Effectiveness of Music-Based Intervention in Improving Uncomfortable Symptoms in ICU Patients: An Umbrella Review
Abstract
:1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Search Strategy
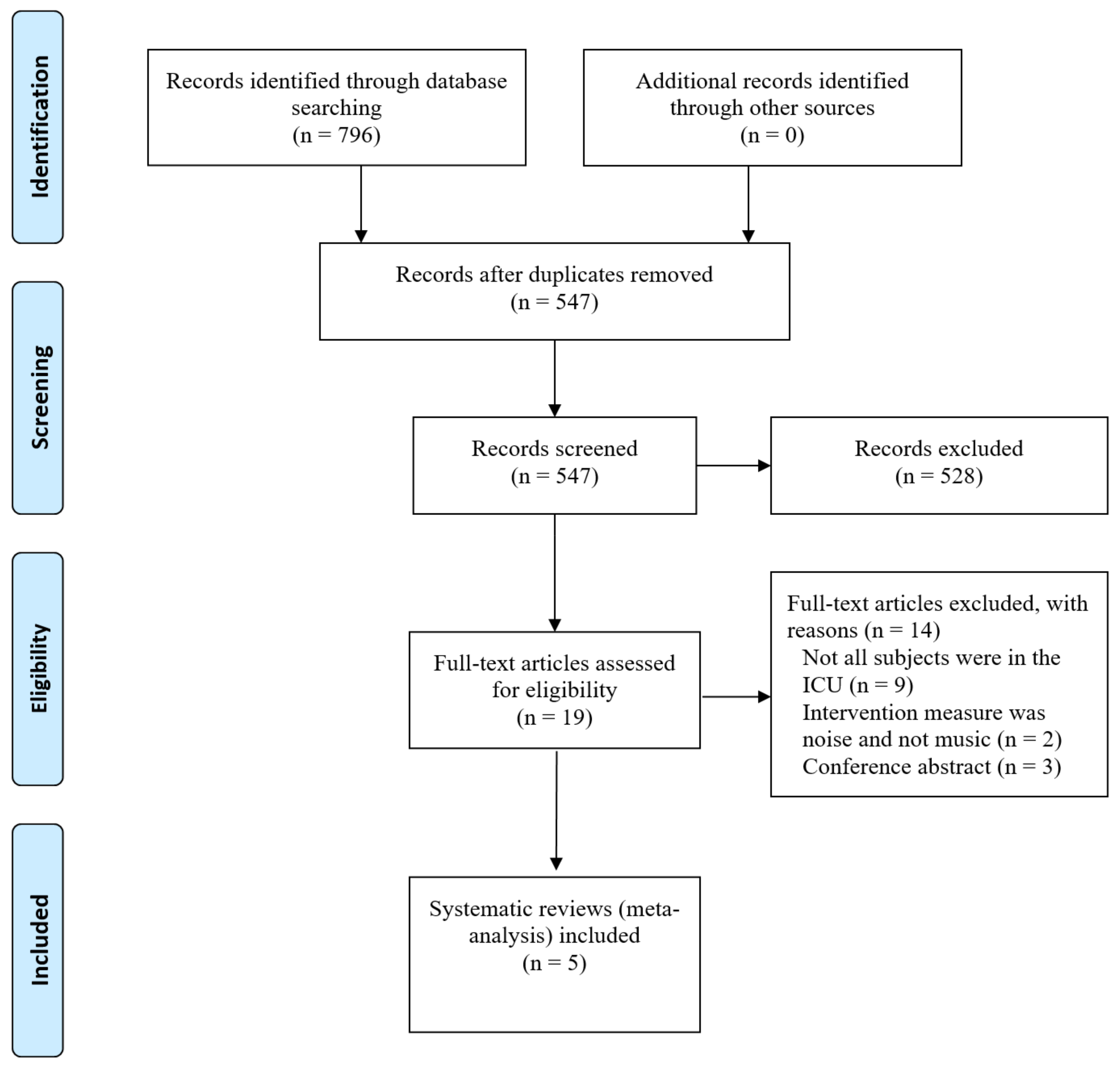
2.4. Study Selection
2.5. Data Extraction
2.6. Quality Appraisal
3. Results
3.1. Results of the Search Process
3.2. Description of Included SRs
3.3. Summary of Music-Based Interventions Characteristics
3.4. Critical Appraisal of Included SRs
4. Discussion
4.1. Music-Based Interventions
4.2. Symptoms
4.3. Agitation and Sedation
4.4. Methodology
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stretch, B.; Shepherd, S.J. Criteria for intensive care unit admission and severity of illness. Surgery 2021, 39, 22–28. [Google Scholar] [CrossRef]
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [CrossRef] [Green Version]
- Anastasia, A.G. Teaching Discomfort: Students’ and Teachers’ Descriptions of Discomfort in First-Year Writing Classes; University of Wisconsin Milwaukee: Milwaukee, WI, USA, 2015. [Google Scholar]
- Oxford Learner’s Dictionaries, Definition of Discomfort Noun from the Oxford Advanced Learner’s Dictionary. 2020. Available online: https://www.oxfordlearnersdictionaries.com/definition/english/discomfort_1?q=discomfort (accessed on 3 May 2021).
- Carrington, T.; Catasús, B. Auditing stories about discomfort: Becoming comfortable with comfort theory. Eur. Account. Rev. 2007, 16, 35–58. [Google Scholar] [CrossRef]
- Lenz, E.R.; Pugh, L.C.; Milligan, R.A.; Gift, A.; Suppe, F. The middle-range theory of unpleasant symptoms: An update. Adv. Nurs. Sci. 1997, 19, 14–27. [Google Scholar] [CrossRef]
- Rhodes, V.A.; Watson, P.M. Symptom distress—The concept: Past and present. Semin. Oncol. Nurs. 1987, 3, 242–247. [Google Scholar] [CrossRef]
- Sevin, C.M.; Bloom, S.L.; Jackson, J.C.; Wang, L.; Ely, E.W.; Stollings, J.L. Comprehensive care of ICU survivors: Development and implementation of an ICU recovery center. J. Crit. Care 2018, 46, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Beverly, A.; Kaye, A.D.; Ljungqvist, O.; Urman, R.D. Essential elements of multimodal analgesia in enhanced recovery after surgery (ERAS) guidelines. Anesthesiol. Clin. 2017, 35, e115–e143. [Google Scholar] [CrossRef]
- Thrane, S.E.; Hsieh, K.; Donahue, P.; Tan, A.; Exline, M.C.; Balas, M.C. Could complementary health approaches improve the symptom experience and outcomes of critically ill adults? A systematic review of randomized controlled trials. Complement. Ther. Med. 2019, 47, 102166. [Google Scholar] [CrossRef]
- American Music Therapy Association. What is Music Therapy? 2021. Available online: https://www.musictherapy.org/about/musictherapy (accessed on 19 February 2021).
- Stegemann, T.; Geretsegger, M.; Phan Quoc, E.; Riedl, H.; Smetana, M. Music therapy and other music-based interventions in pediatric health care: An overview. Medicines 2019, 6, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lunde, S.J.; Vuust, P.; Garza-Villarreal, E.A.; Vase, L. Music-induced analgesia: How does music relieve pain? Pain 2019, 160, 989–993. [Google Scholar] [CrossRef]
- Chlan, L.L. Music therapy as a nursing intervention for patients supported by mechanical ventilation. AACN Adv. Crit. Care 2000, 11, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Komann, M.; Weinmann, C.; Schwenkglenks, M.; Meissner, W. Non-pharmacological methods and post-operative pain relief: An observational study. Anesthesiol. Pain Med. 2019, 9, e84674. [Google Scholar] [CrossRef] [Green Version]
- Martin-Saavedra, J.S.; Vergara-Mendez, L.D.; Talero-Gutiérrez, C. Music is an effective intervention for the management of pain: An umbrella review. Complement. Ther. Clin. Pract. 2018, 32, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. JBI Evid. Implement. 2015, 13, 132–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joanna Briggs Institute. Critical Appraisal Checklist for Systematic Reviews and Research Syntheses. 2020. Available online: https://wikijbiglobal/display/MANUAL/Appendix+101+JBI+Critical+Appraisal+Checklist+for+Systematic+reviews+and+Research+Syntheses (accessed on 29 July 2021).
- Bradt, J.; Dileo, C. Music interventions for mechanically ventilated patients. Cochrane Database Syst. Rev. 2014, 2014, CD006902. [Google Scholar] [CrossRef] [PubMed]
- Gonzalo Garcia, G.; Almeida, L.; Zorzela, L.; King-Jones, S.; Joffe, A.R.; Hartling, L.; Jou, H.; Vohra, S. Efficacy of music on sedation, analgesia and delirium in critically ill patients. A systematic review of randomized controlled trials. J. Crit. Care 2019, 53, 75–80. [Google Scholar] [CrossRef]
- Meghani, N.; Tracy, M.F.; Hadidi, N.N.; Lindquist, R. Part I: The effects of music for the symptom management of anxiety, pain, and insomnia in critically ill patients: An integrative review of current literature. Dimens. Crit. Care Nurs. 2017, 36, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Richard-Lalonde, M.; Gélinas, C.; Boitor, M.; Gosselin, E.; Feeley, N.; Cossette, S.; Chlan, L.L. The Effect of Music on Pain in the Adult Intensive Care Unit: A Systematic Review of Randomized Controlled Trials. J. Pain Symptom Manag. 2020, 59, 1304. [Google Scholar] [CrossRef]
- Umbrello, M.; Sorrenti, T.; Mistraletti, G.; Formenti, P.; Chiumello, D.; Terzoni, S. Music therapy reduces stress and anxiety in critically ill patients: A systematic review of randomized clinical trials. Minerva Anestesiol. 2019, 85, 886–898. [Google Scholar] [CrossRef]
- Aghaie, B.; Rejeh, N.; Heravi-Karimooi, M.; Ebadi, A.; Moradian, S.T.; Vaismoradi, M.; Jasper, M. Effect of nature-based sound therapy on agitation and anxiety in coronary artery bypass graft patients during the weaning of mechanical ventilation: A randomised clinical trial. Int. J. Nurs. Stud. 2014, 51, 526–538. [Google Scholar] [CrossRef] [PubMed]
- Ames, N.; Shuford, R.; Yang, L.; Moriyama, B.; Frey, M.; Wilson, F.; Sundaramurthi, T.; Gori, D.; Mannes, A.; Ranucci, A. Music listening among postoperative patients in the intensive care unit: A randomized controlled trial with mixed-methods analysis. Integr. Med. Insights 2017, 12, 1178633717716455. [Google Scholar] [CrossRef]
- Beaulieu-Boire, G.; Bourque, S.; Chagnon, F.; Chouinard, L.; Gallo-Payet, N.; Lesur, O. Music and biological stress dampening in mechanically-ventilated patients at the intensive care unit ward-a prospective interventional randomized crossover trial. J. Crit. Care 2013, 28, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Blankfield, R.P.; Zyzanski, S.J.; Flocke, S.A.; Alemagno, S.; Scheurman, K. Taped therapeutic suggestions and taped music as adjuncts in the care of coronary-artery-bypass patients. Am. J. Clin. Hypn. 1995, 37, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Broscious, S.K. Music: An intervention for pain during chest tube removal after open heart surgery. Am. J. Crit. Care 1999, 8, 410–415. [Google Scholar] [CrossRef]
- Chan, M.F. Effects of music on patients undergoing a C-clamp procedure after percutaneous coronary interventions: A randomized controlled trial. Heart Lung J. Crit. Care 2007, 36, 431–439. [Google Scholar] [CrossRef]
- Chan, M.F.; Chung, Y.F.L.; Chung, S.W.A.; Lee, O.K.A. Investigating the physiological responses of patients listening to music in the intensive care unit. J. Clin. Nurs. 2009, 18, 1250–1257. [Google Scholar] [CrossRef]
- Chiasson, A.M.; Linda Baldwin, A.; Mclaughlin, C.; Cook, P.; Sethi, G. The effect of live spontaneous harp music on patients in the intensive care unit. Evid. Based Complement. Altern. Med. 2013, 2013, 428731. [Google Scholar] [CrossRef]
- Chlan, L. Psychophysiologic responses of mechanically ventilated patients to music: A pilot study. Am. J. Crit. Care 1995, 4, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Chlan, L.L. The Relationship of Absorption to the Effects of Music Therapy on Anxiety and Relaxation for Mechanically Ventilated Patients; University of Minnesota: Minneapolis, MN, USA, 1998. [Google Scholar]
- Chlan, L.L.; Engeland, W.C.; Anthony, A.; Guttormson, J. Influence of music on the stress response in patients receiving mechanical ventilatory support: A pilot study. Am. J. Crit. Care 2007, 16, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Chlan, L.L.; Weinert, C.R.; Heiderscheit, A.; Tracy, M.F.; Skaar, D.J.; Guttormson, J.L.; Savik, K. Effects of patient-directed music intervention on anxiety and sedative exposure in critically ill patients receiving mechanical ventilatory support: A randomized clinical trial. JAMA 2013, 309, 2335–2344. [Google Scholar] [CrossRef] [PubMed]
- Ciğerci, Y.; Özbayır, T. The effects of music therapy on anxiety, pain and the amount of analgesics following coronary artery surgery. Turk. J. Thorac. Cardiovasc. Surg. 2016, 24, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Conrad, C.; Niess, H.; Jauch, K.-W.; Bruns, C.J.; Hartl, W.; Welker, L. Overture for growth hormone: Requiem for interleukin-6? Crit. Care Med. 2007, 35, 2709–2713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooke, M.; Chaboyer, W.; Schluter, P.; Foster, M.; Harris, D.; Teakle, R. The effect of music on discomfort experienced by intensive care unit patients during turning: A randomized cross-over study. Int. J. Nurs. Pract. 2010, 16, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, B.M.; Gamel, C.; van der Bijl, J.J.; Bots, M.L.; Kesecioglu, J. The effects of music on physiological responses and sedation scores in sedated, mechanically ventilated patients. J. Clin. Nurs. 2010, 19, 1030–1039. [Google Scholar] [CrossRef]
- Guilbaut, V. Apport de l’intervention musicale standardisée type Music Care© sur les soins douloureux des patients vigiles en soins critiques (Impact of the standardized musical intervention Music Care© on the painful procedures of critically ill patients). In Médecine Humaine et Pathologie; Université Nice Sophia Antipolis: Nice, France, 2017; p. 52. [Google Scholar]
- Han, L.; Li, J.P.; Sit, J.W.; Chung, L.; Jiao, Z.Y.; Ma, W.G. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: A randomised controlled trial. J. Clin. Nurs. 2010, 19, 978–987. [Google Scholar] [CrossRef]
- Hunter, B.C.; Oliva, R.; Sahler, O.J.Z.; Gaisser, D.A.; Salipante, D.M.; Arezina, C.H. Music therapy as an adjunctive treatment in the management of stress for patients being weaned from mechanical ventilation. J. Music Ther. 2010, 47, 198–219. [Google Scholar] [CrossRef]
- Iblher, P.; Mahler, H.; Heinze, H.; Hüppe, M.; Klotz, K.; Eichler, W. Does music harm patients after cardiac surgery? A randomized, controlled study. Appl. Cardiopulm. Pathophysiol. 2011, 15, 14–23. [Google Scholar]
- Jaber, S.; Bahloul, H.; Guétin, S.; Chanques, G.; Sebbane, M.; Eledjam, J.J. Effects of music therapy in intensive care unit without sedation in weaning patients versus non-ventilated patients. Ann. Fr. D’anesthesie Reanim. 2007, 26, 30–38. [Google Scholar] [CrossRef]
- Jafari, H.; Zeydi, A.E.; Khani, S.; Esmaeili, R.; Soleimani, A. The effects of listening to preferred music on pain intensity after open heart surgery. Iran. J. Nurs. Midwifery Res. 2012, 17, 1–6. [Google Scholar]
- Korhan, E.A.; Khorshid, L.; Uyar, M. The effect of music therapy on physiological signs of anxiety in patients receiving mechanical ventilatory support. J. Clin. Nurs. 2011, 20, 1026–1034. [Google Scholar] [CrossRef]
- Kyavar, M.; Karkhaneh, S.; Rohanifar, R.; Azarfarin, R.; Sadeghpour, A.; Alizadehasl, A.; Ghadrdoost, B. Effect of preferred music listening on pain reduction in mechanically ventilated patients after coronary artery bypass graft surgery. Res. Cardiovasc. Med. 2016, 5, e33769. [Google Scholar] [CrossRef]
- Lee, C.-H.; Lee, C.-Y.; Hsu, M.-Y.; Lai, C.-L.; Sung, Y.-H.; Lin, C.-Y.; Lin, L.-Y. Effects of music intervention on state anxiety and physiological indices in patients undergoing mechanical ventilation in the intensive care unit: A randomized controlled trial. Biol. Res. Nurs. 2017, 19, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Lee, O.K.A.; Chung, Y.F.L.; Chan, M.F.; Chan, W.M. Music and its effect on the physiological responses and anxiety levels of patients receiving mechanical ventilation: A pilot study. J. Clin. Nurs. 2005, 14, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Mateu-Capell, M.; Arnau, A.; Juvinyà, D.; Montesinos, J.; Fernandez, R. Sound isolation and music on the comfort of mechanically ventilated critical patients. Nurs. Crit. Care 2019, 24, 290–298. [Google Scholar] [CrossRef]
- Naváis, M.S.; Clavero, G.V.; Guillamet, B.V.; Duran, A.M.; Estalella, G.M. Efecto de la música sobre la ansiedad y el dolor en pacientes con ventilación mecánica. Enferm. Intensiva 2013, 24, 63–71. [Google Scholar] [CrossRef] [Green Version]
- Özer, N.; Özlü, Z.K.; Arslan, S.; Günes, N. Effect of music on postoperative pain and physiologic parameters of patients after open heart surgery. Pain Manag. Nurs. 2013, 14, 20–28. [Google Scholar] [CrossRef]
- Phillips, S.D. Effect of Music Entrainment on Respiration of Patients on Mechanical Ventilation in the Intensive Care Unit; Florida State University: Tallahassee, FL, USA, 2007. [Google Scholar]
- Saadatmand, V.; Rejeh, N.; Heravi-Karimooi, M.; Tadrisi, S.D.; Vaismoradi, M.; Jordan, S. Effects of natural sounds on pain: A randomized controlled trial with patients receiving mechanical ventilation support. Pain Manag. Nurs. 2015, 16, 483–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saadatmand, V.; Rejeh, N.; Heravi-Karimooi, M.; Tadrisi, S.D.; Zayeri, F.; Vaismoradi, M.; Jasper, M. Effect of nature-based sounds’ intervention on agitation, anxiety, and stress in patients under mechanical ventilator support: A randomised controlled trial. Int. J. Nurs. Stud. 2013, 50, 895–904. [Google Scholar] [CrossRef]
- Shultis, C.L. Effects of Music Therapy vs. Music Medicine on Physiological and Psychological Parameters of Intensive Care Patients: A Randomized Controlled Trial; Temple University. Libraries: Philadelphia, PA, USA, 2012. [Google Scholar]
- Su, C.P.; Lai, H.L.; Chang, E.T.; Yiin, L.M.; Perng, S.J.; Chen, P.W. A randomized controlled trial of the effects of listening to non-commercial music on quality of nocturnal sleep and relaxation indices in patients in medical intensive care unit. J. Adv. Nurs. 2013, 69, 1377–1389. [Google Scholar] [CrossRef] [PubMed]
- To, W.T.; Bertolo, T.; Dinh, V.; Jichici, D.; Hamielec, C.M. Mozart piano sonatas as a nonpharmacological adjunct to facilitate sedation vacation in critically ill patients. Music. Med. 2013, 5, 119–127. [Google Scholar] [CrossRef]
- Voss, J.A.; Good, M.; Yates, B.; Baun, M.M.; Thompson, A.; Hertzog, M. Sedative music reduces anxiety and pain during chair rest after open-heart surgery. Pain 2004, 112, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.; Lopez-Nahas, V.; Molassiotis, A. Effects of music therapy on anxiety in ventilator-dependent patients. Heart Lung 2001, 30, 376–387. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.-J.; Chou, F.-H. The effectiveness of music therapy in reducing physiological and psychological anxiety in mechanically ventilated patients. Hu Li Za Zhi J. Nurs. 2008, 55, 35–44. [Google Scholar] [CrossRef]
- Yaghoubinia, F.; Navidian, A.; Nasir-al-din Tabatabaei, S.M.; Sheikh, S. Effect of music on pain intensity among patients with loss of consciousness in an intensive care unit. Med.-Surg. Nurs. J. 2016, 4, 40–47. [Google Scholar]
- Yaman Aktaş, Y.; Karabulut, N. The effects of music therapy in endotracheal suctioning of mechanically ventilated patients. Nurs. Crit. Care 2016, 21, 44–52. [Google Scholar] [CrossRef] [Green Version]
- Yarahmadi, S.; Mohammadi, N.; Ardalan, A.; Najafizadeh, H.; Gholami, M. The combined effects of cold therapy and music therapy on pain following chest tube removal among patients with cardiac bypass surgery. Complement. Ther. Clin. Pract. 2018, 31, 71–75. [Google Scholar] [CrossRef]
- Chlan, L.L.; Heiderscheit, A.; Skaar, D.J.; Neidecker, M.V. Economic Evaluation of a Patient-Directed Music Intervention for ICU Patients Receiving Mechanical Ventilatory Support. Crit. Care Med. 2018, 46, 1430–1435. [Google Scholar] [CrossRef]
- Mofredj, A.; Alaya, S.; Tassaioust, K.; Bahloul, H.; Mrabet, A. Music therapy, a review of the potential therapeutic benefits for the critically ill. J. Crit. Care 2016, 35, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.H.; Xu, C.; Purpura, R.; Durrani, S.; Lindroth, H.; Wang, S.; Gao, S.; Heiderscheit, A.; Chlan, L.; Boustani, M. Decreasing delirium through music: A randomized pilot trial. Am. J. Crit. Care 2020, 29, e31–e38. [Google Scholar] [CrossRef] [Green Version]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R. The Richmond Agitation–Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Rasheed, A.M.; Amirah, M.F.; Abdallah, M.; Parameaswari, P.; Issa, M.; Alharthy, A. Ramsay sedation scale and richmond agitation sedation scale: A Cross-sectional study. Dimens. Crit. Care Nurs. 2019, 38, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Kim, S.; Jeon, S.; Leary, E.B.; Barwick, F.; Mignot, E. Factors associated with fatigue in patients with insomnia. J. Psychiatr. Res. 2019, 117, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Wintermann, G.-B.; Weidner, K.; Strauss, B.; Rosendahl, J. Single assessment of delirium severity during postacute intensive care of chronically critically ill patients and its associated factors: Post hoc analysis of a prospective cohort study in Germany. BMJ Open 2020, 10, e035733. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.F.; Chen, Y.R.; Chung, M.H.; Liao, Y.M.; Chi, M.J.; Chang, C.C.; Chou, K.R. Effectiveness of music intervention in ameliorating cancer patients’ anxiety, depression, pain, and fatigue: A meta-analysis. Cancer Nurs. 2014, 37, E35–E50. [Google Scholar] [CrossRef]
- Chen, Y.-R.; Chang, C.Y.; Kuo, S.M. Active Noise Control and Secondary Path Modeling Algorithms for Earphones. In Proceedings of the 2017 American Control Conference (ACC), Seattle, WA, USA, 24–26 May 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 246–251. [Google Scholar] [CrossRef]
- Harris, W. How Noise-Canceling Headphones Work. How Stuff Works. 2008. Available online: https://electronics.howstuffworks.com/gadgets/audio-music/noise-canceling-headphone3.htm (accessed on 11 February 2021).
- Grander, W.; Müllauer, K.; Koller, B.; Tilg, H.; Dünser, M. Heart rate before ICU discharge: A simple and readily available predictor of short-and long-term mortality from critical illness. Clin. Res. Cardiol. 2013, 102, 599–606. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Physiological Parameters | Symptoms | ||||||
|---|---|---|---|---|---|---|---|---|
| SBP | DBP | HR | RR | SpO2 | Pain | Anxiety | Other | |
| Aghaie, 2014 [25] | FAS (+) | RASS (+) | ||||||
| Ames, 2017 [26] | NRS (+) | |||||||
| Beaulieu-B, 2013 [27] | − | − | − | Serum cortisol (+) | ||||
| Blankfield, 1995 [28] | Depression (−) | |||||||
| Broscious, 1999 [29] | NRS (−) | |||||||
| Chan, 2007 [30] | + | + | + | UCLA (+) | ||||
| Chan, 2009 [31] | + | + | + | + | ||||
| Chiasson, 2013 [32] | TVPS (−) | |||||||
| Chlan, 1995 [33] | − | + | + | + | − | Mood states (+) | ||
| Chlan, 1998 [34] | − | − | STAI (+) | |||||
| Chlan, 2007 [35] | + | Biomarkers § (−) | ||||||
| Chlan, 2013 [36] | VAS (+) | Urine cortisol (+) | ||||||
| Ciğerci, 2016 [37] | VAS (+) | STAI (−) | ||||||
| Conrad, 2007 [38] | − | Sedation level (+) | ||||||
| Cooke, 2010 [39] | NRS (−) | FAS (−) | Discomfort: NRS (−) | |||||
| Dijkstra, 2010 [40] | − | − | − | − | Sedation level (+) | |||
| Guilbaut, 2017 [41] | NRS (+) | |||||||
| Han, 2010 [42] | + | + | + | + | − | STAI (+) | ||
| Hunter, 2010 [43] | + | + | 98% less † | |||||
| Iblher, 2011 [44] | − | − | − | − | Delirium: CAM (−) | |||
| Jaber, 2007 [45] | − | − | − | − | NRS (+) | |||
| Jafari, 2012 [46] | NRS (+) | |||||||
| Korhan, 2011 [47] | + | + | − | + | − | |||
| Kyavar, 2016 [48] | CPOT (+) | |||||||
| Lee, 2017 [49] | + | − | + | STAI/VAS (+) | Serum cortisol (+) | |||
| Lee, 2005 [50] | − | − | + | + | STAI (−) | |||
| Mateu-C, 2019 [51] | BPS (−) | |||||||
| Sanjuan N, 2013 [52] | NRS (−) | STAI (+) | ||||||
| Özer, 2013 [53] | + | VPIS (+) | ||||||
| Phillips, 2007 [54] | − | − | − | |||||
| Saadatmand, 2015 [55] | VAS (+) | |||||||
| Saadatmand, 2013 [56] | + | + | FAS (+) | RASS (+) | ||||
| Shultis, 2012 [57] | VAS (−) | |||||||
| Su, 2013 [58] | + | + | Sleep quality (+) ‡ | |||||
| To, 2013 [59] | − | − | − | Ramsay scores (−) | ||||
| Voss, 2004 [60] | VAS (+) | |||||||
| Wong, 2001 [61] | − | STAI (+) | ||||||
| Wu, 2008 [62] | − | − | − | + | − | VAS (+) | ||
| Yaghoubinia, 2016 [63] | BPS (+) | |||||||
| Yaman A, 2016 [64] | CPOT (+) | |||||||
| Yarahmadi, 2018 [65] | VAS (−) | |||||||
| First Author/ Year/ Review Design | Objective | Included Studies (Range) | Number of Participants (Range) | Countries | Study Designs | Settings | Symptoms/ Phenomena of Interest | Positive Outcomes Related to Symptoms | Summary of Critical Appraisal |
|---|---|---|---|---|---|---|---|---|---|
| Bradt and Dileo, 2014 [20] Systematic review and meta-analysis | Effects of music therapy on anxiety and other outcomes in mechanically ventilated patients | 14 (1995–2013) | 912 (10–373) | 5 USA 3 China 1 Canada 1 Germany 1 France 1 Netherlands 1 Taiwan 1 Turkey | all RCTs | MV patients in ICU, LCAT, or “step-down” unit All participants were alert All adults | - anxiety - physiological parameters | ^ reduction anxiety ^ relaxation response (↓ RR and SBP) | Quality of the evidence (GRADE): low |
| Gonzalo Garcia et al., 2019 [21] Systematic review | Efficacy of music in providing sedation and analgesia and reducing the incidence of delirium in critically ill patients | 6 (1995–2017) | 734 (41–373) | 3 USA 2 Canada 1 Turkey | all RCTs | With or without MV patients in ICU All adults | - sedation and analgesia used - incidence of delirium | 1 ↓ sedation requirements | Quality of the evidence (GRADE): low |
| Meghani et al., 2017 [22] Integrative review | Effects of music on symptom management of anxiety, pain, and insomnia in critically ill patients | 9 (2010–2017) | 943 (17–373) | 2 Iran 2 Turkey 2 USA 1 Australia 1 China 1 Taiwan | 7 RCTs 1 Quasi 1 Feasibility study with historical controls | Critically ill patients in critical care settings 7 MV support 1 Open-heart 1 Medical ICU All adults | - pain - insomnia - anxiety | 1 ↑ sleep quality 3 ↓ anxiety 1 ↓ agitation levels 1 ↓ discomfort 2 ↓ HR and RR 1 ↓ SBP and DBP 1 ↓ RR, SBP, and DBP 1 ↓ HR, RR, BP, and anxiety | American Association of Colleges of Nursing’s evidence leveling hierarchy 6 of level B † 3 of level C ‡ |
| Richard-Lalonde et al., 2020 [23] Systematic review and meta-analysis | Effects of music interventions on pain in adult ICU patients | 18 (1999–2018) | 1173 (17–156) | 5 Iran 5 USA 2 France 2 Spain 2 Turkey 1 Australia 1 China | all RCTs | Patients in ICU All adults | - pain | ^ 20–30 min of music reducing pain | Risk of bias 2 high risk of random sequence 2 high risk of allocation concealment 18 high risk of performance 16 high risk of detection bias 2 high risk of attrition bias |
| Umbrello et al., 2019 [24] Systematic review | Effects of music therapy in reducing stress and anxiety in critically ill patients | 11 (1998–2017) | 959 (17–373) | 4 China 2 USA 2 Taiwan 1 Australia 1 Netherlands 1 Turkey | 10 RCTs 1 Quasi | Patients in ICU All adults | - stress - anxiety | 6 ↓ anxiety 2 ↓ HR and RR 2 ↓ HR, RR, SBP, and DBP 1 ↓ HR 1 ↓ RR and BP 1 ↓ HR, RR, and BP 1 ↑ level of sedation 1 ↓ RR, SBP, and DBP 1 ↑ sleep quality 1 ↓ sedative exposure | Assessment by using PEDro Scale 7: 8 in 11 2: 7 in 11 2: 6 in 11 |
| Author, Year | Music Type | Duration (Min) | Timing/ Setting | Session/Day | Music Selection | Delivery | Comparator | Conscious/Self-Report Ability | Symptoms |
|---|---|---|---|---|---|---|---|---|---|
| Aghaie, 2014 [25] | N-BS | 20 | Weaning MV | 1 | R | HP | NRH | Anxiety (+) Agitation level (+) | |
| Ames, 2017 [26] | MusiCure Dreams Album | 50 | Any time | 4–8 | R | HP | SC | Yes | Pain (+) Opioid use (−) |
| Beaulieu-Boire, 2013 [27] | Classical | 60 | Day | 2 | MT | HP | NRH | Sedation intensity (−) | |
| Blankfield, 1995 [28] | New Age Relaxing | 30 | Day | 2 | R | HP | SC | Opioid requirement (−) | |
| Broscious, 1999 [29] | Ten Categories of Cassettes | 10 | Procedure: CTR | 1 | P | Earphones | WNH, SC | Yes | Pain (−) |
| Chan, 2007 [30] | Three types | 45 | Procedure: C-Clamp | 1 | P | Earphones | SC | Yes | |
| Chan, 2009 [31] | Classical, Religious, and Jazz | 30 | 1 | HP | No control group | Alert | |||
| Chiasson, 2013 [32] | Harpist’s Choice | 10 | Rest | 1 | Music Player | Live Harp | SC | Yes | Pain (−) |
| Chlan, 1995 [33] | Helen Bonny | 30 | 1 | P | HP | NRH | |||
| Chlan, 1998 [34] | Classical, New Age, Country, Religious | 30 | 1 | P | HP | Quiet Rest | Alert | Anxiety (+) | |
| Chlan, 2007 [35] | Classical, New Age, Country | 60 | 1 | P | HP | Quiet Rest | |||
| Chlan, 2013 [36] | Self-initiated Preferred Music | 79.8 (mean) | Day and Night | Diversity | P | HP | NCH, SC | Alert | Anxiety (+) Sedative exposure (+) |
| Ciğerci, 2016 [37] | Folk or Classical | 30 | Rest | 2 | P | HP | SC | Yes | |
| Conrad, 2007 [38] | Mozart Piano Sonatas | 60 | 1 | R | HP | NRH | |||
| Cooke, 2010 [39] | Classical, Jazz, Country, Western, New Age, Easy Listening, “Other” | 15 | Procedure: Turning | 1 | P | Earphones | NRE | Yes | Pain (−), Anxiety (−), Discomfort (−) |
| Dijkstra, 2010 [40] | Classical and Easy Listening | 30 | 3 (2 days) | P | HP | Rest | Ramsay Score: 2–4 | Higher level of sedation (+) | |
| Guilbaut, 2017 [41] | Music Care Selection | 20 | Dressing, ETS, Turning | 1 | P | HP | NRH | Yes | Pain (+) |
| Han, 2010 [42] | Relaxation | 30 | 1 | P | HP | NRH, Rest | Alert | Anxiety (+) | |
| Hunter, 2010 [43] | Patient-Tailored Live Music | 45–60 | Weaning Trials | 3 times/week | Patient-tailored | Live Music | SC (historical controls) | ||
| Iblher, 2011 [44] | Classical, Baroque | 60 | Day | 1 | R | HP | SC | CAM (−) | |
| Jaber, 2007 [45] | U-Shaped Montage | 20 | Rest | 1 | P | HP | SC | Yes | |
| Jafari, 2012 [46] | A List Provided By A Music Expert | 30 | Rest | 1 | P | HP | NRH | Yes | Pain (+) |
| Korhan, 2011 [47] | Classical | 60 | 1 | R | HP | SC | GCS ≥ 9 | ||
| Kyavar, 2016 [48] | 30 | Dressing Change | 1 | P | HP | NRH | |||
| Lee, 2017 [49] | Classical, Natural Sounds | 30 | 4–4.30 pm | 1 | P | HP | NRH | Yes | Anxiety (+) |
| Lee, 2005 [50] | Classical, Religious, Natural Sounds | 30 | 1 | P | HP | NRH | Alert | Anxiety (−) | |
| Mateu-Capell, 2019 [51] | Reikid Merlin’s Magic | 60 | Rest | 1 | MT | HP | NCH | ||
| SanjuanNaváis, 2013 [52] | Researchers’ Selection | 30 | Rest | 3–5 Minimum/8 h | P | Earphones | SC | Yes | |
| Özer, 2013 [53] | Patients’ Selection | 30 | POD 1 | 1 | P | Earphones | Rest | Pain (+) | |
| Phillips, 2007 [54] | Live Music | 25 | 1 | P | Live Music | Quiet Rest | |||
| Saadatmand, 2015 [55] | CDs | 30–90 | Rest | 1 | P | HP | NRH | Yes | Pain (+) |
| Saadatmand, 2013 [56] | N-BS | 30–90 | 1 | HP | NRH | Anxiety (+) Agitation level (+) | |||
| Shultis, 2012 [57] | Researcher-Compiled CDs | 22 (mean) | Rest | 1 | P | CD Player | SC | Yes | Pain (−) |
| Su, 2013 [58] | Noncommercial Music | 45 | Nocturnal Sleep Time | 1 | R | HP | SC | Clear | Sleep quality (+) |
| To, 2013 [59] | Classical | 240 | Day | 1 | R | HP | NRH | Success of sedation vacation (−) | |
| Voss, 2004 [60] | Six Types | 30 | Procedure: Chair Rest | 1 | P | HP | SC | Yes | Pain (+) |
| Wong, 2001 [61] | Various Chinese and Western music | 30 | 1 | P | HP | Rest | Alert | Anxiety (+) | |
| Wu, 2008 [62] | Classical, Orchestral, Religious, New Age, Hymn | 30 | 1 | P | HP | SC | Anxiety (+) | ||
| Yaghoubinia, 2016 [63] | Beach Walk by Arnd Stein | 30 | Rest | 1 (total 3 days) | R | HP | SC | ||
| YamanAktaş, 2016 [64] | Reed Flute | 20 pre- and 20 post-ETS | Procedure: ETS | 1 | R | Music Pillow | SC | Yes | |
| Yarahmadi, 2018 [65] | 15 Pieces | 15 pre- and 15 post-CTR | Procedure: CTR | 1 | P | HP | SC | Yes | Pain (−) |
| Citation/Questions | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bradt and Dileo, 2014 [20] |  |  |  |  |  |  |  |  |  |  |  |
| Gonzalo Garcia et al., 2019 [21] |  |  |  |  |  |  |  |  |  |  |  |
| Richard-Lalonde et al., 2020 [22] |  |  |  |  |  |  |  |  |  |  |  |
| Umbrello et al., 2019 [23] |  |  |  |  |  |  |  |  |  |  |  |
| Meghani et al., 2017 [24] |  |  |  |  |  |  |  |  |  |  |  |
 ; NA = Not applicable
; NA = Not applicable  ; U = Unclear
; U = Unclear  ; Y = Yes
; Y = Yes  . Source: Joanna Briggs Institute (2020) [19]. Items by each criterion (question number): Q1: Was the review question clearly and explicitly stated?; Q2: Were the inclusion criteria appropriate for the review question?; Q3: Was the search strategy appropriate?; Q4: Were the sources and resources used to search for studies adequate?; Q5: Were the criteria for appraising studies appropriate?; Q6: Was the critical appraisal independently conducted by two or more reviewers?; Q7: Were there methods to minimize errors in data extraction?; Q8: Were the methods used to combine studies appropriate?; Q9: Was the likelihood of publication bias assessed?; Q10: Were recommendations for policy and/or practice supported by the reported data?; Q11: Were the specific directives for new research appropriate?
. Source: Joanna Briggs Institute (2020) [19]. Items by each criterion (question number): Q1: Was the review question clearly and explicitly stated?; Q2: Were the inclusion criteria appropriate for the review question?; Q3: Was the search strategy appropriate?; Q4: Were the sources and resources used to search for studies adequate?; Q5: Were the criteria for appraising studies appropriate?; Q6: Was the critical appraisal independently conducted by two or more reviewers?; Q7: Were there methods to minimize errors in data extraction?; Q8: Were the methods used to combine studies appropriate?; Q9: Was the likelihood of publication bias assessed?; Q10: Were recommendations for policy and/or practice supported by the reported data?; Q11: Were the specific directives for new research appropriate?Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-F.; Chang, M.-Y.; Chow, L.-H.; Ma, W.-F. Effectiveness of Music-Based Intervention in Improving Uncomfortable Symptoms in ICU Patients: An Umbrella Review. Int. J. Environ. Res. Public Health 2021, 18, 11500. https://doi.org/10.3390/ijerph182111500
Chen Y-F, Chang M-Y, Chow L-H, Ma W-F. Effectiveness of Music-Based Intervention in Improving Uncomfortable Symptoms in ICU Patients: An Umbrella Review. International Journal of Environmental Research and Public Health. 2021; 18(21):11500. https://doi.org/10.3390/ijerph182111500
Chicago/Turabian StyleChen, Yu-Fen, Mei-Yu Chang, Lok-Hi Chow, and Wei-Fen Ma. 2021. "Effectiveness of Music-Based Intervention in Improving Uncomfortable Symptoms in ICU Patients: An Umbrella Review" International Journal of Environmental Research and Public Health 18, no. 21: 11500. https://doi.org/10.3390/ijerph182111500
APA StyleChen, Y.-F., Chang, M.-Y., Chow, L.-H., & Ma, W.-F. (2021). Effectiveness of Music-Based Intervention in Improving Uncomfortable Symptoms in ICU Patients: An Umbrella Review. International Journal of Environmental Research and Public Health, 18(21), 11500. https://doi.org/10.3390/ijerph182111500






