Effects of Regular Long-Term Circuit Training (Once per Week) on Cardiorespiratory Fitness in Previously Sedentary Adults
Abstract
1. Introduction
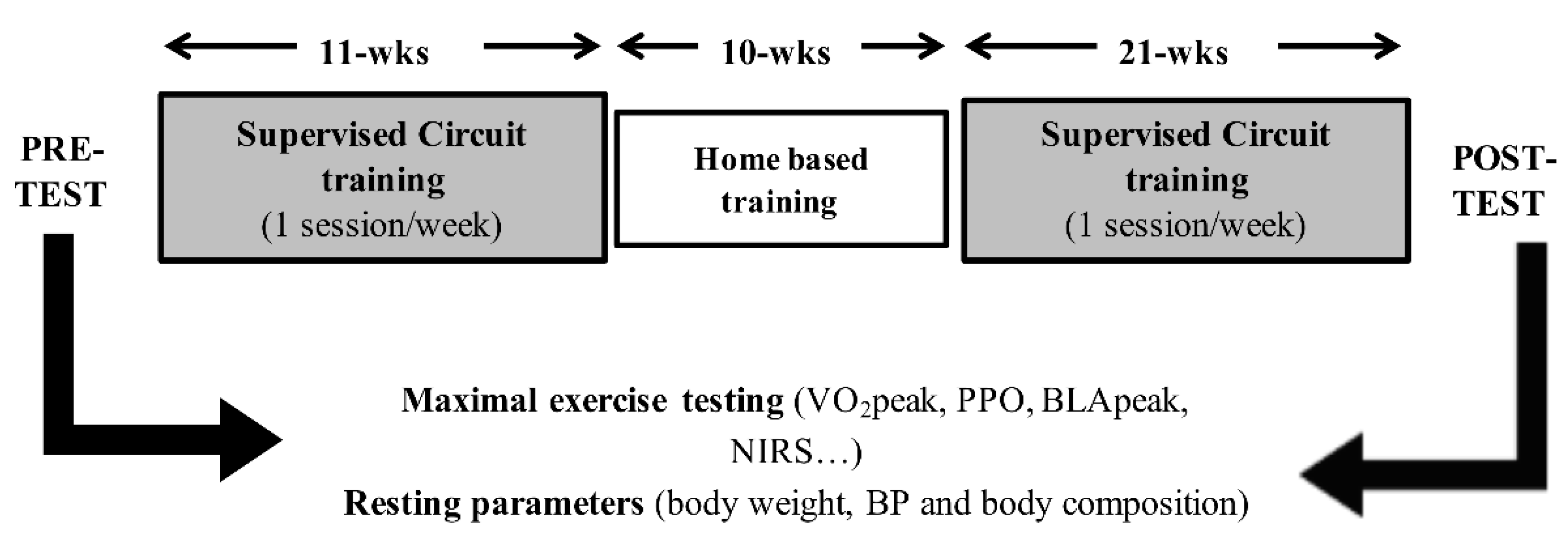
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.2.1. Resting Measurements
2.2.2. Exercise Testing
2.3. Intervention, Physical Activity
2.4. Statistical Analysis
3. Results
3.1. Training Adaptions within the SG
3.2. Training Adaptions within the AG
3.3. Between-Group Differences in Training Adaptions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Szostak, J.; Laurant, P. The forgotten face of regular physical exercise: A ‘natural’ anti-atherogenic activity. Clin. Sci. 2011, 121, 91–106. [Google Scholar] [CrossRef]
- Myers, J.; Prakash, M.; Froelicher, V.; Do, D.; Partington, S.; Atwood, J.E. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 2002, 346, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, P.; Myers, J.; Kokkinos, J.P.; Pittaras, A.; Narayan, P.; Manolis, A.; Karasik, P.; Greenberg, M.; Papademetriou, V.; Singh, S. Exercise capacity and mortality in black and white men. Circulation 2008, 117, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Group, L.P.A.S.W. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Murias, J.M.; Kowalchuk, J.M.; Paterson, D.H. Time course and mechanisms of adaptations in cardiorespiratory fitness with endurance training in older and young men. J. Appl. Physiol. 2010, 108, 621–627. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S.; American College of Sports Medicine. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- Romero-Arenas, S.; Martínez-Pascual, M.; Alcaraz, P.E. Impact of resistance circuit training on neuromuscular, cardiorespiratory and body composition adaptations in the elderly. Aging Dis. 2013, 4, 256–263. [Google Scholar] [CrossRef]
- Buckley, S.; Knapp, K.; Lackie, A.; Lewry, C.; Horvey, K.; Benko, C.; Trinh, J.; Butcher, S. Multimodal high-intensity interval training increases muscle function and metabolic performance in females. Appl. Physiol. Nutr. Metab. 2015, 40, 1157–1162. [Google Scholar] [CrossRef]
- McRae, G.; Payne, A.; Zelt, J.G.; Scribbans, T.D.; Jung, M.E.; Little, J.P.; Gurd, B.J. Extremely low volume, whole-body aerobic-resistance training improves aerobic fitness and muscular endurance in females. Appl. Physiol. Nutr. Metab. 2012, 37, 1124–1131. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Campo, D.J.; Andreu-Caravaca, L.; Carrasco-Poyatos, M.; Benito, P.J.; Rubio-Arias, J. Effects of circuit resistance training on body composition, strength, and cardiorespiratory fitness in middle-aged and older women: A systematic review and meta-analysis. J. Aging Phys. Act. 2021, 1–14. [Google Scholar] [CrossRef]
- Myers, T.R.; Schneider, M.G.; Schmale, M.S.; Hazell, T.J. Whole-body aerobic resistance training circuit improves aerobic fitness and muscle strength in sedentary young females. J. Strength Cond. Res. 2015, 29, 1592–1600. [Google Scholar] [CrossRef] [PubMed]
- Kaikkonen, H.; Yrjämä, M.; Siljander, E.; Byman, P.; Laukkanen, R. The effect of heart rate controlled low resistance circuit weight training and endurance training on maximal aerobic power in sedentary adults. Scand. J. Med. Sci. Sports 2000, 10, 211–215. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.; Bredin, S.S. Reflections on physical activity and health: What should we recommend? Can. J. Cardiol. 2016, 32, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.; Janssen, I. Is the frequency of weekly moderate-to-vigorous physical activity associated with the metabolic syndrome in Canadian adults? Appl. Physiol. Nutr. Metab. 2013, 38, 773–778. [Google Scholar] [CrossRef][Green Version]
- Glowacki, S.P.; Martin, S.E.; Maurer, A.; Baek, W.; Green, J.S.; Crouse, S.F. Effects of resistance, endurance, and concurrent exercise on training outcomes in men. Med. Sci. Sports Exerc. 2004, 36, 2119–2127. [Google Scholar] [CrossRef]
- Sperlich, B.; Wallmann-Sperlich, B.; Zinner, C.; Von Stauffenberg, V.; Losert, H.; Holmberg, H.C. Functional high-intensity circuit training improves body composition, peak oxygen uptake, strength, and alters certain dimensions of quality of life in overweight women. Front. Physiol. 2017, 8, 172. [Google Scholar] [CrossRef]
- Aittasalo, M.; Livson, M.; Lusa, S.; Romo, A.; Vähä-Ypyä, H.; Tokola, K.; Sievänen, H.; Mänttäri, A.; Vasankari, T. Moving to business—Changes in physical activity and sedentary behavior after multilevel intervention in small and medium-size workplaces. BMC Public Health 2017, 17, 319. [Google Scholar] [CrossRef]
- Carlin, A.; Perchoux, C.; Puggina, A.; Aleksovska, K.; Buck, C.; Burns, C.; Cardon, G.; Chantal, S.; Ciarapica, D.; Condello, G.; et al. A life course examination of the physical environmental determinants of physical activity behaviour: A “Determinants of Diet and Physical Activity” (DEDIPAC) umbrella systematic literature review. PLoS ONE 2017, 12, e0182083. [Google Scholar] [CrossRef]
- Bacon, A.P.; Carter, R.E.; Ogle, E.A.; Joyner, M.J. VO2max trainability and high intensity interval training in humans: A meta-analysis. PLoS ONE 2013, 8, e73182. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Boushel, R.; Langberg, H.; Olesen, J.; Gonzales-Alonzo, J.; Bülow, J.; Kjaer, M. Monitoring tissue oxygen availability with near infrared spectroscopy (NIRS) in health and disease. Scand. J. Med. Sci. Sports 2001, 11, 213–222. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, ON, Canada, 1988. [Google Scholar]
- Delecluse, C.; Colman, V.; Roelants, M.; Verschueren, S.; Derave, W.; Ceux, T.; Eijnde, B.O.; Seghers, J.; Pardaens, K.; Brumagne, S.; et al. Exercise programs for older men: Mode and intensity to induce the highest possible health-related benefits. Prev. Med. 2004, 39, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Murias, J.M.; Kowalchuk, J.M.; Paterson, D.H. Mechanisms for increases in V•O2max with endurance training in older and young women. Med. Sci. Sports Exerc. 2010, 42, 1891–1898. [Google Scholar] [CrossRef] [PubMed]
- Sillanpää, E.; Häkkinen, A.; Punnonen, K.; Häkkinen, K.; Laaksonen, D.E. Effects of strength and endurance training on metabolic risk factors in healthy 40–65-year-old men. Scand. J. Med. Sci. Sports 2009, 19, 885–895. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, M.; Gatterer, H.; Kunczicky, H.; Brandstätter, E.; Ulmer, H. Supervised exercise in patients with impaired fasting glucose: Impact on exercise capacity. Clin. J. Sport Med. 2009, 19, 394–398. [Google Scholar] [CrossRef]
- Kusy, K.; Zieliński, J. Aerobic capacity in speed-power athletes aged 20-90 years vs endurance runners and untrained participants. Scand. J. Med. Sci. Sports 2014, 24, 68–79. [Google Scholar] [CrossRef]
- Ichimura, S.; Murase, N.; Osada, T.; Kime, R.; Homma, T.; Ueda, C.; Nagasawa, T.; Motobe, M.; Hamaoka, T.; Katsumura, T. Age and activity status affect muscle reoxygenation time after maximal cycling exercise. Med. Sci. Sports Exerc. 2006, 38, 1277–1281. [Google Scholar] [CrossRef]
- Neary, J.P.; McKenzie, D.C.; Bhambhani, Y.N. Effects of short-term endurance training on muscle deoxygenation trends using NIRS. Med. Sci. Sports Exerc. 2002, 34, 1725–1732. [Google Scholar] [CrossRef]
- Carneiro, H.A.; Song, R.J.; Lee, J.; Schwartz, B.; Vasan, R.S.; Xanthakis, V. Association of blood pressure and heart rate responses to submaximal exercise with incident heart failure: The framingham heart study. J. Am. Heart Assoc. 2021, 10, e019460. [Google Scholar] [CrossRef] [PubMed]
- Kjeldsen, S.E.; Mundal, R.; Sandvik, L.; Erikssen, G.; Thaulow, E.; Erikssen, J. Exercise blood pressure predicts cardiovascular death and myocardial infarction. Blood Press. Monit. 1997, 2, 147–153. [Google Scholar] [PubMed]
- Lovell, D.I.; Cuneo, R.; Gass, G.C. Strength training improves submaximum cardiovascular performance in older men. J. Geriatr. Phys. Ther. 2009, 32, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Venturelli, M.; Cè, E.; Limonta, E.; Schena, F.; Caimi, B.; Carugo, S.; Veicsteinas, A.; Esposito, F. Effects of endurance, circuit, and relaxing training on cardiovascular risk factors in hypertensive elderly patients. Age 2015, 37, 101. [Google Scholar] [CrossRef] [PubMed]
| SG | AG | |||||
|---|---|---|---|---|---|---|
| Female (n = 5) | Male (n = 5) | Total (n = 10) | Female (n = 3) | Male (n = 7) | Total (n = 10) | |
| Age [years] | 52 ± 5 | 51 ± 8 | 51 ± 6 | 53 ± 11 | 51 ± 7 | 51 ± 8 |
| Height [m] | 1.72 ± 0.05 | 1.78 ± 0.04 | 1.74 ± 0.08 | 1.65 ± 0.05 | 1.78 ± 0.05 | 1.74 ± 0.07 |
| BMI [kg/m2] | 24.4 ± 2.9 | 26.8 ± 3.7 | 25.6 ± 3.1 | 22.6 ± 0.7 | 25.2 ± 0.8 | 24.4 ± 1.4 |
| Sedentary Group | Active Group | Group × Time | Time | η2p | η2p | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Pre-Test | Post-Test | n | Pre-Test | Post-Test | p-Value | p-Values | Group × Time | Time | |
| Resting parameters | ||||||||||
| HRrest [bpm] | 9 | 74 ± 13 | 78 ± 13 | 10 | 66 ± 13 | 65 ± 10 | 0.515 | 0.534 | 0.025 | 0.023 |
| Body mass [kg] | 10 | 78.2 ± 10.9 | 78.5 ± 11.9 | 10 | 74.5 ± 9.3 | 75.6 ± 9.8 * | 0.410 | 0.142 | 0.038 | 0.116 |
| SBP [mmHg] | 10 | 120 ± 11 | 117 ± 15 | 10 | 126 ± 13 | 128 ± 24 | 0.422 | 0.905 | 0.036 | 0.001 |
| DBP [mmHg] | 10 | 84 ± 12 | 84 ± 10 | 10 | 83 ± 9 | 88 ± 12 | 0.306 | 0.226 | 0.058 | 0.080 |
| FFM [%] | 10 | 71.2 ± 8.7 | 72.6 ± 6.3 | 10 | 76.9 ± 4.8 | 78.2 ± 5.3 * | 0.960 | 0.184 | 0.000 | 0.096 |
| MM [%] | 10 | 47.0 ± 6.2 | 48.0 ± 5.5 | 10 | 53.6 ± 4.6 | 54.2 ± 4.7 | 0.695 | 0.128 | 0.009 | 0.124 |
| FM [%] | 10 | 27.8 ± 6.7 | 27.4 ± 6.3 | 10 | 23.1 ± 4.8 | 21.8 ± 5.3 * | 0.511 | 0.222 | 0.024 | 0.082 |
| Exercise testing | ||||||||||
| VO2peak [mL/min] | 9 | 2367 ± 494 | 2232 ± 461 | 9 | 3246 ± 859 | 3086 ± 795 | 0.822 | 0.018 | 0.003 | 0.301 |
| VO2peak [mL/kg/min] | 9 | 30.8 ± 6.9 | 28.9 ± 6.0 | 9 | 43.1 ± 7.3 | 40.3 ± 6.5 * | 0.509 | 0.005 | 0.028 | 0.405 |
| PPO [watts] | 10 | 181 ± 45 | 171 ± 44 | 10 | 252 ± 66 | 235 ± 65 * | 0.484 | 0.012 | 0.028 | 0.300 |
| PPO [watts/kg] | 10 | 2.3 ± 0.6 | 2.2 ± 0.6 | 10 | 3.3 ± 0.6 | 3.1 ± 0.6 * | 0.258 | 0.009 | 0.070 | 0.321 |
| BLApeak [mmol/L] | 10 | 8.4 ± 2.3 | 7.3 ± 2.0 | 10 | 11.0 ± 2.4 | 8.8 ± 2.9 * | 0.218 | 0.002 | 0.083 | 0.428 |
| HRpeak [bpm] | 10 | 174 ± 10 | 171 ± 13 | 9 | 178 ± 10 | 172 ± 8 | 0.563 | 0.016 | 0.021 | 0.314 |
| RPEpeak | 10 | 18.3 ± 1.7 | 17.4 ± 1.3 | 10 | 18.4 ± 1.4 | 17.4 ± 1.3 | 0.908 | 0.063 | 0.001 | 0.188 |
| SBP 100 watts [mmHg] | 7 | 180 ± 14 | 170 ± 17 * | 9 | 173 ± 21 | 171 ± 18 | 0.330 | 0.146 | 0.068 | 0.145 |
| DBP 100 watts [mmHg] | 7 | 100 ± 20 | 93 ± 11 | 9 | 89 ± 9 | 86 ± 10 | 0.525 | 0.184 | 0.029 | 0.122 |
| HRsubmax [bpm] | 9 | 128 ± 11 | 125 ± 11 | 9 | 113 ± 15 | 114 ± 16 | 0.616 | 0.643 | 0.016 | 0.014 |
| BLAsubmax [mmol/L] | 9 | 1.9 ± 0.8 | 2.1 ± 2.0 | 10 | 1.6 ± 0.7 | 1.7 ± 0.8 | 0.741 | 0.412 | 0.007 | 0.040 |
| Deoxygenation [%] | 9 | −9.2 ± 8.3 | −8.3 ± 11.3 | 7 | −15.4 ± 7.8 | −17.9 ± 9.0 | 0.267 | 0.600 | 0.087 | 0.020 |
| Reoxygenation [%] | 9 | 7.0 ± 6.3 | 11.0 ± 8.9 * | 7 | 12.3 ± 8.1 | 13.6 ± 10.7 | 0.230 | 0.028 | 0.101 | 0.299 |
| nTHImean [au] | 9 | 0.966 ± 0.127 | 0.974 ± 0.084 | 6 | 1.053 ± 0.118 | 1.094 ± 0.078 | 0.613 | 0.455 | 0.020 | 0.044 |
| nTHI30 s [au] | 9 | 0.969 ± 0.187 | 1.003 ± 0.093 | 7 | 1.037 ± 0.149 | 1.091 ± 0.113 | 0.802 | 0.285 | 0.005 | 0.081 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menz, V.; Gatterer, H.; Amin, S.B.; Huber, R.; Burtscher, M. Effects of Regular Long-Term Circuit Training (Once per Week) on Cardiorespiratory Fitness in Previously Sedentary Adults. Int. J. Environ. Res. Public Health 2021, 18, 10897. https://doi.org/10.3390/ijerph182010897
Menz V, Gatterer H, Amin SB, Huber R, Burtscher M. Effects of Regular Long-Term Circuit Training (Once per Week) on Cardiorespiratory Fitness in Previously Sedentary Adults. International Journal of Environmental Research and Public Health. 2021; 18(20):10897. https://doi.org/10.3390/ijerph182010897
Chicago/Turabian StyleMenz, Verena, Hannes Gatterer, Sachin B. Amin, Reinhard Huber, and Martin Burtscher. 2021. "Effects of Regular Long-Term Circuit Training (Once per Week) on Cardiorespiratory Fitness in Previously Sedentary Adults" International Journal of Environmental Research and Public Health 18, no. 20: 10897. https://doi.org/10.3390/ijerph182010897
APA StyleMenz, V., Gatterer, H., Amin, S. B., Huber, R., & Burtscher, M. (2021). Effects of Regular Long-Term Circuit Training (Once per Week) on Cardiorespiratory Fitness in Previously Sedentary Adults. International Journal of Environmental Research and Public Health, 18(20), 10897. https://doi.org/10.3390/ijerph182010897







