Subjective Psychophysical Experiences in the Course of Inflammatory Bowel Disease—A Comparative Analysis Based on the Polish Pediatric Crohn’s and Colitis Cohort (POCOCO)
Abstract
1. Introduction
2. Materials and Methods
- Department of Pediatric Gastroenterology and Metabolic Diseases, Poznań University of Medical Sciences;
- The Department of Gastroenterology, Hepatology, Feeding Disorders and Paediatrics; The Children’s Memorial Health Institute, Warsaw;
- Department of Pediatric Gastroenterology and Nutrition, Medical University of Warsaw;
- Department and Clinic of Pediatrics, Gastroenterology and Nutrition, Wroclaw Medical University;
- Department of Pediatrics, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice;
- Department of Pediatrics, Faculty of Medical Sciences, Medical University of Silesia in Katowice;
- Department of Pediatric Endoscopy and Gastrointestinal Function Testing, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toruń, Bydgoszcz.
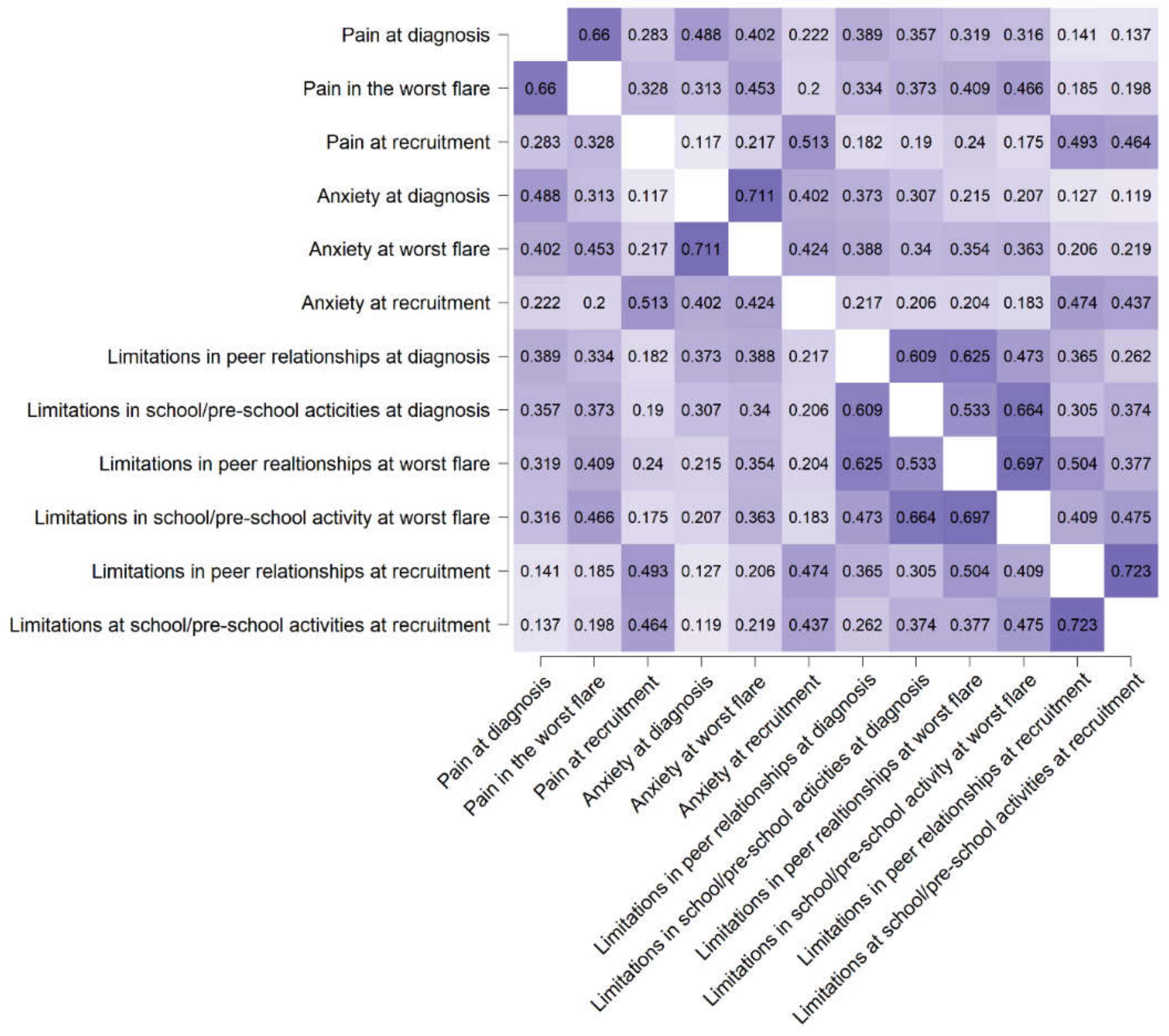
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ochsenkühn, T.; D’Haens, G. Current misunderstandings in the management of ulcerative colitis. Gut 2011, 60, 1294–1299. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Devlen, J.; Beusterien, K.; Yen, L.; Ahmed, A.; Cheifetz, A.S.; Moss, A.C. The burden of inflammatory bowel disease: A patient-reported qualitative analysis and development of a conceptual model. Inflamm. Bowel Dis. 2014, 20, 545–552. [Google Scholar] [CrossRef]
- Dibley, L.; Norton, C. Experiences of fecal incontinence in people with inflammatory bowel disease: Self-reported experiences among a community sample. Inflamm. Bowel Dis. 2013, 19, 1450–1462. [Google Scholar] [CrossRef] [PubMed]
- Greenley, R.N.; Hommel, K.A.; Nebel, J.; Raboin, T.; Li, S.-H.; Simpson, P.; Mackner, L. A meta-analytic review of the psychosocial adjustment of youth with inflammatory bowel disease. J. Pediatr. Psychol. 2010, 35, 857–869. [Google Scholar] [CrossRef]
- Mackner, L.M.; Greenley, R.N.; Szigethy, E.; Herzer, M.; Deer, K.; Hommel, K.A. Psychosocial issues in pediatric inflammatory bowel disease: Report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Navabi, S.; Gorrepati, V.S.; Yadav, S.; Chintanaboina, J.; Maher, S.; Demuth, P.; Stern, B.; Stuart, A.; Tinsley, A.; Clarke, K.; et al. Influences and Impact of Anxiety and Depression in the Setting of Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2018, 24, 2303–2308. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Chun, J.; Han, K.; Park, S.; Soh, H.; Kim, J.; Lee, J.; Lee, H.J.; Im, J.P.; Kim, J.S. Risk of Anxiety and Depression in Patients with Inflammatory Bowel Disease: A Nationwide, Population-Based Study. J. Clin. Med. 2019, 8, 654. [Google Scholar] [CrossRef]
- Bannaga, A.S.; Selinger, C.P. Inflammatory bowel disease and anxiety: Links, risks, and challenges faced. Clin. Exp. Gastroenterol. 2015, 8, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Katon, W.; Ciechanowski, P. Impact of major depression on chronic medical illness. J. Psychosom. Res. 2002, 53, 859–863. [Google Scholar] [CrossRef]
- Patten, S.B.; Beck, C.A.; Kassam, A.; Williams, J.V.A.; Barbui, C.; Metz, L.M. Long-term medical conditions and major depression: Strength of association for specific conditions in the general population. Can. J. Psychiatry 2005, 50, 195–202. [Google Scholar] [CrossRef]
- Scott, K.M.; Bruffaerts, R.; Tsang, A.; Ormel, J.; Alonso, J.; Angermeyer, M.C.; Benjet, C.; Bromet, E.; de Girolamo, G.; de Graaf, R.; et al. Depression-anxiety relationships with chronic physical conditions: Results from the World Mental Health Surveys. J. Affect. Disord. 2007, 103, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Nahon, S.; Lahmek, P.; Durance, C.; Olympie, A.; Lesgourgues, B.; Colombel, J.F.; Gendre, J.P. Risk factors of anxiety and depression in inflammatory bowel disease. Inflamm. Bowel Dis. 2012, 18, 2086–2091. [Google Scholar] [CrossRef] [PubMed]
- Best, W.R.; Becktel, J.M.; Singleton, J.W.; Kern, F. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology 1976, 70, 439–444. [Google Scholar] [CrossRef]
- Kappelman, M.D.; Long, M.D.; Martin, C.; DeWalt, D.A.; Kinneer, P.M.; Chen, W.; Lewis, J.D.; Sandler, R.S. Evaluation of the patient-reported outcomes measurement information system in a large cohort of patients with inflammatory bowel diseases. Clin. Gastroenterol. Hepatol. 2014, 12, 1315–1323.e2. [Google Scholar] [CrossRef]
- Garrett, J.W.; Drossman, D.A. Health status in inflammatory bowel disease. Biological and behavioral considerations. Gastroenterology 1990, 99, 90–96. [Google Scholar] [CrossRef]
- Irvine, E.J.; Zhou, Q.; Thompson, A.K. The Short Inflammatory Bowel Disease Questionnaire: A quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am. J. Gastroenterol. 1996, 91, 1571–1578. [Google Scholar]
- Hjortswang, H.; Järnerot, G.; Curman, B.; Sandberg-Gertzén, H.; Tysk, C.; Blomberg, B.; Almer, S.; Ström, M. The Short Health Scale: A valid measure of subjective health in ulcerative colitis. Scand. J. Gastroenterol. 2006, 41, 1196–1203. [Google Scholar] [CrossRef]
- Guyatt, G.; Mitchell, A.; Irvine, E.J.; Singer, J.; Williams, N.; Goodacre, R.; Tompkins, C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology 1989, 96, 804–810. [Google Scholar] [CrossRef]
- Chen, X.L.; Zhong, L.H.; Wen, Y.; Liu, T.W.; Li, X.Y.; Hou, Z.K.; Hu, Y.; Mo, C.W.; Liu, F.B. Inflammatory bowel disease-specific health-related quality of life instruments: A systematic review of measurement properties. Health Qual. Life Outcomes 2017, 15, 177. [Google Scholar] [CrossRef]
- Glapa-Nowak, A.; Szczepanik, M.; Kwiecień, J.; Szaflarska-Popławska, A.; Flak-Wancerz, A.; Iwańczak, B.; Osiecki, M.; Kierkuś, J.; Pytrus, T.; Lebensztejn, D.; et al. Insolation and Disease Severity in Paediatric Inflammatory Bowel Disease-A Multi-Centre Cross-Sectional Study. J. Clin. Med. 2020, 9, 3957. [Google Scholar] [CrossRef]
- Byrne, G.; Rosenfeld, G.; Leung, Y.; Qian, H.; Raudzus, J.; Nunez, C.; Bressler, B. Prevalence of Anxiety and Depression in Patients with Inflammatory Bowel Disease. Can. J. Gastroenterol. Hepatol. 2017, 2017, 1–6. [Google Scholar] [CrossRef]
- Graff, L.A.; Walker, J.R.; Bernstein, C.N. Depression and anxiety in inflammatory bowel disease: A review of comorbidity and management. Inflamm. Bowel Dis. 2009, 15, 1105–1118. [Google Scholar] [CrossRef] [PubMed]
- Abautret-Daly, Á.; Dempsey, E.; Parra-Blanco, A.; Medina, C.; Harkin, A. Gut–brain actions underlying comorbid anxiety and depression associated with inflammatory bowel disease. Acta Neuropsychiatr. 2018, 30, 275–296. [Google Scholar] [CrossRef] [PubMed]
- Loftus, E.V.; Guérin, A.; Yu, A.P.; Wu, E.Q.; Yang, M.; Chao, J.; Mulani, P.M. Increased Risks of Developing Anxiety and Depression in Young Patients With Crohnʼs Disease. Am. J. Gastroenterol. 2011, 106, 1670–1677. [Google Scholar] [CrossRef] [PubMed]
- Morys, J.M.; Kaczówka, A.; Jeżewska, M. Assessment of selected psychological factors in patients with inflammatory bowel disease. Prz. Gastroenterol. 2016, 11, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Andrzejewska, J.; Talarska, D.; Michalak, M.; Linke, K. Quality of life in patients with Crohn’s disease and ulcerative colitis. Comparative analysis. Gastroenterol. Rev. Prz. Gastroenterol. 2009, 4, 251–255. [Google Scholar]
- Nordin, K.; Påhlman, L.; Larsson, K.; Sundberg-Hjelm, M.; Lööf, L. Health-Related Quality of Life and Psychological Distress in a Population-based Sample of Swedish Patients with Inflammatory Bowel Disease. Scand. J. Gastroenterol. 2002, 37, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Walker, E.A.; Roy-Byrne, P.P.; Katon, W.J.; Li, L.; Amos, D.; Jiranek, G. Psychiatric illness and irritable bowel syndrome: A comparison with inflammatory bowel disease. AJP 1990, 147, 1656–1661. [Google Scholar] [CrossRef]
- Addolorato, G.; Capristo, E.; Stefanini, G.F.; Gasbarrini, G. Inflammatory Bowel Disease: A Study of the Association between Anxiety and Depression, Physical Morbidity, and Nutritional Status. Scand. J. Gastroenterol. 1997, 32, 1013–1021. [Google Scholar] [CrossRef]
- Häuser, W.; Janke, K.-H.; Klump, B.; Hinz, A. Anxiety and depression in patients with inflammatory bowel disease: Comparisons with chronic liver disease patients and the general population. Inflamm. Bowel Dis. 2011, 17, 621–632. [Google Scholar] [CrossRef]
- Richman, L.S.; Kubzansky, L.; Maselko, J.; Kawachi, I.; Choo, P.; Bauer, M. Positive Emotion and Health: Going Beyond the Negative. Health Psychol. 2005, 24, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Ogińska-Bulik, N.; Juczyński, Z. Personality traits conducive to somatic diseases—The role of type D. Psychoonkologia 2008, 12, 7–13. [Google Scholar]
- Hauser, G.; Tkalcić, M.; Stimac, D.; Milić, S.; Sincić, B.M. Gender related differences in quality of life and affective status in patients with inflammatory bowel disease. Coll. Antropol. 2011, 35, 203–207. [Google Scholar] [PubMed]
- Bielińska, J.; Liebert, A.; Lesiewska, N.; Bieliński, M.; Mieczkowski, A.; Sopońska-Brzoszczyk, A.; Brzoszczyk, B.; Długosz, D.; Guenter, W.; Borkowska, A.; et al. Depressive and anxiety symptoms among patients with inflammatory bowel diseases. Med. Res. J. 2017, 2, 6–12. [Google Scholar]
- Lesage, A.-C.; Hagège, H.; Tucat, G.; Gendre, J.-P. Results of a national survey on quality of life in inflammatory bowel diseases. Clin. Res. Hepatol. Gastroenterol. 2011, 35, 117–124. [Google Scholar] [CrossRef]
- Muller, K.R.; Prosser, R.; Bampton, P.; Mountifield, R.; Andrews, J.M. Female gender and surgery impair relationships, body image, and sexuality in inflammatory bowel disease. Inflamm. Bowel Dis. 2010, 16, 657–663. [Google Scholar] [CrossRef]
- Becker, H.M.; Grigat, D.; Ghosh, S.; Kaplan, G.G.; Dieleman, L.; Wine, E.; Fedorak, R.N.; Fernandes, A.; Panaccione, R.; Barkema, H.W. Living with inflammatory bowel disease: A Crohn’s and Colitis Canada survey. Can. J. Gastroenterol. Hepatol. 2015, 29, 77–84. [Google Scholar] [CrossRef]
- Argyriou, K.; Kapsoritakis, A.; Oikonomou, K.; Manolakis, A.; Tsakiridou, E.; Potamianos, S. Disability in Patients with Inflammatory Bowel Disease: Correlations with Quality of Life and Patient’s Characteristics. Can. J. Gastroenterol. Hepatol. 2017, 2017, 1–11. [Google Scholar] [CrossRef]
- Brooks, A.J.; Rowse, G.; Ryder, A.; Peach, E.J.; Corfe, B.M.; Lobo, A.J. Systematic review: Psychological morbidity in young people with inflammatory bowel disease—Risk factors and impacts. Aliment. Pharmacol. Ther. 2016, 44, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Schäfer, M.; Schöls, M.; Köcke, J.; Elsenbruch, S.; Lauche, R.; Engler, H.; Dobos, G.; Langhorst, J. Randomised clinical trial: Yoga vs written self-care advice for ulcerative colitis. Aliment. Pharmacol. Ther. 2017, 45, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Elsenbruch, S.; Langhorst, J.; Popkirowa, K.; Müller, T.; Luedtke, R.; Franken, U.; Paul, A.; Spahn, G.; Michalsen, A.; Janssen, O.E.; et al. Effects of mind-body therapy on quality of life and neuroendocrine and cellular immune functions in patients with ulcerative colitis. Psychother. Psychosom. 2005, 74, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Langhorst, J.; Wulfert, H.; Lauche, R.; Klose, P.; Cramer, H.; Dobos, G.J.; Korzenik, J. Systematic review of complementary and alternative medicine treatments in inflammatory bowel diseases. J. Crohns Colitis 2015, 9, 86–106. [Google Scholar] [CrossRef] [PubMed]
| Variables Median (IQR) or n (%) | Crohn’s Disease n = 196 | Ulcerative Colitis n = 180 | p-Value |
|---|---|---|---|
| Age [years] | |||
| at inclusion | 15.0 (13.2–17.0) | 15.2 (11.7–16.8) | 0.0774 |
| at diagnosis | 12.4 (9.8–14.6) | 12.1 (8.1–14.9) | 0.4520 |
| at worst flare | 13.6 (11.5–15.9) | 13.8 (10.2–15.9) | 0.3694 |
| Duration of the disease (years) | 2.2 (0.7–4.2) | 1.7 (0.4–3.7) | 0.2430 |
| Sex | 75 (38.3) females | 80 (44.4) females | 0.2491 |
| Nutritional status | |||
| Weight at diagnosis (kg) | 38.8 (27.0–51.0) | 40.0 (28.8–54.0) | 0.5455 |
| Weight at diagnosis (z score) | −0.81 ([−1.38]–0.00) | −0.52 ([−1.14]–0.22) | 0.0106 |
| Height at diagnosis (cm) | 150.5 (136.0–166.0) | 151.5 (131.0–168.5) | 0.7550 |
| Height at diagnosis (z score) | −0.30 ([−1.20]–0.51) | 0.11 ([−0.67]–0.86) | 0.0042 |
| Body mass index at diagnosis (kg/m2) | 16.6 (14.6–18.4) | 17.3 (15.5–19.1) | 0.0407 |
| Body mass index at diagnosis (z score) | −0.79 ([−1.45]–[−0.03]) | −0.49 ([−1.02]–0.14) | 0.0169 |
| Albumin level at diagnosis (g/dL) | 3.9 (3.5–4.3) | 4.1 (3.7–4.41) | 0.0028 |
| Parameter of inflammation | |||
| CRP at diagnosis (mg/L) | 12.9 (2.0–30.3) | 2.1 (0.5–9.5) | <0.0001 |
| CRP at worst flare (mg/L) | 13.0 (3.0–35.0) | 2.7 (0.6–13.4) | <0.0001 |
| Disease activity scales | |||
| PCDAI/PUCAI at diagnosis | 30 (23–48) | 38 (30–53) | * |
| PCDAI/PUCAI at worst flare | 40 (30–53) | 56 (38–75) | * |
| Treatment | |||
| Systemic glucocorticosteroids ** | 107 (54.6) | 129 (71.7) | 0.0007 |
| Immunosuppressive treatment *** | 153 (78.1) | 103 (57.5) | <0.0001 |
| Biological therapy **** | 98 (50.0) | 46 (25.6) | <0.0001 |
| Operative treatment ***** | 24 (12.2) | 3 (1.7) | <0.0001 |
| Subjective psychophysical experiences at recruitment | |||
| Pain | 1 (0–2) | 1 (0–3) | 0.1528 |
| Anxiety | 2 (0–3) | 2 (1–5) | 0.0210 |
| Limitations at school/preschool activities | 1 (0–4) | 2 (0–6) | 0.0235 |
| Limitations in peer relationships | 0 (0–3) | 1 (0–5) | 0.0731 |
| Pain | p-Value | Anxiety | p-Value | Limitations in Peer Relationships | p-Value | Limitations in School Activities | p-Value | |
|---|---|---|---|---|---|---|---|---|
| IBD | ||||||||
| UC | 6 (4–8) | 0.637 | 5 (3–8) | 0.162 | 3 (0–7) | 0.472 | 5 (3–8) | 0.348 |
| CD | 6 (4–8) | 5 (2–7) | 3 (0–6) | 5 (2–8) | ||||
| Systemic glucocorticosteroids | ||||||||
| Yes | 7 (4–8) | 0.002 | 5 (3–8) | 0.105 | 4 (1–7) | 0.004 | 5 (3–8) | 0.057 |
| No | 6 (3–7) | 5 (2–7) | 2 (0–5) | 4 (1–8) | ||||
| Immunosuppressive treatment | ||||||||
| Yes | 7 (4–8) | <0.001 | 5 (3–8) | 0.009 | 4 (1–7) | <0.001 | 5 (3–8) | 0.103 |
| No | 5 (2–7) | 4 (2–6) | 2 (0–5) | 4 (1–8) | ||||
| Biological therapy | ||||||||
| Yes | 7 (4–8) | 0.015 | 5 (2–8) | 0.533 | 4 (1–7) | 0.007 | 5 (2–9) | 0.055 |
| No | 6 (3–8) | 5 (3–7) | 3 (0–5) | 4 (2–8) | ||||
| Surgery * | ||||||||
| Yes | 6 (4–7) | 0.291 | 5 (3–6) | 0.373 | 4 (1–6) | 0.536 | 6 (3–10) | 0.147 |
| No | 6 (4–8) | 5 (3–8) | 3 (0–6) | 5 (2–8) |
| Pain | p-Value | Anxiety | p-Value | Limitations in Peer Relationships | p-Value | Limitations in School Activities | p-Value | |
|---|---|---|---|---|---|---|---|---|
| IBD | ||||||||
| UC | 8 (6–9) | 0.661 | 7 (4–9) | 0.095 | 5 (2–8) | 0.556 | 8 (4–10) | 0.091 |
| CD | 8 (5–9) | 6 (4–8) | 5 (1–8) | 6 (3–9) | ||||
| Systemic glucocorticosteroids | ||||||||
| Yes | 8 (6–10) | <0.001 | 7 (5–9) | 0.015 | 6 (2–9) | 0.016 | 8 (4–10) | 0.005 |
| No | 8 (5–9) | 6 (3–8) | 4 (1–8) | 6 (2–9) | ||||
| Immunosuppressive treatment | ||||||||
| Yes | 8 (6–10) | <0.001 | 7 (5–9) | 0.031 | 6 (2–8) | 0.003 | 8 (4–10) | 0.003 |
| No | 8 (4–9) | 6 (3–8) | 3 (0–8) | 6 (1–9) | ||||
| Biological therapy | ||||||||
| Yes | 9 (7–10) | 4 × 10−5 | 7 (5–9) | 0.005 | 7 (2–9) | <0.001 | 9 (5–10) | 0.019 |
| No | 8 (5–9) | 6 (4–8) | 4 (1–8) | 6 (2–9) | ||||
| Surgery * | ||||||||
| Yes | 8 (7–10) | 0.610 | 7 (5–8) | 0.532 | 7 (4–9) | 0.083 | 9 (4–10) | 0.185 |
| No | 8 (6–9) | 7 (4–8) | 5 (1–8) | 7 (3-10) |
| Subjective Psychophysical Experiences | Treatment Parameter | p-Value | rho |
|---|---|---|---|
| Pain at diagnosis 1 | Number of glucocorticosteroid courses | 0.0005 | 0.18 |
| Number of immunosuppressants | 0.0011 | 0.17 | |
| Age at first immunosuppression | 0.0146 | −0.15 | |
| Number of biological agents | 0.0100 | 0.13 | |
| Pain at the worst flare 2 | Number of glucocorticosteroid courses | 0.0131 | 0.22 |
| Number of immunosuppressants | 0.0005 | 0.18 | |
| Number of biological agents | 0.0229 | 0.21 | |
| Anxiety at diagnosis 3 | Number of glucocorticosteroid courses | 0.0392 | 0.11 |
| Number of immunosuppressants | 0.0142 | 0.13 | |
| Age at first immunosuppression | 0.0268 | −0.14 | |
| Anxiety at the worst flare 4 | Number of immunosuppressants | 0.0220 | 0.23 |
| Age at first immunosuppression | 0.0085 | −0.17 | |
| Number of biological agents | 0.0070 | 0.14 | |
| Limitations in peer relationships at diagnosis 5 | Number of glucocorticosteroid courses | 0.0002 | 0.20 |
| Number of immunosuppressants | 0.0002 | 0.19 | |
| Time to first immunosuppression | 0.0455 | −0.13 | |
| Age at first immunosuppression | 0.0238 | −0.14 | |
| Number of biological agents | 0.0087 | 0.14 | |
| Limitations in peer relationships at the worst flare 6 | Number of glucocorticosteroid courses | 0.0220 | 0.23 |
| Number of biological agents | 0.0005 | 0.18 | |
| Age at first biological treatment | 0.0271 | −0.19 | |
| Limitations in school activities at diagnosis 7 | Number of glucocorticosteroid courses | 0.0100 | 0.13 |
| Number of immunosuppressants | 0.0360 | 0.11 | |
| Number of biological agents | 0.0494 | 0.10 | |
| Limitations in school activities at the worst flare 8 | Number of glucocorticosteroid courses | 0.0026 | 0.26 |
| Number of immunosuppressants | 0.0433 | 0.21 | |
| Age at first immunosuppression | 0.0247 | −0.14 | |
| Number of biological agents | 0.0143 | 0.23 | |
| Age at first biological treatment | 0.0281 | −0.19 |
| Subjective Psychophysical Experiences | Severity Parameter Per 1 Year of The Disease | p-Value | rho |
|---|---|---|---|
| Pain at diagnosis | Hospitalisations for relapse | 0.3182 | 0.07 |
| Days of hospitalisation for relapse | 0.4678 | 0.05 | |
| Relapses from diagnosis | 0.0671 | 0.13 | |
| Severe relapses from diagnosis | 0.1278 | 0.11 | |
| Pain at the worst flare | Hospitalisations for relapse | 0.0510 | 0.13 |
| Days of hospitalisation for relapse | 0.0243 | 0.15 | |
| Relapses from diagnosis | 0.0013 | 0.22 | |
| Severe relapses from diagnosis | 0.0123 | 0.17 | |
| Anxiety at diagnosis | Hospitalisations for relapse | 0.9622 | 0.00 |
| Days of hospitalisation for relapse | 0.8922 | –0.01 | |
| Relapses from diagnosis | 0.8685 | –0.01 | |
| Severe relapses from diagnosis | 0.4897 | 0.05 | |
| Anxiety at the worst flare | Hospitalisations for relapse | 0.3447 | 0.06 |
| Days of hospitalisation for relapse | 0.0412 | 0.14 | |
| Relapses from diagnosis | 0.1706 | 0.09 | |
| Severe relapses from diagnosis | 0.0097 | 0.18 | |
| Limitations in peer relationships at diagnosis | Hospitalisations for relapse | 0.0327 | 0.27 |
| Days of hospitalisation for relapse | 0.0047 | 0.32 | |
| Relapses from diagnosis | 0.0001 | 0.26 | |
| Severe relapses from diagnosis | 0.0016 | 0.22 | |
| Limitations in peer relationships at the worst flare | Hospitalisations for relapse | 0.0254 | 0.28 |
| Days of hospitalisation for relapse | 0.0019 | 0.35 | |
| Relapses from diagnosis | 0.0129 | 0.29 | |
| Severe relapses from diagnosis | 0.0048 | 0.19 | |
| Limitations in school activities at diagnosis | Hospitalisations for relapse | 0.0172 | 0.28 |
| Days of hospitalisation for relapse | 0.0165 | 0.30 | |
| Relapses from diagnosis | 0.0002 | 0.25 | |
| Severe relapses from diagnosis | 0.0657 | 0.13 | |
| Limitations in school activities at the worst flare | Hospitalisations for relapse | 0.0049 | 0.33 |
| Days of hospitalisation for relapse | 0.0004 | 0.39 | |
| Relapses from diagnosis | 0.0012 | 0.37 | |
| Severe relapses from diagnosis | 0.0078 | 0.30 |
| Subjective Psychophysical Experiences | Disease Activity Scale | p-Value | rho |
|---|---|---|---|
| Pain at diagnosis | PCDAI at worst flare | 0.0003 | 0.28 |
| Pain at worst flare | PCDAI at worst flare | 0.0159 | 0.19 |
| Limitations in peer relationships at diagnosis | PCDAI at diagnosis | 0.0213 | 0.17 |
| PCDAI at worst flare | 0.0109 | 0.20 | |
| Limitations in school activities at diagnosis | PCDAI at worst flare | 0.0373 | 0.17 |
| Limitations in school activities at worst flare | PCDAI at worst flare | 0.0052 | 0.22 |
| Pain at diagnosis | PUCAI at worst flare | 0.0160 | 0.20 |
| Pain at the worst flare | PUCAI at diagnosis | 0.0122 | 0.20 |
| PUCAI at worst flare | 0.0278 | 0.33 | |
| Anxiety at the worst flare | PUCAI at diagnosis | 0.0210 | 0.18 |
| PUCAI at worst flare | 0.0433 | 0.32 | |
| Limitations in peer relationships at diagnosis | PUCAI at diagnosis | 0.0048 | 0.22 |
| PUCAI at worst flare | 0.0425 | 0.17 | |
| Limitations in peer relationships at the worst flare | PUCAI at diagnosis | 0.0137 | 0.19 |
| PUCAI at worst flare | 0.0263 | 0.18 | |
| Limitations in school activities at diagnosis | PUCAI at diagnosis | 0.0373 | 0.17 |
| Limitations in school activities at the worst flare | PUCAI at diagnosis | 0.0007 | 0.27 |
| PUCAI at worst flare | 0.0001 | 0.31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Glapa-Nowak, A.; Bukowska-Posadzy, A.; Szczepanik, M.; Kwiecień, J.; Szaflarska-Popławska, A.; Iwańczak, B.; Flak-Wancerz, A.; Dembiński, Ł.; Osiecki, M.; Kierkuś, J.; et al. Subjective Psychophysical Experiences in the Course of Inflammatory Bowel Disease—A Comparative Analysis Based on the Polish Pediatric Crohn’s and Colitis Cohort (POCOCO). Int. J. Environ. Res. Public Health 2021, 18, 784. https://doi.org/10.3390/ijerph18020784
Glapa-Nowak A, Bukowska-Posadzy A, Szczepanik M, Kwiecień J, Szaflarska-Popławska A, Iwańczak B, Flak-Wancerz A, Dembiński Ł, Osiecki M, Kierkuś J, et al. Subjective Psychophysical Experiences in the Course of Inflammatory Bowel Disease—A Comparative Analysis Based on the Polish Pediatric Crohn’s and Colitis Cohort (POCOCO). International Journal of Environmental Research and Public Health. 2021; 18(2):784. https://doi.org/10.3390/ijerph18020784
Chicago/Turabian StyleGlapa-Nowak, Aleksandra, Anna Bukowska-Posadzy, Mariusz Szczepanik, Jarosław Kwiecień, Anna Szaflarska-Popławska, Barbara Iwańczak, Anna Flak-Wancerz, Łukasz Dembiński, Marcin Osiecki, Jarosław Kierkuś, and et al. 2021. "Subjective Psychophysical Experiences in the Course of Inflammatory Bowel Disease—A Comparative Analysis Based on the Polish Pediatric Crohn’s and Colitis Cohort (POCOCO)" International Journal of Environmental Research and Public Health 18, no. 2: 784. https://doi.org/10.3390/ijerph18020784
APA StyleGlapa-Nowak, A., Bukowska-Posadzy, A., Szczepanik, M., Kwiecień, J., Szaflarska-Popławska, A., Iwańczak, B., Flak-Wancerz, A., Dembiński, Ł., Osiecki, M., Kierkuś, J., Banasiewicz, T., Walach, H., Banaszkiewicz, A., & Walkowiak, J. (2021). Subjective Psychophysical Experiences in the Course of Inflammatory Bowel Disease—A Comparative Analysis Based on the Polish Pediatric Crohn’s and Colitis Cohort (POCOCO). International Journal of Environmental Research and Public Health, 18(2), 784. https://doi.org/10.3390/ijerph18020784






