Health Related Values and Preferences Regarding Meat Intake: A Cross-Sectional Mixed-Methods Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Questionnaire and Study Procedures
2.4. Data Synthesis and Analysis
2.4.1. Quantitative Analysis
2.4.2. Qualitative Analysis
2.4.3. Integrating Qualitative and Quantitative Analyses
3. Results
3.1. Online Survey
3.1.1. Participants’ Characteristics
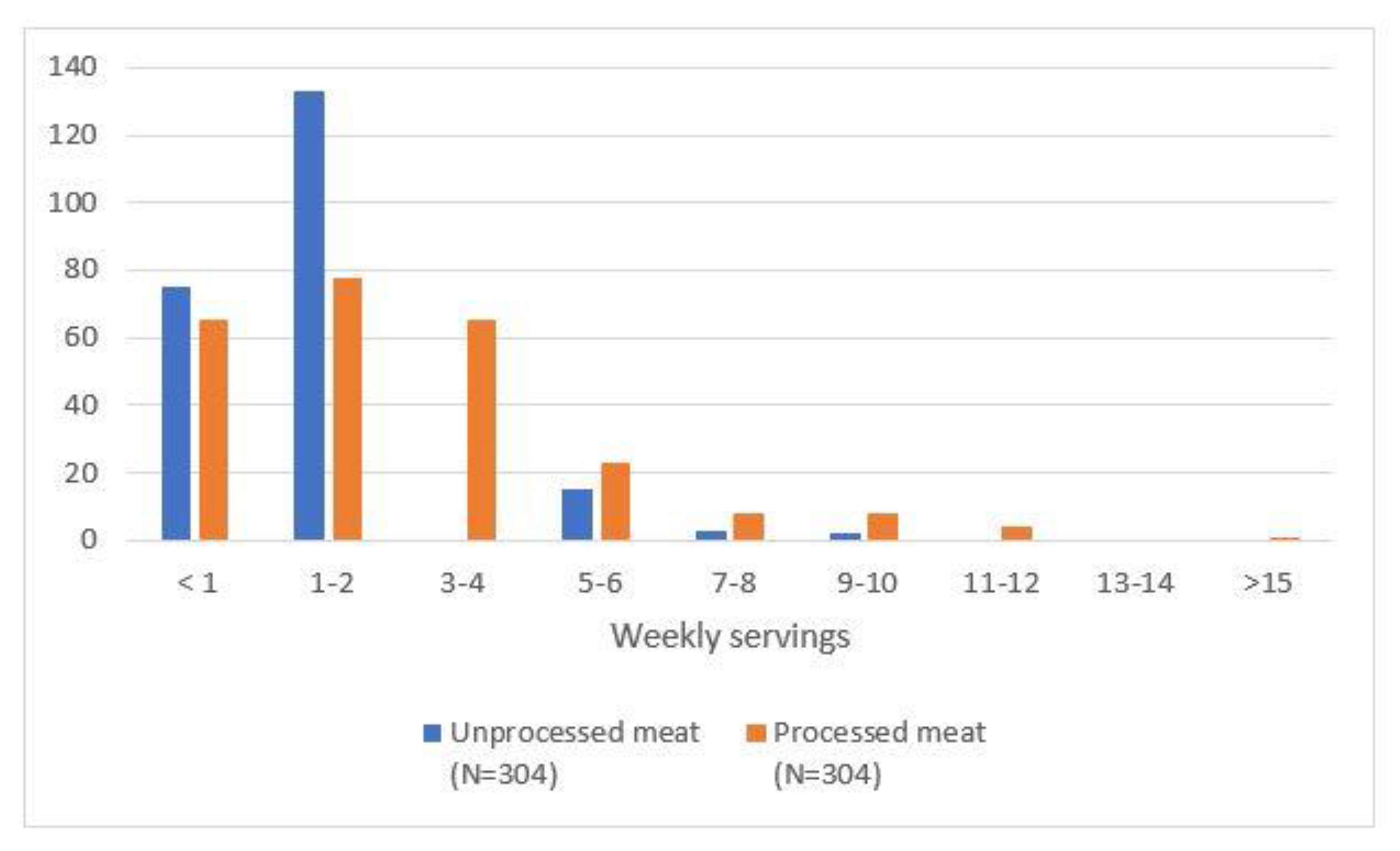
3.1.2. Participants’ Meat Consumption Behaviour
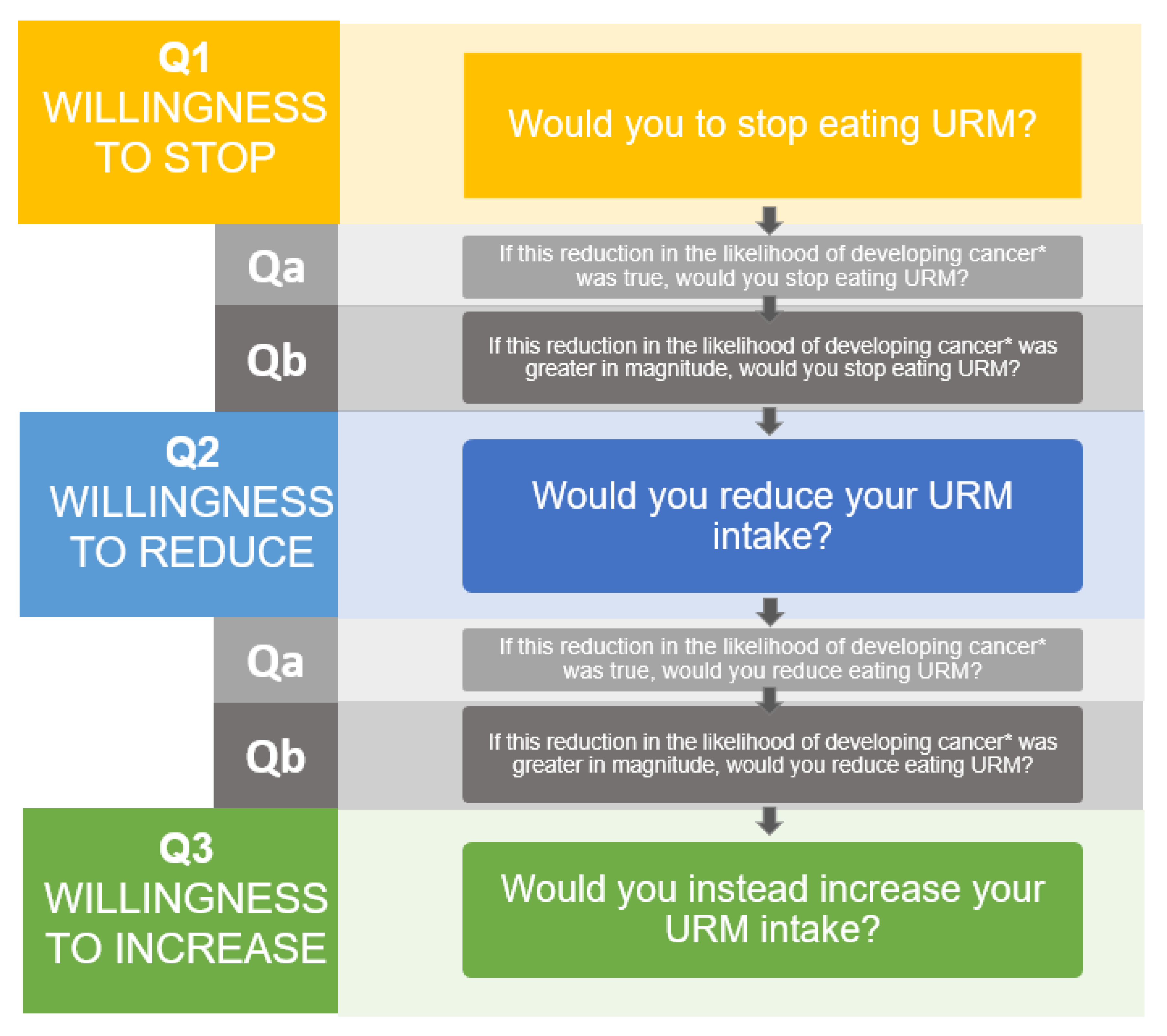
3.1.3. Willingness to Change Meat Consumption (Questions 1, 2 and 3)
3.1.4. Willingness to Change Meat Consumption with Higher Certainty (Questions a)
3.1.5. Willingness to Change Meat Consumption with a Larger Risk Reduction (Questions b)
3.1.6. Predictors of Willingness to Change Meat Consumption
3.2. Semi-Structured Interviews
3.2.1. Participants’ Characteristics
3.2.2. Participants’ Meat Consumption Behaviour
3.2.3. Meat Consumption Preferences
Social and/or Family Context Meat Consumption
Health- and Non-Health-Related Concerns about Meat
Uncertainty of the Evidence
3.3. Integrated Data
3.4. Follow-Up Assessment at 3 Months
4. Discussion
4.1. Main Findings
4.2. Our Results in the Context of Previous Research
4.3. Strengths and Limitations
4.4. Implications for Practice and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| IARC | International Agency for Research in Cancer |
| IQR | inter-quartile-range |
| SR | systematic review |
| URM | unprocessed red meat |
| PM | processed meat |
References
- Stok, F.M.; Hoffmann, S.; Volkert, D.; Boeing, H.; Ensenauer, R.; Stelmach-Mardas, M.; Kiesswetter, E.; Weber, A.; Rohm, H.; Lien, N.; et al. The DONE framework: Creation, evaluation, and updating of an interdisciplinary, dynamic framework 2.0 of determinants of nutrition and eating. PLoS ONE 2017, 12, e0171077. [Google Scholar] [CrossRef]
- Rabassa, M.; Ruiz, S.G.-R.; Solà, I.; Pardo-Hernandez, H.; Alonso-Coello, P.; García, L.M. Nutrition guidelines vary widely in methodological quality: An overview of reviews. J. Clin. Epidemiol. 2018, 104, 62–72. [Google Scholar] [CrossRef]
- Blake, P.; Durão, S.; E Naude, C.; Bero, L. An analysis of methods used to synthesize evidence and grade recommendations in food-based dietary guidelines. Nutr. Rev. 2018, 76, 290–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouvard, V.; Loomis, D.; Guyton, K.Z.; Grosse, Y.; El Ghissassi, F.; Benbrahim-Tallaa, L.; Guha, N.; Mattock, H.; Straif, K. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015, 16, 1599–1600. [Google Scholar] [CrossRef] [Green Version]
- Canada’s Food Guide. 2019. Available online: https://food-guide.canada.ca/en/ (accessed on 26 November 2020).
- US Department of Health and Human Services and US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed.; US Department of Health and Human Services and US Department of Agriculture: Washington, DC, USA, 2015.
- Public Health England: The Eat Well Guide. 2016. Available online: https://www.nhs.uk/live-well/eat-well/the-eatwell-guide/ (accessed on 26 November 2020).
- Valli, C.; Rabassa, M.; Johnston, B.C.; Kuijpers, R.; Prokop-Dorner, A.; Zajac, J.; Storman, D.; Storman, M.; Bala, M.M.; Solà, I.; et al. Health-Related Values and Preferences Regarding Meat Consumption: A Mixed-Methods Systematic Review. Ann. Intern. Med. 2019, 171, 742–755. [Google Scholar] [CrossRef] [PubMed]
- Han, M.A.; Zeraatkar, D.; Guyatt, G.H.; Vernooij, R.W.M.; Dib, R.E.; Zhang, Y.; Algarni, A.; Leung, G.; Storman, D.; Valli, C.; et al. Reduction of Red and Processed Meat Intake and Cancer Mortality and Incidence: A Systematic Review and Meta-analysis of Cohort Studies. Ann. Intern. Med. 2019, 171, 711–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiseman, M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Proc. Nutr. Soc. 2008, 67, 253–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valli, C.; Howatt, V.; Prokop-Dorner, A.; Rabassa, M.; Johnston, B.C.; Zajac, J.; Han, M.A.; Nampo, F.K.; Guyatt, G.H.; Bala, M.M.; et al. Evaluating adults’ health-related values and preferences about unprocessed red meat and processed meat consumption: Protocol for a cross-sectional mixed-methods study [version 2; peer review: 2 approved]. F1000Research 2021, 9, 346. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnston, B.C.; Alonso-Coello, P.; Bala, M.M.; Zeraatkar, D.; Rabassa, M.; Valli, C.; Marshall, C.; Dib, R.E.; Vernooij, R.W.M.; Vandvik, P.O.; et al. Methods for trustworthy nutritional recommendations NutriRECS (Nutritional Recommendations and accessible Evidence summaries Composed of Systematic reviews): A protocol. BMC Med. Res. Methodol. 2018, 18, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howatt, V.; Prokop-Dorner, A.; Valli, C.; Zajac, J.; Bala, M.M.; Alonso-Coello, P.; Guyatt, G.H.; Johnston, B.C. Values and Preferences Related to Cancer Risk among Red and Processed Meat Eaters: A Pilot Cross-Sectional Study with Semi-Structured Interviews. Foods 2021, 10, 2182. [Google Scholar] [CrossRef] [PubMed]
- R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013; Available online: https://www.R-project.org/ (accessed on 8 March 2021).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Cathain, A.; Murphy, E.; Nicholl, J. Three techniques for integrating data in mixed methods studies. Br. Med. J. 2010, 341, c4587. [Google Scholar] [CrossRef] [PubMed]
- Guetterman, T.C.; Fetters, M.D.; Creswell, J.W. Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Ann. Fam. Med. 2015, 13, 6554–6561. [Google Scholar] [CrossRef] [PubMed]
- Suarez, M.V.; Mañas, R.J.; Fernández, S.R.; de Robledo, D. Spanish National Dietary Survey in Adults, Elderly and Pregnant Women; EFSA Supporting Publications: Parma, Italy, 2016. [Google Scholar]
- Prokop-Dorner, A.; Piłat, A.; Zając, J.; Luśtyk, M.; Valli, C.; Łapczuk, A.; Brzyska, M.; Johnston, B.C.; Alonso-Coello, P.; Zera, D.; et al. Health-Related Values and Preferences Linked to Red and Processed Meat Consumption: An Advanced Online Survey and Semi-Structured Interviews. J. Public Health Nutr. 2021, 171, 742–755. [Google Scholar] [CrossRef]
- Cheah, I.; Shimul, A.S.; Liang, J.; Phau, I. Drivers and barriers toward reducing meat consumption. Appetite 2020, 149, 104636. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Sabate, R.; Sabaté, J. Consumer Attitudes Towards Environmental Concerns of Meat Consumption: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 1220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Overall (n = 304) | |
|---|---|
| Sex, n (%) | |
| Women | 189 (62.0) |
| Men | 115 (38.0) |
| Age, years | |
| Mean (SD) | 39.8 (10.7) |
| Median (Q1, Q3) | 38.0 (32.0, 46.0) |
| Education level, n (%) | |
| Primary education | 3 (1.0) |
| Secondary education | 14 (4.6) |
| Professional education | 24 (7.9) |
| University education | 259 (85.2) |
| No studies | 1 (0.3) |
| Employment status, n (%) | |
| Employed | 247 (81.2) |
| Unemployed | 34 (11.2) |
| Student | 20 (6.6) |
| Marital status, n (%) | |
| Married | 94 (30.9) |
| Common-law couple | 5 (1.6) |
| Living with my partner or family | 87 (28.6) |
| Separated | 2 (0.7) |
| Divorced | 12 (3.9) |
| Widow/widower | 1 (0.3) |
| Single | 100 (32.9) |
| Children, n (%) | |
| One child | 42 (13.8) |
| Two children | 62 (20.4) |
| Three or more children | 14 (4.6) |
| None | 183 (60.2) |
| Religion, n (%) | |
| Catholicism | 62 (20.4) |
| Other | 9 (3.0) |
| None | 230 (75.7) |
| Physical activity intensity ¥, n (%) | |
| Low | 82 (27.0) |
| Moderate | 139 (45.7) |
| High | 80 (26.3) |
| Weight, kg | |
| Mean (SD) | 69.9 (14.5) |
| Median(Q1, Q3) | 68.0(59.8, 79.0) |
| Height, m | |
| Mean (SD) | 1.70 (0.1) |
| Median (Q1, Q3) | 1.70 (1.6, 1.8) |
| BMI | |
| Mean (SD) | 24.3 (4.1) |
| Median (Q1, Q3) | 23.6 (21.5, 26.2) |
| Comorbidities, n (%) | |
| Hormonal system disorders | 14 (4.6) |
| Digestive diseases | 12 (3.9) |
| Musculoskeletal disorders | 8 (2.6) |
| Other | 41 (13.5) |
| None | 226 (74.3) |
| Family history of cancer, n (%) | |
| Yes | 198 (65.1) |
| No | 73 (24.0) |
| I don’t know | 30 (9.9) |
| Past reduction due to health reasons | |
|---|---|
| Unprocessed red meat | |
| N | 283 |
| No, n (%) | 200 (65.8) |
| Yes, n (%) | 83 (27.3) |
| Processed meat | |
| N | 283 |
| No, n (%) | 167 (54.9) |
| Yes, n (%) | 116 (38.2) |
| Past reduction due to other reasons | |
| Meat in general | |
| N | 282 |
| No, n (%) | 165 (54.3) |
| Yes, n (%) | 117 (38.5) |
| Other reasons, n (%) | |
| Animal welfare | 62 (20.4) |
| Environmental concerns | 67 (22.0) |
| Family preferences | 15 (4.9) |
| Social context | 7 (2.3) |
| Availability/accessibility | 5 (1.6) |
| Flavour | 21 (6.9) |
| Cost | 14 (4.6) |
| Other | 31 (10.2) |
| URM | PM | |
|---|---|---|
| Willingness to stop—Question 1 | ||
| Cancer Incidence | ||
| N | 126 | 163 |
| Willing, n (%) | 27 (21.4) | 36 (22.1) |
| Unwilling, n (%) | 99 (78.6) | 127 (77.9) |
| Median | 3.0 | 3.0 |
| Q1, Q3 | (1.0, 4.0) | (2.0, 4.0) |
| Cancer Mortality | ||
| N | 118 | 157 |
| Willing, n (%) | 29 (24.6) | 37 (23.6) |
| Unwilling, n (%) | 89 (75.4) | 120 (76.4) |
| Median | 3.0 | 3.0 |
| Q1, Q3 | (1.0, 4.0) | (2.0, 4.0) |
| Willingness to stop with higher certainty—Question a | ||
| Cancer Incidence | ||
| N | 94 | 120 |
| Willing, n (%) | 25 (26.6) | 43 (35.8) |
| Unwilling, n (%) | 69 (73.4) | 77 (64.2) |
| Median | 3.0 | 3.0 |
| Q1, Q3 | (2.0, 5.0) | (2.0, 5.0) |
| Cancer Mortality | ||
| N | 84 | 106 |
| Willing, n (%) | 16 (19.0) | 31 (29.2) |
| Unwilling, n (%) | 68 (81.0) | 75 (70.8) |
| Median | 3.0 | 3.0 |
| Q1, Q3 | (1.0, 4.0) | (2.0, 5.0) |
| Willingness to stop with a larger risk reduction—Question b | ||
| Cancer Incidence | ||
| N | 68 | 50 |
| Unwilling, n (%) | 21 (31.0) | 17 (34.0) |
| Willing, n (%) | 25 (37.0) | 19 (38.0) |
| Neither unwilling nor willing, n (%) | 22 (32.0) | 14 (28.0) |
| Cancer Mortality | ||
| N | 67 | 74 |
| Unwilling, n (%) | 21 (31.0) | 17 (23.0) |
| Willing, n (%) | 28 (42.0) | 41 (55.0) |
| Neither unwilling nor willing, n (%) | 18 (27.0) | 16 (22.0) |
| Willingness to reduce—Question 2 | ||
| Cancer Incidence | ||
| N | 37 | 47 |
| Willing, n (%) | 7 (18.9) | 4 (8.5) |
| Unwilling, n (%) | 30 (81.1) | 43 (91.5) |
| Median | 3.0 | 2.0 |
| Q1, Q3 | (1.0, 4.0) | (1.0, 3.0) |
| Cancer Mortality | ||
| N | 35 | 30 |
| Willing, n (%) | 5 (14.3) | 6 (20.0) |
| Unwilling, n (%) | 30 (85.7) | 24 (80.0) |
| Median | 3.0 | 3.0 |
| Q1, Q3 | (1.0, 4.0) | (2.0,4.0) |
| Willingness to reduce with higher certainty—Question a | ||
| Cancer Incidence | ||
| N | 30 | 39 |
| Willing, n (%) | 2 (6.7) | 4 (10.3) |
| Unwilling, n (%) | 28 (93.3) | 35 (89.7) |
| Median | 3.0 | 3.0 |
| Q1, Q3 | (1.0, 4.0) | (2.0, 4.0) |
| Cancer Mortality | ||
| N | 29 | 22 |
| Willing, n (%) | 2 (6.9) | 3 (13.6) |
| Unwilling, n (%) | 27 (93.1) | 19 (86.4) |
| Median | 2.0 | 3.0 |
| Q1, Q3 | (1.0, 4.0) | (1.3,4.0) |
| Willingness to reduce with a larger risk reduction—Question b | ||
| Cancer Incidence | ||
| N | 27 | 20 |
| Unwilling, n (%) | 12 (44.0) | 10 (50.0) |
| Willing, n (%) | 15 (56.0) | 10 (50.0) |
| Neither unwilling nor willing, n (%) | 0 (0) | 0 (0) |
| Cancer Mortality | ||
| N | 26 | 20 |
| Unwilling, n (%) | 12 (46.0) | 10 (50.0) |
| Willing, n (%) | 14 (54.0) | 10 (50.0) |
| Neither unwilling nor willing, n (%) | 0 (0) | 0 (0) |
| Willingness to increase—Question 3 | ||
| Cancer Incidence | ||
| N | 22 | 25 |
| Willing, n (%) | 0 | 0 (0.0) |
| Unwilling, n (%) | 22 (100.0) | 25 (100.0) |
| Median | 1.0 | 1.0 |
| Q1, Q3 | (1.0, 2.0) | (1.0, 2.0) |
| Cancer Mortality | ||
| N | 13 | 13 |
| Willing, n (%) | 0 (0.0) | 0 (0.0) |
| Unwilling, n (%) | 13 (100.0) | 13 (100.0) |
| Median | 1.0 | 1.0 |
| Q1, Q3 | (1.0, 1.0) | (1.0, 4.0) |
| Qualitative Data | Quantitative Data | Representative Quotes | Interpretation | |
|---|---|---|---|---|
| Semi-Structured Interview Themes | Online Survey Questions | Online Survey Results | ||
| Social and/or family context meat consumption | What are the most important factors that favour your consumption of red meat and processed meat? Select all that apply * | Social context was selected as a factor favouring unprocessed red meat and processed meat consumption by 52% and 40% of participants respectively. | “I consume meat especially social occasions” | Participants reported that social gatherings influenced their meat consumption. |
| Family preference was selected as a factor favouring unprocessed red meat and processed meat consumption by 50% and 33% of participants respectively. | “I have to adapt to the needs of my children and family” | Participants reported that family preference influenced their meat consumption. | ||
| Tradition was selected as a factor favouring unprocessed red meat and processed meat consumption by 57% and 33% of participants respectively. | “Even, for tradition, I consume game meat when I return to the family home” | Participants reported that tradition influenced their meat consumption | ||
| Health- and non-health-related concerns about meat | What are the most important factors that favour your consumption of unprocessed red meat? Select all that apply * | Health was selected by 41% of participants as a factor favouring unprocessed red meat consumption. | “I consider red meat necessary to have certain nutritional values such as iron or vitamin B12” | Participants highlighted the nutritional value of unprocessed red meat as a reason for consuming it. |
| In the past, have you cut back on red and/or processed meat for non-health reasons? | Environmental concerns were selected by 22% of participants.The second highest selected reason as a non-health-related reason for having reduced meat consumption in the past. | “Livestock farming is one of the human activities that generates the most CO2 emissions” | Non-health-related reasons such as environmental concerns play an important role in people’s meat consumption habits. | |
| Uncertainty of the evidence | What are the most important factors that favour your consumption of unprocessed red meat and processed meat? Select all that apply * | Taste was selected as a factor favouring unprocessed red meat and processed meat consumption by 79% and 49% of participants respectevely. The most selected factor. | “I like meat, and it is for sure a barrier to reduce or quit its consumption, especially when the evidence is unclear” | Taste was one of the most voted factors for consuming meat, and this could explain why in the face of uncertain evidence, participants were unwilling to stop and/or reduce their intake. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valli, C.; Santero, M.; Prokop-Dorner, A.; Howatt, V.; Johnston, B.C.; Zajac, J.; Han, M.-A.; Pereira, A.; Kenji Nampo, F.; Guyatt, G.H.; et al. Health Related Values and Preferences Regarding Meat Intake: A Cross-Sectional Mixed-Methods Study. Int. J. Environ. Res. Public Health 2021, 18, 11585. https://doi.org/10.3390/ijerph182111585
Valli C, Santero M, Prokop-Dorner A, Howatt V, Johnston BC, Zajac J, Han M-A, Pereira A, Kenji Nampo F, Guyatt GH, et al. Health Related Values and Preferences Regarding Meat Intake: A Cross-Sectional Mixed-Methods Study. International Journal of Environmental Research and Public Health. 2021; 18(21):11585. https://doi.org/10.3390/ijerph182111585
Chicago/Turabian StyleValli, Claudia, Marilina Santero, Anna Prokop-Dorner, Victoria Howatt, Bradley C. Johnston, Joanna Zajac, Mi-Ah Han, Ana Pereira, Fernando Kenji Nampo, Gordon H. Guyatt, and et al. 2021. "Health Related Values and Preferences Regarding Meat Intake: A Cross-Sectional Mixed-Methods Study" International Journal of Environmental Research and Public Health 18, no. 21: 11585. https://doi.org/10.3390/ijerph182111585
APA StyleValli, C., Santero, M., Prokop-Dorner, A., Howatt, V., Johnston, B. C., Zajac, J., Han, M.-A., Pereira, A., Kenji Nampo, F., Guyatt, G. H., Bala, M. M., Alonso-Coello, P., & Rabassa, M. (2021). Health Related Values and Preferences Regarding Meat Intake: A Cross-Sectional Mixed-Methods Study. International Journal of Environmental Research and Public Health, 18(21), 11585. https://doi.org/10.3390/ijerph182111585







