.; Wu, X.; Zhao, W. Estimating Economic Losses Caused by COVID-19 under Multiple Control Measure Scenarios with a Coupled Infectious Disease—Economic Model: A Case Study in Wuhan, China. Int. J. Environ. Res. Public Health 2021, 18, 11753. https://doi.org/10.3390/ijerph182211753
Chen X, Gong W, Wu X, Zhao W. Estimating Economic Losses Caused by COVID-19 under Multiple Control Measure Scenarios with a Coupled Infectious Disease—Economic Model: A Case Study in Wuhan, China. International Journal of Environmental Research and Public Health. 2021; 18(22):11753. https://doi.org/10.3390/ijerph182211753
Chicago/Turabian StyleChen, Xingtian, Wei Gong, Xiaoxu Wu, and Wenwu Zhao. 2021. "Estimating Economic Losses Caused by COVID-19 under Multiple Control Measure Scenarios with a Coupled Infectious Disease—Economic Model: A Case Study in Wuhan, China" International Journal of Environmental Research and Public Health 18, no. 22: 11753. https://doi.org/10.3390/ijerph182211753
APA StyleChen, X., Gong, W., Wu, X., & Zhao, W. (2021). Estimating Economic Losses Caused by COVID-19 under Multiple Control Measure Scenarios with a Coupled Infectious Disease—Economic Model: A Case Study in Wuhan, China. International Journal of Environmental Research and Public Health, 18(22), 11753. https://doi.org/10.3390/ijerph182211753







