Generalized Anxiety as a Risk Factor for Dysfunctional Eating Behavior after Obesity Surgery during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Method
2.1. Participants and Procedure
2.2. Measures
2.3. Data Analysis
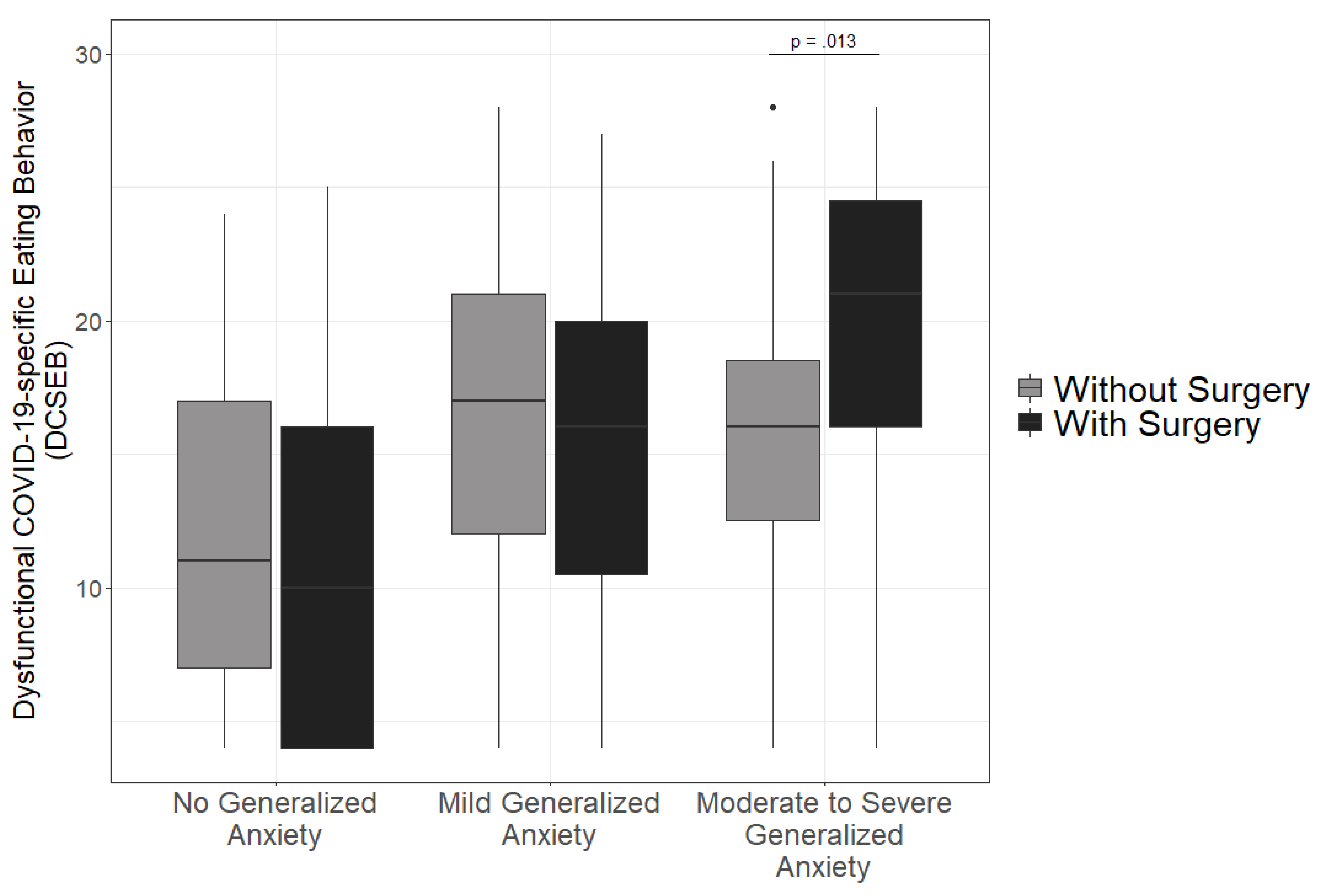
3. Results
4. Discussion
4.1. Limitations
4.2. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Remarks at the Media Briefing on 2019-nCoV on 11 February 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed on 23 June 2021).
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 23 June 2021).
- Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; Naghavi, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Dietz, W.; Santos-Burgoa, C. Obesity and its implications for COVID-19 mortality. Obesity 2020, 28, 1005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capelo, A.; Da Fonseca, V.; Peixoto, M.; de Carvalho, S.; Azevedo, C.; Elsas, M.; Marques, B. Visceral adiposity is associated with cytokines and decrease in lung function in women with persistent asthma. Rev. Port. Pneumol. 2016, 22, 255–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muniyappa, R.; Gubbi, S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am. J. Physiol.-Endocrinol. Metab. 2020, 318, E736–E741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Tartof, S.Y.; Qian, L.; Hong, V.; Wei, R.; Nadjafi, R.F.; Fischer, H.; Li, Z.; Shaw, S.F.; Caparosa, S.L.; Nau, C.L. Obesity and mortality among patients diagnosed with COVID-19: Results from an integrated health care organization. Ann. Intern. Med. 2020, 173, 773–781. [Google Scholar] [CrossRef]
- Mack, I.; Olschlager, S.; Sauer, H.; von Feilitzsch, M.; Weimer, K.; Junne, F.; Peeraully, R.; Enck, P.; Zipfel, S.; Teufel, M. Does Laparoscopic Sleeve Gastrectomy Improve Depression, Stress and Eating Behaviour? A 4-Year Follow-up Study. Obes. Surg. 2016, 26, 2967–2973. [Google Scholar] [CrossRef]
- Rajan, T.; Menon, V. Psychiatric disorders and obesity: A review of association studies. J. Postgrad. Med. 2017, 63, 182. [Google Scholar]
- Sheehan, D.V.; Herman, B.K. The Psychological and Medical Factors Associated With Untreated Binge Eating Disorder. Prim. Care Companion. CNS Disord. 2015. [Google Scholar] [CrossRef] [Green Version]
- Simon, G.E.; Von Korff, M.; Saunders, K.; Miglioretti, D.L.; Crane, P.K.; van Belle, G.; Kessler, R.C. Association between obesity and psychiatric disorders in the US adult population. Arch. Gen. Psychiatry 2006, 63, 824–830. [Google Scholar] [CrossRef] [Green Version]
- Luppino, F.S.; de Wit, L.M.; Bouvy, P.F.; Stijnen, T.; Cuijpers, P.; Penninx, B.W.; Zitman, F.G. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch. Gen. Psychiatry 2010, 67, 220–229. [Google Scholar] [CrossRef]
- Sockalingam, S.; Leung, S.E.; Cassin, S.E. The impact of coronavirus disease 2019 on bariatric surgery: Redefining psychosocial care. Obesity 2020, 28, 1010–1012. [Google Scholar] [CrossRef] [Green Version]
- Braden, A.; Musher-Eizenman, D.; Watford, T.; Emley, E. Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite 2018, 125, 410–417. [Google Scholar] [CrossRef]
- Kelly, N.R.; Tanofsky-Kraff, M.; Vannucci, A.; Ranzenhofer, L.M.; Altschul, A.M.; Schvey, N.A.; Shank, L.M.; Brady, S.M.; Galescu, O.; Kozlosky, M. Emotion dysregulation and loss-of-control eating in children and adolescents. Health Psychol. 2016, 35, 1110. [Google Scholar] [CrossRef]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Skoda, E.-M.; Bäuerle, A.; Schweda, A.; Dörrie, N.; Musche, V.; Hetkamp, M.; Kohler, H.; Teufel, M.; Weismüller, B. Severely increased generalized anxiety, but not COVID-19-related fear in individuals with mental illnesses: A population based cross-sectional study in Germany. Int. J. Soc. Psychiatry 2020, 67, 0020764020960773. [Google Scholar] [CrossRef]
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020, 10, e12386. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Munguía, L.; Mestre-Bach, G.; Steward, T.; Etxandi, M.; Baenas, I.; Granero, R.; Sánchez, I.; Ortega, E.; Andreu, A. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity—A collaborative international study. Eur. Eat. Disord. Rev. 2020, 28, 871–883. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Varela, J.E. Bariatric surgery for obesity and metabolic disorders: State of the art. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 160. [Google Scholar] [CrossRef] [PubMed]
- Deutsche Gesellschaft für Allgemein- und Viszeralchirurgie. S3-Leitlinie: Chirurgie der Adipositas und metabolischer Erkrankungen. Available online: https://www.awmf.org/uploads/tx_szleitlinien/088-001l_S3_Chirurgie-Adipositasmetabolische-Erkrankungen_2018-02.pdf (accessed on 23 June 2021).
- Osterhues, A.; von Lengerke, T.; Mall, J.W.; de Zwaan, M.; Müller, A. Health-Related Quality of Life, Anxiety, and Depression in Bariatric Surgery Candidates Compared to Patients from a Psychosomatic Inpatient Hospital. Obes. Surg. 2017, 27, 2378–2387. [Google Scholar] [CrossRef] [PubMed]
- Behrens, S.C.; Lenhard, K.; Junne, F.; Ziser, K.; Lange, J.; Zipfel, S.; Giel, K.E.; Teufel, M.; Mack, I. Effects of Bariatric Surgery on Depression: Role of Body Image. Obes. Surg. 2021, 31, 1864–1868. [Google Scholar] [CrossRef]
- Wimmelmann, C.L.; Dela, F.; Mortensen, E.L. Psychological predictors of mental health and health-related quality of life after bariatric surgery: A review of the recent research. Obes. Res. Clin. Pract. 2014, 8, e314–e324. [Google Scholar] [CrossRef]
- Nasirzadeh, Y.; Kantarovich, K.; Wnuk, S.; Okrainec, A.; Cassin, S.E.; Hawa, R.; Sockalingam, S. Binge Eating, Loss of Control over Eating, Emotional Eating, and Night Eating After Bariatric Surgery: Results from the To-ronto Bari-PSYCH Cohort Study. Obes. Surg. 2018, 28, 2032–2039. [Google Scholar] [CrossRef]
- Kubik, J.F.; Gill, R.S.; Laffin, M.; Karmali, S. The impact of bariatric surgery on psychological health. J. Obes. 2013, 2013, 837989. [Google Scholar] [CrossRef] [Green Version]
- Arroll, B.; Goodyear-Smith, F.; Crengle, S.; Gunn, J.; Kerse, N.; Fishman, T.; Falloon, K.; Hatcher, S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann. Fam. Med. 2010, 8, 348–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Kertz, S.; Bigda-Peyton, J.; Bjorgvinsson, T. Validity of the Generalized Anxiety Disorder-7 Scale in an acute psychiatric sample. Clin. Psychol. Psychother. 2013, 20, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Bäuerle, A.; Steinbach, J.; Schweda, A.; Beckord, J.; Hetkamp, M.; Weismüller, B.; Kohler, H.; Musche, V.; Dörrie, N.; Teufel, M. Mental health burden of the COVID-19 outbreak in germany: Predictors of mental health impairment. J. Prim. Care Community Health 2020, 11, 2150132720953682. [Google Scholar] [CrossRef] [PubMed]
- Weismüller, B.; Schweda, A.; Dörrie, N.; Musche, V.; Fink, M.; Kohler, H.; Skoda, E.M.; Teufel, M.; Bäuerle, A. Different Correlates of COVID-19-Related Adherent and Dysfunctional Safety Behavior. Front. Public Health 2020, 8, 625664. [Google Scholar] [CrossRef]
- Maechler, M.; Rousseeuw, P.; Croux, C.; Todorov, V.; Ruckstuhl, A.; Salibian-Barrera, M.; Verbeke, T.; Koller, M.; Conceicao, E.L.; di Palma, M.A. Package ‘robustbase’. Basic Robust Stat. Available online: https://cran.r-project.org/web/packages/robustbase/index.html (accessed on 10 October 2021).
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child. Adolesc. Psychiatry 2021, 25, 1–11. [Google Scholar]
- Montemurro, N. The emotional impact of COVID-19: From medical staff to common people. BrainBehav. Immun. 2020, 87, 23–24. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Bulik, C.M.; Sullivan, P.F.; Fear, J.; Joyce, P.R. Eating disorders and antecedent anxiety disorders: A controlled study. Acta Psychiatr. Scand. 1997, 96, 101–107. [Google Scholar] [CrossRef]
- Kaye, W.; Bulik, C.; Thornton, L.; Barbarich, N.; Masters, K.; Group PFC. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am. J. Psychiatry 2004, 161, 2215–2221. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, A.; Danner, U.; Parks, M. Emotion regulation in binge eating disorder: A review. Nutrients 2017, 9, 1274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckner, J.D.; Silgado, J.; Lewinsohn, P.M. Delineation of differential temporal relations between specific eating and anxiety disorders. J. Psychiatr. Res. 2010, 44, 781–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matos, M.I.R.; Aranha, L.S.; Faria, A.N.; Ferreira, S.R.; Bacaltchuck, J.; Zanella, M.T. Binge eating disorder, anxiety, depression and body image in grade III obesity patients. Braz. J. Psychiatry 2002, 24, 165–169. [Google Scholar] [CrossRef] [Green Version]
- Wonderlich-Tierney, A.L.; Vander Wal, J.S. The effects of social support and coping on the relationship between social anxiety and eating disorders. Eat. Behav. 2010, 11, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Kate, P.; Deshmukh, G.; Datir, R.; Rao, J. Good mood foods. J. Nutr. Health Food Eng. 2017, 7, 345–351. [Google Scholar]
- Volkow, N.; Wang, G.; Fowler, J.; Tomasi, D.; Baler, R. Food and drug reward: Overlapping circuits in human obesity and addiction. Brain Imaging Behav. Neurosci. 2011, 11, 1–24. [Google Scholar]
- Walędziak, M.; Różańska-Walędziak, A.; Pędziwiatr, M.; Szeliga, J.; Proczko-Stepaniak, M.; Wysocki, M.; Stefura, T.; Major, P. Bariatric surgery during COVID-19 pandemic from patients’ point of view—The results of a national survey. J. Clin. Med. 2020, 9, 1697. [Google Scholar] [CrossRef] [PubMed]
- Wild, B.; Hunnemeyer, K.; Sauer, H.; Schellberg, D.; Muller-Stich, B.P.; Konigsrainer, A.; Weiner, R.; Zipfel, S.; Herzog, W.; Teufel, M. Sustained effects of a psychoeducational group intervention following bariatric surgery: Follow-up of the randomized controlled BaSE study. Surg. Obes. Relat. Dis. 2017, 13, 1612–1618. [Google Scholar] [CrossRef] [PubMed]
- Archid, R.; Archid, N.; Meile, T.; Hoffmann, J.; Hilbert, J.; Wulff, D.; Teufel, M.; Muthig, M.; Quante, M.; Konigsrainer, A.; et al. Patients with Schizophrenia Do Not Demonstrate Worse Outcome After Sleeve Gastrectomy: A Short-Term Cohort Study. Obes. Surg. 2019, 29, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Robitzsch, A.; Schweda, A.; Hetkamp, M.; Niedergethmann, M.; Dörrie, N.; Herpertz, S.; Hasenberg, T.; Tagay, S.; Teufel, M.; Skoda, E.-M. The Impact of Psychological Resources on Body Mass Index in Obesity Surgery Candidates. Front. Psychiatry 2020, 11, 649. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, W.C.; Arunagiri, V.; Funk, A.P.; Ginsburg, K.L.; Krychiw, J.K.; Limowski, A.R.; Olesnycky, O.S.; Stout, Z. The nature and treatment of pandemic-related psychological distress. J. Contemp. Psychother. 2020, 50, 251–263. [Google Scholar] [CrossRef]
- Bäuerle, A.; Graf, J.; Jansen, C.; Dörrie, N.; Junne, F.; Teufel, M.; Skoda, E.-M. An e-mental health intervention to support burdened people in times of the COVID-19 pandemic: CoPE It. J. Public Health 2020, 42, 647–648. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Schweda, A.; Weismüller, B.; Bäuerle, A.; Dörrie, N.; Musche, V.; Fink, M.; Kohler, H.; Teufel, M.; Skoda, E.-M. Phenotyping mental health: Age, community size, and depression differently modulate COVID-19-related fear and generalized anxiety. Compr. Psychiatry 2021, 104, 152218. [Google Scholar] [CrossRef]
| Without Surgery | With Surgery | ||||
|---|---|---|---|---|---|
| N | % | N | % | p-Value | |
| Sex | |||||
| Female | 99 | 86.8 | 124 | 87.3 | |
| Male | 15 | 13.2 | 16 | 11.3 | 0.821 |
| Age | |||||
| 18–24 years | 5 | 4.4 | 1 | 0.7 | |
| 25–34 years | 26 | 22.8 | 27 | 19 | |
| 35–44 years | 45 | 39.5 | 52 | 36.6 | |
| 45–54 years | 26 | 22.8 | 30 | 21.1 | |
| 55–64 years | 11 | 9.6 | 25 | 17.6 | |
| 65–74 years | 1 | 0.9 | 5 | 3.5 | |
| ≥75 years | 0 | 0 | 2 | 1.4 | 0.100 |
| Marital status | |||||
| Single | 24 | 21.1 | 30 | 21.1 | |
| Married | 61 | 53.5 | 70 | 49.3 | |
| In a relationship | 16 | 14 | 27 | 19 | |
| Divorced/separated | 12 | 10.5 | 8 | 5.6 | |
| Widowed | 1 | 0.9 | 4 | 2.8 | 0.371 |
| Educational level | |||||
| University education | 12 | 10.5 | 20 | 14.1 | |
| Higher education entrance qualification | 33 | 28.9 | 32 | 22.5 | |
| Higher secondary education | 42 | 36.8 | 63 | 44.4 | |
| Lower secondary education | 22 | 19.3 | 25 | 17.6 | 0.460 |
| Employment | |||||
| Employed | 63 | 55.3 | 98 | 69 | |
| Not employed | 37 | 32.5 | 44 | 31 | 0.402 |
| City size (Population) | |||||
| 100,000 residents | 65 | 57 | 85 | 59.9 | |
| 20,000 residents | 21 | 18.4 | 25 | 17.6 | |
| 5000 residents | 18 | 15.8 | 14 | 9.9 | |
| <5000 residents | 10 | 8.8 | 18 | 12.7 | 0.428 |
| Mental illness | |||||
| yes | 34 | 29.8 | 42 | 29.6 | |
| no | 80 | 70.2 | 100 | 70.4 | |
| 1.000 | |||||
| Somatic illness | |||||
| none | 15 | 13.2 | 29 | 20.4 | 0.172 |
| Cardiovascular disease | 11 | 9.6 | 6 | 4.2 | 0.271 |
| Diabetes mellitus | 23 | 20.2 | 28 | 19.7 | 1.000 |
| Chronic respiratory disease | 24 | 21.1 | 26 | 18.3 | 0.695 |
| Hypertension | 56 | 49.1 | 47 | 33.1 | 0.014 |
| Intermittent claudication | 1 | 0.9 | 3 | 2.1 | 0.776 |
| Sleep apnea | 21 | 18.4 | 25 | 17.6 | 0.996 |
| Lip-metabolic disorder | 12 | 10.5 | 14 | 9.9 | 1.000 |
| Articular gout | 11 | 9.6 | 13 | 3.2 | 1.000 |
| Hypothyroidism | 35 | 30.7 | 44 | 31 | 0.142 |
| Polycystic ovary syndrome | 8 | 7 | 11 | 7.7 | 1.000 |
| Arthropathy | 41 | 36 | 49 | 34.5 | 0.912 |
| other | 18 | 15.8 | 26 | 18.3 | 0.715 |
| Total | 114 | 100 | 142 | 100 | |
| Without Surgery | With Surgery | |
|---|---|---|
| N | 114 | 142 |
| Weight | 132.72 (31.57) | 101.43 (22.26) |
| Body Mass | 45.59 (10.49) | 35.49 (8.96) |
| COVID-19-related fear | 4.21 (1.95) | 4.14 (1.89) |
| Generalized anxiety (GAD-7) | 7.21 (5.19) | 6.37 (6.00) |
| Depression symptoms (PHQ-8) | 9.02 (5.19) | 8.00 (6.58) |
| Dysfunctional safety behavior | 3.27 (1.57) | 3.11 (1.61) |
| Dysfunctional COVID-19-specific eating behavior (DCSEB) | 14.69 (6.23) | 14.22 (7.50) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pfeiffer, C.; Schweda, A.; Schüren, L.C.; Niedergethmann, M.; Steinbach, J.; Rentrop, V.; Robitzsch, A.; Dörrie, N.; Bäuerle, A.; Teufel, M.; et al. Generalized Anxiety as a Risk Factor for Dysfunctional Eating Behavior after Obesity Surgery during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10890. https://doi.org/10.3390/ijerph182010890
Pfeiffer C, Schweda A, Schüren LC, Niedergethmann M, Steinbach J, Rentrop V, Robitzsch A, Dörrie N, Bäuerle A, Teufel M, et al. Generalized Anxiety as a Risk Factor for Dysfunctional Eating Behavior after Obesity Surgery during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(20):10890. https://doi.org/10.3390/ijerph182010890
Chicago/Turabian StylePfeiffer, Corinna, Adam Schweda, Lynik Chantal Schüren, Marco Niedergethmann, Jasmin Steinbach, Vanessa Rentrop, Anita Robitzsch, Nora Dörrie, Alexander Bäuerle, Martin Teufel, and et al. 2021. "Generalized Anxiety as a Risk Factor for Dysfunctional Eating Behavior after Obesity Surgery during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 20: 10890. https://doi.org/10.3390/ijerph182010890
APA StylePfeiffer, C., Schweda, A., Schüren, L. C., Niedergethmann, M., Steinbach, J., Rentrop, V., Robitzsch, A., Dörrie, N., Bäuerle, A., Teufel, M., Skoda, E.-M., & Weismüller, B. (2021). Generalized Anxiety as a Risk Factor for Dysfunctional Eating Behavior after Obesity Surgery during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(20), 10890. https://doi.org/10.3390/ijerph182010890







