Abstract
(1) Background: Numerous educational interventions have been conducted to improve hand hygiene (HH) compliance and effectiveness among nursing students, with mixed results. The aim is to evaluate the effectiveness of posters as a teaching tool and factors associated with HH quality. (2) Methods: A pre-post experimental intervention study was conducted with a total of 293 nursing students randomly assigned to two groups (experimental and control) who, before and after HH, took cell culture samples from their non-dominant hands. Only the experimental group was exposed to the poster. (3) Results: In the experimental group, significant differences were observed among students older than 22 years (p = 0.017; V = 0.188), with a higher percentage of failures (15.7% vs. 3.6%). Poster displaying was associated with passing, other variables being equal, although without statistical significance (ORa = 2.07; 95% CI = 0.81–5.26). Pre-practice hand contamination was weakly associated with lower HH quality (ORa = 0.99, 95% CI = 0.99–0.99). (4) Conclusions: The use of posters as a teaching method shows indications of efficacy. Prior hand contamination slightly affects the quality of HH. Further evaluation of teaching methods is needed to ensure good technical performance of HH to prevent the spread of infectious diseases during the COVID-19 pandemic.
1. Introduction
The effectiveness and utility of hand hygiene (HH) for infection prevention in healthcare is undisputed, and this is all the more true during the COVID-19 pandemic [1,2,3,4,5] While nurses generally tend to comply with HH recommendations [6], this form of hygiene is not always performed correctly [7,8,9,10].
Numerous interventions have been proposed to maintain adherence over time, with inconclusive results [11,12]. A number of interventions have been based on performance feedback or on placing alcohol-based hand rub (ABHR) at key points of care [11,13]. However, there is insufficient evidence to make specific recommendations on the content and implementation of such interventions [13].
Nursing students can act as potential vectors of infectious diseases during their clinical placements [7,8], which is why theory and practical training in HH is provided from the very beginning of their academic studies [7,14,15]. Overall, nursing students’ attitudes towards HH are favourable [7,10,16,17], but conventional teaching methods do not seem to provide a proper understanding of HH [7,18,19]. Additionally, Løyland et al. (2020) [20] confirmed that the adhesion to HH in the medical personnel, including nursing students, had a negative balance, which affected to the prevention of nosocomial infections and even prevented the reduction of the instructions of the antibiotic treatment in patients. In studies such as the one developed by Sundal et al. [19], the degree of general compliance in HH in nursing students was estimated to be 83.5% during their clinical internship. In these studies, the five moments of the HH of the WHO were evaluated: firstly, before touching the patient; secondly, before the cleaning/washing procedure; thirdly, after exposure to body fluids; fourthly, after touching the patient; and finally, after touching a patient in the environment [19,20]. Elola-Vicente et al. [21] evaluated the effectiveness of the HH technique in medical personnel. It would be advisable to consider it in the nursing students. A large body of research stresses the need to improve the training of future healthcare workers [8,10,18,22]. In addition to knowledge, other factors such as students’ sex, age, academic year, work experience, beliefs, perceived barriers, and attitudes influence the adoption of effective HH behaviours [7,8,23,24,25].
Innovative, multidisciplinary interventions have been proposed in the search for effective learning methods, with mixed results [7,9,14,15,18,26,27,28].
Posters have traditionally been used in health and social care as a resource to promote HH, albeit with poor results [29,30]. However, the WHO recommends the use of posters as reminders in the workplace and as tools for training healthcare workers [31]. To the best of our knowledge, there are no studies to date assessing the effectiveness of posters as a teaching method for improving the HH technique among nursing students.
This study has two aims: firstly, to evaluate the effectiveness of the poster as a tool for improving the quality of HH among nursing students; secondly, to determine the factors associated with correct HH among nursing students.
2. Materials and Methods
2.1. Study Design and Participants
An experimental pre–post intervention study was carried out at a public university in southern Spain during the 2019–2020 academic year. The nursing degree in Spain is divided into four years and students receive basic HH training in the first year, with clinical placements starting in the third year.
All undergraduate nursing students who had passed their basic HH training during the second, third, and fourth years and who voluntarily agreed to participate were invited to do so.
For a population of 321 students, the necessary sample size was estimated to be 140 participants, with a power of 95%, a 5% level of accuracy, and an expected proportion of 80%. Students were allocated to the intervention and control groups using random sampling stratified per academic year. To ensure that the practices ran smoothly, students were divided into groups of 20. The last group of fourth-year students, who were assigned to the control group, were not able to participate in the study due to the suspension of face-to-face tuition caused by the COVID-19 pandemic. However, the participation rate for that academic year was 74%. This study was performed according to the STROBE statement, Strengthening the Reporting of Observational studies in Epidemiology.
2.2. Description of the Intervention and Data Collection
The intervention consisted of two practice sessions per group led by the research team and an accredited laboratory technician. The first session lasted one hour and included a brief reminder of nosocomial infections, with special emphasis on the role of nursing professionals as the main vectors of transmission. The differences between the different HH techniques were defined, recalling the five moments recommended by the WHO, as well as the importance of keeping nails short, clean, and without nail polish or gel. Each student received two sterile swabs and a Petri dish with a previously identified agar culture. They then divided the plate into two equal parts to differentiate pre- and post-HH seeding and proceeded to sample and culture the non-dominant hand in the pre-HH part. Škodová et al. [25] confirmed that the most contaminated areas after HH are the thumbs and interdigital areas of the non-dominant hand. The decision was made to sample only that hand, in line with Cruz and Bashtawi [32], Elola-Vicente et al. [21], Silva et al. [33], and Škodová et al. [25].
The hands were then cleaned with ABHR. Sanitisers with alcohol concentrations above 60% have been shown to have similar efficacy to hand washing with soap and water. They were used because of their current availability in healthcare facilities [11,13]. All students were administered the same amount of ABHR with an alcohol concentration of 75% and performed the handwashing technique. The intervention group did so with the WHO poster displayed [34] and the control group did so without it. Finally, they performed a second sampling and seeding of the same hand in the post-HH zone. At the end of the process, the plates were placed in a culture oven at 35 °C for 48 h. HH and the Petri dish seeding process were supervised at all times by two members of the research team and an accredited laboratory technician.
This was followed by the second session, which lasted 15 min. Each student checked their plate and manually counted the colony forming units (CFU) under the supervision of their instructors. The results were recorded on a data sheet, which included socio-demographic and academic data.
Figure 1 shows the group selection process. Figure 2 depicts the procedure for collecting and evaluating the results of the practice.
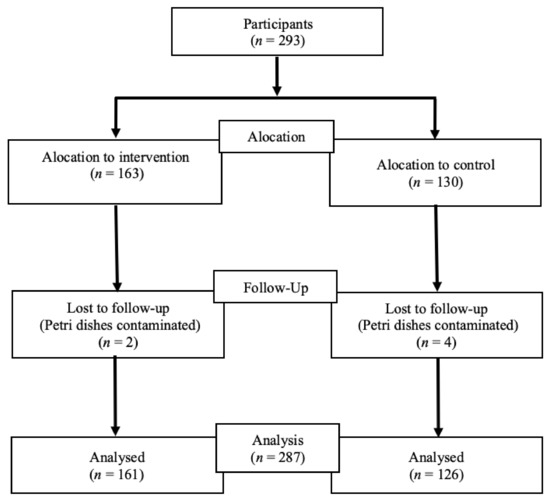
Figure 1.
The group selection process.
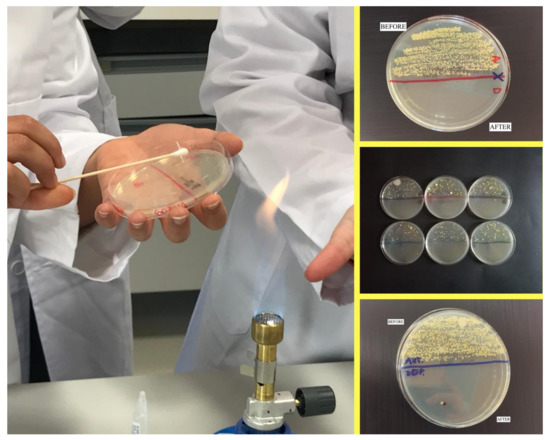
Figure 2.
Description of the intervention and data collection.
The variables to be considered were: group (intervention and control), age (continuous and dichotomised: ≤22 and >22), sex (male, female), academic year (second, third, fourth), conducting a clinical placement (yes, no), and pre- and post-HH contamination assessed using the number of CFU/cm2.
2.3. Data Analysis
HH effectiveness was assessed by classifying students as either pass or fail. The classification was conducted according to the recommendations of the Chinese Centre for Disease Control and Prevention, i.e., by counting the number of CFU/cm2. Aerobic bacterial counts are required to be under 10 CFU/cm2 among healthcare workers in general clinical units [35,36].
Descriptive statistics were applied using frequency and dispersion measures according to the nature of each variable. The Chi-square test was used to assess differences in age, gender, academic year, and year of study between the control and experimental groups. Pre- and post-intervention differences between and within groups were calculated using Spearman’s chi-square. The effect size was assessed using Cramér’s V and Cohen’s d statistic. Explanatory bivariate and multivariate logistic regression models were designed to adjust for all study variables, calculating crude and adjusted odds ratios, respectively, and their 95% CIs.
Every analysis has been conducted using the Statistical Package for the Social Sciences (SPSS) program, version 25, (IBM, New York, NY, USA, for Mac).
2.4. Ethical Considerations
This study was approved by the university centre and the Granada Research Ethics Committee (code number: 0100-N-21). Participants signed an informed consent form for data collection purposes in compliance with the European Directive 2001/20/EC and Spanish Law 14/2007 of 3 July on Biomedical Research.
3. Results
3.1. Characteristics of the Participants
After the CFU count, six plates (two belonging to the intervention group and four to the control group) were found to be contaminated and were therefore excluded. As a result, the final number of participants was 287. Their sociodemographic and academic characteristics are shown in Table 1.

Table 1.
Characteristics of the participants.
3.2. Outcome of the Intervention
Table 2 shows the numbers and percentages of students in each group who were classified as either pass or fail before and after the intervention. A significant improvement was observed.

Table 2.
Intervention data (HH).
No differences in results were identified between the experimental group and the control group before and after performing HH with ABHR (Table 3).

Table 3.
Intervention data (HH). Independent sample results.
Table 4 shows the distribution of sociodemographic and academic variables by study group after the workshops. In the experimental group, significant differences were observed by age (p = 0.017; V = 0.188), with students aged over 22 showing a higher percentage of fails (15.7%). A moderate association was found between pre-HH hand contamination and HH outcomes between the two groups (p = 0.005; d = 0.418), meaning that students who passed obtained a lower mean number of CFUs compared to those who failed.

Table 4.
Post-HH data: comparisons based on sociodemographic and academic variables.
The results of the bivariate and multivariate logistic regression are shown in Table 5. The use of posters as a teaching method for improving HH shows indications of effectiveness when adjusting for the other variables, although these are not statistically significant (OR = 2.07; 95% CI = 0.810–5.264). The number of CFUs prior to hand rubbing was slightly associated with the degree of cleanliness of the hands after the workshop (OR = 0.99; 95% CI = 0.991–0.999).

Table 5.
Logistic regression for students who passed (post-HH).
4. Discussion
This study explored the potential association between the use of a poster as a teaching tool and the quality of HH among nursing students in response to the need to find an effective method to improve the HH technique to control nosocomial infections among this group [25,32,37,38].
Our findings are in line with the results of numerous studies showing that the use of ABHR considerably reduces the microbial burden and is thus considered a suitable procedure for nosocomial infection control [25,27,32,39,40,41].
We observed no sex-based differences in the level of HH after using the poster as a teaching tool. Nonetheless, the available evidence on the influence of this variable based on various interventions remains controversial. Anderson et al. [42] and Pérez-Pérez et al. [38] point out that, regardless of the techniques used, women performed HH better than men in all cases. In contrast, Cruz and Bashtawi [32] report that being male and being in the first years of university study were predictive of greater knowledge of the technique. Recently, Merino-Plaza et al. [43] studied adherence to HH among healthcare professionals. Initially, men scored more poorly than women on adherence to HH. However, when targeted improvements in care services based on monitoring and feedback were implemented, men’s scores improved to match those of women. These strategies, which were also included in our training practices, may be behaving in a similar way in our study.
In the intervention group, we identified a relationship between age and the number of CFUs, whereby students aged 22 years and older had higher numbers of CFUs, perhaps as a result of being overconfident during the HH procedure [21,44]. Minervini [45] and Sancho [46] suggest that visual tools used for teaching, such as infographics, must be tailored to the characteristics of the students, including their age. Our findings suggest the need to adapt HH practices to take into account students’ ages.
Second-year students achieved the same results as those in senior years. This may be explained by the fact that knowledge of the subject increases in line with the academic year, resulting in an improvement in HH performance among senior students. However, Cruz and Bashtawi [32] failed to observe this relationship. Surprisingly, a number of authors argue that the closer undergraduates are to entering the labour market, the more confident they may feel about performing the technique, resulting in poorer performance [21,44]. According to Fernández-Prada et al. [37], the use of infographics as a teaching tool tends to improve the teaching–learning process during the first academic years. However, the overexposure to digital teaching materials that our students are currently experiencing may be diminishing the effect of posters with the passing of the academic years, leading to a shift away from the results reported by other researchers [47,48].
The multivariate model designed to explain the association between displaying the poster and the likelihood of passing has shown signs of effectiveness when adjusting for the other study variables, although it has not reached statistical significance. Visual tools certainly seem to be useful for optimising and accelerating comprehension processes and are often highly valued by students [29,47]. However, as Bicen and Behesti [49] point out, the main obstacle to the effectiveness of these tools is a lack of precise theoretical knowledge of the subject matter among students and excessive time required to analyse visual tools. The same may be said of infographics. Further studies are required to better assess the impact of these variables on the results obtained in our study.
Pre-HH hand contamination was slightly associated with a lower likelihood of passing. However, we agree with several authors in recommending that HH should be performed with soap and water whenever hands are visibly soiled or have been in contact with contaminants [34,50,51].
Limitations
A potential classification bias may have been introduced by using the same Petri dish for pre- and post-HH culture. To avoid this limitation, we should have used one culture plate for each sample. However, only six plates were contaminated and excluded from the study. If this bias was present, it would be a non-differential bias across all comparison groups.
The last group of fourth-year students, who were assigned to the control group, were not able to participate in the study due to the suspension of face-to-face tuition caused by the COVID-19 pandemic. However, the participation rate for that academic year was 74%, which was satisfactory.
Another limitation could be the presence of an observer during practice. This could result in student nurses washing their hands more thoroughly than usual and obtaining better results regardless of the poster. However, it would be a non-differential bias, since it would affect the two comparison groups equally.
5. Conclusions
This practice-based teaching method combining HH with ABHR and the display of a specific poster on HH shows indications of being effective in improving the quality of HH among nursing students. However, further research is required to confirm this association. A high level of hand contamination prior to the practices decreased the likelihood of achieving a good level of cleanliness. Further evaluation of teaching methods to ensure good technical performance of HH at university level is required to prevent the spread of infectious diseases during the COVID-19 pandemic.
The lack of a constant presence of an observer in future work in the hospital may significantly affect the frequency and implementation of hand-washing procedures.
The evaluation of new HH teaching methods in the college setting ensures that future nurses are educated and sensitised to the spread of infectious diseases during the COVID-19 pandemic.
Improving the hand hygiene procedure is possible if the level of hygiene awareness increases and future health care workers are convinced of the legitimacy and necessity of the effective application of hygiene procedures (internal motivation).
Author Contributions
Conceptualisation: M.G.-L., E.M.-G. and M.Á.P.-M.; methodology: M.G.-L., E.M.-G., A.M.-S., M.Á.P.-M., R.A.C.-G. and M.A.Á.-S.; formal analysis: M.A.Á.-S. and I.G.-G.; investigation: M.G.-L. and M.A.Á.-S.; data curation: I.G.-G. and M.A.Á.-S.; writing—original draft preparation: M.G.-L., E.M.-G., A.M.-S., I.G.-G., M.Á.P.-M., R.A.C.-G. and M.A.Á.-S.; writing—review and editing: M.G.-L., E.M.-G., A.M.-S., I.G.-G., M.Á.P.-M., R.A.C.-G. and M.A.Á.-S.; visualization: M.G.-L. and A.M.-S.; supervision: M.G.-L. All of the authors have read and approved the final manuscript and its submission to the journal. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by Research Ethics Committee of the province of Granada under No 0100-N-21 on 3/15/21.
Informed Consent Statement
Informed consent was obtained from all of the subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Acknowledgments
To all students who participated in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alzyood, M.; Jackson, D.; Aveyard, H.; Brooke, J. COVID-19 reinforces the importance of handwashing. J. Clin. Nurs. 2020, 29, 2760–2761. [Google Scholar] [CrossRef] [PubMed]
- Haque, M. Handwashing in averting infectious diseases: Relevance to COVID-19. J. Popul. Ther. Clin. Pharmacol. 2020, 27, e37–e52. [Google Scholar] [CrossRef]
- Litchman, G.; Marson, J.; Bhatia, N.; Berman, B. Revisiting Handwashing–As It Is Absolutely Essential. J. Drugs Dermatol. 2020, 19, 1127–1129. [Google Scholar] [CrossRef] [PubMed]
- Nieradko-Iwanicka, B. Hygiene–gold standard not only in prevention of COVID-19 infection. Rheumatology 2020, 58, 191–195. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines on Core Components of Infection Prevention and Control Programmes at the National and Acute Health Care Facility Level; World Health Organization: Geneva, Switzerland, 2016; Available online: http://apps.who.int/iris/bitstream/10665/251730/1/%209789241549929-eng.pdf?ua=1 (accessed on 4 April 2021).
- dos Santos, R.P.; Konkewicz, L.R.; Nagel, F.M.; Lisboa, T.; Xavier, R.C.; Jacoby, T.; Gastal, S.L.; Kuplich, N.M.; Pires, M.R.; Lovatto, C.G.; et al. Changes in hand hygiene compliance after a multimodal intervention and seasonality variation. Am. J. Infect. Control. 2013, 41, 1012–1016. [Google Scholar] [CrossRef] [PubMed]
- Ceylan, B.; Gunes, U.; Baran, L.; Ozturk, H.; Sahbudak, G. Examining the hand hygiene beliefs and practices of nursing students and the effectiveness of their handwashing behaviour. J. Clin. Nurs. 2020, 29, 4057–4065. [Google Scholar] [CrossRef] [PubMed]
- Kitsanapun, A.; Yamarat, K. Handwashing determinants and practices among public health students in Thailand. Pak. J. Public Health 2019, 9, 57–60. [Google Scholar] [CrossRef]
- Kitsanapun, A.; Yamarat, K. Evaluating the effectiveness of the “Germ-Free Hands” intervention for improving the hand hygiene practices of public health students. J. Multidiscip. Healthc. 2019, 12, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; McEnroe-Petitte, D.M.; van de Mortel, T.; Nasirudeen, A.M.A. A systematic review on hand hygiene knowledge and compliance in student nurses. Int. Nurs. Rev. 2018, 65, 336–348. [Google Scholar] [CrossRef]
- Gould, D.J.; Moralejo, D.; Drey, N.; Chudleigh, J.H.; Taljaard, M. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst. Rev. 2017, 68, 193–202. [Google Scholar] [CrossRef]
- Luangasanatip, N.; Hongsuwan, M.; Limmathurotsakul, D.; Lubell, Y.; Lee, A.S.; Harbarth, S.; Day, N.P.J.; Graves, N.; Cooper, B. Comparative efficacy of interventions to promote hand hygiene in hospital: Systematic review and network meta-analysis. BMJ 2015, 28, h3728. [Google Scholar] [CrossRef]
- Price, L.; MacDonald, J.; Gozdzielewska, L.; Howe, T.; Flowers, P.; Shepherd, L.; Watt, Y.; Reilly, J. Interventions to improve healthcare workers’ hand hygiene compliance: A systematic review of systematic reviews. Infect. Control Hosp. Epidemiol. 2018, 39, 1449–1456. [Google Scholar] [CrossRef]
- Salmon, S.; Wang, X.; Seetoh, T.; Lee, S.; Fisher, D.A. A novel approach to improve hand hygiene compliance of student nurses. Antimicrob. Resist. Infect. Control. 2013, 2, 16. Available online: http://www.aricjournal.com/content/2/1/16 (accessed on 4 April 2021). [CrossRef]
- Whitcomb, K.S. Using a Multidimensional Approach to Improve Quality Related to Students’ Hand Hygiene Practice. Nurse Educ. 2014, 39, 269–273. [Google Scholar] [CrossRef]
- Kingston, L.M.; O’Connell, N.H.; Dunne, C.P. Survey of attitudes and practices of Irish nursing students towards hand hygiene, including handrubbing with alcohol-based hand rub. Nurse Educ. Today 2017, 52, 57–62. [Google Scholar] [CrossRef]
- Paudel, I.S.; Ghosh, V.; Adhikari, P. Knowledge, Attitude and Practice of nursing students on Hospital Acquired Infections in Western region of Nepal. J. Coll. Med. Sci.-Nepal. 2016, 12, 103–107. [Google Scholar] [CrossRef][Green Version]
- Kısacık, Ö.G.; Ciğerci, Y.; Güneş, Ü. Impact of the fluorescent concretization intervention on effectiveness of hand hygiene in nursing students: A randomized controlled study. Nurse Educ. Today 2021, 97, 104719. [Google Scholar] [CrossRef]
- Sundal, J.S.; Aune, A.G.; Storvig, E.; Aasland, J.K.; Fjeldsaeter, K.L.; Torjuul, K. The hand hygiene compliance of student nurses during clinical placements. J. Clin. Nurs. 2017, 26, 4646–4653. [Google Scholar] [CrossRef]
- Løyland, B.; Peveri, A.M.; Hessevaagbakke, E.; Taasen, I.; Lindeflaten, K. Students’ observations of hand hygiene in nursing homes using the five moments of hand hygiene. J. Clin. Nurs. 2020, 29, 821–830. [Google Scholar] [CrossRef]
- Elola-Vicente, P.; Aroca-Palencia, J.; Huertas-Paredero, M.V.; Díez-Sebastián, J.; Rivas-Bellido, L.; Martínez-Martínez, G.; Nájera-Santos, M.D.L.C.; Muñoz-García, M.L. Programa de formación sobre la higiene de las manos. Estudio comparativo aleatorizado del lavado higiénico y el uso de soluciones alcohólicas. Enferm. Clín. 2008, 18, 5–10. [Google Scholar] [CrossRef]
- Carradine, C. Does Knowledge Make A Difference? Assessing Nursing Students’ Knowledge of Proper Hand Hygiene Techniques in Correlation with Their Progression through Nursing School. 2014. Available online: https://aquila.usm.edu/honors_theses/245 (accessed on 22 April 2021).
- Freitas, M.R.; Gama, Z.A.; Batista, A.M.; Campos, H.H. Implementing patient safety interprofessional practice in developing regions. Med. Educ. 2015, 49, 1157–1158. [Google Scholar] [CrossRef]
- Al-Khawaldeh, O.A.; Al-Hussami, M.; Darawad, M. Influence of Nursing Students Handwashing Knowledge, Beliefs, and Attitudes on Their Handwashing Compliance. Health 2015, 07, 572. [Google Scholar] [CrossRef]
- Škodová, M.; Gimeno-Benítez, A.; Martínez-Redondo, E.; Morán-Cortés, J.F.; Jiménez-Romano, R.; Gimeno-Ortiz, A. Hand hygiene technique quality evaluation in nursing and medicine students of two academic courses. Rev. Lat. Am. Enfermagem. 2015, 23, 708–717. [Google Scholar] [CrossRef]
- Konicki, T.; Miller, E. Use of a simulation intervention to examine differences in nursing students’ hand hygiene knowledge, beliefs, and behaviors. Nurse Educ. Today 2016, 45, 96–101. [Google Scholar] [CrossRef]
- Suen, L.K.P.; Wong, J.W.S.; Lo, K.Y.K.; Lai, T.K.H. The use of hand scanner to enhance hand hygiene practice among nursing students: A single-blinded feasibility study. Nurse Educ. Today 2019, 76, 137–147. [Google Scholar] [CrossRef]
- Öncü, E.; Vayısoğlu, S.K.; Lafcı, D.; Yıldız, E. An evaluation of the effectiveness of nursing students’ hand hygiene compliance: A cross-sectional study. Nurse Educ. Today 2018, 65, 218–224. [Google Scholar] [CrossRef]
- Jenner, E.A.; Jones, F.; Fletcher, B.C.; Miller, L.; Scott, G.M. Hand hygiene posters: Selling the message. J. Hosp. Infect. 2005, 59, 77–82. [Google Scholar] [CrossRef]
- Lawson, A.; Vaganay-Miller, M. The Effectiveness of a Poster Intervention on Hand Hygiene Practice and Compliance When Using Public Restrooms in a University Setting. Int. J. Environ. Res. Public Health 2019, 16, 5036. [Google Scholar] [CrossRef]
- Safety, W.P. Guía de Aplicación de la Estrategia Multimodal de la OMS Para la Mejora de la Higiene de las Manos. Ministerio de Sanidad, Política Social e Igualdad. 2010, p. 49. Available online: https://apps.who.int/iris/bitstream/handle/10665/102536/WHO_IER_PSP_2009.02_spa.pdf (accessed on 22 April 2021).
- Cruz, J.P.; Bashtawi, M.A. Predictors of hand hygiene practice among Saudi nursing students: A cross-sectional self-reported study. J. Infect. Public Health 2016, 9, 485–493. [Google Scholar] [CrossRef]
- Da Silva, V.D.; Caetano, J.Á.; Silva LA da Freitas, M.M.C.; de Almeida, P.C.; Rodrigues, J.L.N. Assessment of hand hygiene of nursing and medical students. Rev. Rede Enferm Nordeste 2017, 18, 257. Available online: http://www.repositorio.ufc.br/handle/riufc/22725 (accessed on 22 April 2021). [CrossRef]
- Safety, W.P. Manual Técnico de Referencia Para la higiene de Las Manos: Dirigido a Los Profesionales Sanitarios, a Los Formadores ya Los Observadores de Las Prácticas de Higiene de Las Manos. Ministerio de Sanidad, Política Social e Igualdad. 2009. Available online: https://apps.who.int/iris/bitstream/handle/10665/102537/WHO_IER_PSP_2009.02_spa.pdf (accessed on 22 April 2021).
- Ministry of Health of the People’s Republic of China. Standard of Health Workers’ Hand Hygiene. Chin. J. Nosocomiol. 2009, 19, I–II. [Google Scholar]
- Xiong, P.; Zhang, J.; Wang, X.; Wu, T.L.; Hall, B.J. Effects of a mixed media education intervention program on increasing knowledge, attitude, and compliance with standard precautions among nursing students: A randomized controlled trial. Am. J. Infect. Control. 2017, 45, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Prada, M.; González-Cabrera, J.; Ortega-López, Y.; Martínez-Bellón, M.; Fernández-Crehuet, M.; Bueno-Cavanillas, A. Evaluación de un taller práctico sobre higiene de manos impartido por estudiantes entrenados. Educ. Med. 2012, 15, 149–154. [Google Scholar]
- Pérez-Pérez, P.; Herrera-Usagre, M.; Bueno-Cavanillas, A.; Alonso-Humada, M.S.; Buiza-Camacho, B.; Vázquez-Vázquez, M. Higiene de las manos: Conocimientos de los profesionales y áreas de mejora. Cad. Saúde Pública 2015, 31, 149–160. [Google Scholar] [CrossRef][Green Version]
- Romero, D.M.P.; Reboredo, M.M.; Gomes, E.P.; Coelho, C.M.; de Paula, M.A.S.; de Souza, L.C.; Colugnati, F.A.B.; Pinheiro, B.V. Effects of the implementation of a hand hygiene education program among ICU professionals: An interrupted time-series analysis. J. Bras. Pneumol. 2019, 45, e20180152. [Google Scholar] [CrossRef]
- Schwartz, J.; King, C.-C.; Yen, M.-Y. Protecting Healthcare Workers during the Coronavirus Disease 2019 (COVID-19) Outbreak: Lessons from Taiwan’s Severe Acute Respiratory Syndrome Response. Clin. Infect. Dis. 2020, 71, 858–860. [Google Scholar] [CrossRef]
- Wong, S.C.Y.; Kwong, R.T.-S.; Wu, T.C.; Chan, J.W.M.; Chu, M.Y.; Lee, S.Y.; Wong, H.; Lung, D. Risk of nosocomial transmission of coronavirus disease 2019: An experience in a general ward setting in Hong Kong. J. Hosp. Infect. 2020, 105, 119–127. [Google Scholar] [CrossRef]
- Anderson, J.L.; Warren, C.A.; Perez, E.; Louis, R.I.; Phillips, S.; Wheeler, J.; Cole, M.; Misra, R. Gender and ethnic differences in hand hygiene practices among college students. Am. J. Infect. Control. 2008, 36, 361–368. [Google Scholar] [CrossRef]
- Merino-Plaza, M.J.; Rodrigo-Bartual, V.; Boza-Cervilla, M.; García-Llopis, A.; Gomez-Pajares, F.; Carrera-Hueso, F.J.; Fikri-Benbrahim, N. ¿Cómo Incrementar la Adhesión del Personal Sanitario al Protocolo de Higiene de Manos? Rev. Esp. Salud Pública 2020, 92, e201810072. Available online: https://www.scielosp.org/pdf/resp/2018.v92/e201810072/es (accessed on 6 May 2021).
- Dembilio-Villar, T.; González-Chordá, V.M.; Cervera-Gascch, Á.; Mena-Tudela, D.; Dembilio-Villar, T.; González-Chordá, V.M.; Mena-Tudela, D. Cooperative Learning and Hand Disinfection in Nursing Students. Investig. Educ. Enferm. 2018, 36. [Google Scholar] [CrossRef]
- Minervini, M.A. La Infografía Como Recurso Didáctico. Rev. Lat. Comun. Soc. 2005, 8. Available online: https://www.redalyc.org/pdf/819/81985906.pdf (accessed on 6 May 2021).
- Sancho, J.L.V. La comunicación de contenidos en la infografía digital. Estud. Sobre Mensaje Periodís 2010, 16, 469–483. Available online: https://revistas.ucm.es/index.php/ESMP/article/view/ESMP1010110469A/11514 (accessed on 6 May 2021).
- Aguirre, C.R.; Valencia, E.M.; Morales, H.L. Elaboración de infografías: Hacia el desarrollo de competencias del siglo XXI. Diá-Logos 2015, 23–37. [Google Scholar] [CrossRef][Green Version]
- Naparin, H.; Binti Saad, A. Infographics in Education: Review on Infographics Design. Int. J. Multimed Its Appl. 2017, 9, 15–24. [Google Scholar] [CrossRef]
- Bicen, H.; Beheshti, M. The Psychological Impact of Infographics in Education. BRAIN Broad Res. Artif. Intell. Neurosci. 2017, 8, 99–108. Available online: https://www.researchgate.net/publication/335137517 (accessed on 6 May 2021).
- Chen, X.; Ran, L.; Liu, Q.; Hu, Q.; Du, X.; Tan, X. Hand Hygiene, Mask-Wearing Behaviors and Its Associated Factors during the COVID-19 Epidemic: A Cross-Sectional Study among Primary School Students in Wuhan, China. Int. J. Environ. Res. Public Health 2020, 17, 2893. [Google Scholar] [CrossRef]
- Sánchez-Payá, J.; Galicia-García, M.D.; Gracia-Rodríguez, R.M.; García-González, C.; Fuster-Pérez, M.; López-Fresneña, N.; Avendaño-Corcoles, F.; González-Torga, A. Grado de cumplimiento y determinantes de las recomendaciones sobre la higiene de manos. Enferm. Infecc. Microbiol. Clín. 2007, 25, 369–375. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).