Utilisation of Skilled Birth Attendant in Low- and Middle-Income Countries: Trajectories and Key Sociodemographic Factors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Samples
2.3. Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- AbouZahr, C. Safe Motherhood: A brief history of the global movement 1947–2002. Br. Med. Bull. 2003, 67, 13–25. [Google Scholar] [CrossRef] [Green Version]
- WHO. Trends in Maternal Mortality: 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division; World Health Organization: Geneva, Switzerland, 2019; p. 104. ISBN 978-92-4-151648-8. [Google Scholar]
- Ronsmans, C.; Graham, W.J. Lancet Maternal Survival Series steering group, Maternal mortality: Who, when, where, and why. Lancet 2006, 368, 1189–1200. [Google Scholar] [CrossRef]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015. [Google Scholar]
- Banke-Thomas, O.E.; Banke-Thomas, A.E.; Ameh, C.A. Factors influencing utilisation of maternal health services by adolescent mothers in Low-and middle-income countries: A systematic review. Bio.-Med. Cent. Pregnancy Childbirth 2017, 17, 65. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Database on Skilled Birth Attendant at Delivery. Available online: http://www.who.int/reprodutive-health/global_monitoring/data.htm (accessed on 13 April 2020).
- Yaya, S.; Bishwajit, G.; Ekholuenetale, M. Factors associated with the utilization of institutional delivery services in Bangladesh. PLoS ONE 2017, 12, e0171573. [Google Scholar] [CrossRef] [Green Version]
- Singh, A.; Kumar, A.; Pranjali, P. Utilization of maternal healthcare among adolescent mothers in urban India: Evidence from DLHS-3. PeerJ 2014, 2, e592. [Google Scholar] [CrossRef] [Green Version]
- Santhya, K.; Jejeebhoy, S.; Ghosh, S. Early Marriage and Sexual and Reproductive Health Risks: Experiences of Young Women and Men in Andhra Pradesh and Madhya Pradesh, India; Population Council: New Delhi, India, 2008. [Google Scholar]
- Bloom, S.S.; Wypij, D.; Das Gupta, M. Dimensions of women’s autonomy and the influence on maternal health care utilization in a north Indian city. Demography 2001, 38, 67–78. [Google Scholar] [CrossRef]
- Ghosh, D. Effect of mothers’ exposure to electronic mass media on knowledge and use of prenatal care services: Comparative analysis of Indian states. Prof. Geogr. 2006, 58, 278–293. [Google Scholar] [CrossRef]
- Singh, P.K.; Kumar, C.; Rai, R.K.; Singh, L. Factors associated with maternal healthcare services utilization in nine high focus states in India: A multilevel analysis based on 14,385 communities in 292 districts. Health Policy Plan. 2014, 29, 542–559. [Google Scholar] [CrossRef] [Green Version]
- Magadi, M.A.; Madise, N.J.; Rodrigues, R.N. Frequency and timing of antenatal care in Kenya: Explaining the variations between women of different communities. Soc. Sci. Med. 2000, 51, 551–561. [Google Scholar] [CrossRef]
- Habibov, N.N. On the socio-economic determinants of antenatal care utilization in Azerbaijan: Evidence and policy implications for reforms. Health Econ. Policy Law 2011, 6, 175–203. [Google Scholar] [CrossRef]
- Gage, A.J. Barriers to the utilization of maternal health care in rural Mali. Soc. Sci. Med. 2007, 65, 1666–1682. [Google Scholar] [CrossRef]
- Gage, A.J.; Calixte, G.M. Effects of the physical accessibility of maternal health services on their use in rural Haiti. Popul. Stud. 2006, 60, 271–288. [Google Scholar] [CrossRef]
- Iacoella, F.; Tirivayi, N. Determinants of maternal healthcare utilization among married adolescents: Evidence from 13 Sub-Saharan African countries. Public Health 2019, 177, 1–9. [Google Scholar] [CrossRef]
- Huda, T.M.; Chowdhury, M.; El Arifeen, S.; Dibley, M.J. Individual and community level factors associated with health facility delivery: A cross sectional multilevel analysis in Bangladesh. PLoS ONE 2019, 14, e0211113. [Google Scholar] [CrossRef]
- Woldemicael, G.; Tenkorang, E.Y. Women’s Autonomy and Maternal Health-Seeking Behavior in Ethiopia. Matern Child Health J. 2010, 14, 988–998. [Google Scholar] [CrossRef]
- Tsawe, M.; Sathiya Susuman, A. Factors associated with the upsurge in the use of delivery care services in Sierra Leone. Public Health 2020, 180, 74–81. [Google Scholar] [CrossRef]
- Say, L.; Raine, R. A systematic review of inequalities in the use of maternal health care in developing countries: Examining the scale of the problem and the importance of context. Bull. World Health Organ. 2007, 85, 812–819. [Google Scholar] [CrossRef]
- Osorio, A.M.; Tovar, L.M.; Rathmann, K. Individual and local level factors and antenatal care use in Colombia: A multilevel analysis. Cad. Saude Publica 2014, 30, 1079–1092. [Google Scholar] [CrossRef]
- United Nations. Household surveys in developing and transition countries. In Studies in Methods Series F.; United Nations: New York, NY, USA, 2005; Volume 96. [Google Scholar]
- ICF DHS Program Dataset Types. Available online: https://dhsprogram.com/data/Dataset-Types.cfm (accessed on 13 April 2020).
- Kishor, S.; Sybaiya, L. Understanding Women’s Empowerment: A Comparative Analysis of Demographic and Health Surveys (DHS) Data; Macro International Inc.: Calverton, MD, USA, 2008. [Google Scholar]
- National Population and Family Planning Board (BKKBN); Statistics Indonesia (BPS); Ministry of Health (Kemenkes); ICF. Indonesia Demographic and Health Survey 2017; BKKBN, BPS, Kemenkes, and ICF: Jakarta, Indonesia, 2019. [Google Scholar]
- National Population Commission. Nigeria Demographic and Health Survey 2013; National Population Commission (NCP) [Nigeria] and ICF International: Abuja, Nigeria; Rockville, MD, USA, 2014. [Google Scholar]
- Magadi, M.A.; Zulu, E.M.; Brockerhoff, M. The inequality of maternal health care in urban sub-Saharan Africa in the 1990s. Popul. Stud. 2003, 57, 347–366. [Google Scholar] [CrossRef]
- Gabrysch, S.; Campbell, O.M.R. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 2009, 9, 34. [Google Scholar] [CrossRef] [Green Version]
- Croft, T.N.; Marshall, A.M.J.; Allen, C.K.; et al. Guide to DHS Statistics DHS-7. In The Demographic and Health Surveys Program; ICF: Rockville, MD, USA, 2018; Available online: https://www.dhsprogram.com/pubs/pdf/DHSG1/Guide_to_DHS_Statistics_DHS-7.pdf (accessed on 13 April 2020).
- Bhowmik, J.; Biswas, R.K.; Ananna, N. Women’s education and coverage of skilled birth attendance: An assessment of Sustainable Development Goal 3.1 in the South and Southeast Asian Region. PLoS ONE 2020, 15, e0231489. [Google Scholar] [CrossRef] [Green Version]
- Agresti, A.; Kateri, M. Categorical Data Analysis. In International Encyclopedia of Statistical Science; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2001; pp. 206–208. [Google Scholar]
- Mehata, S.; Paude, Y.R.; Dariang, M.; Aryal, K.K.; Lal, B.K.; Khanal, M.N.; Thomas, D. Trends and Inequalities in Use of Maternal Health Care Services in Nepal: Strategy in the Search for Improvements. BioMed Res. Int. 2017, 2017, 11. [Google Scholar] [CrossRef] [Green Version]
- Ronsmans, C.; Etard, J.F.; Walraven, G.; Hoj, L.; Dumont, A.; de Bernis, L.; Kodio, B. Maternal mortality and access to obstetric services in West Africa. Trop. Med. Int. Health 2003, 8, 940–948. [Google Scholar] [CrossRef]
- Rai, R.K.; Singh, P.K.; Singh, L. Utilization of maternal health care services among married adolescent women: Insights from the Nigeria Demographic and Health Survey. Womens Heatlh Issues 2008, 22, e407–e414. [Google Scholar] [CrossRef]
- Singh, P.K.; Rai, R.K.; Alagarajan, M.; Singh, L. Determinants of maternity care services utilization among married adolescents in rural India. PLoS ONE 2012, 7, e31666. [Google Scholar] [CrossRef] [Green Version]
- Obokoh, A. Examing Nigeria’s Healthcare Challenges. Available online: https://businessday.ng/why-nigeria-is-broke/article/examining-nigerias-healthcare-challenges/ (accessed on 1 November 2020).
- Rai, R.K.; Singh, P.K.; Singh, L.; Kumar, C. Individual characteristics and use of maternal and child health services by adolescent mothers in Niger. Matern. Child Health J. 2014, 18, 592–603. [Google Scholar] [CrossRef]
- Khanal, V.; Adhikari, M.; Karkee, R.; Gavidia, T. Factors associated with the utilisation of postnatal care services among the mothers of Nepal: Analysis of Nepal demographic and health survey 2011. BMC Womens Health 2014, 14, 19. [Google Scholar] [CrossRef] [Green Version]
- Valente, T.W.; Poppe, P.R.; Merritt, A.P. Mass-media-generated interpersonal communication as sources of information about family planning. J. Health Commun. 1996, 1, 247–265. [Google Scholar] [CrossRef]
- Tiruneh, F.N.; Chuang, K.Y.; Chuang, Y.C. Women’s autonomy and maternal healthcare service utilization in Ethiopia. BMC Health Serv. Res. 2017, 17, 718. [Google Scholar] [CrossRef] [Green Version]
| Variables | Indonesia n (%) | Nigeria n (%) |
|---|---|---|
| Year of survey | ||
| Period 1 (2002–2003) | 12,760 (22.5) | 3911 (6.1) |
| Period 2 (2007–2008) | 14,043 (24.8) | 17,635 (27.6) |
| Period 3 (2012–2013) | 14,782 (26.1) | 20,467 (32) |
| Period 4 (2017–2018) | 15,021 (26.5) | 21,911 (34.3) |
| Age | ||
| 15 to 29 | 28,384 (50.1) | 33,331 (52.1) |
| 30 to 49 | 28,222 (49.9) | 30,594 (47.9) |
| Educational attainment of husband/partner | ||
| Primary or lower | 21,215 (37.9) | 34,091 (56.1) |
| Secondary or higher | 34,784 (62.1) | 26,717 (43.9) |
| Has a say in household decision making | ||
| No | 15,356 (27.5) | 42,424 (70) |
| Yes | 40,426 (72.5) | 18,197 (30) |
| Educational attainment of participant | ||
| Primary or lower | 22,122 (39.1) | 41,676 (65.2) |
| Secondary or higher | 34,484 (60.9) | 22,249 (34.8) |
| Exposure to newspaper, radio and television is at least once a week | ||
| No | 8514 (15.1) | 33,486 (52.6) |
| Yes | 48,014 (84.9) | 30,131 (47.4) |
| Birth interval between most recent and preceding birth less than 24 months | ||
| No | 33,115 (90.0) | 41,970 (79.9) |
| Yes | 3672 (10.0) | 10,555 (20.1) |
| First or second order birth | ||
| No | 19,280 (34.1) | 41,854 (65.5) |
| Yes | 37,327 (65.9) | 22,071 (34.5) |
| Received Antenatal care at least once during pregnancy | ||
| No | 2900 (5.1) | 24,133 (37.9) |
| Yes | 53,569 (94.9) | 39,532 (62.1) |
| Wealth Index (Combined) | ||
| Poor/Poorer | 23,054 (40.7) | 28,541 (44.6) |
| Middle/Upper | 33,553 (59.3) | 35,384 (55.4) |
| Place of residence | ||
| Rural | 30,106 (53.2) | 41,459 (64.9) |
| Urban | 26,501 (46.8) | 22,465 (35.1) |
| Can read part or whole sentences | ||
| No | 2849 (5.1) | 37,023 (58.3) |
| Yes | 53,504 (94.9) | 26,517 (41.7) |
| Had Skilled birth attendant at most recent live birth | ||
| No | 11,207 (19.8) | 36,964 (58.0) |
| Yes | 45,273 (80.2) | 26,760 (42.0) |
| Perception of the distance to healthcare facility | ||
| Small or no problem | 49,270 (87.2) | 43,390 (68.1) |
| Big problem | 7249 (12.8) | 20,365 (31.9) |
| Geographic Quartiles (based on 2007/2008 SBA ratings) | ||
| Regional Quartile 1 | 8064 (14.3) | 26,580 (41.6) |
| Regional Quartile 2 | 18,421 (32.6) | 12,351 (19.3) |
| Regional Quartile 3 | 20,322 (35.9) | 12,497 (19.5) |
| Regional Quartile 4 | 9765 (17.3) | 12,496 (19.5) |
| Skilled Birth Attendance | ||||||
|---|---|---|---|---|---|---|
| Indonesia | Nigeria | |||||
| No (%) | Yes (%) | p-Value | No (%) | Yes (%) | p-Value | |
| Year of survey | ||||||
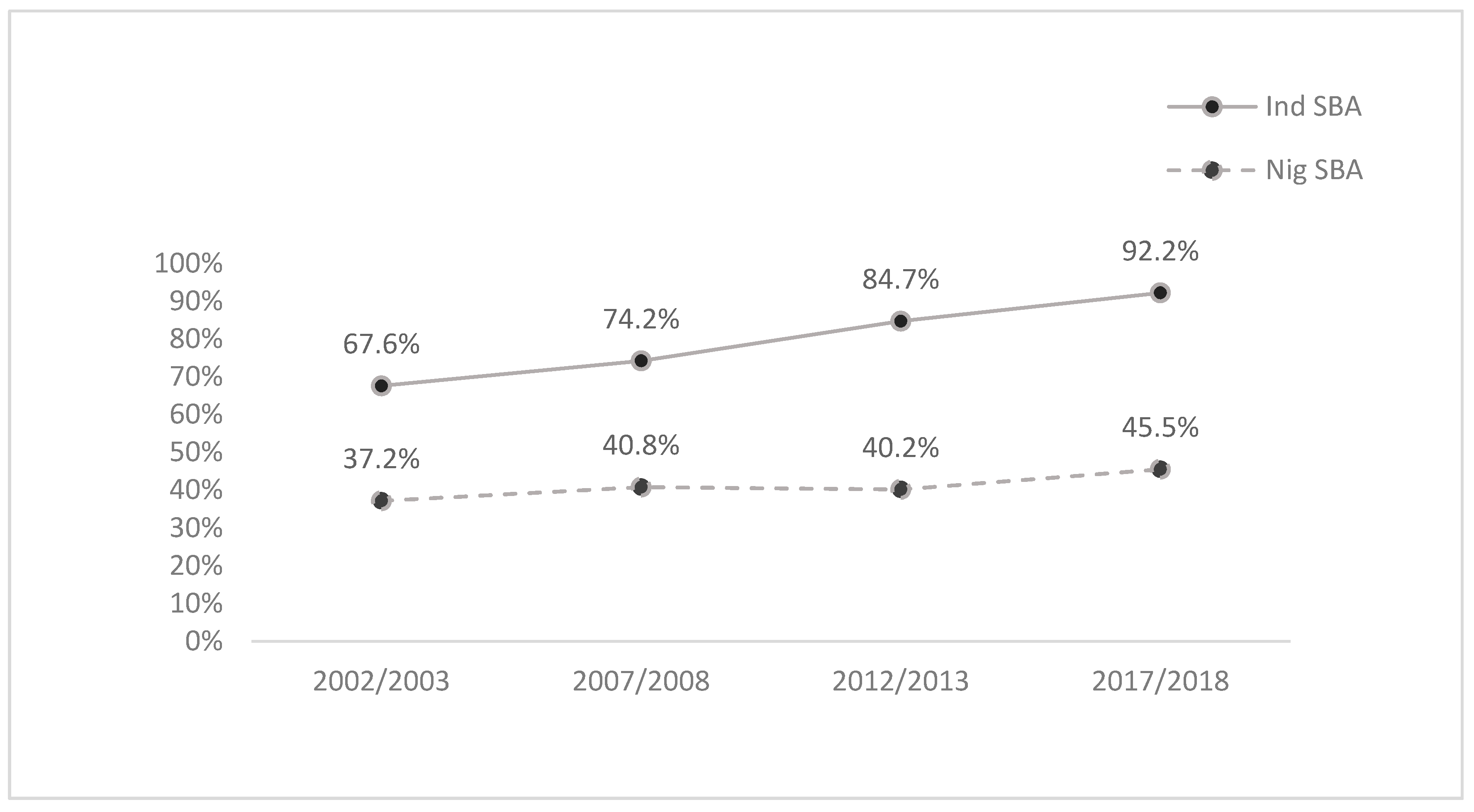
| 2002/2003 | 4130 (32.4) | 8600 (67.6) | <0.001 | 2451 (62.8) | 1449 (37.2) | <0.001 |
| 2007/2008 | 3624 (25.8) | 10,419 (74.2) | 10,380 (59.2) | 7157 (40.8) | ||
| 2012/2013 | 2256 (15.3) | 12,466 (84.7) | 12,195 (59.8) | 8181 (40.2) | ||
| 2017/2018 | 1198 (8.0) | 13,788 (92.0) | 11,938 (54.5) | 9973 (45.5) | ||
| Age | ||||||
| 15 to 29 years. | 5968 (21.1) | 22,369 (78.9) | <0.001 | 20,127 (60.6) | 13,099 (39.4) | <0.001 |
| 30 to 49 years. | 5239 (18.6) | 22,904 (81.4) | 16,836 (55.2) | 13,661 (44.8) | ||
| Educational attainment of husband/partner | ||||||
| Primary or lower | 7678 (36.3) | 13,489 (63.7) | <0.001 | 26,326 (77.5) | 7623 (22.5) | <0.001 |
| Secondary or higher | 3432 (9.9) | 31,278 (90.1) | 9076 (34.0) | 17,593 (66.0) | ||
| Has a say in household decision making | ||||||
| No | 3541 (23.1) | 11,788 (76.9) | <0.001 | 28,862 (68.3) | 13,408 (31.7) | <0.001 |
| Yes | 7553 (18.7) | 32,784 (81.3) | 6582 (36.3) | 11,575 (63.7) | ||
| Educational attainment of participant | ||||||
| Primary or lower | 8280 (37.5) | 13,778 (62.5) | <0.001 | 31,846 (76.7) | 9663 (23.3) | <0.001 |
| Secondary or higher | 2928 (8.5) | 31,494 (91.5) | 5117 (23.0) | 17,097 (77.0) | ||
| Exposure to newspaper, radio and television is at least once a week | ||||||
| No | 3290 (38.8) | 5200 (61.2) | <0.001 | 24,349 (73.0) | 9012 (27.0) | <0.001 |
| Yes | 7895 (16.5) | 40,016 (83.5) | 12,412 (41.3) | 17,646 (58.7) | ||
| Birth interval between most recent and preceding birth less than 24 months | ||||||
| No | 7273 (22.0) | 25,759 (78.0) | <0.001 | 25,205 (60.2) | 16,649 (39.8) | 0.014 |
| Yes | 956 (26.1) | 2701 (73.9) | 6462 (61.5) | 4039 (38.5) | ||
| First or second order birth | ||||||
| No | 5248 (27.3) | 13,966 (72.7) | <0.001 | 26,168 (62.7) | 15,538 (37.3) | <0.001 |
| Yes | 5960 (16.0) | 31,307 (84.0) | 10,796 (49.0) | 11,223 (51.0) | ||
| Received Antenatal care at least once during pregnancy | ||||||
| No | 2242 (77.3) | 658 (22.7) | <0.001 | 22,460 (93.4) | 1592 (6.6) | <0.001 |
| Yes | 8957 (16.7) | 44,603 (83.3) | 14,372 (36.4) | 25,101 (63.6) | ||
| Wealth Index (Combined) | ||||||
| Poor/Poorer | 7984 (34.7) | 15,009 (65.3) | <0.001 | 24,183 (85.0) | 4252 (15.0) | <0.001 |
| Middle/Upper | 3224 (9.6) | 30,264 (90.4) | 12,780 (36.2) | 22,508 (63.8) | ||
| Place of residence | ||||||
| Rural | 8495 (28.3) | 21,548 (71.7) | <0.001 | 29,917 (72.40) | 11,390 (27.60) | <0.001 |
| Urban | 2713 (10.3) | 23,725 (89.7) | 7046 (31.4) | 15,370 (68.6) | ||
| Can read part or whole sentences | ||||||
| No | 1600 (56.4) | 1238 (43.6) | <0.001 | 29,460 (79.9) | 7416 (20.1) | <0.001 |
| Yes | 9533 (17.9) | 43,856 (82.1) | 7273 (27.5) | 19,193 (72.5) | ||
| Perception of the distance to healthcare facility | ||||||
| Small or no problem | 8445 (17.2) | 40,721 (82.8) | <0.001 | 22,194 (51.3) | 21,076 (48.7) | <0.001 |
| Big problem | 2752 (38.1) | 4475 (61.9) | 14,663 (72.3) | 5629 (27.7) | ||
| Geographic Quartiles (based on 2008 SBA ratings) | ||||||
| Regional Quartile 1 | 2736 (34.0) | 5311 (66.0) | <0.001 | 22,471 (84.9) | 4005 (15.1) | <0.001 |
| Regional Quartile 2 | 4703 (25.6) | 13,664 (74.4) | 8462 (68.8) | 3834 (31.2) | ||
| Regional Quartile 3 | 2902 (14.3) | 17,395 (85.7) | 4286 (34.3) | 8194 (65.7) | ||
| Regional Quartile 4 | 863 (8.9) | 8872 (91.1) | 1744 (14.0) | 10,727 (86.0) | ||
| Indonesia (N = 56,607) | Nigeria (N = 63,924) | |||
|---|---|---|---|---|
| Characteristic | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
| Year of survey (Ref: Period 1) | ||||
| 2007/2008 | 1.38 (1.31–1.46) *** | 1.28 (1.18–1.38) *** | 1.17 (1.09–1.25) *** | 0.93 (0.82–1.05) |
| 2012/2013 | 2.65 (2.5–2.81) *** | 2.20 (2.02–2.4) *** | 1.13 (1.06–1.22) *** | 0.94 (0.83–1.05) |
| 2017/2018 | 5.53 (5.16–5.93) *** | 4.7 (4.26–5.18) *** | 1.41 (1.32–1.52) *** | 1.14 (1.02–1.28) * |
| Sociodemographic Factors | ||||
| Age (30–49 vs. 15–29) | 1.17 (1.12–1.22) *** | 1.58 (1.47–1.7) *** | 1.25 (1.21–1.29) *** | 1.25 (1.18–1.33) *** |
| Father attained secondary education or higher (yes vs. no) | 5.19 (4.96–5.43) *** | 1.85 (1.72–1.99) *** | 6.69 (6.46–6.94) *** | 1.38 (1.29–1.47) *** |
| Empowerment | ||||
| Autonomy (yes vs. no) | 1.3 (1.25–1.36) *** | 1.14 (1.06–1.22) *** | 3.79 (3.65–3.93) *** | 1.22 (1.15–1.3) *** |
| Secondary or higher education (yes vs. no) | 6.46 (6.17–6.77) *** | 2.24 (2.08–2.42) *** | 11.01 (10.59–11.44) *** | 1.76 (1.62–1.92) *** |
| Media exposure at least once a week (yes vs. no) | 3.21 (3.05–3.37) *** | 1.17 (1.08–1.26) *** | 3.84 (3.72–3.97) *** | 1.13 (1.06–1.19) *** |
| Family Planning | ||||
| Birth interval less than 24 months (yes vs. no) | 0.8 (0.74–0.86) *** | 0.98 (0.88–1.08) | 0.95 (0.91–0.99) * | 0.94 (0.88–1.01) |
| First or second birth order (yes vs. no) | 1.97 (1.89–2.06) *** | 1.34 (1.24–1.43) *** | 1.75 (1.69–1.81) *** | 1.15 (1.07–1.24) *** |
| At least one Antenatal appointment (yes vs. no) | 16.97 (15.51–18.56) ** | 7.60 (6.71–8.61) *** | 24.65 (23.33–26.04) *** | 11.38 (10.55–12.27) *** |
| Economic Accessibility | ||||
| Wealth Quintile (upper middle vs. Poor) | 4.99 (4.77–5.23) *** | 2.21 (2.06–2.38) *** | 10.02 (9.63–10.42) *** | 1.77 (1.66–1.9) *** |
| Community Impacting Factors | ||||
| Residence (urban vs. Rural) | 3.45 (3.29–3.61) *** | 1.55 (1.44–1.67) *** | 5.73 (5.53–5.94) *** | 1.50 (1.41–1.6) *** |
| Literacy (can read part or whole sentences vs. not) | 5.95 (5.50–6.43) *** | 1.39 (1.24–1.54) *** | 10.48 (10.10–10.88) *** | 1.41 (1.31–1.53) ** |
| Distance to HCF (big problem vs. small or no problem) | 0.34 (0.32–0.36) *** | 0.62 (0.57–0.68) *** | 0.40 (0.39–0.42) ** | 0.76 (0.71–0.8) *** |
| Geographic SBA Distribution (Ref: Quartile 1) | ||||
| Regional Quartile 2 | 1.5 (1.41–1.58) *** | 1.30 (1.20–1.42) *** | 2.54 (2.42–2.67) *** | 1.71 (1.59–1.84) *** |
| Regional Quartile 3 | 3.09 (2.91–3.28) *** | 2.95 (2.69–3.23) *** | 10.72 (10.2–11.27) *** | 5.84 (5.41–6.3) *** |
| Regional Quartile 4 | 5.3 (4.87–5.76) *** | 4.98 (4.42–5.61) *** | 34.51(32.47–36.67) *** | 10.92 (9.99–11.93) *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walker, T.; Woldegiorgis, M.; Bhowmik, J. Utilisation of Skilled Birth Attendant in Low- and Middle-Income Countries: Trajectories and Key Sociodemographic Factors. Int. J. Environ. Res. Public Health 2021, 18, 10722. https://doi.org/10.3390/ijerph182010722
Walker T, Woldegiorgis M, Bhowmik J. Utilisation of Skilled Birth Attendant in Low- and Middle-Income Countries: Trajectories and Key Sociodemographic Factors. International Journal of Environmental Research and Public Health. 2021; 18(20):10722. https://doi.org/10.3390/ijerph182010722
Chicago/Turabian StyleWalker, Tania, Mulu Woldegiorgis, and Jahar Bhowmik. 2021. "Utilisation of Skilled Birth Attendant in Low- and Middle-Income Countries: Trajectories and Key Sociodemographic Factors" International Journal of Environmental Research and Public Health 18, no. 20: 10722. https://doi.org/10.3390/ijerph182010722
APA StyleWalker, T., Woldegiorgis, M., & Bhowmik, J. (2021). Utilisation of Skilled Birth Attendant in Low- and Middle-Income Countries: Trajectories and Key Sociodemographic Factors. International Journal of Environmental Research and Public Health, 18(20), 10722. https://doi.org/10.3390/ijerph182010722







