Performing Simulated Basic Life Support without Seeing: Blind vs. Blindfolded People
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants and Selection Criteria
2.3. Intervention
2.4. Variables
2.5. Statistics
2.6. Ethics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.P.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef]
- Requena-Morales, R.; Palazón-Bru, A.; Rizo-Baeza, M.M.; Adsuar-Quesada, J.M.; Gil-Guillén, V.F.; Cortés-Castell, E. Mortality after out-of-hospital cardiac arrest in a Spanish Region. PLoS ONE 2017, 12, e0175818. [Google Scholar] [CrossRef]
- Perkins, G.D.; Handley, A.J.; Koster, R.W.; Castrén, M.; Smyth, M.A.; Olasveengen, T.; Monsieurs, K.G.; Raffay, V.; Gräsner, J.T.; Wenzel, V.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation 2015, 95, 81–99. [Google Scholar] [CrossRef] [Green Version]
- Greif, R.; Lockey, A.S.; Conaghan, P.; Lippert, A.; De Vries, W.; Monsieurs, K.G.; Ballance, J.H.; Barelli, A.; Biarent, D.; Bossaert, L.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 10. Education and implementation of resuscitation. Resuscitation 2015, 95, 288–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villalobos, F.; Del Pozo, A.; Rey-Reñones, C.; Granado-Font, E.; Sabaté-Lissner, D.; Poblet-Calaf, C.; Basora, J.; Castro, A.; Flores-Mateo, G. Lay People Training in CPR and in the Use of an Automated External Defibrillator, and Its Social Impact: A Community Health Study. Int. J. Environ. Res. Public Health 2019, 16, 2870. [Google Scholar] [CrossRef] [Green Version]
- Holmberg, M.J.; Vognsen, M.; Andersen, M.S.; Donnino, M.W.; Andersen, L.W. Bystander automated external defibrillator use and clinical outcomes after out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation 2017, 120, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Wissenberg, M.; Lippert, F.K.; Folke, F.; Weeke, P.; Hansen, C.M.; Christensen, E.F.; Jans, H.; Hansen, P.A.; Lang-Jensen, T.; Olesen, J.B.; et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA 2013, 310, 1377–1384. [Google Scholar] [CrossRef] [Green Version]
- González-Salvado, V.; Rodríguez-Ruiz, E.; Abelairas-Gómez, C.; Ruano-Raviña, A.; Peña-Gil, C.; González-Juanatey, J.R.; Rodríguez-Núñez, A. Training adult laypeople in basic life support. A systematic review. Rev. Esp Cardiol 2020, 73, 53–68. [Google Scholar] [CrossRef]
- Martínez-Isasi, S.; Abelairas-Gómez, C.; Fernández-Méndez, F.; Barcala-Furelos, R.; Jorge-Soto, C.; Gómez-Gónzalez, C.; Rodríguez-Núñez, A. Is it necessary to see to save a life? Pilot study of basic CPR training for blind people. Resuscitation 2019, 134, 165–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodríguez-Núñez, A.; Regueiro-García, A.; Jorge-Soto, C.; Cañas-González, J.; Leboráns-Iglesias, P.; García-Crespo, O.; Barcala-Furelos, R. Quality of chest compressions by Down syndrome people: A pilot trial. Resuscitation 2015, 89, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Jorge-Soto, C.; Barcala-Furelos, R.; Gómez-González, C.; Leborans-Iglesias, P.; Campos-Varela, I.; Rodríguez-Núñez, A. Brief training in automated external defibrillation use for persons with down syndrome. Resuscitation 2017, 113, e5–e6. [Google Scholar] [CrossRef] [Green Version]
- WHO. Blindness and Vision Impairment. Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 14 September 2021).
- ONCE. Conoce los datos anuales de nuestros afiliados-Web ONCE. Available online: https://www.once.es/dejanos-ayudarte/afiliacion/datos-de-afiliados-a-la-once (accessed on 19 May 2020).
- Oulego-Erroz, I.; Busto-Cuiñas, M.; García-Sánchez, N.; Rodríguez-Blanco, S.; Rodríguez-Núñez, A. A popular song improves CPR compression rate and skill retention by schoolchildren: A manikin trial. Resuscitation 2011, 82, 499–500. [Google Scholar] [CrossRef] [PubMed]
- Bjørnshave, K.; Krogh, L.Q.; Hansen, S.B.; Nebsbjerg, M.A.; Thim, T.; Løfgren, B. Teaching basic life support with an automated external defibrillator using the two-stage or the four-stage teaching technique. Eur. J. Emerg. Med. 2018, 25, 18–24. [Google Scholar] [CrossRef]
- Cartledge, S.; Finn, J.; Bray, J.E.; Case, R.; Barker, L.; Missen, D.; Shaw, J.; Stub, D. Incorporating cardiopulmonary resuscitation training into a cardiac rehabilitation programme: A feasibility study. Eur. J. Cardiovasc. Nurs. J. 2018, 17, 148–158. [Google Scholar] [CrossRef]
- Lee, J.H.; Cho, Y.; Kang, K.H.; Cho, G.C.; Song, K.J.; Lee, C.H. The Effect of the Duration of Basic Life Support Training on the Learners’ Cardiopulmonary and Automated External Defibrillator Skills. BioMed Res. Int. 2016, 2016, 2420568. [Google Scholar] [CrossRef] [Green Version]
- Hughes, P.G.; Hughes, K.E.; Ahmed, R.A. Setup and Execution of the Blindfolded Code Training Exercise. JOVE 2019, 145, e59248. [Google Scholar] [CrossRef]
- Baldi, E.; Cornara, S.; Contri, E.; Epis, F.; Fina, D.; Zelaschi, B.; Dossena, C.; Fichtner, F.; Tonani, M.; Di Maggio, M.; et al. Real-time visual feedback during training improves laypersons’ CPR quality: A randomized controlled manikin study. CJEM 2017, 19, 480–487. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, R.; Hughes, K.; Hughes, P. The blindfolded code training exercise. Clin. Teach. 2018, 15, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Pichel López, M.; Martínez-Isasi, S.; Barcala-Furelos, R.; Fernández-Méndez, F.; Vázquez Santamariña, D.; Sánchez-Santos, L.; Rodríguez-Nuñez, A. A first step to teaching basic life support in schools: Training the teachers. An. Pediatr. 2018, 89, 265–271. [Google Scholar] [CrossRef] [PubMed]
- González-Salvado, V.; Abelairas-Gómez, C.; Peña-Gil, C.; Neiro-Rey, C.; Barcala-Furelos, R.; González-Juanatey, J.R.; Rodríguez-Núñez, A. A community intervention study on patients’ resuscitation and defibrillation quality after embedded training in a cardiac rehabilitation program. Health Educ. Res. 2019, 34, 289–299. [Google Scholar] [CrossRef]
- González-Salvado, V.; Abelairas-Gómez, C.; Gude, F.; Peña-Gil, C.; Neiro-Rey, C.; González-Juanatey, J.R.; Rodriguez-Nunez, A. Targeting relatives: Impact of a cardiac rehabilitation programme including basic life support training on their skills and attitudes. Eur. J. Prev. Cardiol. 2019, 26, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Fungueiriño-Suárez, R.; Barcala-Furelos, R.; González-Fermoso, M.; Martínez-Isasi, S.; Fernández-Méndez, F.; González-Salvado, V.; Navarro-Patón, R.; Rodríguez-Núñez, A. Coastal Fishermen as Lifesavers While Sailing at High Speed: A Crossover Study. BioMed Res. Int. 2018, 2018, 2747046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Méndez-Martínez, C.; Martínez-Isasi, S.; García-Suárez, M.; Peña-Rodríguez, M.A.; Gómez-Salgado, J.; Fernández-García, D. Acquisition of Knowledge and Practical Skills after a Brief Course of BLS-AED in First-Year Students in Nursing and Physiotherapy at a Spanish University. Int. J. Environ. Res. Public Health 2019, 16, 766. [Google Scholar] [CrossRef] [Green Version]
- Battal, C.; Occelli, V.; Bertonati, G.; Falagiarda, F.; Collignon, O. General Enhancement of Spatial Hearing in Congenitally Blind People. Psychol. Sci. 2020, 31, 1129–1139. [Google Scholar] [CrossRef]
- Stronks, H.C.; Nau, A.C.; Ibbotson, M.R.; Barnes, N. The role of visual deprivation and experience on the performance of sensory substitution devices. Brain Res. 2015, 1624, 140–152. [Google Scholar] [CrossRef] [PubMed]
- Arnaud, L.; Gracco, V.; Ménard, L. Enhanced perception of pitch changes in speech and music in early blind adults. Neuropsychologia 2018, 117, 261–270. [Google Scholar] [CrossRef]
- Anderson, R.; Sebaldt, A.; Lin, Y.; Cheng, A. Optimal training frequency for acquisition and retention of high-quality CPR skills: A randomized trial. Resuscitation 2019, 135, 153–161. [Google Scholar] [CrossRef] [PubMed]


| Variables | Blind | Blindfolded | p |
|---|---|---|---|
| Global QCPR (%) | 43.9 (38.1) | 45.3 (31.1) | 0.721 |
| Time to start CC (seconds) | 35.77 (12.6) | 36.5 (14.4) | 0.844 |
| Time to discharge (seconds) | 66.0 (27.0) | 86.0 (24.9) | 0.004 |
| Compression time (%) | 99,4 (1.2) | 99.4 (1.4) | 1 |
| CC with adequate hand position (%) | 93.1 (19.9) | 88.6 (30.0) | 0.626 |
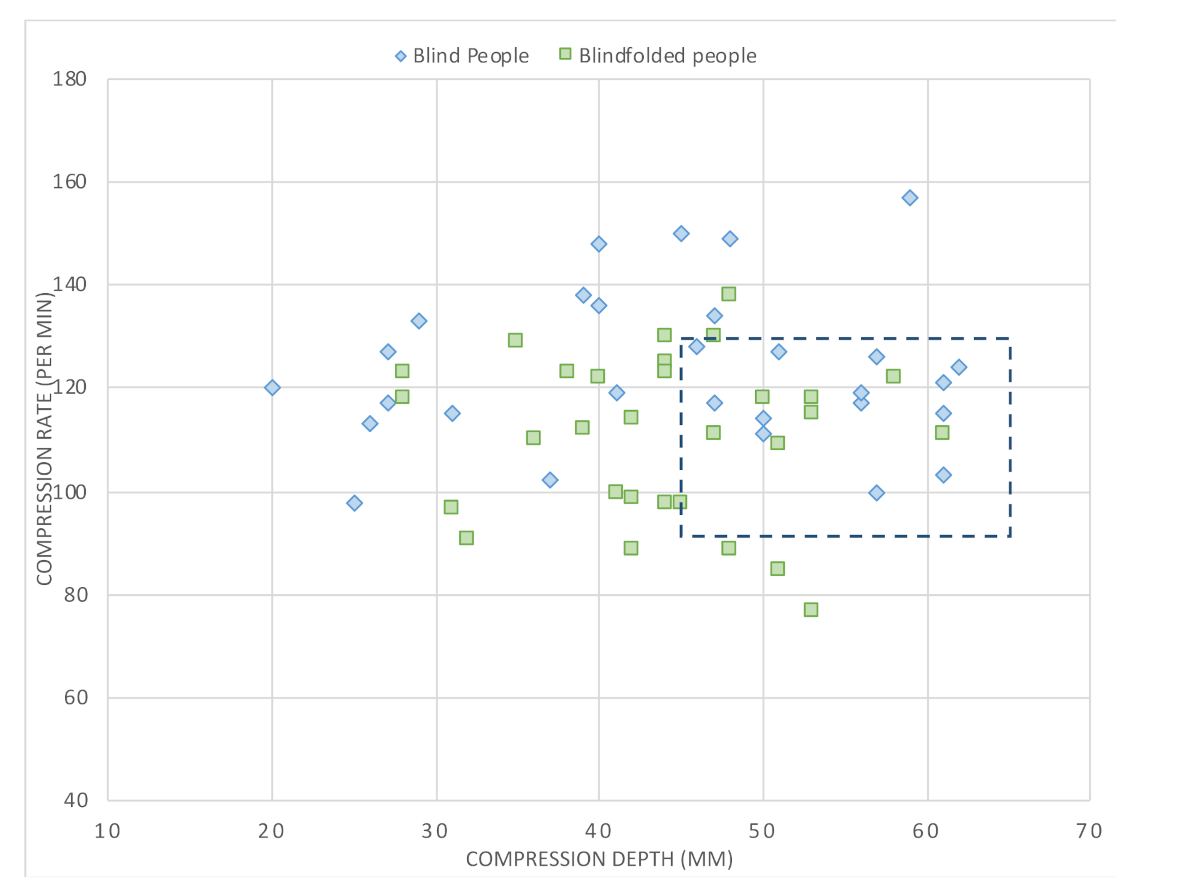
| Mean compression depth (mm) | 44.7 (12.7) | 43.8 (7.3) | 0.761 |
| CC with full chest recoil (%) | 69.8 (36.6) | 65.1 (36.5) | 0.721 |
| Correct CC by depth (%) | 32.3 (38.0) | 29.9 (35.7) | 0.939 |
| Correct CC by rate (%) | 39.3 (38.0) | 43.7 (37.0) | 0.357 |
| Mean compression rate (comp/min) | 123.4 (15.2) | 110.8 (15.3) | 0.002 |
| Variables | BP *,a | BFP *,a | Teachers [15] a | Cardiac Patients [16] b | Participants Free Course [17] | Relatives [18] b | Fisherman [19] a | Nurse Students [20] a |
|---|---|---|---|---|---|---|---|---|
| Global QCPR (%) | 43.9 (38.1) | 45.3 (31.1) | 70.2 (31.1) | 86 (71–92) | 69 (20.5–89) | 43 (10) | 55.2 (24.9) | |
| CC time (%) | 99.4 (1.2) | 99.4 (1.4) | 98.8 (8.0) | 74.7 (7.6) | ||||
| CC with adequate hand positions (%) | 93.1 (19.9) | 88.6 (30.0) | 97.7 (11.9) | 100 (100–100) | 99.3 | 100 (100–100) | 98.2 (13.0) | |
| Mean CC depth (mm) | 44.7 (12.7) | 43.8 (7.3) | 48.21 (9.2) | 56 (50–61) | 46 (41–56) | 56.5 (5) | 44.2 (10.7) | |
| CC with full chest recoil (%) | 69.8 (36.6) | 65.1 (36.5) | 78.7 (29.7) | 73 (25–98) | 88.8 | 91 (45–99.5) | 115 (16) | 79.1 (26.9) |
| Correct CC by Depth (%) | 32.3 (38.0) | 29.9 (35.7) | 46.9 (38.8) | 39 (7–75) | 75.7 | 38 (3–64.5) | 32.6 (39.7) | |
| Correct CC by rate (%) | 39.3 (38.0) | 43.7 (37.0) | 64.2 (36.9) | 55 (7–88) | 18 (0.5–80.5) | 50.4 (35.9) | ||
| Mean compression rate (comp/min) | 123.4 (15.2) | 110.8 (15.3) | 109.7 (14.3) | 106 (93–116) | 92.5 | 106 (89–123) | 113.1 (13.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Isasi, S.; Jorge-Soto, C.; Barcala-Furelos, R.; Abelairas-Gómez, C.; Carballo-Fazanes, A.; Fernández-Méndez, F.; Gómez-González, C.; Nadkarni, V.M.; Rodríguez-Núñez, A. Performing Simulated Basic Life Support without Seeing: Blind vs. Blindfolded People. Int. J. Environ. Res. Public Health 2021, 18, 10724. https://doi.org/10.3390/ijerph182010724
Martínez-Isasi S, Jorge-Soto C, Barcala-Furelos R, Abelairas-Gómez C, Carballo-Fazanes A, Fernández-Méndez F, Gómez-González C, Nadkarni VM, Rodríguez-Núñez A. Performing Simulated Basic Life Support without Seeing: Blind vs. Blindfolded People. International Journal of Environmental Research and Public Health. 2021; 18(20):10724. https://doi.org/10.3390/ijerph182010724
Chicago/Turabian StyleMartínez-Isasi, Santiago, Cristina Jorge-Soto, Roberto Barcala-Furelos, Cristian Abelairas-Gómez, Aida Carballo-Fazanes, Felipe Fernández-Méndez, Candela Gómez-González, Vinay M. Nadkarni, and Antonio Rodríguez-Núñez. 2021. "Performing Simulated Basic Life Support without Seeing: Blind vs. Blindfolded People" International Journal of Environmental Research and Public Health 18, no. 20: 10724. https://doi.org/10.3390/ijerph182010724
APA StyleMartínez-Isasi, S., Jorge-Soto, C., Barcala-Furelos, R., Abelairas-Gómez, C., Carballo-Fazanes, A., Fernández-Méndez, F., Gómez-González, C., Nadkarni, V. M., & Rodríguez-Núñez, A. (2021). Performing Simulated Basic Life Support without Seeing: Blind vs. Blindfolded People. International Journal of Environmental Research and Public Health, 18(20), 10724. https://doi.org/10.3390/ijerph182010724







