Abstract
Background: Rising healthcare expenditures have been partially attributed to suboptimal management of inflammatory bowel diseases (IBD). Electronic health interventions may help improve care management for IBD patients, but there is a need to better understand patient perspectives on these emerging technologies. Aims: The primary aim was to evaluate patient satisfaction and experience with the UCLA eIBD mobile application, an integrative care management platform with disease activity monitoring tools and educational modules. The secondary objective was to capture patient feedback on how to improve the mobile application. Methods: We surveyed IBD patients treated at the UCLA Center for Inflammatory Bowel Diseases. The patient experience survey assessed the patients’ overall satisfaction with the application, perception of health outcomes after participation in the program, and feedback on educational modules as well as areas for application improvement. Results: 50 patients were included. The responses indicated that the patients were greatly satisfied with the ease of patient–provider communication within the application and appointment scheduling features (68%). A majority of respondents (54%) also reported that program participation resulted in improved perception of disease control and quality of life. Lastly, a majority of participants (79%) would recommend this application to others. Conclusions: Mobile tools such as UCLA eIBD have promising implications for integration into patients’ daily lives. This patient satisfaction study suggests the feasibility of using this mobile application by patients and providers. We further showed that UCLA eIBD and its holistic approach led to improved patient experience and satisfaction, which can provide useful recommendations for future electronic health solutions.
1. Introduction
Value-based healthcare (VBHC) can be described as the systematic pursuit of the triple aim in healthcare: to improve the individual’s experience, improve health outcomes, and reduce costs [1]. The concept of VBHC is particularly ready for application to long-term management of chronic illnesses since rising healthcare expenditures have been partially attributed to suboptimal management of chronic illnesses, including IBD [2]. The estimated annual disease-attributable cost of IBD is $6.3 billion [3]. Hospitalizations represented over a third of costs, outpatient services—one third. Reducing hospitalization and readmission rates, therefore, continues to be a challenge in chronic disease management. There is clearly an opportunity to reduce costs by increasing the efficiency of outpatient care and preventing hospitalizations.
Electronic health (e-health) interventions are one solution for more effective IBD care management beyond the clinical setting, both in terms of patient outcomes and cost reduction. Smartphone applications are widely available for consumers, and the large population of smartphone users make applications useful tools to manage chronic illnesses like IBD [4]. In fact, smartphone devices with mobile applications and short message reminders have been used effectively by patients with IBD of mild or moderate severity [5].
Furthermore, mobile health technologies have been shown to improve patient outcomes and quality of life [6]. Patient satisfaction with mobile technologies has been observed for many chronic diseases, including asthma [7], HIV [8], diabetes [9], atrial fibrillation [10], and IBD [11]. IBD patients generally have positive views on mobile applications, but there are desirable improvements. A study of Con et al. [11] surveying 86 IBD patients found that 98.8% of the participants were willing to use communication technologies for IBD management, with mobile applications being one of the top two preferred forms. These previous IBD mobile technologies were often created to assess a major single aspect such as quality of life [5], education curriculum [12], or diets [13]. Additional features that patients seek in their chronic disease management applications include easy user interface [14], tracking of disease symptoms [11], and easy access to medical data and services [11].
A systematic assessment of 26 IBD mobile applications found that applications offered a variety of features including diary functionality, pain tracking, bowel movement tracking, and reminders, with application’s content playing a major role in driving patient behavior change [4]. The MyIBD Coach telemedicine tool, which monitors adherence, disease activity, quality of life, and mental health among other measures through validated questionnaires, was shown to be successful, with high rates of patient satisfaction and compliance [15]. It involves collaboration among healthcare providers but is not synchronized with electronic medical records and lacks educational application features on alternative medicine, behavioral health, and physical activity.
To enhance VBHC in IBD, we developed UCLA eIBD to integrate various successful features of previous applications (e.g., appointment reminders, medication trackers) in addition to a healthcare provider portal. UCLA eIBD seeks to provide patients more agency in managing their IBD by increasing their access to healthcare professionals and providing self-help educational modules. Access to care providers through a messaging application provides patients with fast feedback on their conditions and streamlines patient care [16]. The application also contains disease activity, quality of life, and work productivity surveys that facilitate interactions between patients and providers. These tools allow healthcare providers to monitor patients’ disease activity and give direct feedback. This comprehensive application therefore seeks to enhance patient outcomes by including direct connections to the healthcare team and extensive module options.
We previously conducted a pilot study of UCLA eIBD, which found significantly fewer endoscopies and decreases in healthcare utilization, long-term steroid use and IBD-related costs [17]. While it is important to evaluate the efficacy and outcomes of IBD management platforms, it is just as crucial to understand patients’ satisfaction with these platforms to inform their feasibility. Gathering user feedback is necessary to develop the next generation of applications, improve product design, and reduce the gap between application developers and consumers [18,19,20]. This study therefore aims to provide an evaluation of perceived patient satisfaction and experience with the UCLA eIBD mobile application.
2. Materials and Methods
2.1. Objectives
The primary objective was to measure patient satisfaction and experience with the UCLA eIBD mobile application for care management. The secondary objective was to capture patient feedback on how to improve the mobile application.
2.2. Design and Population
We surveyed IBD patients treated at the UCLA Center for Inflammatory Bowel Diseases from October 2017 to October 2018. Included patients were at least 18 years old; diagnosed with Crohn’s disease (CD) or ulcerative colitis (UC) either by means of endoscopy, imaging, or pathology; and had objectively logged into the application in the past year (assessed on the platform). Patients with intestinal cancer, active chemotherapy, or a known intestinal infection were excluded.
All the eligible patients who had logged into the application in the past year were emailed and asked to complete a patient experience survey. Those who did not complete the survey in response to the initial email were followed up and interviewed via phone. No sample size estimation was performed.
2.3. Description of UCLA eIBD
UCLA eIBD is a mobile application that administers a clinic-centered, care management program to its users (Figure 1). It was designed to be a comprehensive tool for patients’ long-term disease management in the IBD outpatient setting. The features of this application include disease activity monitoring, messaging, educational modules, lifestyle modules, and electronic cognitive behavioral therapy (eCBT). The platform is also integrated with UCLA Health’s electronic medical records, allowing patients to view their testing and laboratory results within the application.
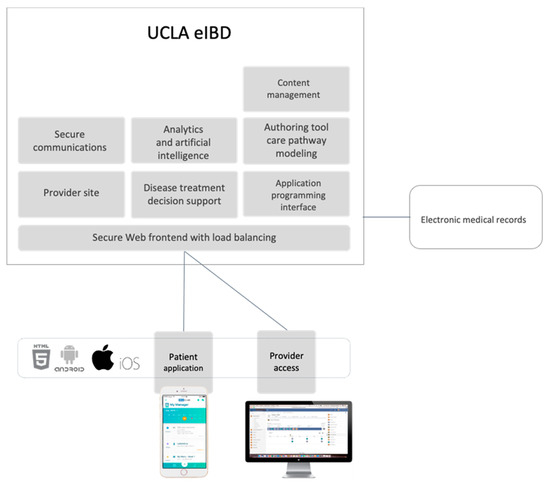
Figure 1.
The UCLA eIBD mobile application is an integrative care management platform for patients and providers.
For disease activity monitoring, a previously validated tool called the Mobile Health Index was integrated to assess the patients’ disease activity, quality of life, and work productivity [21]. If the surveys indicated poor disease control or a significant change from prior surveys, a message was automatically generated through the application to clinic staff. The enrolled patients could also elect to take these surveys in their own time if they felt they were experiencing a sudden change in their health.
Lastly, the application provided education through several optional interactive modules designed to promote healthy lifestyle habits, including nutrition (My Menu), exercise (My Yoga, My Fitness), relaxation (My Acupressure, My Meditation), and mental health (My Coach). My Menu teaches patients about specific foods to eat and avoid and includes recipes (breakfast, snack, lunch and dinner) designed for IBD patients. My Yoga provides a 6-week program promoting relaxation and flexibility for users. My Acupressure teaches patients about different pressure points for alleviating IBD pain via instructional videos and pictures. My Meditation is a self-guided mindfulness therapy tool that aims to reduce stress-related health issues. My Coach is a personalized mental life coaching program (6-week mental support program) aimed at improving mental well-being and stress management through a cognitive behavioral therapy method.
2.4. Data Collection and Outcomes
Patient demographic data were acquired via chart review. The data from the patient experience survey were collected via REDCap [22]. The patient experience survey (Table 1) consisted of 24 items aimed at assessing the patients’ overall satisfaction with the application and their perception of health outcomes after participation in the program. Responses were provided either via a Likert scale or open text. Questionnaire items addressing the application’s features and interface requested feedback on the ease of application use, ability to communicate with staff, and informativeness of modules. Questionnaire items pertaining to the patient’s outcomes asked the patients how effective they felt the application was at improving disease control, work productivity, and quality of life. Lastly, the patients could provide optional open-ended feedback via free text input on ways to improve the application.

Table 1.
Patient experience survey.
3. Results
3.1. Patient Demographics
In total, 151 patients had been active on the mobile application in the past year, of whom 50 patients responded and completed the survey and thus were included in this study. Regarding the type of IBD, 44% were diagnosed with CD (n = 22), 56%—with UC (n = 28). Our inclusion cohort had a mean age of 43 years (SD, 14 years) and an average BMI of 25.3 (SD, 6.6). Of the patients, 44% were female, and the majority were White (42%) and non-Hispanic (90%) (Table 2). Most of the patients were non-smokers (78%), and 28% of the patients reported alcohol use. The patients stated use of the following medications: anti-TNF (34%), ASA (16%), combination therapy (32%), IMM (10%), and steroids (6%). Previous abdominal surgeries were reported in 36% of the participants.

Table 2.
Patient demographics.
3.2. Patient Satisfaction
Fifty participants out of the 151 users responded and completed the patient experience survey to provide feedback on the mobile application (Table 1). Responses to the Likert scale questions indicated that the patients were overall satisfied with the patient–provider communication interface of the application. When asked how easy it was to communicate with the program’s staff overall, 52% of the participants responded with “very easy” and 16% responded with “somewhat easy”. A majority of the participants also found it easy to schedule appointments through the application, with 52% and 16% responding with “very easy” and “somewhat easy”, respectively. In addition, a large majority (88%) of the participants reported that the frequency of completing laboratory tests and surveys and scheduling clinic visits was “just right” (Table 1). Regarding the ease of application use, 74% of the participants indicated the application was either “very easy” or “somewhat easy” to navigate.
Additionally, a majority of the participants reported an improved perception of disease control and QoL; 54% of the participants indicated significant or some improvement in their disease control. When asked how program participation affected QoL, 26% indicated significant improvement, 30%—some improvement. Regarding work productivity, 44% indicated significant or some improvement.
When the participants were asked whether they would recommend this application to their friends, family, or other patients on a ten-point scale, with 10 being most likely, the median score was 8, and 79% indicated a score greater than 5. When asked about how informative the application was, 46% of the patients felt that the application was “somewhat” or “very” informative.
3.3. Patient Usage of Educational Modules
A majority of the patients completed modules as part of their participation in the program. The most used modules were My Fitness and My Menu (Table 1). Among the patients who participated in the CBT modules (12%), 28% indicated significant or some improvement in their mental health.
When asked about what they liked and disliked about the modules, the patients identified positive aspects to be the modules’ informative content, ease of use, and support of overall well-being (Table 3). For example, one patient said, “They’re easy and I feel great afterwards.” Another patient expressed liking the modules because they “encourage me to take care of my whole self instead of the focus just being on taking my meds”.

Table 3.
The patients’ optional feedback on the modules (n = 50). The patients provided open-ended feedback about the educational modules. Their responses were grouped into categories based on the common themes identified across the responses.
The most common reason for not liking the modules was being unsure of the purpose or need for them (8%), particularly for the modules where patients already had their own interventions in place. For example, one patient said they “didn’t feel [the modules] applied to me” while another expressed that they “thought [the module] was good but [I have my] own routine for working out [with regards to My Fitness]”.
3.4. Patient Feedback
In the patient experience survey, the patients could provide optional suggestions about additional topics and functionalities they would like the application to cover which were not presently included (Table 4). One participant, for instance, suggested adding a subsection about nutritional advice related to veganism within the My Menu module. Other recommendations included adding a “symptoms tracker”, allowing patients to indicate what symptoms or lack thereof they were experiencing and generating in-application reminders for blood draws or laboratory orders. The other patient-recommended categories to add were the ability to chart laboratory results, side effects of their consequent medications, and gender-specific health topics (Table 4).

Table 4.
The patients’ optional feedback on UCLA eIBD. The patients provided open-text suggestions to improve the application in general. These suggestions were grouped into categories of comment types, including improvements in application content such as possible additional topics and features, as well as miscellaneous critiques.
The patients’ feedback regarding general comments about the application is also shown in Table 4 (miscellaneous improvement suggestions). One patient stated, “I think this is a great idea and will be very helpful to future patients. I really like being able to communicate with the office without always having to call.” Most patients who provided comments also highlighted aspects that could be improved, such as the application’s interface (e.g., adding a touch ID option to log in; preventing automatic logoff from the application). Other participants reported critical feedback on the application’s content. For instance, one patient stated that the application “is good for people new to IBD, but doesn’t offer as much for people who have had IBD for a while and want more in depth information”.
3.5. Summary of Principal Findings
The outcomes suggest that the patients strongly favored the ease of patient–provider communication, with 78% being satisfied. Beneficial outcomes were also seen in patient-reported measures, with 54% reporting a perceived improvement in disease control and 56% reporting a perceived improvement in QoL, indicating that a majority of patients felt the platform positively impacted their health. Additionally, the participants rated this application with a median score out of 10 (10 being most likely) to recommend this application to friends, family, or other patients. My Fitness and My Menu were the two most used optional wellness modules, each reaching the 34% completed status.
4. Discussion
4.1. Strengths and Comparisons
Our study collected feedback on patient experiences with the UCLA eIBD application after one year of use. Our results could provide guidance for further application development and provide critical feedback for other e-health applications like this one. In fact, mobile tools such as UCLA eIBD have been shown to have promising implications in improving healthcare delivery and integrating into patients’ daily lives. Earlier comparison studies of UCLA eIBD found impacts on costs and healthcare utilization and identified its unique features, such as automated messaging to care coordinators [17,23,24,25]. To complement the previous outcome studies, this study aimed to understand patients’ satisfaction and feedback to help elucidate gaps in the current e-health technologies and inform future designs.
For instance, GI Buddy is a mobile application developed by the Crohn’s Colitis Foundation which enables patients to self-monitor their disease and receive reminders about clinical appointments; however, users cannot directly interact with their providers [26]. Similarly, while the current applications for IBD may be useful for patient monitoring and self-management, many lack professional medical involvement and adherence to clinical guidelines [4]. UCLA eIBD addressed this gap by allowing users to make appointments and message their providers via the platform, in which a majority of users found it “easy” or “very easy” to communicate with their providers. Another self-management tool, myIBD Coach, showed feasibility among patients and providers [15]. As many as 79% of UCLA eIBD users would recommend this application to others (indicated by a score of greater than 5 on the recommendation score item), compared to the 93% found in the myIBD Coach feasibility study [15].
The findings of this novel patient satisfaction study demonstrate the feasibility of UCLA eIBD as a home monitoring tool and some advantages it can provide for both patients and providers. In addition to the patient–provider communication features, the platform’s educational modules are more diverse than the previous tools and provide patients with more alternatives to aid traditional medicine, such as acupuncture, cognitive behavioral therapy, and meditation. These optional modules may improve IBD patients’ well-being and productivity beyond the scope of their disease. For providers, tracking the various modules that the patients use can also provide guidance for tailoring treatment and counseling to the patients’ interests, including nutrition, exercise, and mental health. Lastly, the holistic nature of the application, including features about alternative medicine and assessments for work productivity via the Mobile Health Index, can more completely address the complex, multidimensional factors of chronic disease management.
While the integration of mobile health in IBD management is rapidly expanding, our study also presents novel data from the patient perspective and emphasizes a patient-centered approach towards mobile application development. For instance, the patients’ suggestions to improve the application were centered on specific content interests and the need for additional educational categories (e.g., female health topics), rather than technical problems or lack of need in an application. The fact that the suggestions were less focused on design features could be explained by the overall satisfaction rate of 74% of the participants finding the application easy to navigate. The current and future applications can thus utilize these methods and/or findings to adapt their platforms to address patients’ specific needs, improve satisfaction with their product, and better engage patients in their medical care beyond a doctor’s office visit.
4.2. Limitations
Some study limitations should be noted. As the selected patients were individuals who use smartphones, they may be more adept at the usage of applications. Participants were also actively recruited and agreed to participate in this study; thus, a selection bias may have impacted the study results due to the participants being predisposed to wanting to improve their health via e-health solutions. We further acknowledge the sample size was small and relatively homogenous; however, we feel it was adequate for the purpose of directing the future development of this UCLA application and other healthcare applications.
Additionally, the fact that we invited participants to evaluate the application’s feasibility rather than making it mandatory during application usage may explain the response rate of 33%. The response rate should further be considered in the context of challenges associated with adopting e-health technologies into the healthcare space. The obstacles to widespread long-term integration of e-health technologies (e.g., loss of interest, data entry burdens) are still being investigated [27,28]. Despite the growing population of individuals who use mobile health applications, many stop using them over time [29]. Our findings help provide insight to consumer perspectives on application usability and possible explanations to circumvent these challenges.
4.3. Future Directions
In an era where the use of mobile technology has become irreplaceable in daily life, there is undoubted benefit of incorporating e-health applications in the management of chronic conditions. Studies have shown proven effect of mobile applications, but also that patients still desire improvements to the existing solutions. We showed that UCLA eIBD and its holistic approach led to greater patient experience and satisfaction, which can provide useful recommendations for healthcare providers and application developers. However, larger and controlled studies are recommended to assess its efficacy at a larger scale and its impact on costs.
Author Contributions
A.Z.: study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; study supervision; A.N.: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; C.R.: study concept and design; drafting of the manuscript; critical revision of the manuscript for important intellectual content; A.K.: acquisition of data; administrative, technical, or material support, drafting of the manuscript; critical revision of the manuscript for important intellectual content; E.E.: revision of the manuscript for important intellectual content; D.H.: study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; study supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Institutional Review Board at UCLA with IRB protocol number 17-001208. All the procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all the individuals included in the study.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Berwick, D.M.; Nolan, T.W.; Whittington, J. The Triple Aim: Care, Health, and Cost. Health Aff. 2008, 27, 759–769. [Google Scholar] [CrossRef]
- Thorpe, K.E. The Rise in Health Care Spending and What To Do About It. Health Aff. 2005, 24, 1436–1445. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kappelman, M.D.; Rifas–Shiman, S.L.; Porter, C.Q.; Ollendorf, D.A.; Sandler, R.S.; Galanko, J.A.; Finkelstein, J.A. Direct Health Care Costs of Crohn’s Disease and Ulcerative Colitis in US Children and Adults. Gastroenterology 2008, 135, 1907–1913. [Google Scholar] [CrossRef]
- Con, D.; De Cruz, P.; Van Mierlo, T.; Aramaki, E. Mobile Phone Apps for Inflammatory Bowel Disease Self-Management: A Systematic Assessment of Content and Tools. JMIR mHealth uHealth 2016, 4, e13. [Google Scholar] [CrossRef] [PubMed]
- Stunkel, L.; Karia, K.; Okoji, O.; Warren, R.; Jean, T.; Jacob, V.; Swaminath, A.; Scherl, E.; Bosworth, B. Impact on quality of life of a smart device mobile application in patients with inflammatory bowel disease. Am. J. Gastroenterol. 2012, 107, S635–S636. [Google Scholar] [CrossRef]
- Atreja, A.; Khan, S.; Szigethy, E.; Otobo, E.; Shroff, H.; Chang, H.; Keefer, L.; Rogers, J.; Deorocki, A.; Ullman, T.; et al. Improved quality of care for IBD patients using healthPROMISE App: A randomized, control trial. Am. J. Gastroenterol. 2018, 113, S1. [Google Scholar]
- Geryk, L.L.; Roberts, C.A.; Sage, A.J.; Coyne-Beasley, T.; Sleath, B.L.; Carpenter, D.M.; Hall, A.; Rhee, H.; Morrison, C.; Morrison, D. Parent and Clinician Preferences for an Asthma App to Promote Adolescent Self-Management: A Formative Study. JMIR Res. Protoc. 2016, 5, e229. [Google Scholar] [CrossRef]
- Swendeman, D.; Farmer, S.; Mindry, D.; Lee, S.-J.; Medich, M. HIV Care Providers’ Attitudes regarding Mobile Phone Applications and Web-Based Dashboards to support Patient Self-Management and Care Coordination: Results from a Qualitative Feasibility Study. J. HIV AIDS 2016, 2, 1310–1318. [Google Scholar]
- Lyles, C.R.; Harris, L.T.; Le, T.; Flowers, J.; Tufano, J.; Britt, D.; Hoath, J.; Hirsch, I.B.; Goldberg, H.I.; Ralston, J.D. Qualitative Evaluation of a Mobile Phone and Web-Based Collaborative Care Intervention for Patients with Type 2 Diabetes. Diabetes Technol. Ther. 2011, 13, 563–569. [Google Scholar] [CrossRef]
- Hirschey, J.; Bane, S.; Mansour, M.; Sperber, J.; Agboola, S.; Kvedar, J.; Jethwani, K. Evaluating the Usability and Usefulness of a Mobile App for Atrial Fibrillation Using Qualitative Methods: Exploratory Pilot Study. JMIR Hum. Factors 2018, 5, e13. [Google Scholar] [CrossRef]
- Con, D.; Jackson, B.; Gray, K.; De Cruz, P. eHealth for inflammatory bowel disease self-management—The patient perspective. Scand. J. Gastroenterol. 2017, 2017, 1–8. [Google Scholar] [CrossRef]
- Hommel, K.A.; Gray, W.N.; Hente, E.; Loreaux, K.; Ittenbach, R.F.; Maddux, M.; Baldassano, R.N.; Sylvester, F.A.; Crandall, W.; Doarn, C.; et al. The Telehealth Enhancement of Adherence to Medication (TEAM) in pediatric IBD trial: Design and methodology. Contemp. Clin. Trials 2015, 43, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Vlahou, C.H.; Cohen, L.L.; Woods, A.M.; Lewis, J.D.; Gold, B.D. Age and Body Satisfaction Predict Diet Adherence in Adolescents with Inflammatory Bowel Disease. J. Clin. Psychol. Med. Settings 2008, 15, 278–286. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, L.; Chang, P.; Lamb, K.V.; Cui, Y.; Wua, Y. What features of smartphone medication applications are patients with chronic diseases and caregivers looking for? Stud. Health Technol. Inform. 2016, 225, 515–519. [Google Scholar]
- De Jong, M.; Van Der Meulen-De Jong, A.; Romberg-Camps, M.; Degens, J.; Becx, M.; Markus, T.; Tomlow, H.; Cilissen, M.; Ipenburg, N.; Verwey, M.; et al. Development and Feasibility Study of a Telemedicine Tool for All Patients with IBD: MyIBDcoach. Inflamm. Bowel. Dis. 2017, 23, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Ventola, C.L. Mobile Devices and Apps for Health Care Professionals: Uses and Benefits. P T: A peer-reviewed. J. Formul. Manag. 2014, 39, 356–364. [Google Scholar]
- Van Deen, W.K.; Spiro, A.; Burak Ozbay, A.; Skup, M.; Centeno, A.; Duran, N.E.; Lacey, P.N.; Jatulis, D.; Esrailian, E.; van Oijen, M.G.H.; et al. The impact of value-based healthcare for inflammatory bowel diseases on healthcare utilization: A pilot study. Eur. J. Gastroenterol. Hepatol. 2017, 29, 331–337. [Google Scholar] [CrossRef]
- Jake-Schoffman, D.E.; Silfee, V.J.; Waring, M.E.; Boudreaux, E.D.; Sadasivam, R.S.; Mullen, S.P.; Carey, J.L.; Hayes, R.B.; Ding, E.Y.; Bennett, G.G.; et al. Methods for Evaluating the Content, Usability, and Efficacy of Commercial Mobile Health Apps. JMIR mHealth uHealth 2017, 5, e190. [Google Scholar] [CrossRef] [PubMed]
- Liew, M.S.; Zhang, J.; See, J.; Ong, Y.L. Usability Challenges for Health and Wellness Mobile Apps: Mixed-Methods Study Among mHealth Experts and Consumers. JMIR mHealth uHealth 2019, 7, e12160. [Google Scholar] [CrossRef]
- Maramba, I.; Chatterjee, A.; Newman, C. Methods of usability testing in the development of eHealth applications: A scoping review. Int. J. Med. Inform. 2019, 126, 95–104. [Google Scholar] [CrossRef]
- Deen, W.K.; Van Jong, A.E.V.D.M.; Parekh, N.K.; Kane, E.; Zand, A.; Dinicola, C.A.; Hall, L.; Inserra, E.K.; Choi, J.M.; Ha, C.Y.; et al. Development and Validation of an Inflammatory Bowel Diseases Monitoring Index for Use with Mobile Health Technologies. Clin. Gastroenterol. Hepatol. 2016, 14, 1742–1750.e7. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Walsh, A.; Travis, S. What’s app? Electronic health technology in inflammatory bowel disease. Intest. Res. 2018, 16, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Yin, A.L.; Hachuel, D.; Pollak, J.P.; Scherl, E.J.; Estrin, D. Digital Health Apps in the Clinical Care of Inflammatory Bowel Disease: Scoping Review. J. Med. Int. Res. 2019, 21, e14630. [Google Scholar] [CrossRef]
- Kelso, M.; Feagins, L.A. Can Smartphones Help Deliver Smarter Care for Patients with Inflammatory Bowel Disease? Inflamm. Bowel. Dis. 2018, 24, 1453–1459. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, O.; Atreja, A.; Markus-kennell, S.; Frederick, K. CCFA GI Buddy provides patient reported outcomes and IBD symptoms evaluation: P-50. Inflamm. Bowel. Dis. 2012, 18, 35–36. [Google Scholar] [CrossRef]
- Gutiérrez-Ibarluzea, I.; Chiumente, M.; Dauben, H.-P. The Life Cycle of Health Technologies. Challenges and Ways Forward. Front. Pharmacol. 2017, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.; Cannady, M.; Howley, K.; Shea, C.; Snyderman, R. An evaluation of mHealth adoption and health self-management in emerging adulthood. AMIA Annu. Symp. Proc. AMIA Symp. 2020, 2019, 1021–1030. [Google Scholar] [PubMed]
- Krebs, P.; Duncan, D.T. Health App Use among US Mobile Phone Owners: A National Survey. JMIR mHealth uHealth 2015, 3, e101. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).