Comparison of Polydrug Use Prevalences and Typologies between Men Who Have Sex with Men and General Population Men, in Madrid and Barcelona
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Variables and Data Collection
2.3. Data Analysis
3. Results
3.1. Participant’s General Characteristics
3.2. Prevalence of Drug Use in MSM and GPM
3.3. Differences in Drug Use Risk between the Two Groups of Men
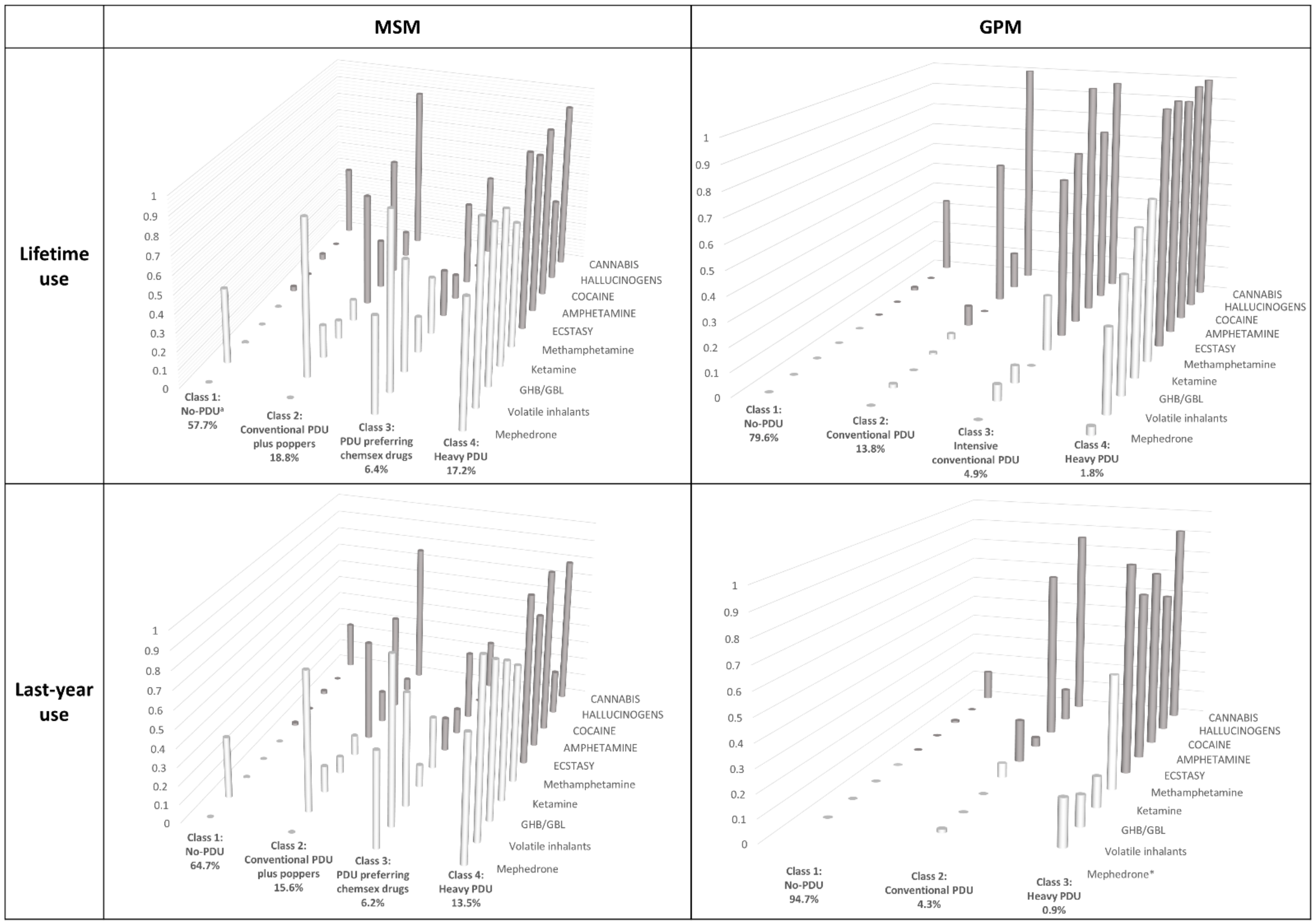
3.4. PDU Typologies
- -
- Class (1) No-PDU, with a high probability of only cannabis and volatile inhalants use (0.38 and 0.41) and a very low or zero probability (<0.05) of using any other drugs considered;
- -
- Class (2) Conventional PDU plus poppers, with extremely high probability of using both cannabis and volatile inhalants (0.85), very high probability of using cocaine and ecstasy (>0.6), and medium probability of using amphetamine, methamphetamine and GHB/GBL (0.12–0.27);
- -
- Class (3) PDU preferring chemsex drugs, with almost universal use of volatile inhalants (0.95), very high probability of using GHB/GBL, mephedrone, methamphetamine, cocaine and cannabis (0.44–0.61), and intermediate probability of using other drugs under consideration, except hallucinogens;
- -
- Class (4) Heavy-PDU, with extremely high use-probability for all drugs (≥0.68) except hallucinogens.
- -
- Class (1) No-PDU, very similar to the homonymous MSM class but with hardly any volatile inhalant use;
- -
- Class (2) Conventional PDU, similar to the homonymous MSM group, but with zero or ≤2% probability of inhalant, GHB/GBL, ketamine, mephedrone, amphetamine, and methamphetamine use, lower probability of ecstasy use, and similar use of cocaine, hallucinogens, and cannabis;
- -
- Class (3) Intensive conventional-PDU, shows higher levels of more traditional drugs being used than MSM;
- -
- Class (4) Heavy-PDU, again similar to the MSM group, but with practically universal use of non-chemsex drugs and lower chemsex drug use, especially mephedrone.
4. Discussion
4.1. Main Findings
4.2. Comparison with Other Studies
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Methysos Project Group
References
- Gonzales, G.; Henning-Smith, C. Health Disparities by Sexual Orientation: Results and Implications from the Behavioral Risk Factor Surveillance System. J. Community Health 2017, 42, 1163–1172. [Google Scholar] [CrossRef]
- Jin, F.; Dore, G.J.; Matthews, G.; Luhmann, N.; Macdonald, V.; Bajis, S.; Baggaley, R.; Mathers, B.; Verster, A.; Grulich, A.E. Prevalence and incidence of hepatitis C virus infection in men who have sex with men: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 39–56. [Google Scholar] [CrossRef]
- Kneale, D.; Thomas, J.; French, R. Inequalities in Health and Care Among Lesbian, Gay, and Bisexual People Aged 50 and Older in the United Kingdom: A Systematic Review and Meta-analysis of Sources of Individual Participant Data. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 75, 1758–1771. [Google Scholar] [CrossRef]
- Mercer, C.H.; Prah, P.; Field, N.; Tanton, C.; Macdowall, W.; Clifton, S.; Hughes, G.; Nardone, A.; Wellings, K.; Johnson, A.M.; et al. The health and well-being of men who have sex with men (MSM) in Britain: Evidence from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). BMC Public Health 2016, 16, 525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, C.E.; Vasilenko, S.A.; Fish, J.N.; Lanza, S.T. Sexual minority health disparities: An examination of age-related trends across adulthood in a national cross-sectional sample. Ann. Epidemiol. 2019, 31, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Wei, D.; Wang, X.; You, X.; Luo, X.; Hao, C.; Gu, J.; Peng, S.; Yang, X.; Hao, Y.; Silenzio, V.M.B.; et al. Prevalence of depression, anxiety and suicide among men who have sex with men in China: A systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 2020, 29, e136. [Google Scholar] [CrossRef] [PubMed]
- Knight, D.A.; Jarrett, D. Preventive Health Care for Men Who Have Sex with Men. Am. Fam. Physician 2015, 91, 844–851. [Google Scholar] [PubMed]
- Rosinska, M.; Gios, L.; Nostlinger, C.; Vanden Berghe, W.; Marcus, U.; Schink, S.; Sherriff, N.; Jones, A.M.; Folch, C.; Dias, S.; et al. Prevalence of drug use during sex amongst MSM in Europe: Results from a multi-site bio-behavioural survey. Int. J. Drug Policy 2018, 55, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.J.; Bourne, A.; Weatherburn, P.; Reid, D.; Marcus, U.; Hickson, F. Illicit drug use among gay and bisexual men in 44 cities: Findings from the European MSM Internet Survey (EMIS). Int. J. Drug Policy 2016, 38, 4–12. [Google Scholar] [CrossRef]
- Guerra, F.M.; Salway, T.J.; Beckett, R.; Friedman, L.; Buchan, S.A. Review of sexualized drug use associated with sexually transmitted and blood-borne infections in gay, bisexual and other men who have sex with men. Drug Alcohol Depend. 2020, 216, 108237. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.; Shahmanesh, M.; Gafos, M. Chemsex behaviours among men who have sex with men: A systematic review of the literature. Int. J. Drug Policy 2019, 63, 74–89. [Google Scholar] [CrossRef] [PubMed]
- Tomkins, A.; George, R.; Kliner, M. Sexualised drug taking among men who have sex with men: A systematic review. Perspect. Public Health 2018, 139, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Guerras, J.M.; Hoyos, J.; Agusti, C.; Casabona, J.; Sordo, L.; Pulido, J.; de la Fuente, L.; Belza, M.J.; Euro HIVEdat Working Group. Substance use in Sexual Context among Spanish Resident Men who have Sex with Men. Adicciones 2020, 0, 1371. [Google Scholar] [PubMed]
- Guerras, J.M.; Hoyos, J.; Agusti, C.; Chanos, S.; Pichon, F.; Kuske, M.; Cigan, B.; Fuertes, R.; Stefanescu, R.; Ooms, L.; et al. Association of Sexualized Drug Use Patterns with HIV/STI Transmission Risk in an Internet Sample of Men Who Have Sex with Men from Seven European Countries. Arch. Sex. Behav. 2021, 50, 461–477. [Google Scholar] [CrossRef] [PubMed]
- Hampel, B.; Kusejko, K.; Kouyos, R.D.; Boni, J.; Flepp, M.; Stockle, M.; Conen, A.; Beguelin, C.; Kunzler-Heule, P.; Nicca, D.; et al. Chemsex drugs on the rise: A longitudinal analysis of the Swiss HIV Cohort Study from 2007 to 2017. HIV Med. 2020, 21, 228–239. [Google Scholar] [CrossRef]
- Coyer, L.; Boyd, A.; Davidovich, U.; van Bilsen, W.P.H.; Prins, M.; Matser, A. Increase in recreational drug use between 2008 and 2018: Results from a prospective cohort study among HIV-negative men who have sex with men. Addiction 2021, 0, 15666. [Google Scholar] [CrossRef] [PubMed]
- Barrett, P.; O’Donnell, K.; Fitzgerald, M.; Schmidt, A.J.; Hickson, F.; Quinlan, M.; Keogh, P.; O’Connor, L.; McCartney, D.; Igoe, D. Drug use among men who have sex with men in Ireland: Prevalence and associated factors from a national online survey. Int. J. Drug Policy 2019, 64, 5–12. [Google Scholar] [CrossRef] [Green Version]
- Dirks, H.; Esser, S.; Borgmann, R.; Wolter, M.; Fischer, E.; Potthoff, A.; Jablonka, R.; Schadendorf, D.; Brockmeyer, N.; Scherbaum, N. Substance use and sexual risk behaviour among HIV-positive men who have sex with men in specialized out-patient clinics. HIV Med. 2012, 13, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Stall, R.; Paul, J.P.; Greenwood, G.; Pollack, L.M.; Bein, E.; Crosby, G.M.; Mills, T.C.; Binson, D.; Coates, T.J.; Catania, J.A. Alcohol use, drug use and alcohol-related problems among men who have sex with men: The Urban Men’s Health Study. Addiction 2001, 96, 1589–1601. [Google Scholar] [CrossRef]
- Gonzales, G.; Przedworski, J.; Henning-Smith, C. Comparison of Health and Health Risk Factors Between Lesbian, Gay, and Bisexual Adults and Heterosexual Adults in the United States: Results From the National Health Interview Survey. JAMA Intern. Med. 2016, 176, 1344–1351. [Google Scholar] [CrossRef] [Green Version]
- Boyd, C.J.; Veliz, P.T.; McCabe, S.E. Severity of DSM-5 cannabis use disorders in a nationally representative sample of sexual minorities. Subst. Abus. 2020, 41, 191–195. [Google Scholar] [CrossRef]
- Branstrom, R.; Pachankis, J.E. Sexual orientation disparities in the co-occurrence of substance use and psychological distress: A national population-based study (2008-2015). Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 403–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schuler, M.S.; Rice, C.E.; Evans-Polce, R.J.; Collins, R.L. Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug Alcohol Depend. 2018, 189, 139–146. [Google Scholar] [CrossRef]
- Lunn, M.R.; Cui, W.; Zack, M.M.; Thompson, W.W.; Blank, M.B.; Yehia, B.R. Sociodemographic Characteristics and Health Outcomes Among Lesbian, Gay, and Bisexual U.S. Adults Using Healthy People 2020 Leading Health Indicators. LGBT Health 2017, 4, 283–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCabe, S.E.; Hughes, T.L.; Bostwick, W.B.; West, B.T.; Boyd, C.J. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction 2009, 104, 1333–1345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roxburgh, A.; Lea, T.; de Wit, J.; Degenhardt, L. Sexual identity and prevalence of alcohol and other drug use among Australians in the general population. Int. J. Drug Policy 2016, 28, 76–82. [Google Scholar] [CrossRef]
- Goldstein, N.D.; Burstyn, I.; LeVasseur, M.T.; Welles, S.L. Drug use among men by sexual behaviour, race and ethnicity: Prevalence estimates from a nationally representative US sample. Int. J. Drug Policy 2016, 36, 148–150. [Google Scholar] [CrossRef]
- Hunter, L.J.; Dargan, P.I.; Benzie, A.; White, J.A.; Wood, D.M. Recreational drug use in men who have sex with men (MSM) attending UK sexual health services is significantly higher than in non-MSM. Postgrad. Med. J. 2014, 90, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Schuler, M.S.; Stein, B.D.; Collins, R.L. Differences in Substance Use Disparities Across Age Groups in a National Cross-Sectional Survey of Lesbian, Gay, and Bisexual Adults. LGBT Health 2019, 6, 68–76. [Google Scholar] [CrossRef]
- Woody, G.E.; VanEtten-Lee, M.L.; McKirnan, D.; Donnell, D.; Metzger, D.; Seage, G., 3rd; Gross, M.; Team, H.V.P. Substance use among men who have sex with men: Comparison with a national household survey. J. Acquir. Immune Defic. Syndr. 2001, 27, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Bergman, L.R.; Magnusson, D. A person-oriented approach in research on developmental psychopathology. Dev. Psychopathol. 1997, 9, 291–319. [Google Scholar] [CrossRef]
- Melendez-Torres, G.J.; Bourne, A.; Reid, D.; Hickson, F.; Bonell, C.; Weatherburn, P. Typology of drug use in United Kingdom men who have sex with men and associations with socio-sexual characteristics. Int. J. Drug Policy 2018, 55, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.H.; Cheung, D.H.; Guadamuz, T.E.; Wei, C.; Koe, S.; Altice, F.L. Latent class analysis of substance use among men who have sex with men in Malaysia: Findings from the Asian Internet MSM Sex Survey. Drug Alcohol Depend. 2015, 151, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Newcomb, M.E.; Ryan, D.T.; Greene, G.J.; Garofalo, R.; Mustanski, B. Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug Alcohol Depend. 2014, 141, 65–71. [Google Scholar] [CrossRef] [Green Version]
- Card, K.G.; Armstrong, H.L.; Carter, A.; Cui, Z.; Wang, L.; Zhu, J.; Lachowsky, N.J.; Moore, D.M.; Hogg, R.S.; Roth, E.A. A latent class analysis of substance use and culture among gay, bisexual and other men who have sex with men. Cult. Health Sex. 2018, 20, 1424–1439. [Google Scholar] [CrossRef] [PubMed]
- EMIS Spain. Encuesta Europea on-Line Para Hombres Que Tienen Sexo Con Hombres (EMIS-2017): Resultados en España. 2020. Available online: https://sigmaresearch.org.uk/files/local/EMIS-2017_National-Report_ES.pdf (accessed on 12 October 2021).
- Instituto Nacional de Estadística. Encuesta de Salud y Hábitos Sexuales. Spain. 2003. Available online: https://www.ine.es/uc/olvXwfzA (accessed on 20 August 2021).
- Observatorio Español de las Drogas y las Adicciones. Encuesta Sobre Alcohol y Drogas en España (EDADES), 1995–2017. Ministerio de Sanidad, Consumo y Bienestar Social. Spain. 2019. Available online: https://pnsd.sanidad.gob.es/profesionales/sistemasInformacion/sistemaInformacion/pdf/2019_Informe_EDADES.pdf (accessed on 20 August 2021).
- Espelt, A.; Mari-Dell′Olmo, M.; Penelo, E.; Bosque-Prous, M. Applied Prevalence Ratio estimation with different Regression models: An example from a cross-national study on substance use research. Adicciones 2016, 29, 105–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barros, A.J.; Hirakata, V.N. Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Med. Res. Methodol. 2003, 3, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, L.M.; Lanza, S.T. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences; John Wiley & Sons: Hoboken, NJ, USA, 2009; Volume 718. [Google Scholar]
- Achterbergh, R.C.A.; Druckler, S.; van Rooijen, M.S.; van Aar, F.; Slurink, I.A.L.; de Vries, H.J.C.; Boyd, A. Sex, drugs, and sexually transmitted infections: A latent class analysis among men who have sex with men in Amsterdam and surrounding urban regions, the Netherlands. Drug Alcohol Depend. 2020, 206, 107526. [Google Scholar] [CrossRef] [PubMed]
- Drew, A.L.; Jeffrey, B.L. poLCA: An R Package for Polytomous Variable Latent Class Analysis. J. Stat. Softw. 2011, 42, 1–29. [Google Scholar]
- Dziak, J.J.; Coffman, D.L.; Lanza, S.T.; Li, R.; Jermiin, L.S. Sensitivity and specificity of information criteria. Brief. Bioinform. 2020, 21, 553–565. [Google Scholar] [CrossRef]
- Prah, P.; Hickson, F.; Bonell, C.; McDaid, L.M.; Johnson, A.M.; Wayal, S.; Clifton, S.; Sonnenberg, P.; Nardone, A.; Erens, B.; et al. Men who have sex with men in Great Britain: Comparing methods and estimates from probability and convenience sample surveys. Sex. Transm. Infect. 2016, 92, 455–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| MSM | GPM a | |||
|---|---|---|---|---|
| n = 2658 | n = 1720 | |||
| n | % | n | % | |
| Age group | ||||
| 16–24 | 414 | 15.6 b | 330 | 19.2 |
| 25–34 | 1155 | 43.5 | 470 | 27.3 |
| 35–44 | 664 | 25.0 | 466 | 27.1 |
| 45–54 | 312 | 11.7 | 268 | 15.6 |
| 55–64 | 113 | 4.3 | 186 | 10.8 |
| Country of birth | ||||
| Spain | 1606 | 60.4 | 1431 | 91.3 |
| Latin American countries | 765 | 28.8 | 29 | 1.8 |
| Other countries | 287 | 10.8 | 108 | 6.9 |
| Size of place of residence (inhabitants) | ||||
| >1 million | 2073 | 78.7 | 665 | 38.7 |
| 50,001–1 million | 393 | 14.9 | 607 | 35.3 |
| 10,001–50,000 | 97 | 3.7 | 303 | 17.6 |
| ≤10,000 | 72 | 2.7 | 145 | 8.4 |
| Education level | ||||
| ≤lower secondary (≤10 education years) | 169 | 6.4 | 668 | 39.0 |
| Upper secondary (11–12 education years) | 905 | 34.2 | 650 | 38.0 |
| University (>12 education years) | 1572 | 59.4 | 394 | 23.0 |
| Employment status c | ||||
| Employed | 1262 | 75.3 | 1134 | 66.9 |
| Unemployed | 120 | 7.2 | 198 | 11.7 |
| Other | 293 | 17.5 | 362 | 21.4 |
| Cohabitation c | ||||
| Alone | 682 | 39.9 | 285 | 17.0 |
| Spouse/partner without children d | 359 | 21.0 | 403 | 24.1 |
| Spouse/partner with children d | 8 | 0.5 | 450 | 26.9 |
| Children without spouse/partner d | 4 | 0.2 | 33 | 2.0 |
| Other relatives | 270 | 15.8 | 494 | 29.5 |
| Non-relatives exclusively | 385 | 22.5 | 8 | 0.5 |
| Prevalence in MSM a | Prevalence in GPM | Crude Prevalence Ratio MSM/GPM | ||||
|---|---|---|---|---|---|---|
| Point | 95% CI | Point | 95% CI | Point | 95% CI b | |
| Psychoactive Drug c | ||||||
| Lifetime drug use | ||||||
| Cannabis | 57.3 | 55.4–59.2 | 47.1 | 44.7–49.5 | 1.2 | 1.1–1.3 |
| Hallucinogens | 10.4 | 9.3–11.7 | 7.9 | 6.6–9.2 | 1.3 | 1.1–1.6 |
| Cocaine | 32.9 | 31.2–34.8 | 16.7 | 14.9–18.5 | 2.0 | 1.8–2.2 |
| Amphetamine | 21.0 | 19.5–22.6 | 5.5 | 4.4–6.6 | 3.8 | 3.1–4.7 |
| Ecstasy | 31.2 | 29.5–33.0 | 6.3 | 5.2–7.5 | 5.0 | 4.1–6.0 |
| Methamphetamine | 16.1 | 14.7–17.6 | 2.6 | 1.9–3.5 | 6.2 | 4.6–8.4 |
| Ketamine | 17.7 | 16.3–19.2 | 1.2 | 0.7–1.8 | 14.7 | 9.5–22.9 |
| GHB/GBL | 22.3 | 20.8–24.0 | 1.2 | 0.7–1.8 | 18.6 | 12.0–28.8 |
| Volatile inhalants | 62.4 | 60.6–64.3 | 1.2 | 0.7–1.8 | 52.0 | 33.8–80.0 |
| Mephedrone | 15.1 | 13.8–16.6 | 0.1 | 0.0–0.3 | 151.2 | 33.4–685.3 |
| Any drug d | 77.6 | 76.0–79.2 | 48.7 | 46.8–50.6 | 1.6 | 1.5–1.7 |
| Last-year drug use | ||||||
| Cannabis | 40.7 | 38.8–42.6 | 17.8 | 15.9–19.7 | 2.3 | 2.0–2.6 |
| Hallucinogens | 4.2 | 3.5–5.1 | 1.2 | 0.7–1.8 | 3.5 | 2.2–5.6 |
| Cocaine | 23.6 | 22.1–25.3 | 5.1 | 4.1–6.3 | 4.6 | 3.7–5.7 |
| Amphetamine | 13.5 | 12.3–14.9 | 1.1 | 0.6–1.6 | 12.3 | 7.8–19.5 |
| Ecstasy | 23.1 | 21.5–24.8 | 1.8 | 1.1–2.4 | 12.8 | 9.0–18.3 |
| Methamphetamine | 12.2 | 11.0–13.5 | 0.8 | 0.4–1.2 | 15.2 | 8.9–26.0 |
| Ketamine | 12.4 | 11.2–13.8 | 0.2 | 0.0–0.5 | 62.1 | 21.3–181.2 |
| GHB/GBL | 17.7 | 16.3–19.2 | 0.1 | 0.0–0.4 | 176.8 | 39.4–794.1 |
| Volatile inhalants | 51.7 | 49.8–53.7 | 0.2 | 0.0–0.5 | 258.5 | 89.5–746.1 |
| Mephedrone | 12.4 | 11.2–13.7 | 0.0 | 0.0–0.2 | ∞ | _ |
| Any drug d | 67.0 | 65.2–68.8 | 19.8 | 18.3–21.3 | 3.4 | 3.1–3.7 |
| N e | 2658 | 1720 | ||||
| Lifetime Drug Use | Last-Year Drug Use | |||
|---|---|---|---|---|
| Psychoactive Drug b | aPR | 95% CI | aPR | 95% CI |
| Cannabis | 1.1 | 1.1–1.3 | 2.0 | 1.8–2.3 |
| Hallucinogens | 1.2 | 0.9–1.5 | 2.8 | 1.6–5.1 |
| Cocaine | 1.8 | 1.6–2.2 | 3.9 | 3.1–5.1 |
| Amphetamine | 3.6 | 2.9–4.7 | 11.3 | 6.7–19.0 |
| Ecstasy | 4.2 | 3.4–5.2 | 10.1 | 6.8–15.2 |
| Methamphetamine | 5.4 | 3.9–7.6 | 13.6 | 7.5–24.9 |
| Ketamine | 11.6 | 7.3–18.6 | 77.4 | 19.7–305.5 |
| GHB/GBL | 15.5 | 9.8–24.8 | 101.5 | 25.4–406.1 |
| Volatile inhalants | 53.6 | 33.6–85.7 | 234.1 | 75.9–722.1 |
| Mephedrone | 190.4 | 26.2–1388.4 | _ | _ |
| Any drug c | 1.5 | 1.4–1.6 | 3.1 | 2.8–3.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerras, J.-M.; Hoyos, J.; García de Olalla, P.; de la Fuente, L.; Herrero, L.; Palma, D.; del Romero, J.; García-Pérez, J.-N.; Belza, M.-J.; The Methysos Project Group. Comparison of Polydrug Use Prevalences and Typologies between Men Who Have Sex with Men and General Population Men, in Madrid and Barcelona. Int. J. Environ. Res. Public Health 2021, 18, 11609. https://doi.org/10.3390/ijerph182111609
Guerras J-M, Hoyos J, García de Olalla P, de la Fuente L, Herrero L, Palma D, del Romero J, García-Pérez J-N, Belza M-J, The Methysos Project Group. Comparison of Polydrug Use Prevalences and Typologies between Men Who Have Sex with Men and General Population Men, in Madrid and Barcelona. International Journal of Environmental Research and Public Health. 2021; 18(21):11609. https://doi.org/10.3390/ijerph182111609
Chicago/Turabian StyleGuerras, Juan-Miguel, Juan Hoyos, Patricia García de Olalla, Luis de la Fuente, Lidia Herrero, David Palma, Jorge del Romero, Jorge-Néstor García-Pérez, María-José Belza, and The Methysos Project Group. 2021. "Comparison of Polydrug Use Prevalences and Typologies between Men Who Have Sex with Men and General Population Men, in Madrid and Barcelona" International Journal of Environmental Research and Public Health 18, no. 21: 11609. https://doi.org/10.3390/ijerph182111609
APA StyleGuerras, J.-M., Hoyos, J., García de Olalla, P., de la Fuente, L., Herrero, L., Palma, D., del Romero, J., García-Pérez, J.-N., Belza, M.-J., & The Methysos Project Group. (2021). Comparison of Polydrug Use Prevalences and Typologies between Men Who Have Sex with Men and General Population Men, in Madrid and Barcelona. International Journal of Environmental Research and Public Health, 18(21), 11609. https://doi.org/10.3390/ijerph182111609







