Effect of Case-Based Small-Group Learning on Care Workers’ Emergency Coping Abilities
Abstract
1. Introduction
1.1. Background
1.2. Purpose
1.3. Research Hypotheses
- (1)
- The level of knowledge and performance in emergencies will be higher in the experimental group (EG; i.e., care workers who underwent the emergency coping education program) than the control group (CG).
- (2)
- Emergency coping abilities will be higher in the EG than in the CG.
- (3)
- Self-efficacy in coping with emergencies will be higher in the EG than in the CG.
- (4)
- Confidence in communication will be higher in the EG than in the CG.
2. Method
2.1. Study Design
2.2. Study Participants
2.3. Measurement Tools
2.3.1. Level of Knowledge and Performance in Emergencies in Long-Term Care Facilities
2.3.2. Emergency Coping Ability
2.3.3. Self-Efficacy in Coping with Emergencies
2.3.4. Confidence in Communication
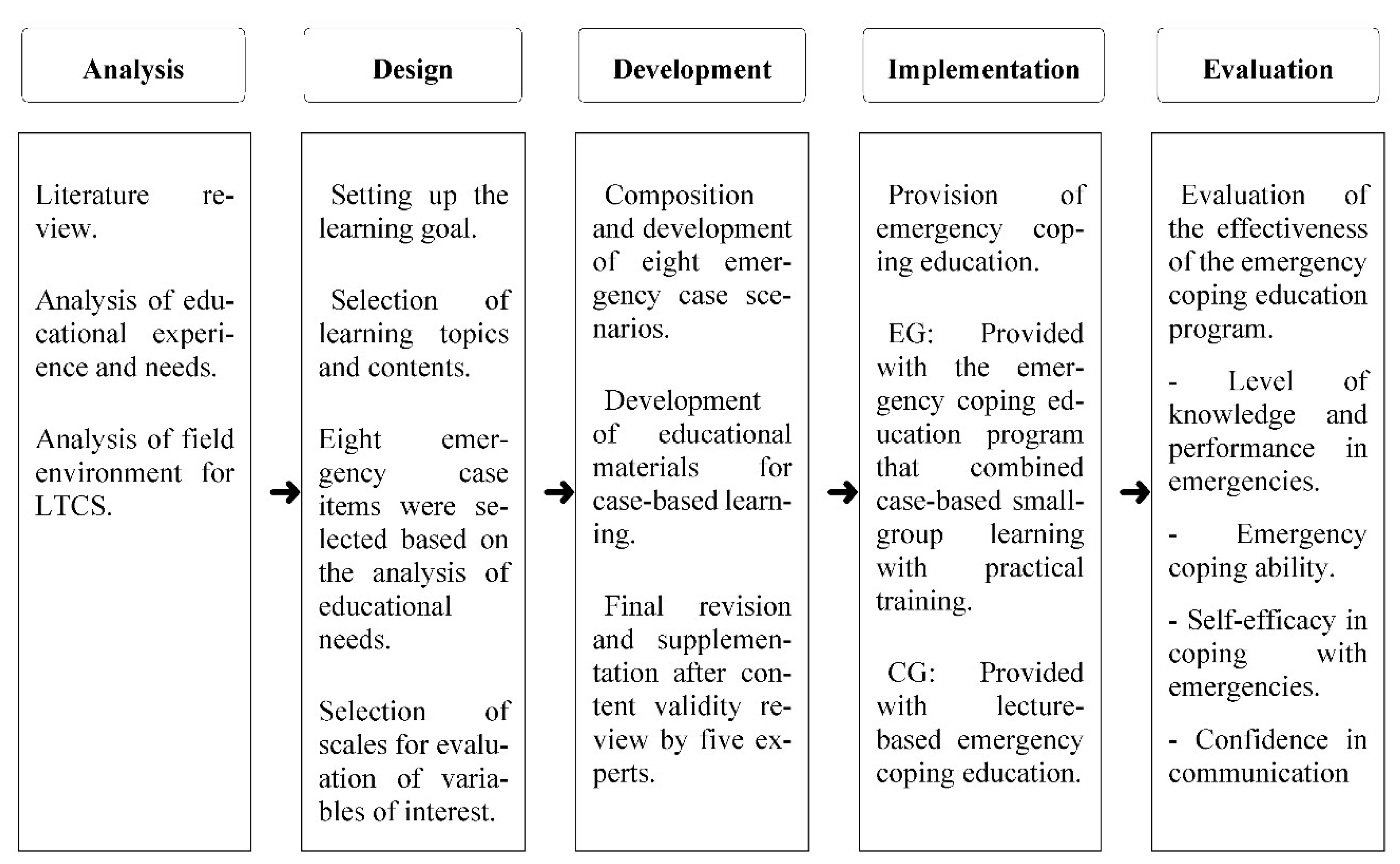
2.4. Research Process
2.4.1. Analysis
2.4.2. Design
2.4.3. Development
2.5. Implementation
2.5.1. Emergency Coping Education Incorporating Case-Based Small-Group Learning
2.5.2. Lecture-Based Education
2.6. Evaluation
2.7. Data Collection
2.8. Data Analysis
- For the general characteristics of the EG and CG, percentages, means, and standard deviations were calculated.
- An independent t-test was performed for preliminary homogeneity analysis on the dependent variables of the two groups.
- The differences in the dependent variables between the two groups before and after the educational program were analyzed by an independent t-test.
2.9. Ethical Considerations
3. Results
3.1. Participants’ General Characteristics and Homogeneity Testing of the Two Groups
3.2. Verification of the Difference in the Dependent Variable after Intervention
3.2.1. Hypothesis 1
3.2.2. Hypothesis 2
3.2.3. Hypothesis 3
3.2.4. Hypothesis 4
3.3. Difference between Levels of Knowledge and Performance in Emergencies at Posttest
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization. Ageing. 2018. Available online: https://www.who.int/news-room/facts-in-pitures/detail/ageing (accessed on 19 May 2020).
- Understanding Nursing Insurance Scheme Policies. Available online: http://www.mohw.go.kr/react/policy/index.jsp?PAR_MENU_ID=06&MENU_ID=06390301&PAGE=1&topTitle=%EC%A0%95%EC%B1%85%EC%9D%98%20%EC%9D%B4%ED%95%B4 (accessed on 19 May 2020).
- Ministry of Health and Welfare. Long Term Care Insurance Statistical Yearbook; Ministry of Health and Welfare: Sejong, Korea, 2019.
- Korea Institute for Health and Social Affairs. Survey of the Actual State of the Elderly; Korea Institute for Health and Social Affairs: Sejong, Korea, 2018. [Google Scholar]
- Kojima, G. Prevalence of frailty in nursing homes: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2015, 16, 940–945. [Google Scholar] [CrossRef]
- Jørgensen, L.B.; Thorleifsson, B.M.; Selbaek, G.; Saltyte Benth, J.; Helvik, A.S. Physical diagnoses in nursing home residents—Is dementia or severity of dementia of importance? BMC Geriatr. 2018, 18, 254. [Google Scholar] [CrossRef]
- Lemoyne, S.E.; Herbots, H.H.; De Blick, D.; Remmen, R.; Monsieurs, K.G.; Van Bogaert, P. Appropriateness of transferring nursing home residents to emergency departments: A systematic review. BMC Geriatr. 2019, 19, 17. [Google Scholar] [CrossRef] [PubMed]
- Laging, B.; Kenny, A.; Bauer, M.; Nay, R. Recognition and assessment of resident’ deterioration in the nursing home setting: A critical ethnography. J. Clin. Nurs. 2018, 27, 1452–1463. [Google Scholar] [CrossRef]
- O’Neill, B.; Parkinson, L.; Dwyer, T.; Reid-Searl, K. Nursing home nurses’ perceptions of emergency transfers from nursing homes to hospital: A review of qualitative studies using systematic methods. Geriatr. Nurs. 2015, 36, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Overview of the Long-term Care Insurance System for the Elderly. Available online: http://m.nhis.or.kr/comWeb/wo/e/wcea00.html (accessed on 19 May 2020).
- Lee, M.S. A Study on the Method of Dealing with Patients and Patient Transfer Process at the Elderly Care Facility before Going to Emergency Department. Master’s Thesis, Korea National Open University, Seoul, Korea, 2015. [Google Scholar]
- Kim, S.Y.; Kim, S.O. Patient safety awareness and emergency response ability perceived by nursing homes and home visiting caregivers. J. Korean Acad. Soc. Nurs. Educ. 2018, 24, 347–357. [Google Scholar] [CrossRef]
- Kim, S.O. Comparison of emergency experience and first aid knowledge, emergency coping ability, educational experience and educational needs of facilities and home caregivers. J. Korean Public Health Nurs. 2019, 33, 390–408. [Google Scholar] [CrossRef]
- Kim, S.O.; Kim, S.Y. Experience of emergency situation and experience of education, first aid knowledge and educational needs of caregivers. J. Korean Public Health Nurs. 2018, 32, 288–303. [Google Scholar] [CrossRef]
- Lim, H.-J. The relation between the problem solving ability and satisfaction on clinical practice of dental hygiene students. J. Korean Soc. Sch. Commun. Health Educ. 2017, 18, 97–105. [Google Scholar]
- Lim, H.Y.; Lee, M.J. The effect of managerial leadership on the care burden of care workers: Focus on the leadership of top-leader and leadership of mid-level leaders. J. Korea Contents Acad. Assoc. 2017, 17, 308–318. [Google Scholar] [CrossRef]
- Tannazzo, T.; Breuer, L.; Williams, S.; Andreoli, N.A. A dementia training program to benefit certified nurse assistant satisfaction and nursing home resident outcomes. Alzheimer’s Care Today 2008, 9, 221–229. [Google Scholar] [CrossRef]
- Lee, J.K.; Jang, S.N. Comparative study of formal education systems for long-term care workers in six countries. J. Long Term Care 2018, 6, 6–30. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.Y. A study on care workers’ job performance and competency at long-term care homes. Health Soc. Welf. Rev. 2013, 33, 243–273. [Google Scholar] [CrossRef]
- Cho, Y.R.; Lee, K.Y. Current prehospital care status, knowledge, and prehospital care confidence toward the elderly among 119 emergency medical technicians. Korean J. Emerg. Med. Serv. 2014, 18, 19–35. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. 2019 Nursing Care Professional Training Standard Textbook: Types and Contents of Nursing Care Services; Ministry of Health and Welfare: Sejong, Korea, 2018; pp. 514–533.
- Dugan, E.; Roberts, C.P.; Cohen, S.J.; Preisser, J.S.; Davis, C.C.; Bland, D.R.; Albertson, E. Why older community-dwelling adults do not discuss urinary incontinence with their primary care physicians. J. Am. Geriatr. Soc. 2001, 49, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.G.; Park, M.S. Effects of the elderly care education program for caregivers in geriatric hospital: Cased-based small group learning. J. Korean Gerontol. Soc. 2020, 40, 855–869. [Google Scholar] [CrossRef]
- Michaelsen, L.K.; Parmelee, D.X.; McMahon, K.K.; Levine, R.E. (Eds.) Team-Based Learning for Health Professions Education: A Guide to Using Small Groups for Improving Learning; Stylus Publishing LLC: Sterling, VA, USA, 2007. [Google Scholar]
- Zhang, L.; Zhang, T.; Sun, Y. A newly designed intensive caregiver education program reduces cognitive impairment, anxiety, and depression in patients with acute ischemic stroke. Braz. J. Med. Biol. Res. 2019, 52, e8533. [Google Scholar] [CrossRef]
- Griffiths, P.C.; Kovaleva, M.; Higgins, M.; Langston, A.H.; Hepburn, K. Tele-savvy: An online program for dementia caregivers. Am. J. Alzheimers Dis. Other Demen. 2018, 33, 269–276. [Google Scholar] [CrossRef]
- Hong, H.H.; Gu, M.O. Development and effects of a coping skill training program for caregivers in feeding difficulty of older adults with dementia in long-term care facilities. J. Korean Acad. Nurs. 2018, 48, 167–181. [Google Scholar] [CrossRef]
- Lee, K.Y.; Lim, S.R. Effect of professional oral healthcare program on the oral status of elderly residents in long-term care facilities. J. Dent. Hyg. Sci. 2016, 16, 432–441. [Google Scholar] [CrossRef][Green Version]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analysis using G*Power3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.-K.; Jeon, Y.-Y.; Kim, J.-H. Analysis of early childhood teachers’ perception of coping methods for dealing with emergency situations and the gap between knowledge and practice levels. J. Korea Open Assoc. Early Child. Edu. 2018, 23, 221–245. [Google Scholar] [CrossRef]
- Hwang, K.H.; Lee, O.C. Factors affecting safety awareness and emergency response capability among employees of public facilities. Crisisonomy 2017, 13, 1–12. [Google Scholar] [CrossRef]
- Jung, J.S.; Hur, H.K. Effectiveness and retention of repeated simulation-based basic life support training for nursing students. J. Korean Crit. Care Nurs. 2013, 6, 24–36. [Google Scholar]
- Lee, O.C. Effects of safety education on the Public Safety Consciousness Index (PSCI) and self-efficacy of the emergency response in university students. Crisis Emerg. Manag. 2014, 10, 1–18. [Google Scholar] [CrossRef]
- Kim, E.J. The Effect of Simulation-based SBAR Training Program on Nursing Students Communication and Clinical Judgement. Ph.D. Dissertation, Chonnam National University, Gwangju, Korea, 2018. [Google Scholar]
- Byeon, D.H. Effect of fire safety education based on the theory of planned behavior on the fire safety behavior of care worker trainees. Fire Sci. Eng. 2019, 33, 147–155. [Google Scholar] [CrossRef]
- Dilou, Y.T. Effectiveness of an educational intervention about the level of knowledge of informal caregivers of elderlies. Rev. Cuba. Enfermería 2020, 36, 1–15. [Google Scholar]
- Aluisio, A.R.; Daniel, P.; Grock, A.; Freedman, J.; Singh, A.; Papanagnou, D.; Arquilla, B. Case-based learning outperformed simulation exercises in disaster preparedness education among nursing trainees in India: A randomized controlled trial. Prehosp. Disaster Med. 2016, 31, 516–523. [Google Scholar] [CrossRef]
- Hammad, K.S.; Arbon, P.; Gebbie, K.M. Emergency nurses and disaster response: An exploration of South Australian emergency nurses’ knowledge and perception of their roles in disaster response. Australas. Emerg. Nurs. J. 2011, 14, 87–94. [Google Scholar] [CrossRef]
- Jeong, M.-E.; Park, H.-S. Effects of case-based learning on clinical decision making and nursing performance in undergraduate nursing students. J. Korean Acad. Fundam. Nurs. 2015, 22, 308–317. [Google Scholar] [CrossRef][Green Version]
- Park, M.-S. Effects of a Cultural Competence Promoting Program for Multicultural Maternity Nursing Care: Case-based Small Group Learning. Ph.D. Dissertation, Chosun University, Gwangju, Korea, 2013. [Google Scholar]
- Starr, S.; Wallace, D.C. Self–reported cultural competence of public health nurses in a southeastern U.S. public health department. Public Health Nurs. 2009, 26, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.-J. Effects of case-based small group learning on daycare center teachers’ coping ability in emergency situations: Focus on daily life and cardiopulmonary resuscitation. Child. Health Nurs. Res. 2013, 19, 168–176. [Google Scholar] [CrossRef]
- Hamasu, S.; Morimoto, T.; Kuramoto, N.; Horiguchi, M.; Iwami, T.; Nishiyama, C.; Takada, K.; Kubota, Y.; Seki, S.; Maeda, Y.; et al. Effects of BLS training on factors associated with attitude toward CPR in college students. Resuscitation 2009, 80, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Prickett, K.; Deshpande, A.; Paschal, H.; Simon, D.; Hebber, K.B. Simulation-based education to improve emergency management skills in caregivers of tracheostomy patients. Int. J. Pediatr. Otorhinolaryngol. 2019, 120, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.Y.; Kang, K.A. The influence of case-based learning using video in emergency care of infants and toddlers. J. Korea Acad. Ind. Coop. Soc. 2016, 17, 292–300. [Google Scholar] [CrossRef]
- Stark, R.; Kopp, V.; Fischer, M.R. Case-based learning with worked examples in complex domains: Two experimental studies in undergraduate medical education. Learn. Instr. 2011, 21, 22–33. [Google Scholar] [CrossRef]
- Stocker, M.; Burmester, M.; Allen, M. Optimisation of simulated team training through the application of learning theories: A debate for a conceptual framework. BMC Med. Edu. 2014, 14, 69. [Google Scholar] [CrossRef]
- Creutzfeldt, J.; Hedman, L.; Heinrichs, L.; Youngblood, P.; Felländer-Tsai, L. Cardiopulmonary resuscitation training in high school using avatars in virtual worlds: An international feasibility study. J. Med. Internet Res. 2013, 15, e9. [Google Scholar] [CrossRef]
- Dykes, P.C.; Carroll, D.; McColgan, K.; Hurley, A.C.; Lipsitz, S.R.; Colombo, L.; Zuyev, L.; Middleton, B. Scales for assessing self-efficacy of nurses and assistants for preventing falls. J. Adv. Nurs. 2011, 67, 438–449. [Google Scholar] [CrossRef] [PubMed]
- Park, O.K. Effectiveness of Case-Centered Education Program based on Nursing Protocol for Pressure Injury Stages. Ph.D. Dissertation, Korea University, Seoul, Korea, 2018. [Google Scholar]
- Choi, Y.-R. Development and Evaluation of an Emergency Management Education Program Based on a Shared Mental Model for Practitioners in Nursing Homes. Ph.D. Dissertation, Korea University, Seoul, Korea, 2020. [Google Scholar]
- Park, S.-J.; Choi, H.-S. The effect of case-based SBAR communication training program on critical thinking disposition, communication self-efficacy and communication competence of nursing students. J. Korea Acad. Ind. Coop. Soc. 2018, 19, 426–434. [Google Scholar] [CrossRef]
- Shrader, S.; Dunn, B.; Blake, E.; Phillips, C. Incorporating standardized colleague simulations in a clinical assessment course and evaluating the impact on interprofessional communication. Am. J. Pharm. Educ. 2015, 79, 57. [Google Scholar] [CrossRef] [PubMed]
- De Meester, K.; Verspuy, M.; Monsieurs, K.G.; Van Bogaert, P. SBAR improves nurse-physician communication and reduces unexpected death: A pre and post intervention study. Resuscitation 2013, 84, 1192–1196. [Google Scholar] [CrossRef]
- Renz, S.M.; Boltz, M.P.; Wagner, L.M.; Capezuti, E.A.; Lawrence, T.E. Examining the feasibility and utility of an SBAR protocol in long-term care. Geriatr. Nurs. 2013, 34, 295–301. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Solet, D.J.; Norvell, J.M.; Rutan, G.H.; Frankel, R.M. Lost in translation: Challenges and opportunities in physician-to-physician communication during patient handovers. Acad. Med. 2015, 80, 1094–1099. [Google Scholar] [CrossRef] [PubMed]
- Riesenberg, L.A.; Leitzsch, J.; Cunningham, J.M. Nursing handoffs: A systematic review of the literature. Am. J. Nurs. 2010, 110, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Liang, Z.; Blazeck, A.; Greene, B. Improving Chinese nursing students’ communication skills by utilizing video-stimulated recall and role-play case scenarios to introduce them to the SBAR technique. Nurse Educ. Today 2015, 35, 881–887. [Google Scholar] [CrossRef]
- Baldwin, T.T.; Ford, J.K. Transfer of training: A review and directions for future research. Personnel Psychol. 1998, 41, 63–105. [Google Scholar] [CrossRef]
| Modules | Learning Objectives | Lesson Contents | Time (min) | Pedagogy Strategy |
|---|---|---|---|---|
| (Introduction) Case-based education for improving emergency coping ability in care workers |
|
| 60 |
|
| (Module 1) Older adults whose heart stopped beating |
|
| 50 |
|
| 40 |
| ||
| (Module 2) Older adults with a rice cake stuck in the throat |
|
| 50 |
|
| 40 |
| ||
| (Module 3) Older adults showing signs of reduced brain function |
|
| 50 |
|
| 40 |
| ||
| (Module 4) Older adults falling unconscious |
|
| 50 |
|
| 40 |
| ||
| (Module 5) Older adults suffering from shortness of breath |
|
| 50 |
|
| 40 |
| ||
| (Module 6) Older adults having a severe convulsion (seizure) |
|
| 50 |
|
| 40 |
| ||
| (Module 7) Older adults feeling dizzy owing to low blood sugar |
|
| 50 |
|
| 40 |
| ||
| (Module 8) Older adults falling in the living room and being unable to move |
|
| 50 |
|
| 40 |
|
| Variables | Categories | Experimental Group (n = 36) n (%) or M ± SD | Control Group (n = 36) n (%) or M ± SD | χ2/t | p |
|---|---|---|---|---|---|
| Age (yr) | Average age | 60.47 ± 4.48 | 59.78 ± 4.85 | 0.631 | 0.530 |
| Education | Middle school or less | 7 (19.4) | 9 (25.0) | 0.444 | 0.910 |
| High school | 27 (75.0) | 24 (66.7) | |||
| College or above | 2 (5.6) | 3 (8.3) | |||
| Work experience | Less than 1 year | 1 (2.8) | 4 (11.1) | 3.050 | 0.569 |
| 1 to less than 3 years | 7 (19.4) | 5 (13.9) | |||
| 3 to less than 5 years | 7 (19.4) | 8 (22.2) | |||
| 5 to less than 10 years | 8 (22.2) | 10 (27.8) | |||
| Over 10 years | 13 (36.1) | 9 (25.0) | |||
| Working time | Everyday 9 to 6 | 7 (11.1) | 8 (22.2) | 0.508 | 0.776 |
| Three shifts | 11 (38.9) | 8 (22.2) | |||
| Part-time | 18 (50.0) | 20 (55.6) | |||
| Work place | OACF | 18 (50.0) | 16 (44.4) | 0.223 | 0.637 |
| HCC | 18 (50.0) | 20 (55.6) | |||
| Outcome variables | |||||
| Emergency situation | Knowledge level | 51.56 ± 10.57 | 48.33 ± 3.58 | 1.733 | 0.090 |
| Practice level | 48.50 ± 5.42 | 46.75 ± 3.77 | 1.590 | 0.116 | |
| Emergency coping ability | Basic life support | 21.42 ± 3.51 | 20.33 ± 3.66 | 1.281 | 0.204 |
| General first aid | 33.64 ± 5.87 | 31.44 ± 3.26 | 1.961 | 0.054 | |
| Total | 55.06 ± 8.86 | 51.78 ± 5.52 | 1.884 | 0.064 | |
| Self-efficacy in coping with emergencies | 50.17 ± 10.56 | 48.06 ± 3.64 | 1.134 | 0.263 | |
| Confidence in communication | 19.39 ± 5.63 | 17.06 ± 5.70 | 1.747 | 0.085 | |
| Variables | Groups | Pretest | Posttest | Difference | t | p | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |||||
| Emergency situation | Knowledge level | EG (n = 36) | 51.56 ± 10.57 | 72.75 ± 4.81 | 21.19 ± 13.08 | 4.379 | <0.001 * |
| CG (n = 36) | 42.78 ± 4.99 | 67.08 ± 6.10 | 18.75 ± 6.52 | ||||
| Performance level | EG (n = 36) | 48.50 ± 5.42 | 73.33 ± 3.62 | 24.83 ± 6.71 | 4.954 | <0.001 * | |
| CG (n = 36) | 39.81 ± 5.06 | 66.56 ± 7.37 | 19.81 ± 7.07 | ||||
| Emergency coping ability | Basic life support | EG (n = 36) | 21.42 ± 3.51 | 34.08 ± 3.23 | 12.67 ± 4.34 | 2.855 | 0.006 * |
| CG (n = 36) | 17.56 ± 1.50 | 31.50 ± 4.37 | 11.17 ± 6.75 | ||||
| General first aid | EG (n = 36) | 33.64 ± 5.87 | 51.72 ± 4.08 | 18.08 ± 6.39 | 3.592 | 0.001 * | |
| CG (n = 36) | 26.42 ± 3.40 | 47.08 ± 6.59 | 15.63 ± 8.87 | ||||
| Total | EG (n = 36) | 55.06 ± 8.86 | 85.81 ± 6.76 | 30.75 ± 12.72 | 3.508 | 0.001 * | |
| CG (n = 36) | 43.97 ± 4.41 | 78.58 ± 10.34 | 26.80 ± 14.43 | ||||
| Self-efficacy in coping with emergencies | EG (n = 36) | 50.17 ± 10.56 | 85.53 ± 12.71 | 35.36 ± 17.21 | 4.295 | <0.001 * | |
| CG (n = 36) | 43.72 ± 10.82 | 69.42 ± 18.58 | 21.36 ± 17.17 | ||||
| Confidence in communication | EG (n = 36) | 19.39 ± 5.63 | 33.81 ± 5.82 | 14.42 ± 7.73 | 3.085 | 0.003 | |
| CG (n = 36) | 17.06 ± 5.70 | 29.08 ± 7.11 | 12.01 ± 9.34 | ||||
| Variables | Groups | Knowledge Level | Performance Level | Means Difference | t | p | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | ||||||
| Differences between levels of knowledge and performance | Total | EG (n = 36) | 3.64 ± 0.24 | 3.67 ± 0.18 | 0.03 | −0.627 | 0.535 |
| CG (n = 36) | 3.35 ± 0.30 | 3.33 ± 0.37 | 0.02 | 0.461 | 0.648 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-O. Effect of Case-Based Small-Group Learning on Care Workers’ Emergency Coping Abilities. Int. J. Environ. Res. Public Health 2021, 18, 11458. https://doi.org/10.3390/ijerph182111458
Kim S-O. Effect of Case-Based Small-Group Learning on Care Workers’ Emergency Coping Abilities. International Journal of Environmental Research and Public Health. 2021; 18(21):11458. https://doi.org/10.3390/ijerph182111458
Chicago/Turabian StyleKim, Soon-Ok. 2021. "Effect of Case-Based Small-Group Learning on Care Workers’ Emergency Coping Abilities" International Journal of Environmental Research and Public Health 18, no. 21: 11458. https://doi.org/10.3390/ijerph182111458
APA StyleKim, S.-O. (2021). Effect of Case-Based Small-Group Learning on Care Workers’ Emergency Coping Abilities. International Journal of Environmental Research and Public Health, 18(21), 11458. https://doi.org/10.3390/ijerph182111458





