Higher Neighborhood Population Density Is Associated with Lower Potassium Intake in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Selection Criteria
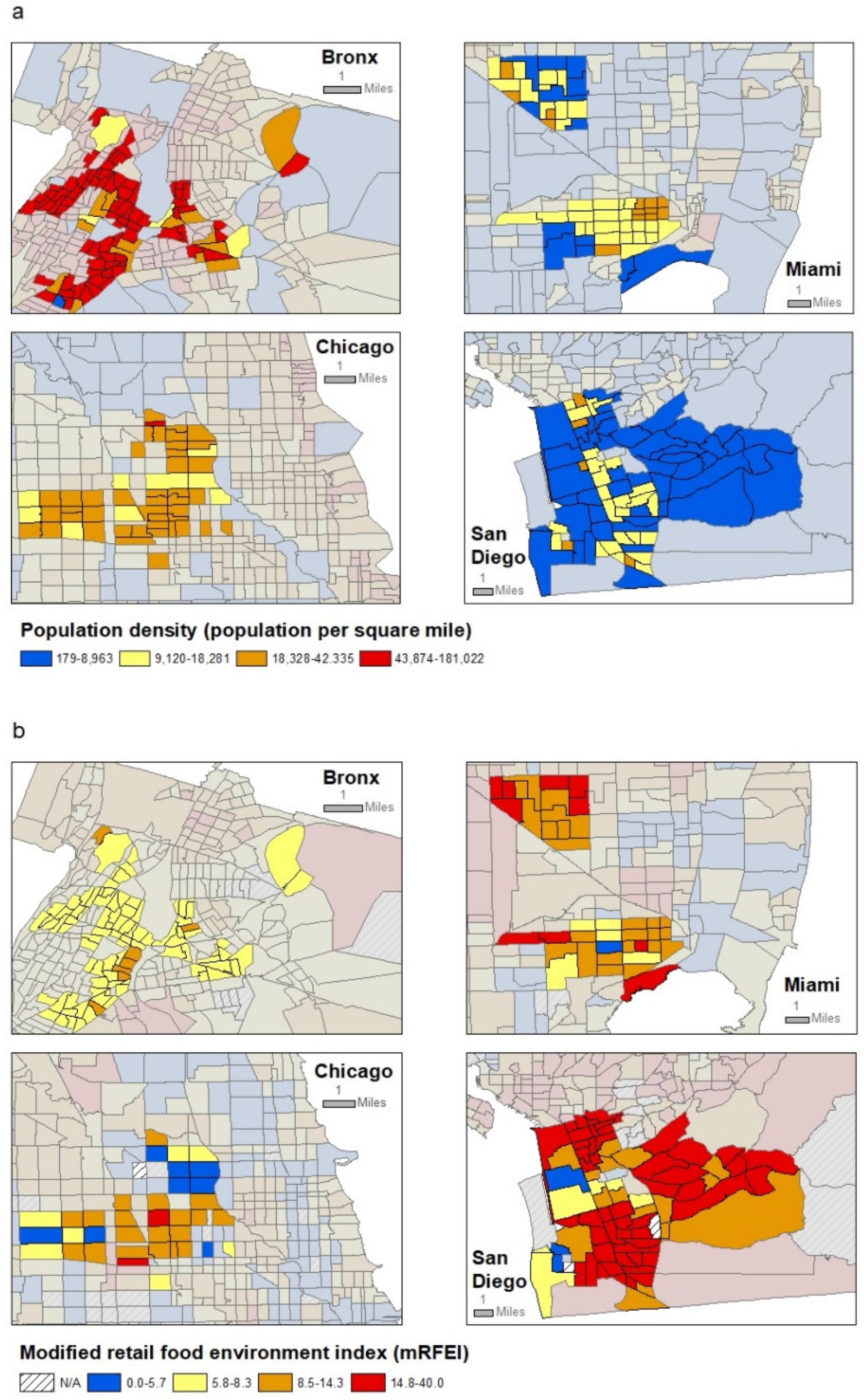
2.2. Neighborhood-Level Exposures of Interest
2.3. Covariates
2.4. Objectively Measured Potassium Intake
2.5. Statistical Analysis
3. Results
3.1. Study Population Characteristics, and Neighborhood Variation in Potassium Intake
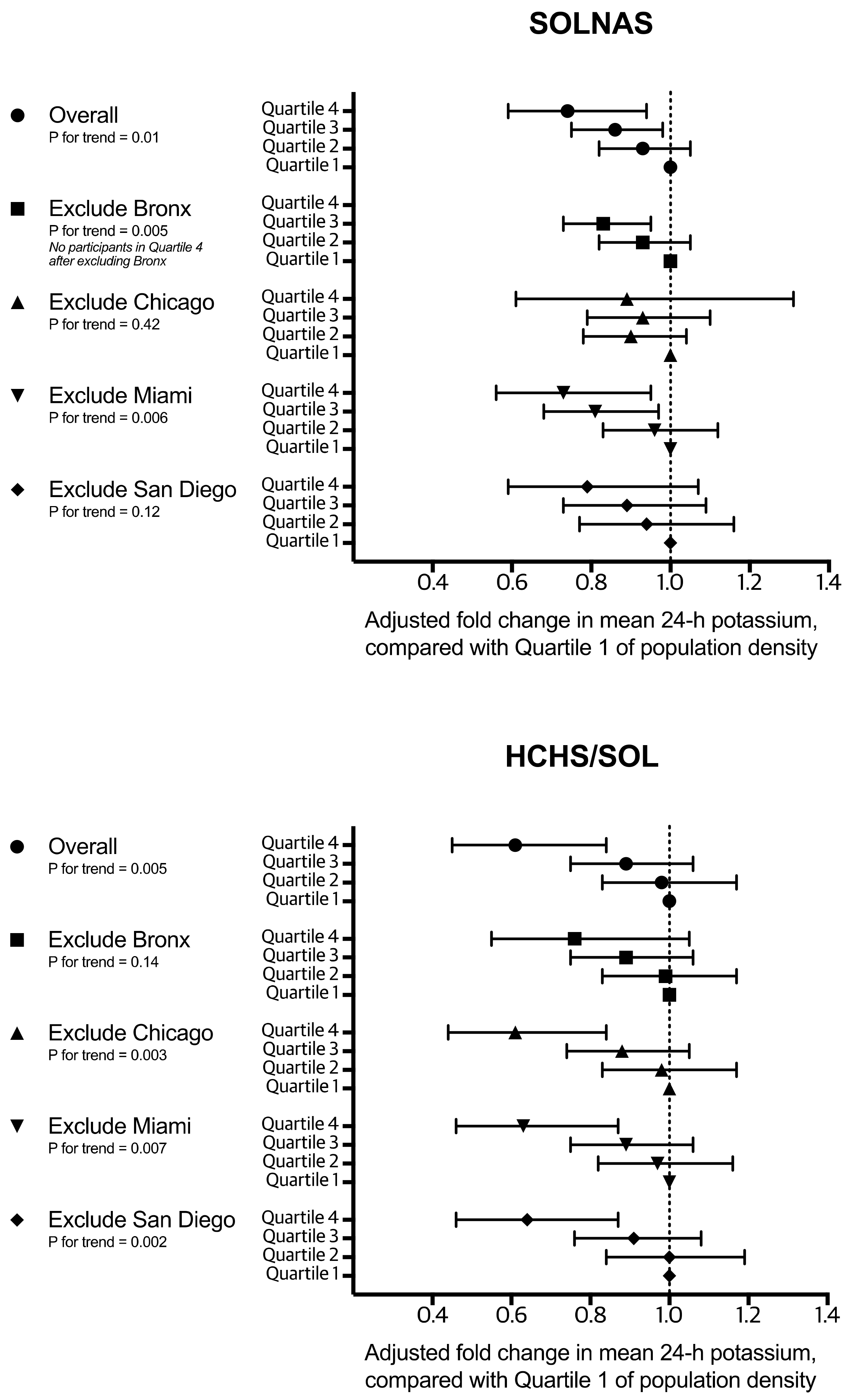
3.2. Adjusted Associations of Neighborhood Characteristics with Potassium Intake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Intersalt Cooperative Research Group. Intersalt: An international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988, 297, 319–328. [Google Scholar] [CrossRef]
- Adrogue, H.J.; Madias, N.E. Sodium and potassium in the pathogenesis of hypertension. N. Engl. J. Med. 2007, 356, 1966–1978. [Google Scholar] [CrossRef]
- Cook, N.R.; Obarzanek, E.; Cutler, J.A.; Buring, J.E.; Rexrode, K.M.; Kumanyika, S.K.; Appel, L.J.; Whelton, P.K.; Trials of Hypertension Prevention Collaborative Research Group. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: The Trials of Hypertension Prevention follow-up study. Arch. Intern. Med. 2009, 169, 32–40. [Google Scholar] [CrossRef]
- Yang, Q.; Liu, T.; Kuklina, E.V.; Flanders, W.D.; Hong, Y.; Gillespie, C.; Chang, M.H.; Gwinn, M.; Dowling, N.; Khoury, M.J.; et al. Sodium and potassium intake and mortality among US adults: Prospective data from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 2011, 171, 1183–1191. [Google Scholar] [CrossRef] [PubMed]
- Mente, A.; O’Donnell, M.J.; Rangarajan, S.; McQueen, M.J.; Poirier, P.; Wielgosz, A.; Morrison, H.; Li, W.; Wang, X.; Di, C.; et al. Association of urinary sodium and potassium excretion with blood pressure. N. Engl. J. Med. 2014, 371, 601–611. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; Wang, X.; Liu, L.; Yan, H.; Lee, S.F.; Mony, P.; Devanath, A.; et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N. Engl. J. Med. 2014, 371, 612–623. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 9th Edition. 2020–2025. Available online: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf (accessed on 28 September 2021).
- Cogswell, M.E.; Loria, C.M.; Terry, A.L.; Zhao, L.; Wang, C.Y.; Chen, T.C.; Wright, J.D.; Pfeiffer, C.M.; Merritt, R.; Moy, C.S.; et al. Estimated 24-hour urinary sodium and potassium excretion in US adults. JAMA 2018, 319, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Perez-Escamilla, R.; Putnik, P. The role of acculturation in nutrition, lifestyle, and incidence of type 2 diabetes among Latinos. J. Nutr. 2007, 137, 860–870. [Google Scholar] [CrossRef]
- Siega-Riz, A.M.; Sotres-Alvarez, D.; Ayala, G.X.; Ginsberg, M.; Himes, J.H.; Liu, K.; Loria, C.M.; Mossavar-Rahmani, Y.; Rock, C.L.; Rodriguez, B.; et al. Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. Am. J. Clin. Nutr. 2014, 99, 1487–1498. [Google Scholar] [CrossRef] [PubMed]
- Elfassy, T.; Sotres-Alvarez, D.; Van Horn, L.; Angell, S.; Schneiderman, N.; Rundek, T.; Raij, L.; Smoller, S.W.; Mossavar-Rahmani, Y.; Daviglus, M.; et al. Daily intake of sodium and potassium among diverse US Hispanics/Latinos, the Hispanic Community Health Study/Study of Latinos. Am. J. Hypertens. 2019, 32, 868–879. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Larson, N.I.; Story, M.T.; Nelson, M.C. Neighborhood environments: Disparities in access to healthy foods in the U.S. Am. J. Prev. Med. 2009, 36, 74–81. [Google Scholar] [CrossRef]
- Mujahid, M.S.; Diez Roux, A.V.; Morenoff, J.D.; Raghunathan, T.E.; Cooper, R.S.; Ni, H.; Shea, S. Neighborhood characteristics and hypertension. Epidemiology 2008, 19, 590–598. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 7th Edition. 2010. Available online: https://www.dietaryguidelines.gov/sites/default/files/2019-05/DietaryGuidelines2010.pdf (accessed on 28 September 2021).
- Murakami, K.; Sasaki, S.; Takahashi, Y.; Uenishi, K.; Japan Dietetic Students’ Study for Nutrition and Biomarkers Group. Neighbourhood food store availability in relation to 24 h urinary sodium and potassium excretion in young Japanese women. Br. J. Nutr. 2010, 104, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.V.; Diez Roux, A.V.; Nettleton, J.A.; Jacobs, D.R.; Franco, M. Fast-food consumption, diet quality, and neighborhood exposure to fast food: The Multi-ethnic Study of Atherosclerosis. Am. J. Epidemiol. 2009, 170, 29–36. [Google Scholar] [CrossRef]
- Elfassy, T.; Yi, S.S.; Llabre, M.M.; Schneiderman, N.; Gellman, M.; Florez, H.; Prado, G.; Zeki Al Hazzouri, A. Neighbourhood socioeconomic status and cross-sectional associations with obesity and urinary biomarkers of diet among New York City adults: The Heart Follow-up Study. BMJ Open 2017, 7, e018566. [Google Scholar] [CrossRef] [PubMed]
- Mercille, G.; Richard, L.; Gauvin, L.; Kestens, Y.; Shatenstein, B.; Daniel, M.; Payette, H. The food environment and diet quality of urban-dwelling older women and men: Assessing the moderating role of diet knowledge. Can. J. Public Health 2016, 107 (Suppl. S1), 5309. [Google Scholar] [CrossRef]
- Sorlie, P.D.; Aviles-Santa, L.M.; Wassertheil-Smoller, S.; Kaplan, R.C.; Daviglus, M.L.; Giachello, A.L.; Schneiderman, N.; Raij, L.; Talavera, G.; Allison, M.; et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann. Epidemiol. 2010, 20, 629–641. [Google Scholar] [CrossRef]
- Lavange, L.M.; Kalsbeek, W.D.; Sorlie, P.D.; Aviles-Santa, L.M.; Kaplan, R.C.; Barnhart, J.; Liu, K.; Giachello, A.; Lee, D.J.; Ryan, J.; et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann. Epidemiol. 2010, 20, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Mossavar-Rahmani, Y.; Shaw, P.A.; Wong, W.W.; Sotres-Alvarez, D.; Gellman, M.D.; Van Horn, L.; Stoutenberg, M.; Daviglus, M.L.; Wylie-Rosett, J.; Siega-Riz, A.M.; et al. Applying recovery biomarkers to calibrate self-report measures of energy and protein in the Hispanic Community Health Study/Study of Latinos. Am. J. Epidemiol. 2015, 181, 996–1007. [Google Scholar] [CrossRef] [PubMed]
- Mossavar-Rahmani, Y.; Sotres-Alvarez, D.; Wong, W.W.; Loria, C.M.; Gellman, M.D.; Van Horn, L.; Alderman, M.H.; Beasley, J.M.; Lora, C.M.; Siega-Riz, A.M.; et al. Applying recovery biomarkers to calibrate self-report measures of sodium and potassium in the Hispanic Community Health Study/Study of Latinos. J. Hum. Hypertens. 2017, 31, 462–473. [Google Scholar] [CrossRef]
- U.S. Department of Commerce. Geographic Areas Reference Manual; U.S. Department of Commerce: Washington, DC, USA, 1994.
- U.S. Census Bureau. American Community Survey. Available online: http://www.census.gov/acs/www/ (accessed on 28 September 2021).
- Centers for Disease Control; Prevention Div. of Nutrition Physical Activity and Obesity. Children’s Food Environment State Indicator Report. 2011. Available online: https://www.cdc.gov/obesity/downloads/ChildrensFoodEnvironment.pdf (accessed on 28 September 2021).
- Greer, S.; Schieb, L.; Schwartz, G.; Onufrak, S.; Park, S. Association of the neighborhood retail food environment with sodium and potassium intake among US adults. Prev. Chronic. Dis. 2014, 11, E70. [Google Scholar] [CrossRef]
- Mercado, C.I.; Cogswell, M.E.; Valderrama, A.L.; Wang, C.Y.; Loria, C.M.; Moshfegh, A.J.; Rhodes, D.G.; Carriquiry, A.L. Difference between 24-h diet recall and urine excretion for assessing population sodium and potassium intake in adults aged 18-39 y. Am. J. Clin. Nutr. 2015, 101, 376–386. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition. Available online: https://www.dietaryguidelines.gov/sites/default/files/2019-05/2015-2020_Dietary_Guidelines.pdf (accessed on 28 September 2021).
- Holbrook, J.T.; Patterson, K.Y.; Bodner, J.E.; Douglas, L.W.; Veillon, C.; Kelsay, J.L.; Mertz, W.; Smith, J.C., Jr. Sodium and potassium intake and balance in adults consuming self-selected diets. Am. J. Clin. Nutr. 1984, 40, 786–793. [Google Scholar] [CrossRef]
- Clark, A.J.; Mossholder, S. Sodium and potassium intake measurements: Dietary methodology problems. Am. J. Clin. Nutr. 1986, 43, 470–476. [Google Scholar] [CrossRef]
- McCullough, M.L.; Swain, J.F.; Malarick, C.; Moore, T.J. Feasibility of outpatient electrolyte balance studies. J. Am. Coll. Nutr. 1991, 10, 140–148. [Google Scholar] [CrossRef]
- Freedman, L.S.; Midthune, D.; Carroll, R.J.; Krebs-Smith, S.; Subar, A.F.; Troiano, R.P.; Dodd, K.; Schatzkin, A.; Bingham, S.A.; Ferrari, P.; et al. Adjustments to improve the estimation of usual dietary intake distributions in the population. J. Nutr. 2004, 134, 1836–1843. [Google Scholar] [CrossRef]
- Singer, J.D. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J. Educ. Behav. Stat. 1998, 24, 323–355. [Google Scholar] [CrossRef]
- Merlo, J.; Chaix, B.; Yang, M.; Lynch, J.; Rastam, L. A brief conceptual tutorial of multilevel analysis in social epidemiology: Linking the statistical concept of clustering to the idea of contextual phenomenon. J. Epidemiol. Community Health 2005, 59, 443–449. [Google Scholar] [CrossRef]
- Harnack, L.J.; Cogswell, M.E.; Shikany, J.M.; Gardner, C.D.; Gillespie, C.; Loria, C.M.; Zhou, X.; Yuan, K.; Steffen, L.M. Sources of sodium in US adults from 3 geographic regions. Circulation 2017, 135, 1775–1783. [Google Scholar] [CrossRef]
- Molenberghs, G.; Fitzmaurice, G.; Kenward, M.G.; Tsiatis, A.; Verbeke, G. Handbook of Missing Data Methodology; Chapman and Hall/CRC: London, UK, 2015. [Google Scholar]
- Moulton, B.R. An illustration of a pitfall in estimating the effects of aggregate variables on micro units. Rev. Econ. Stat. 1990, 72, 334–338. [Google Scholar] [CrossRef]
- Shaw, P.A.; He, J.; Shepherd, B.E. Regression calibration to correct correlated errors in outcome and exposure. Stat. Med. 2021, 40, 271–286. [Google Scholar] [CrossRef]
- Baldoni, P.; Sotres-Alvarez, D.; Lumley, T.S.; Shaw, P.A. On the use of regression calibration in a complex sampling design with application to the Hispanic Community Health Study/Study of Latinos. Am. J. Epidemiol. 2021, 190, 1366–1376. [Google Scholar] [CrossRef]
- Pudrovska, T.; Reither, E.N.; Logan, E.S.; Sherman-Wilkins, K.J. Gender and reinforcing associations between socioeconomic disadvantage and body mass over the life course. J. Health Soc. Behav. 2014, 55, 283–301. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Chaix, B.; Rosvall, M.; Merlo, J. Assessment of the magnitude of geographical variations and socioeconomic contextual effects on ischaemic heart disease mortality: A multilevel survival analysis of a large Swedish cohort. J. Epidemiol. Community Health 2007, 61, 349–355. [Google Scholar] [CrossRef]
- Chaix, B.; Rosvall, M.; Lynch, J.; Merlo, J. Disentangling contextual effects on cause-specific mortality in a longitudinal 23-year follow-up study: Impact of population density or socioeconomic environment? Int. J. Epidemiol. 2006, 35, 633–643. [Google Scholar] [CrossRef]
- Meijer, M.; Kejs, A.M.; Stock, C.; Bloomfield, K.; Ejstrud, B.; Schlattmann, P. Population density, socioeconomic environment and all-cause mortality: A multilevel survival analysis of 2.7 million individuals in Denmark. Health Place 2012, 18, 391–399. [Google Scholar] [CrossRef]
- Nakaya, T.; Honjo, K.; Hanibuchi, T.; Ikeda, A.; Iso, H.; Inoue, M.; Sawada, N.; Tsugane, S. Associations of all-cause mortality with census-based neighbourhood deprivation and population density in Japan: A multilevel survival analysis. PLoS ONE 2014, 9, e97802. [Google Scholar]
- Drewnowski, A.; Rehm, C.D.; Maillot, M.; Monsivais, P. The relation of potassium and sodium intakes to diet cost among U.S. adults. J. Hum. Hypertens. 2015, 29, 14–21. [Google Scholar] [CrossRef][Green Version]
- Murakami, K.; Sasaki, S.; Takahashi, Y.; Uenishi, K.; Japan Dietetic Students’ Study for Nutrition and Biomarkers Group. Neighborhood socioeconomic disadvantage is associated with higher ratio of 24-hour urinary sodium to potassium in young Japanese women. J. Am. Diet. Assoc. 2009, 109, 1606–1611. [Google Scholar] [CrossRef]
- Yi, S.S.; Ruff, R.R.; Jung, M.; Waddell, E.N. Racial/ethnic residential segregation, neighborhood poverty and urinary biomarkers of diet in New York City adults. Soc. Sci. Med. 2014, 122, 122–129. [Google Scholar] [CrossRef]
- Bell, C.N.; Kerr, J.; Young, J.L. Associations between obesity, obesogenic environments, and structural racism vary by county-level racial composition. Int. J. Environ. Res. Public Health 2019, 16, 861. [Google Scholar] [CrossRef]
- Feng, J.; Glass, T.A.; Curriero, F.C.; Stewart, W.F.; Schwartz, B.S. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place 2010, 16, 175–190. [Google Scholar] [CrossRef]
- Thornton, L.E.; Pearce, J.R.; Kavanagh, A.M. Using Geographic Information Systems (GIS) to assess the role of the built environment in influencing obesity: A glossary. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 71. [Google Scholar] [CrossRef]
- Ogburn, E.L.; Rudolph, K.E.; Morello-Frosch, R.; Khan, A.; Casey, J.A. A warning about using predicted values from regression models for epidemiologic inquiry. Am. J. Epidemiol. 2021, 190, 1142–1147. [Google Scholar] [CrossRef]
| SOLNAS (N = 440) | HCHS/SOL (N = 13,835) | |||
|---|---|---|---|---|
| N (%) | Mean 24-h Urinary Biomarker Potassium, mg/day (SD) | N (%) | Imputed Mean 24-h Urinary Biomarker Potassium *, mg/day (SD) | |
| Overall | 440 (100) | 2629 (1124) | 13,835 (100) | 2702 (1347) |
| Sex | ||||
| Female | 271 (62) | 2424 (998) | 8307 (52) | 2506 (1218) |
| Male | 169 (38) | 2959 (1234) | 5528 (48) | 2998 (1469) |
| Age, years | ||||
| 18–24 | 35 (8) | 2276 (1232) | 1328 (16) | 2248 (1097) |
| 25–34 | 49 (11) | 2398 (1162) | 1742 (21) | 2487 (1223) |
| 35–44 | 84 (19) | 2562 (1039) | 2511 (21) | 2679 (1305) |
| 45–54 | 146 (33) | 2746 (1197) | 4200 (19) | 2800 (1370) |
| 55–64 | 101 (23) | 2712 (1015) | 2926 (13) | 2912 (1435) |
| 65–74 | 25 (6) | 2789 (1060) | 1128 (9) | 2715 (1324) |
| Hispanic/Latino background | ||||
| Central American | 48 (11) | 2735 (925) | 1531 (8) | 2860 (1384) |
| Cuban | 64 (15) | 2872 (1060) | 1993 (20) | 3001 (1461) |
| Dominican | 46 (10) | 2569 (1104) | 1159 (9) | 2725 (1330) |
| Mexican | 132 (30) | 2886 (1246) | 6043 (42) | 2724 (1330) |
| Puerto Rican | 112 (25) | 2161 (905) | 2188 (16) | 2257 (1114) |
| South American | 38 (9) | 2651 (1240) | 921 (5) | 2681 (1308) |
| Smoking status | ||||
| Never | 263 (60) | 2673 (1139) | 8471 (62) | 2680 (1321) |
| Former | 86 (20) | 2857 (1127) | 2756 (17) | 2984 (1464) |
| Current | 91 (21) | 2288 (1008) | 2608 (21) | 2477 (1232) |
| Reported annual income, US dollars | ||||
| Not reported | 40 (9) | 2754 (1077) | 1146 (9) | 2693 (1319) |
| <10,000 | 63 (14) | 2421 (1051) | 1944 (13) | 2461 (1196) |
| 10,001–20,000 | 145 (33) | 2420 (1124) | 4176 (29) | 2496 (1222) |
| 20,001–40,000 | 129 (29) | 2873 (1109) | 4387 (31) | 2922 (1432) |
| 40,001–75,000 | 53 (12) | 2748 (1169) | 1660 (13) | 2863 (1406) |
| >75,000 | 10 (2) | 2710 (1175) | 522 (5) | 2912 (1428) |
| Body mass index, kg/m2 | ||||
| <18.5 | 6 (1) | 1983 (176) | 105 (1) | 2171 (1017) |
| 18.5–24.9 | 82 (19) | 2308 (1062) | 2645 (22) | 2922 (1432) |
| 25–29.9 | 177 (40) | 2594 (1123) | 5252 (38) | 2863 (1406) |
| 30+ | 175 (40) | 2836 (1127) | 5833 (40) | 2912 (1428) |
| Dietary supplement use | ||||
| Yes | 213 (48) | 2851 (1167) | 6383 (42) | 2948 (1434) |
| No | 227 (52) | 2422 (1043) | 7452 (58) | 2492 (1227) |
| Employment | ||||
| Retired | 35 (8) | 2554 (1185) | 1298 (8) | 2507 (1221) |
| Unemployed | 199 (45) | 2434 (1006) | 5471 (41) | 2517 (1236) |
| Part-time | 86 (20) | 2688 (1209) | 2371 (17) | 2709 (1328) |
| Full-time | 120 (27) | 2934 (1170) | 4695 (34) | 2968 (1454) |
| Field Center | ||||
| Bronx | 109 (25) | 2260 (1020) | 2888 (25) | 2404 (1222) |
| Chicago | 110 (25) | 2499 (1107) | 3961 (18) | 2579 (1253) |
| Miami | 112 (25) | 2809 (1083) | 3358 (29) | 2924 (1428) |
| San Diego | 109 (25) | 2946 (1167) | 3628 (28) | 2870 (1391) |
| Neighborhood population density, population per square mile | ||||
| Quartile 1: 179–8963 | 75 (17) | 3170 (1215) | 2410 (19) | 2976 (1437) |
| Quartile 2: 9120–18,281 | 91 (21) | 2713 (975) | 3671 (28) | 2914 (1417) |
| Quartile 3: 18,328–42,335 | 175 (40) | 2583 (1143) | 5518 (32) | 2618 (1276) |
| Quartile 4: 43,874–181,022 | 99 (22) | 2226 (976) | 2506 (22) | 2343 (1178) |
| Neighborhood median household income, US dollars | ||||
| Quartile 1: 12,188–27,324 | 130 (30) | 2410 (1052) | 3500 (25) | 2589 (1313) |
| Quartile 2: 27,385–36,132 | 119 (27) | 2743 (1098) | 3844 (28) | 2864 (1417) |
| Quartile 3: 36,319–46,875 | 130 (30) | 2681 (1178) | 4463 (32) | 2649 (1297) |
| Quartile 4: 47,349–129,167 | 61 (14) | 2765 (1165) | 2028 (15) | 2710 (1322) |
| Neighborhood % of population Hispanic/Latino | ||||
| Quartile 1: 7.1–56.4 | 64 (15) | 2647 (1133) | 1900 (18) | 2598 (1266) |
| Quartile 2: 57.0–69.1 | 74 (17) | 2639 (1133) | 2890 (23) | 2728 (1357) |
| Quartile 3: 69.2–81.8 | 157 (36) | 2517 (1113) | 4394 (26) | 2626 (1314) |
| Quartile 4: 82.9–100.0 | 145 (33) | 2738 (1127) | 4651 (34) | 2800 (1384) |
| Neighborhood modified retail food environment index | ||||
| Quartile 1: 0.0–5.7 | 98 (22) | 2322 (1106) | 2436 (18) | 2572 (1300) |
| Quartile 2: 5.8–8.3 | 91 (21) | 2375 (991) | 3100 (21) | 2527 (1265) |
| Quartile 3: 8.5–14.3 | 131 (30) | 2800 (1101) | 4929 (36) | 2748 (1352) |
| Quartile 4: 14.8–40.0 | 117 (27) | 2884 (1174) | 3081 (24) | 2893 (1411) |
| Model 1: Unadjusted | Model 2: Adjusted for Individual-Level Characteristics | Model 3: Model 2 Plus Adjustment for Selected Neighborhood Characteristics | Model 4: Model 3 Plus Additional Adjustment for mRFEI | |||||
|---|---|---|---|---|---|---|---|---|
| Fold Change in Potassium (95% CI) | p-Value * | Fold Change in Potassium (95% CI) | p-Value * | Fold Change in Potassium (95% CI) | p-Value * | Fold Change in Potassium (95% CI) | p-Value * | |
| SOLNAS | ||||||||
| Neighborhood population density | <0.001 | 0.02 | 0.01 | 0.06 | ||||
| Quartile 1 | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Quartile 2 | 0.86 (0.76, 0.97) | 0.02 | 0.94 (0.84, 1.07) | 0.36 | 0.93 (0.82, 1.05) | 0.26 | 0.93 (0.83, 1.05) | 0.27 |
| Quartile 3 | 0.80 (0.71, 0.89) | <0.001 | 0.88 (0.78, 1.00) | 0.05 | 0.86 (0.75, 0.98) | 0.02 | 0.88 (0.77, 1.01) | 0.07 |
| Quartile 4 | 0.69 (0.61, 0.79) | <0.001 | 0.82 (0.68, 0.98) | 0.03 | 0.74 (0.59, 0.94) | 0.01 | 0.80 (0.62, 1.04) | 0.09 |
| Neighborhood median household income | 0.03 | 0.85 | 0.21 | 0.21 | ||||
| Quartile 1 | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Quartile 2 | 1.15 (1.03, 1.28) | 0.02 | 1.10 (0.98, 1.22) | 0.09 | 1.04 (0.93, 1.17) | 0.46 | 1.07 (0.95, 1.20) | 0.29 |
| Quartile 3 | 1.11 (0.99, 1.24) | 0.07 | 1.03 (0.93, 1.15) | 0.54 | 0.96 (0.85, 1.09) | 0.53 | 0.98 (0.86, 1.12) | 0.77 |
| Quartile 4 | 1.16 (1.02, 1.32) | 0.02 | 1.02 (0.90, 1.17) | 0.72 | 0.89 (0.75, 1.07) | 0.21 | 0.89 (0.74, 1.06) | 0.20 |
| Neighborhood modified retail food environment index (mRFEI) | <0.001 | 0.06 | - | 0.18 | ||||
| Quartile 1 | 1.00 | Ref. | 1.00 | Ref. | - | - | 1.00 | Ref. |
| Quartile 2 | 1.04 (0.92, 1.19) | 0.51 | 1.06 (0.94, 1.18) | 0.35 | - | - | 1.05 (0.93, 1.18) | 0.46 |
| Quartile 3 | 1.25 (1.11, 1.40) | <0.001 | 1.14 (1.01, 1.28) | 0.03 | - | - | 1.15 (1.00, 1.33) | 0.045 |
| Quartile 4 | 1.26 (1.11, 1.43) | <0.001 | 1.13 (0.98, 1.30) | 0.10 | - | - | 1.10 (0.94, 1.30) | 0.24 |
| HCHS/SOL | ||||||||
| Neighborhood population density | <0.001 | 0.003 | 0.005 | 0.007 | ||||
| Quartile 1 | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Quartile 2 | 1.03 (0.86, 1.23) | 0.75 | 0.99 (0.83, 1.19) | 0.95 | 0.98 (0.83, 1.17) | 0.85 | 0.99 (0.83, 1.17) | 0.88 |
| Quartile 3 | 0.89 (0.76, 1.05) | 0.17 | 0.89 (0.76, 1.05) | 0.18 | 0.89 (0.75, 1.06) | 0.19 | 0.89 (0.75, 1.06) | 0.20 |
| Quartile 4 | 0.71 (0.60, 0.86) | <0.001 | 0.68 (0.52, 0.89) | 0.005 | 0.61 (0.45, 0.84) | 0.003 | 0.62 (0.45, 0.86) | 0.004 |
| Neighborhood median household income | 0.40 | 0.18 | 0.44 | 0.47 | ||||
| Quartile 1 | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Quartile 2 | 1.10 (0.95, 1.28) | 0.18 | 1.12 (0.97, 1.28) | 0.12 | 1.04 (0.89, 1.20) | 0.64 | 1.04 (0.89, 1.20) | 0.64 |
| Quartile 3 | 0.99 (0.85, 1.15) | 0.86 | 1.06 (0.90, 1.25) | 0.50 | 0.91 (0.75, 1.09) | 0.31 | 0.91 (0.76, 1.10) | 0.32 |
| Quartile 4 | 1.15 (0.95, 1.38) | 0.15 | 1.18 (0.97, 1.43) | 0.10 | 0.95 (0.74, 1.22) | 0.70 | 0.96 (0.75, 1.22) | 0.72 |
| Neighborhood modified retail food environment index (mRFEI) | <0.001 | 0.004 | - | 0.36 | ||||
| Quartile 1 | 1.00 | Ref. | 1.00 | Ref. | - | - | 1.00 | Ref. |
| Quartile 2 | 0.99 (0.92, 1.06) | 0.79 | 1.00 (0.94, 1.06) | 0.92 | - | - | 0.99 (0.96, 1.02) | 0.56 |
| Quartile 3 | 1.18 (1.08, 1.29) | <0.001 | 1.12 (1.02, 1.22) | 0.02 | - | - | 1.02 (0.99, 1.05) | 0.25 |
| Quartile 4 | 1.20 (1.08, 1.34) | <0.001 | 1.15 (1.04, 1.28) | 0.006 | - | - | 1.01 (0.98, 1.05) | 0.48 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanna, D.B.; Hua, S.; Gonzalez, F., II; Kershaw, K.N.; Rundle, A.G.; Van Horn, L.V.; Wylie-Rosett, J.; Gellman, M.D.; Lovasi, G.S.; Kaplan, R.C.; et al. Higher Neighborhood Population Density Is Associated with Lower Potassium Intake in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Int. J. Environ. Res. Public Health 2021, 18, 10716. https://doi.org/10.3390/ijerph182010716
Hanna DB, Hua S, Gonzalez F II, Kershaw KN, Rundle AG, Van Horn LV, Wylie-Rosett J, Gellman MD, Lovasi GS, Kaplan RC, et al. Higher Neighborhood Population Density Is Associated with Lower Potassium Intake in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). International Journal of Environmental Research and Public Health. 2021; 18(20):10716. https://doi.org/10.3390/ijerph182010716
Chicago/Turabian StyleHanna, David B., Simin Hua, Franklyn Gonzalez, II, Kiarri N. Kershaw, Andrew G. Rundle, Linda V. Van Horn, Judith Wylie-Rosett, Marc D. Gellman, Gina S. Lovasi, Robert C. Kaplan, and et al. 2021. "Higher Neighborhood Population Density Is Associated with Lower Potassium Intake in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL)" International Journal of Environmental Research and Public Health 18, no. 20: 10716. https://doi.org/10.3390/ijerph182010716
APA StyleHanna, D. B., Hua, S., Gonzalez, F., II, Kershaw, K. N., Rundle, A. G., Van Horn, L. V., Wylie-Rosett, J., Gellman, M. D., Lovasi, G. S., Kaplan, R. C., Mossavar-Rahmani, Y., & Shaw, P. A. (2021). Higher Neighborhood Population Density Is Associated with Lower Potassium Intake in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). International Journal of Environmental Research and Public Health, 18(20), 10716. https://doi.org/10.3390/ijerph182010716







