Comparing HIV Post-Exposure Prophylaxis, Testing, and New Diagnoses in Two Australian Cities with Different Lockdown Measures during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
3. Results
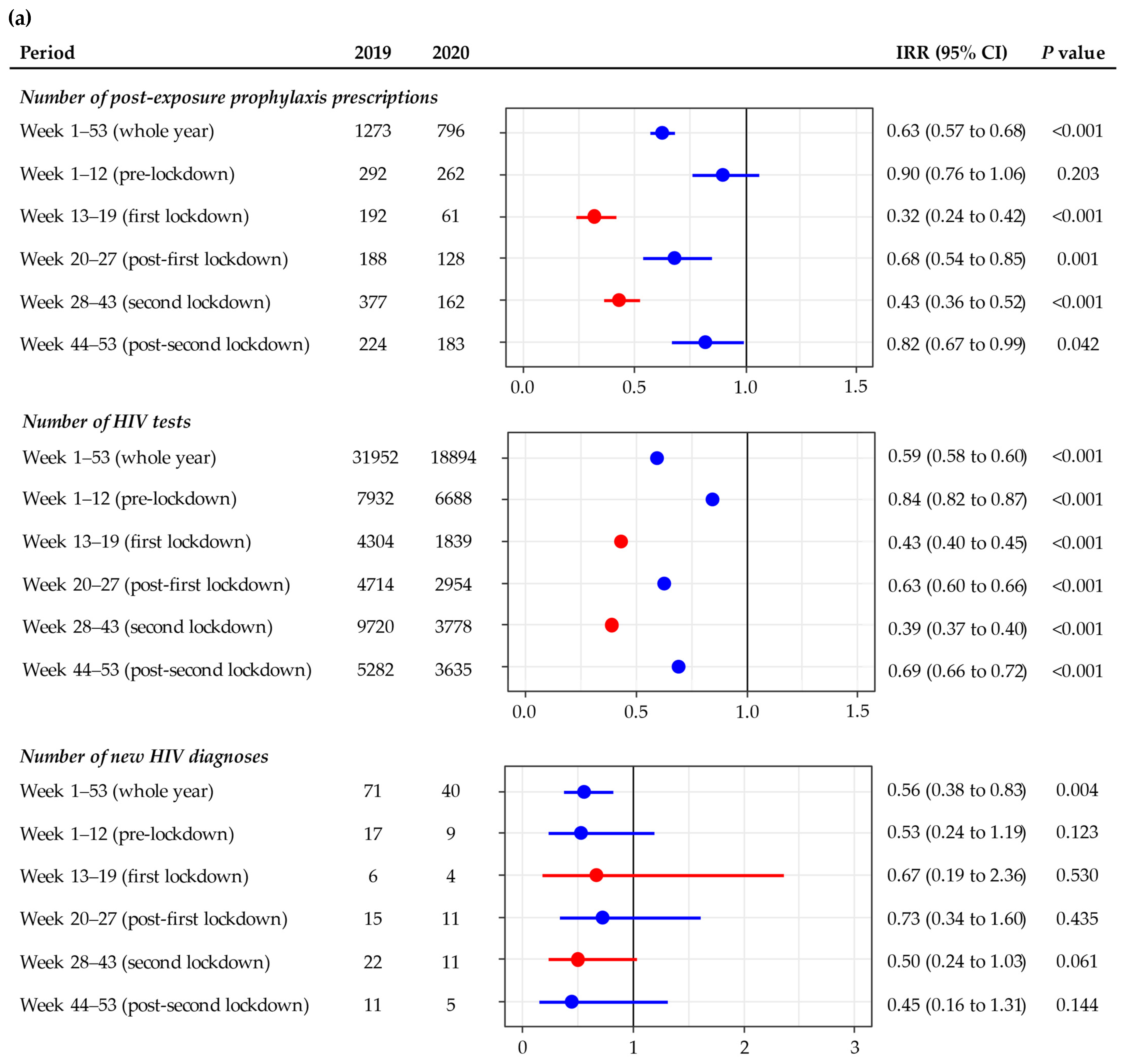
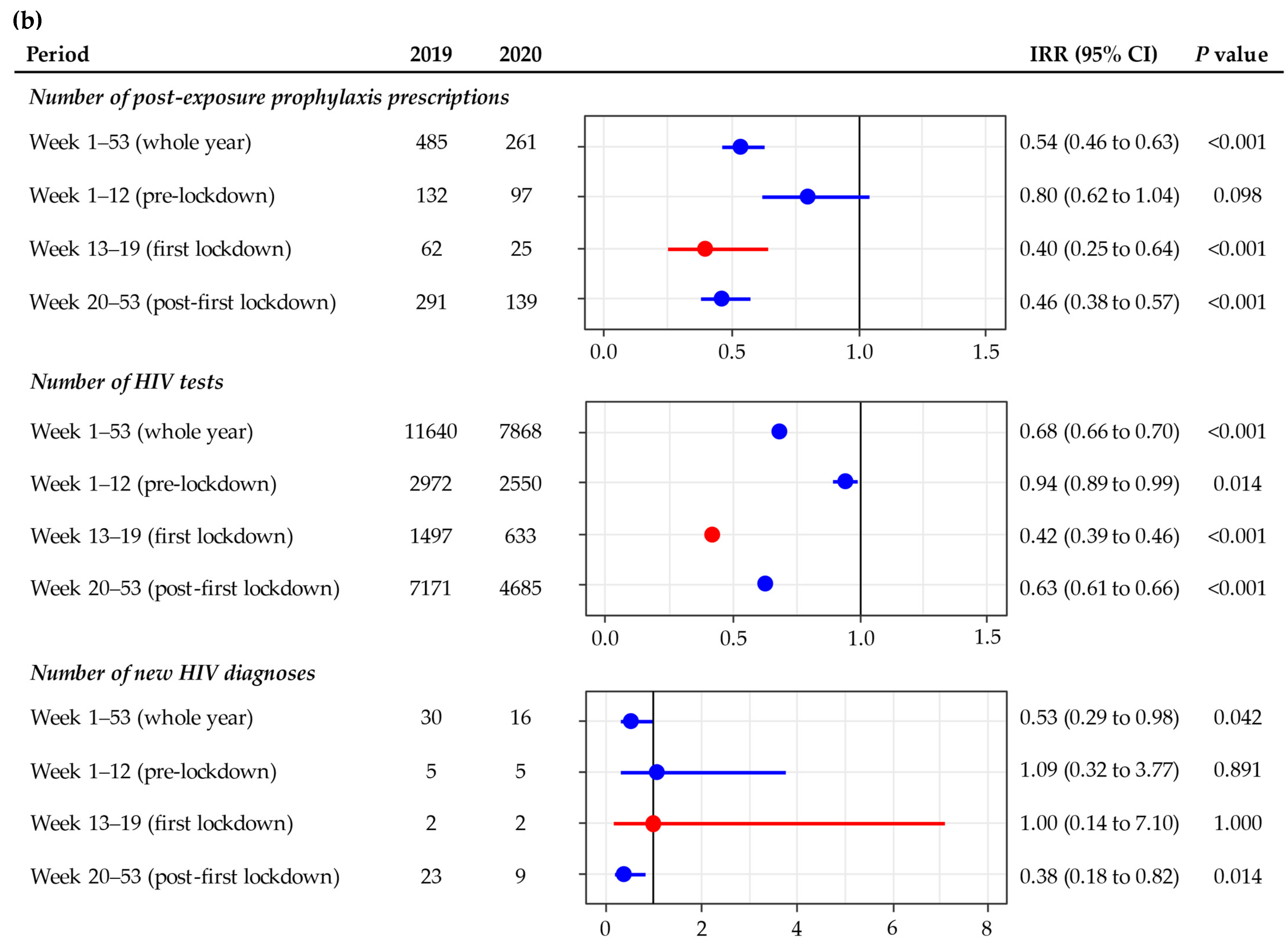
3.1. Melbourne
3.2. Sydney
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chow, E.P.F.; Hocking, J.S.; Ong, J.J.; Phillips, T.R.; Fairley, C.K. Sexually Transmitted Infection Diagnoses and Access to a Sexual Health Service Before and After the National Lockdown for COVID-19 in Melbourne, Australia. Open Forum. Infect. Dis. 2021, 8, ofaa536. [Google Scholar] [CrossRef]
- Coombe, J.; Kong, F.Y.S.; Bittleston, H.; Williams, H.; Tomnay, J.; Vaisey, A.; Malta, S.; Goller, J.L.; Temple-Smith, M.; Bourchier, L.; et al. Love during lockdown: Findings from an online survey examining the impact of COVID-19 on the sexual health of people living in Australia. Sex. Transm. Infect. 2021, 97, 357–362. [Google Scholar] [CrossRef]
- Delcea, C.; Chirilă, V.I.; Săuchea, A.M. Effects of COVID-19 on sexual life—A meta-analysis. Sexologies 2021, 30, e49–e54. [Google Scholar] [CrossRef]
- Pinto, C.N.; Niles, J.K.; Kaufman, H.W.; Marlowe, E.M.; Alagia, D.P.; Chi, G.; Van Der Pol, B. Impact of the COVID-19 Pandemic on Chlamydia and Gonorrhea Screening in the U.S. Am. J. Prev. Med. 2021, 61, 386–393. [Google Scholar] [CrossRef]
- Charles, H.; Ratna, N.; Thorn, L.; Sonubi, T.; Sun, S.; Mohammed, H.; Folkard, K.; Sinka, K. COVID-19 impact on bacterial sexually transmitted infections in England between 1 January 2019 and 31 December 2020. Sex. Transm. Infect. 2021. [Google Scholar] [CrossRef] [PubMed]
- Hammoud, M.A.; Maher, L.; Holt, M.; Degenhardt, L.; Jin, F.; Murphy, D.; Bavinton, B.; Grulich, A.; Lea, T.; Haire, B.; et al. Physical Distancing Due to COVID-19 Disrupts Sexual Behaviors Among Gay and Bisexual Men in Australia: Implications for Trends in HIV and Other Sexually Transmissible Infections. J. Acquir. Immune. Defic. Syndr. 2020, 85, 309–315. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 National Incident Room Surveillance Team. COVID-19, Australia: Epidemiology Report 9 (Reporting week to 23:59 AEDT 29 March 2020). Commun. Dis. Intell. 2020, 44. [Google Scholar] [CrossRef]
- Storen, R.; Corrigan, N. COVID-19: A Chronology of State and Territory Government Announcements (up until 30 June 2020). Available online: https://parlinfo.aph.gov.au/parlInfo/download/library/prspub/7614514/upload_binary/7614514.pdf (accessed on 1 October 2021).
- Lupton, D. Timeline of COVID-19 in Australia: The First Year. Available online: https://deborahalupton.medium.com/timeline-of-covid-19-in-australia-1f7df6ca5f23 (accessed on 4 October 2021).
- COVID-19 National Incident Room Surveillance Team. COVID-19, Australia: Epidemiology Report 22 (Fortnightly Reporting Period Ending 2 August 2020). Commun. Dis. Intell. 2020, 44. [Google Scholar] [CrossRef]
- Australian Government Department of Health Coronavirus (COVID-19). Advice for People with Chronic Health Conditions. Available online: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/advice-for-people-at-risk-of-coronavirus-covid-19/coronavirus-covid-19-advice-for-people-with-chronic-health-conditions (accessed on 1 October 2021).
- Victoria State Government Victorian Coronavirus (COVID-19) Data. Available online: https://www.dhhs.vic.gov.au/victorian-coronavirus-covid-19-data (accessed on 19 July 2021).
- New South Wales Government NSW COVID-19 Cases Data. Available online: https://data.nsw.gov.au/nsw-covid-19-data/cases (accessed on 19 July 2021).
- Sanchez-Rubio, J.; Velez-Diaz-Pallares, M.; Rodriguez Gonzalez, C.; Sanmartin Fenollera, P.; Garcia Yubero, C.; Garcia-Valdecasas, M.F. HIV postexposure prophylaxis during the COVID-19 pandemic: Experience from Madrid. Sex. Transm. Infect. 2021, 97, 100. [Google Scholar] [CrossRef]
- Junejo, M.; Girometti, N.; McOwan, A.; Whitlock, G.; Dean Street Collaborative, G. HIV postexposure prophylaxis during COVID-19. Lancet HIV 2020, 7, e460. [Google Scholar] [CrossRef]
- Maatouk, I.; Assi, M.; Jaspal, R. Emerging impact of the COVID-19 outbreak on sexual health in Lebanon. Sex. Transm. Infect. 2021, 97, 318. [Google Scholar] [CrossRef]
- The Global Fund to Fight AIDS Tuberculosis and Malaria. The impact of COVID-19 on HIV, TB and Malaria Services and Systems for Health: A Snapshot from 502 Health Facilities across Africa and Asia. Available online: https://www.theglobalfund.org/media/10776/covid-19_2020-disruption-impact_report_en.pdf (accessed on 21 July 2021).
- Ponticiello, M.; Mwanga-Amumpaire, J.; Tushemereirwe, P.; Nuwagaba, G.; King, R.; Sundararajan, R. “Everything is a Mess”: How COVID-19 is Impacting Engagement with HIV Testing Services in Rural Southwestern Uganda. AIDS Behav. 2020, 24, 3006–3009. [Google Scholar] [CrossRef]
- Chow, E.P.F.; Hocking, J.S.; Ong, J.J.; Phillips, T.R.; Schmidt, T.; Buchanan, A.; Rodriguez, E.; Maddaford, K.; Fairley, C.K. Brief Report: Changes in PrEP Use, Sexual Practice, and Use of Face Mask During Sex Among MSM During the Second Wave of COVID-19 in Melbourne, Australia. J. Acquir. Immune. Defic. Syndr. 2021, 86, 153–156. [Google Scholar] [CrossRef]
- Chow, E.P.F.; Hocking, J.S.; Ong, J.J.; Schmidt, T.; Buchanan, A.; Rodriguez, E.; Maddaford, K.; Patel, P.; Fairley, C.K. Changing the Use of HIV Pre-exposure Prophylaxis Among Men Who Have Sex With Men During the COVID-19 Pandemic in Melbourne, Australia. Open Forum. Infect. Dis. 2020, 7, ofaa275. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Disruption in HIV, Hepatitis and STI Services Due to COVID-19. Available online: https://www.who.int/docs/default-source/hiv-hq/disruption-hiv-hepatitis-sti-services-due-to-covid19.pdf?sfvrsn=5f78b742_6 (accessed on 21 July 2021).
- Nagendra, G.; Carnevale, C.; Neu, N.; Cohall, A.; Zucker, J. The Potential Impact and Availability of Sexual Health Services During the COVID-19 Pandemic. Sex. Transm. Dis. 2020, 47, 434–436. [Google Scholar] [CrossRef]
- The Lancet HIV. When pandemics collide. Lancet HIV 2020, 7, e301. [Google Scholar] [CrossRef]
- Luis, H.; Fridayantara, W.D.; Mahariski, P.; Wignall, F.S.; Irwanto, I.; Gedela, K. Evolving ART crisis for people living with HIV in Indonesia. Lancet HIV 2020, 7, e384–e385. [Google Scholar] [CrossRef]
- Phillips, T.R.; Fairley, C.K.; Donovan, B.; Ong, J.J.; McNulty, A.; Marshall, L.; Templeton, D.J.; Owen, L.; Ward, A.; Gunathilake, M.; et al. Sexual health service adaptations to the coronavirus disease 2019 (COVID-19) pandemic in Australia: A nationwide online survey. Aust. N. Z. J. Public Health 2021. [Google Scholar] [CrossRef]
- Witzel, T.C.; Eshun-Wilson, I.; Jamil, M.S.; Tilouche, N.; Figueroa, C.; Johnson, C.C.; Reid, D.; Baggaley, R.; Siegfried, N.; Burns, F.M.; et al. Comparing the effects of HIV self-testing to standard HIV testing for key populations: A systematic review and meta-analysis. BMC Med. 2020, 18, 381. [Google Scholar] [CrossRef]
- Ortblad, K.F.; Stekler, J.D. HIV self-testing: Finding its way in the prevention tool box. BMC Med. 2020, 18, 373. [Google Scholar] [CrossRef]
- Jiang, H.; Zhou, Y.; Tang, W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV 2020, 7, e308–e309. [Google Scholar] [CrossRef]
- Lagat, H.; Sharma, M.; Kariithi, E.; Otieno, G.; Katz, D.; Masyuko, S.; Mugambi, M.; Wamuti, B.; Weiner, B.; Farquhar, C. Impact of the COVID-19 Pandemic on HIV Testing and Assisted Partner Notification Services, Western Kenya. AIDS Behav. 2020, 24, 3010–3013. [Google Scholar] [CrossRef]
- Mhango, M.; Chitungo, I.; Dzinamarira, T. COVID-19 Lockdowns: Impact on Facility-Based HIV Testing and the Case for the Scaling Up of Home-Based Testing Services in Sub-Saharan Africa. AIDS Behav. 2020, 24, 3014–3016. [Google Scholar] [CrossRef]
- Jiang, H.; Xie, Y.; Xiong, Y.; Zhou, Y.; Lin, K.; Yan, Y.; Tucker, J.; Ong, J.J.; Wu, D.; Yang, F.; et al. HIV self-testing partially filled the HIV testing gap among men who have sex with men in China during the COVID-19 pandemic: Results from an online survey. J. Int. AIDS Soc. 2021, 24, e25737. [Google Scholar] [CrossRef]
- Odinga, M.M.; Kuria, S.; Muindi, O.; Mwakazi, P.; Njraini, M.; Melon, M.; Kombo, B.; Kaosa, S.; Kioko, J.; Musimbi, J.; et al. HIV testing amid COVID-19: Community efforts to reach men who have sex with men in three Kenyan counties. Gates Open Res. 2020, 4, 117. [Google Scholar] [CrossRef]
- Gunaratnam, P.; Heywood, A.E.; McGregor, S.; Jamil, M.S.; McManus, H.; Mao, L.; Lobo, R.; Brown, G.; Hellard, M.; Marukutira, T.; et al. HIV diagnoses in migrant populations in Australia-A changing epidemiology. PLoS ONE 2019, 14, e0212268. [Google Scholar] [CrossRef] [Green Version]
- Blackshaw, L.C.D.; Chow, E.P.F.; Varma, R.; Healey, L.; Templeton, D.J.; Basu, A.; Turner, D.; Medland, N.A.; Rix, S.; Fairley, C.K.; et al. Characteristics of recently arrived Asian men who have sex with men diagnosed with HIV through sexual health services in Melbourne and Sydney. Aust. N. Z. J. Public Health 2019, 43, 424–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medland, N.A.; Chow, E.P.F.; Read, T.H.R.; Ong, J.J.; Chen, M.; Denham, I.; Gunaratnum, P.; Fairley, C.K. Incident HIV infection has fallen rapidly in men who have sex with men in Melbourne, Australia (2013-2017) but not in the newly-arrived Asian-born. BMC Infect. Dis. 2018, 18, 410. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.P.F.; Medland, N.A.; Denham, I.; Wright, E.J.; Fairley, C.K. Decline in new HIV diagnoses among MSM in Melbourne. Lancet HIV 2018, 5, e479–e481. [Google Scholar] [CrossRef]
- Chow, E.P.F.; Ong, J.J.; Denham, I.; Fairley, C.K. HIV Testing and Diagnoses During the COVID-19 Pandemic in Melbourne, Australia. J. Acquir. Immune. Defic. Syndr. 2021, 86, e114–e115. [Google Scholar] [CrossRef] [PubMed]
- Farquharson, R.M.; Fairley, C.K.; Ong, J.J.; Phillips, T.R.; Chow, E.P.F. Time to healthcare-seeking following the onset of STI-associated symptoms during two waves of the COVID-19 pandemic in Melbourne, Australia. Sex. Transm. Infect. 2021. [Google Scholar] [CrossRef] [PubMed]
- Traeger, M.W.; Patel, P.; Guy, R.; Hellard, M.E.; Stoové, M.A.; Australian Collaboration for Coordinated Enhanced Sentinel Surveillance. Changes in HIV preexposure prophylaxis prescribing in Australian clinical services following COVID-19 restrictions. AIDS 2021, 35, 155–157. [Google Scholar] [CrossRef]
- Stanford, K.A.; McNulty, M.C.; Schmitt, J.R.; Eller, D.S.; Ridgway, J.P.; Beavis, K.V.; Pitrak, D.L. Incorporating HIV Screening With COVID-19 Testing in an Urban Emergency Department During the Pandemic. JAMA Intern. Med. 2021, 181, 1001–1003. [Google Scholar] [CrossRef] [PubMed]
- Jewell, B.L.; Mudimu, E.; Stover, J.; Ten Brink, D.; Phillips, A.N.; Smith, J.A.; Martin-Hughes, R.; Teng, Y.; Glaubius, R.; Mahiane, S.G.; et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: Results from multiple mathematical models. Lancet HIV 2020, 7, e629–e640. [Google Scholar] [CrossRef]
- Lesosky, M.; Myer, L. Modelling the impact of COVID-19 on HIV. Lancet HIV 2020, 7, e596–e598. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chow, E.P.F.; Ong, J.J.; Donovan, B.; Foster, R.; Phillips, T.R.; McNulty, A.; Fairley, C.K. Comparing HIV Post-Exposure Prophylaxis, Testing, and New Diagnoses in Two Australian Cities with Different Lockdown Measures during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10814. https://doi.org/10.3390/ijerph182010814
Chow EPF, Ong JJ, Donovan B, Foster R, Phillips TR, McNulty A, Fairley CK. Comparing HIV Post-Exposure Prophylaxis, Testing, and New Diagnoses in Two Australian Cities with Different Lockdown Measures during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(20):10814. https://doi.org/10.3390/ijerph182010814
Chicago/Turabian StyleChow, Eric P. F., Jason J. Ong, Basil Donovan, Rosalind Foster, Tiffany R. Phillips, Anna McNulty, and Christopher K. Fairley. 2021. "Comparing HIV Post-Exposure Prophylaxis, Testing, and New Diagnoses in Two Australian Cities with Different Lockdown Measures during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 20: 10814. https://doi.org/10.3390/ijerph182010814
APA StyleChow, E. P. F., Ong, J. J., Donovan, B., Foster, R., Phillips, T. R., McNulty, A., & Fairley, C. K. (2021). Comparing HIV Post-Exposure Prophylaxis, Testing, and New Diagnoses in Two Australian Cities with Different Lockdown Measures during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(20), 10814. https://doi.org/10.3390/ijerph182010814





