New Perspective on Why Women Live Longer Than Men: An Exploration of Power, Gender, Social Determinants, and Capitals
Abstract
1. Introduction
Background
2. Methods
2.1. Global Analysis of Gendered Differences in Life Expectancy
2.2. Comparative Case Analysis
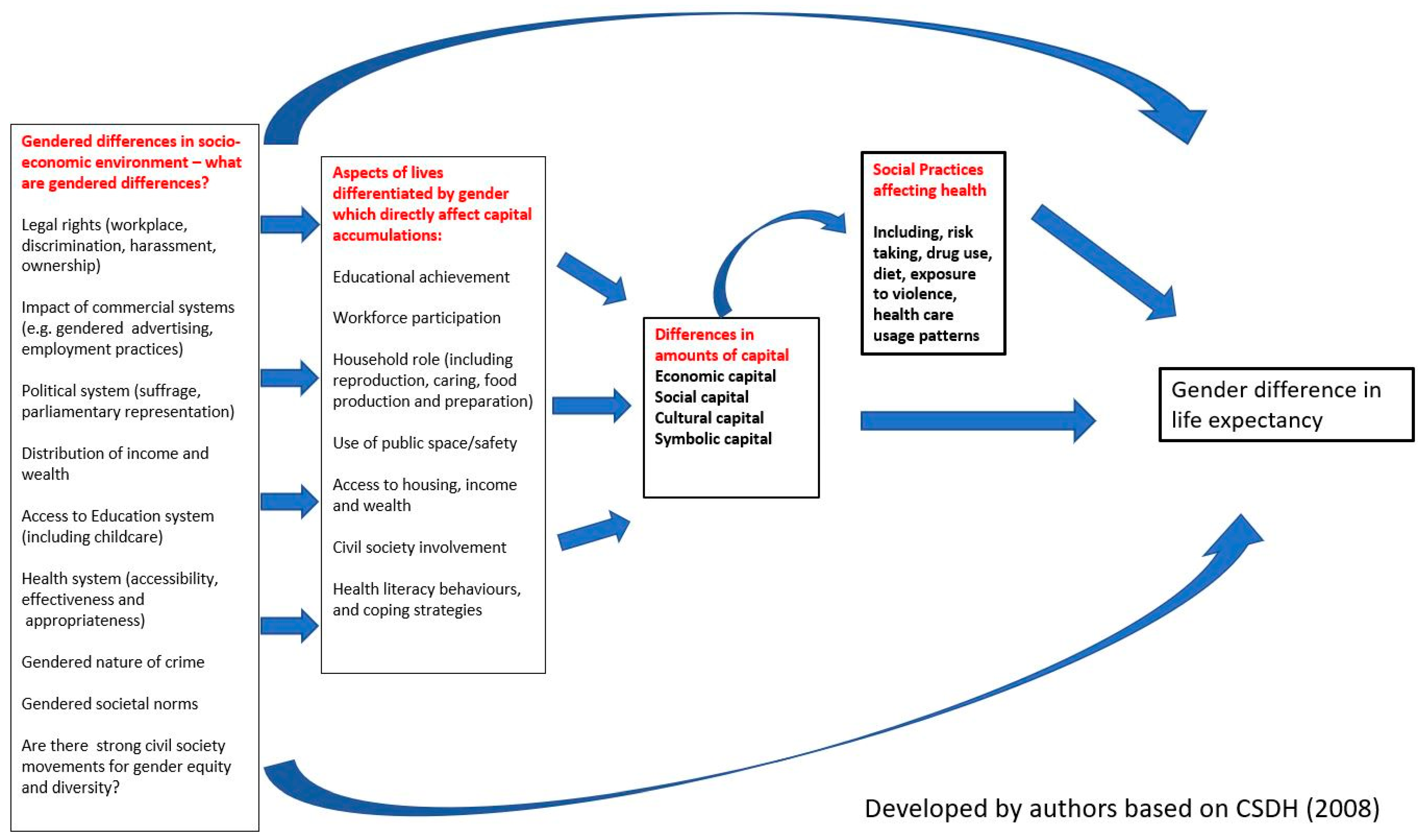
2.2.1. Theoretical Framework for the Comparative Case Analysis
- Economic capital, which refers to material and financial resources.
- Cultural capital, including education, literacy skills and possession of items of distinction.
- Social capital, which is gained from relationships and networks and can be tight knit bonding capital or bridging capital, extended across class, groups and “agencies”.
- Symbolic is the power that comes from the deployment of any form of capital and is associated with honour, prestige, or recognition. It symbolises the value that a person holds within a social field [32].
2.2.2. Ethics
3. Findings
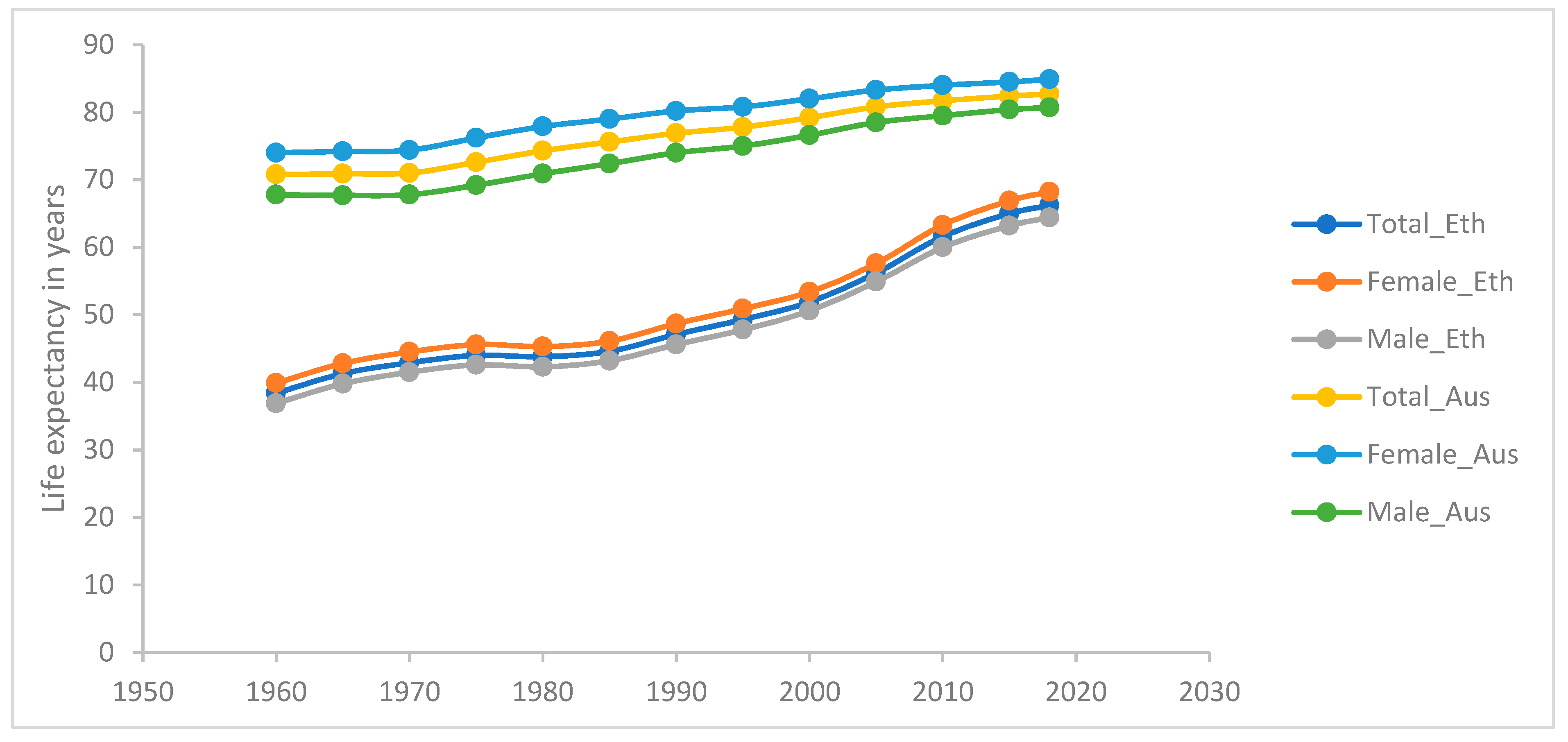
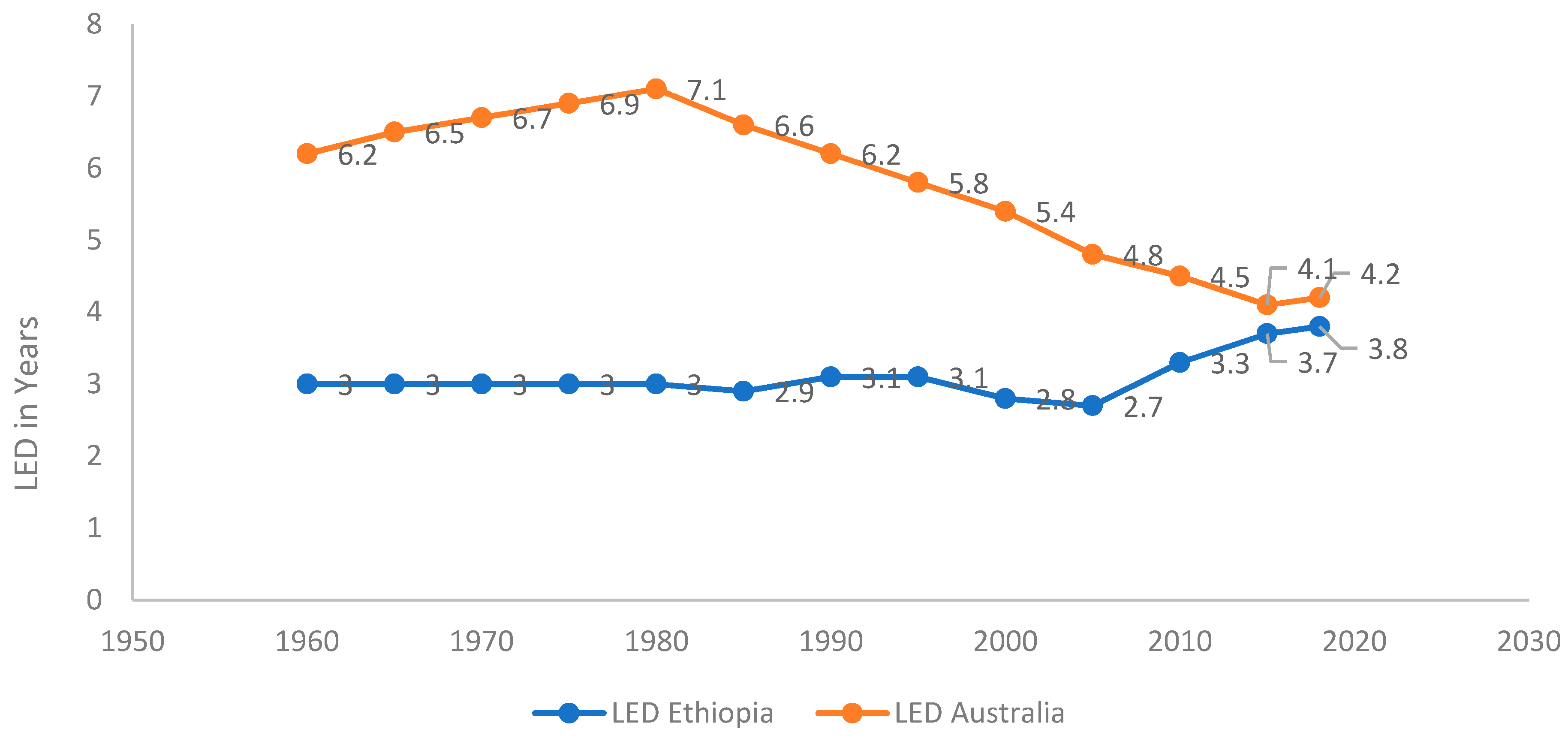
3.1. Global Picture of Gendered Life Expectancy Difference (GLED)
3.2. Comparative Case Analyses: Australia and Ethiopia
3.2.1. Epidemiological Perspective
Measures of Gender Equity
3.2.2. Sociological Perspective Extending Legal and Political Rights: for Women
The Role of Health Systems
Exploring Gendered Everyday Practices through the Lens of Bourdieu’s Capitals
Economic Capital
Cultural Capital
Social Capital
Symbolic Capital
3.3. Gendered Social Health Practices
- Physical activity: 5 in 10 men and 4 in 10 women were sufficiently physically active. (2017–2018).
- Diet: fewer than 1 in 30 men and 1 in 15 women ate enough fruit and vegetables; 12% of males and 6.4% of females were daily consumers of sweetened drinks (2017–2018).
- Smoking: men were 1.5 times as likely to smoke daily as women, but smoking rates have declined overall.
- Weight: 7 in 10 men and 6 in 10 women were overweight or obese (2017–2018).
- Alcohol use: 1 in 4 men and 1 in 11 women were consuming alcohol at levels placing them at lifetime risk of an alcohol-related disease or injury (decreasing over time) (2017–2018).
- Violence: 4 in 10 men and 3 in 10 women had experienced physical violence since the age of 15. 4.7% of men and 18% of women had experienced sexual violence since the age of 15 (2016).
- Self-rated health: males and females were equally likely to rate their health as excellent or very good (2017–2018).
- Smoking: 4% of men and 1% of women reported smoking [78].
- Weight: 21%of women and 12% of men in urban Ethiopia are overweight or obese [78].
- Sexual violence: the prevalence rate of rape among boys was 4.3% [115], the prevalence rates of life time (age 15+ years) and 12 months physical violence among women in Ethiopia in 2016 were 20% and 15%, respectively; and the life time and 12 months sexual violence rates were 10% and 7% respectively [78].
- Alcohol use: a systematic review and meta-analysis conducted in 2019 found that the prevalence of hazardous alcohol consumption in men and women was 11.6% and 1.2%, respectively [116].
4. Discussion
4.1. Data Considerations
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smits, J.; Monden, C. Length of life inequality around the globe. Soc. Sci. Med. 2009, 68, 1114–1123. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpoor, A.R.; Harper, S.; Lee, J.H.; Lynch, J.; Mathers, C.; Abou-Zahr, C. International shortfall inequality in life expectancy in women and in men, 1950–2010. Bull. World Health Organ. 2012, 90, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Barford, A.; Dorling, D.; Smith, G.D.; Shaw, M. Life expectancy: Women now on top everywhere. BMJ 2006, 332, 808. [Google Scholar] [CrossRef] [PubMed]
- Lewer, D.; Jayatunga, W.; Aldridge, R.W.; Edge, C.; Marmot, M.; Story, A.; Hayward, A. Premature mortality attributable to socioeconomic inequality in England between 2003 and 2018: An observational study. Lancet Public Health 2020, 5, e33–e41. [Google Scholar] [CrossRef]
- Cullen, M.R.; Baiocchi, M.; Eggleston, K.; Loftus, P.; Fuchs, V. The weaker sex? Vulnerable men and women’s resilience to socio-economic disadvantage. SSM Popul. Health 2016, 2, 512–524. [Google Scholar] [CrossRef]
- Austad, S.N. Why women live longer than men: Sex differences in longevity. Gend. Med. 2006, 3, 79–92. [Google Scholar] [CrossRef]
- Dobson, R. Men are more likely than women to die early. BMJ 2006, 333, 220. [Google Scholar]
- Kalben, B.B. Why Men die younger. N. Am. Actuar. J. 2000, 4, 83–111. [Google Scholar] [CrossRef]
- Annandale, E.; Hunt, K. Gender Inequalities in Health; Open University Press: Buckingham, UK, 2000. [Google Scholar]
- Hawkes, S.; Allotey, P.; Elhadj, A.S.; Clark, J.; Horton, R. The lancet commission on gender and global health. Lancet 2020, 396, 521–522. [Google Scholar] [CrossRef]
- CSDH. Closing the Gap in a Generation; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Gove, W.R.; Hughes, M. Possible causes of the apparent sex differences in physical health: An empirical investigation. Am. Sociol. Rev. 1979, 44, 126–146. [Google Scholar] [CrossRef]
- Waldron, I. Why do women live longer than men? Soc. Sci. Med. 1976, 10, 349–362. [Google Scholar] [CrossRef]
- Walsh, D.C.; Sorenson, G. Gender, health and cigarette smoking. In Society and Health; Amick, B., Levine, S., Eds.; Oxford University Press: New York, NY, USA, 1995; pp. 131–171. [Google Scholar]
- Verbrugge, L.M. Gender and health: An update on hypotheses and evidence. J. Health Soc. Behav. 1985, 26, 156–182. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.G.; Everett, B.G.; Saint Onge, J.M.; Krueger, P.M. Social, behavioral, and biological factors, and sex differences in mortality. Demography 2010, 47, 555–578. [Google Scholar] [CrossRef]
- Krieger, N. Epidemiology and the People’s Health: Theory and Context; Oxford University Press: New York, NY, USA, 2011. [Google Scholar]
- Macintyre, S. The patterning of health by social position in contemporary Britain: Directions for sociological research. Soc. Sci. Med. 1986, 23, 393–415. [Google Scholar] [CrossRef]
- Drever, F.; Doran, T.; Whitehead, M. Exploring the relation between class, gender, and self rated general health using the new socioeconomic classification. A study using data from the 2001 census. J. Epidemiol. Community Health 2004, 58, 590–596. [Google Scholar] [CrossRef][Green Version]
- Connell, R. Gender, health and theory: Conceptualizing the issue, in local and world perspective. Soc. Sci. Med. 2012, 74, 1675–1683. [Google Scholar] [CrossRef]
- Hankivsky, O. Women’s health, men’s health, and gender and health: Implications of intersectionality. Soc. Sci. Med. 2012, 74, 1712–1720. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.; Horton, R. A coming of age for gender in global health. Lancet 2019, 393, 2367–2369. [Google Scholar] [CrossRef]
- Bates, L.M.; Hankivsky, O.; Springer, K.W. Gender and health inequities: A comment on the Final Report of the WHO Commission on the Social Determinants of Health. Soc. Sci. Med. 2009, 69, 1002–1004. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, S.; Buse, K. The politics of gender and global health. In The Oxford Handbook of Global Health Politics; McInnes, C., Lee, K., Eds.; Oxford University Press: New York, NY, USA, 2020; pp. 237–264. [Google Scholar]
- Popay, J.; Groves, K. ‘Narrative’ in research on gender inequalities in health. In Gender Inequalities in Health; Open University Press: Buckingham, UK, 2000; pp. 64–89. [Google Scholar]
- Risman, B.J.; Froyum, C.M.; Scarborough, W.J. Handbook of the Sociology of Gender, 2nd ed.; Springer Nature: Cham, Switzerland, 2018. [Google Scholar]
- Hart, C.G.; Saperstein, A.; Magliozzi, D.; Westbrook, L. Gender and health: Beyond binary categorical measurement. J. Health Soc. Behav. 2019, 60, 101–118. [Google Scholar] [CrossRef]
- Courtenay, W.H. Constructions of masculinity and their influence on men’s well-being: A theory of gender and health. Soc. Sci. Med. 2000, 50, 1385–1401. [Google Scholar] [CrossRef]
- Springer, K.W.; Hankivsky, O.; Bates, L.M. Gender and health: Relational, intersectional, and biosocial approaches. Soc. Sci. Med. 2012, 74, 1661–1666. [Google Scholar] [CrossRef] [PubMed]
- Connell, R.W.; Messerschmidt, J.W. Hegemonic masculinity:Rethinking the concept. Gend. Soc. 2005, 19, 829–859. [Google Scholar] [CrossRef]
- Gilmore, A.B.; Fooks, G.; Drope, J.; Bialous, S.A.; Jackson, R.R. Exposing and addressing tobacco industry conduct in low-income and middle-income countries. Lancet 2015, 385, 1029–1043. [Google Scholar] [CrossRef]
- Bourdieu, P. The forms of capital. In Handbook of Theory and Research for Sociology of Education; Richardson, J., Ed.; Greenwood Press: New York, NY, USA, 1986. [Google Scholar]
- Laberge, S. Toward an Integration of Gender into Bourdieu’s Concept of Cultural Capital. Sociol. Sport J. 1995, 12, 132. [Google Scholar] [CrossRef]
- Oncini, F.; Guetto, R. Cultural capital and gender differences in health behaviours: A study on eating, smoking and drinking patterns. Health Sociol. Rev. 2018, 27, 15–30. [Google Scholar] [CrossRef]
- Wiltshire, G.; Lee, J.; Williams, O. Understanding the reproduction of health inequalities: Physical activity, social class and Bourdieu’s habitus. Sport Educ. Soc. 2019, 24, 226–240. [Google Scholar] [CrossRef]
- Abel, T. Cultural capital and social inequality in health. J. Epidemiol. Community Health 2008, 62, e13. [Google Scholar] [CrossRef]
- Schneider-Kamp, A. Health capital: Toward a conceptual framework for understanding the construction of individual health. Soc. Theory Health 2020, 1–15. [Google Scholar] [CrossRef]
- Shim, J.K. Cultural health capital: A theoretical approach to understanding health care interactions and the dynamics of unequal treatment. J. Health Soc. Behav. 2010, 51, 1–15. [Google Scholar] [CrossRef]
- Turner, B. Social Capital, inequality and health: The durkheimian revival. Soc. Theory Health 2003, 1, 4–20. [Google Scholar] [CrossRef]
- Pinxten, W.; Lievens, J. The importance of economic, social and cultural capital in understanding health inequalities: Using a Bourdieu-based approach in research on physical and mental health perceptions. Sociol. Health Illn. 2014, 36, 1095–1110. [Google Scholar] [CrossRef] [PubMed]
- Bartley, M. Health Inequality: An Introduction to Concepts, Theory and Methods; Polity Press: Cambridge, UK, 2004. [Google Scholar]
- Thorslund, M.; Wastesson, J.W.; Agahi, N.; Lagergren, M.; Parker, M.G. The rise and fall of women’s advantage: A comparison of national trends in life expectancy at age 65 years. Eur. J. Ageing 2013, 10, 271–277. [Google Scholar] [CrossRef] [PubMed]
- ABS (Australian Bureau of Statistics). Life Tables Statistics About Life Tables for Australia, States and Territories and Life Expectancy at birth Estimates for Sub-State Regions. Available online: https://www.abs.gov.au/statistics/people/population/life-tables/latest-release (accessed on 13 January 2021).
- Worldbank. Life Expectancy at Birth, Total (Years). Available online: https://data.worldbank.org/indicator/SP.DYN.LE00.IN (accessed on 30 September 2020).
- Adair, T.; Lopez, A. Widening inequalities in premature mortality in Australia, 2006–2016. Aust. Popul. Stud. 2020, 4, 37–56. [Google Scholar] [CrossRef]
- AIHW (Australian Institute of Health and Welfare). Australia’s Health 2020: Indigenous Health; AIHW: Canberra, Australia, 2012.
- Stephens, A.S.; Gupta, L.; Thackway, S.; Broome, R.A. Socioeconomic, remoteness and sex differences in life expectancy in New South Wales, Australia, 2001–2012: A population-based study. BMJ Open 2017, 7, e013227. [Google Scholar] [CrossRef]
- Tranvåg, E.J.; Ali, M.; Norheim, O.F. Health inequalities in Ethiopia: Modeling inequalities in length of life within and between population groups. Int. J. Equity Health 2013, 12, 52. [Google Scholar] [CrossRef]
- Weldearegawi, B.; Spigt, M.; Berhane, Y.; Dinant, G. Mortality level and predictors in a rural Ethiopian population: Community based longitudinal study. PLoS ONE 2014, 9, e93099. [Google Scholar] [CrossRef]
- Melaku, Y.A.; Sahle, B.W.; Tesfay, F.H.; Bezabih, A.M.; Aregay, A.; Abera, S.F.; Abreha, L.; Zello, G.A. Causes of death among adults in northern Ethiopia: Evidence from verbal autopsy data in health and demographic surveillance system. PLoS ONE 2014, 9, e106781. [Google Scholar] [CrossRef]
- Frank, T.D.; Carter, A.; Jahagirdar, D.; Biehl, M.H.; Douwes-Schultz, D.; Larson, S.L.; Arora, M.; Dwyer-Lindgren, L.; Steuben, K.M.; Abbastabar, H.; et al. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: A systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV 2017, 6, E831–E859. [Google Scholar] [CrossRef]
- UNDP The 2018 United Nations Development Program Human Development Index. Available online: http://hdr.undp.org/en/content/human-development-index-hdi (accessed on 11 May 2020).
- Russell, L. Sociology Health Professionals; SAGE Publications: London, UK, 2014. [Google Scholar]
- ABS (Australian Bureau of Statistics). Gender Indicators, Australia; Atalogue Number 4125.0; ABS: Canberra, Australia, 2019.
- Nicola, J.; Taveeshi, G.; Bekele, T. Evaluation of Norway’s Support to Women’s Rights and Gender Equality in Development Cooperation Ethiopia Case Study Report; NORAD: Addis Ababa, Ethiopia, 2015. [Google Scholar]
- IPU Percentage of Women in National Parliaments. Available online: https://data.ipu.org/women-ranking?month=9&year=2019 (accessed on 24 October 2020).
- FDRE. National Report on the Implementation of the Beijing Declaration and Platform for Action (1995) and the Outcome of the 23rd Special Session of the United Nations General Assembly (2000); FDRE: Addis Ababa, Ethiopia, 2014.
- Chalachew Getahun, D. The urban informal economy in Ethiopia: Theory and empirical evidence. East. Afr. Soc. Sci. Res. Rev. 2018, 34, 37–64. [Google Scholar]
- MOWCY. Ethiopia and SPRI: Gender Equality, Women’s Empowerment and Child Wellbeing in Ethiopia; UNICEF: Nairobi, Kenya, 2019. [Google Scholar]
- Gray Jamieson, G. The Australian Women’s Health Movement and Public Policy; ANU E Press: Canberra, Australia, 2012. [Google Scholar]
- Duckett, S.; Willcox, S. The Australian Health Care System, 4th ed.; Oxford University Press: South Melbourne, VIC, Australia, 2011. [Google Scholar]
- ABS (Australian Bureau of Statistics). Patient Experiences in Australia: Summary of Findings, 2018–2019; ABS: Canberra, Australia, 2019.
- Ali, E.E. Health care financing in ethiopia: Implications on access to essential medicines. Value Health Reg. Issues 2014, 4, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Hailu, Z. Health Care Financing Reform in Ethiopia: Improving Quality and Equity; USAID: Washington, WA, USA, 2012. [Google Scholar]
- Mebratie, A.D.; Sparrow, R.; Yilma, Z.; Alemu, G.; Bedi, A.S. Enrollment in Ethiopia’s Community-Based Health Insurance Scheme. World Dev. 2015, 74, 58–76. [Google Scholar] [CrossRef]
- Mebratie, A.D.; Sparrow, R.; Yilma, Z.; Abebaw, D.; Alemu, G.; Bedi, A.S. The impact of Ethiopia’s pilot community based health insurance scheme on healthcare utilization and cost of care. Soc. Sci. Med. 2019, 220, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Woldemichael, A.; Takian, A.; Akbari Sari, A.; Olyaeemanesh, A. Inequalities in healthcare resources and outcomes threatening sustainable health development in Ethiopia: Panel data analysis. BMJ Open 2019, 9, e022923. [Google Scholar] [CrossRef] [PubMed]
- FDRE/MOH. Health Sector Transformation Plan I Annual Performance Report, EFY 2008 (2015/16), VERSION 1; Federal Democratic Republic of Ethiopia, Minstry of Health: Addis Ababa, Ethiopia, 2017; pp. 30–33. [Google Scholar]
- Onarheim, K.H.; Taddesse, M.; Norheim, O.F.; Abdullah, M.; Miljeteig, I. Towards universal health coverage for reproductive health services in Ethiopia: Two policy recommendations. Int. J. Equity Health 2015, 14, 86. [Google Scholar] [CrossRef]
- Kibret, G.D.; Leshargie, C.T.; Wagnew, F.; Alebel, A. Willingness to join community based health insurance and its determinants in East Gojjam zone, Northwest Ethiopia. BMC Res. Notes 2019, 12, 31. [Google Scholar] [CrossRef] [PubMed]
- ABS (Australian Bureau of Statistics). Labour Force Survey, Australia; ABS: Canberra, Australia, 2020. [Google Scholar]
- Dawson, E.; Kovac, T.; Lewis, A. Measure For Measure: Gender Equality in Australia; Per Capita: Melbourne, Australia, March 2020. [Google Scholar]
- OECD. Net Childcare Costs (Indicator); OECD: Paris, France, 2020. [Google Scholar]
- Workplace Gender Equality Agency. Australia’s Gender Pay Gap Statistics 2020; Commonwealth of Australia: Canberra, Australia, 2020. [Google Scholar]
- ABS (Australian Bureau of Statistics). Labour Force, Australia: Labour Force Status and Other Characteristics of Families; Australian Bureau of Statistics: Sydney, Australia, 2020.
- Sebastian, A.; Ziv, I. One in Eight: Australian Single Mothers’ Lives Revealed. Report of a National Survey Undertaken in 2018 by the Council of Single Mothers and Their Children; State Government Victoria: Melbourne, Australia, November 2019.
- Feldman, S.; Radermacher, H. Time of Our Lives? Building Opportunity and Capacity for the Economic and Social Partic-Ipation of Older Australian Women; Lord Mayor’s Charitable Foundation: Melbourne, Australia, 2016. [Google Scholar]
- CSA; ICF. Ethiopian Demographic Health Survey 2016; Central Statistical Agency (Ethiopia): Addis Ababa, Ethiopia; ICF International: Calverton, Ethiopia, 2018.
- Lailulo, Y.A.; Sathiya Susuman, A.; Blignaut, R. Correlates of gender characteristics, health and empowerment of women in Ethiopia. BMC Women’s Health 2015, 15, 116. [Google Scholar] [CrossRef]
- IMF. The Federal Democratic Republic of Ethiopia; IMF: Washington, WA, USA, 2018. [Google Scholar]
- Pocock, B.; Williams, P.; Skinner, N. Time Bomb: Work, Rest and Play in Australia Today; NewSouth: Sydney, NSW, Australia, 2012. [Google Scholar]
- Marmot, M. Status Syndrome: How Your Social Standing Directly Affects Your Health and Life Expectancy; Bloomsbury: London, UK, 2004. [Google Scholar]
- Doyal, L. Hazards of Hearth and Home. In What Makes Women Sick: Gender and the Political Economy of Health; Macmillan Education UK: London, UK, 1995; pp. 27–58. [Google Scholar]
- Phillips, S.P. Risky business: Explaining the gender gap in longevity. J. Men’s Health Gend. 2006, 3, 43–46. [Google Scholar] [CrossRef]
- Davey Smith, G. Income inequality and mortality: Why are they related? Br. Med. J. 1996, 312, 987–988. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Goldblatt, P. A social movement, based on evidence, to reduce inequalities in health. Soc. Sci. Med. 2010, 71, 1254–1258. [Google Scholar] [CrossRef]
- Wilkinson, R.G. Income distribution and life expectancy. In The Society and Population Health Reader; New Press: New York, NY, USA, 1999. [Google Scholar]
- Chetty, R.; Stepner, M.; Abraham, S.; Lin, S.; Scuderi, B.; Turner, N.; Bergeron, A.; Cutler, D. The association between income and life expectancy in the United States, 2001–2014. JAMA 2016, 315, 1750–1766. [Google Scholar] [CrossRef] [PubMed]
- UNESCO. Adult and Youth Literacy: National, Regional and Global Trends, 1985–2015; Institute for Statistics: Montreal, QC, Canada, 2013. [Google Scholar]
- Karin, H.; Dehab, B.; Asegedech, B.; Anbesu, B.; Nuri, K. Taking Stock of Girls’ Education in Ethiopia: Preparing for ESD P III; UNESCO: Addis Ababa, Ethiopia, 2005. [Google Scholar]
- UNICEF Ethiopia: Statistics. Available online: http://www.unicef.org/infobycountry/ethiopia_statistics.html (accessed on 30 May 2020).
- Medhanyie, A.; Spigt, M.; Kifle, Y.; Schaay, N.; Sanders, D.; Blanco, R.; GeertJan, D.; Berhane, Y. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: A cross sectional study. BMC Health Serv. Res. 2012, 12, 352. [Google Scholar] [CrossRef]
- Negussie, A.; Girma, G. Is the role of health extension workers in the delivery of maternal and child health care services a significant attribute? The case of Dale district, southern Ethiopia. BMC Health Serv. Res. 2017, 17, 641. [Google Scholar] [CrossRef] [PubMed]
- UNESCO. Ethiopia: Literacy Rate among the Population Aged 15 Years and Older; UNESCO Institute of Statistics: Montreal, QC, Canada, 2020. [Google Scholar]
- Abraha, A. Gender Inequalities in Tertiary Education in Ethiopia: Mediating the Transition to University through the Development of Adaptive Competencies; Center for Universal Education, Brookings Instituion: Washington, DC, USA, 2012. [Google Scholar]
- Conceição, P.; Hall, J.; Hsu, Y.; Jahic, A.; Kovacevic, M.; Mukhopadhyay, T.; Ortubia, A.; Rivera, C.; Tapia, H. Human Development Perspectives. Tackling Social Norms: A Game Changer for Gender Inequalities; United Nations Development Programme: New York, NY, USA, 2020. [Google Scholar]
- Denton, M.; Walters, V. Gender differences in structural and behavioral determinants of health: An analysis of the social production of health. Soc. Sci. Med. 1999, 48, 1221–1235. [Google Scholar] [CrossRef]
- Berry, H.L.; Welsh, J.A. Social capital and health in Australia: An overview from the household, income and labour dynamics in Australia survey. Soc. Sci. Med. 2010, 70, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Baker, D. All the Lonely People: Loneliness in Australia, 2001–2009; The Australia Institute: Canberra, Australia, 2012. [Google Scholar]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
- Osborne, K.; Ziersch, A.; Baum, F. Who participates? Socioeconomic factors associated with women’s participation in voluntary groups. Aust. J. Soc. Issues 2008, 43, 103–122. [Google Scholar] [CrossRef]
- ABS (Australia Bureau of Statistics). Characteristics of Employment, Australia; ABS: Canberra, Australia, 2016.
- Maddison, S.; Sawer, M. The Women’s Movement in Protest, Institutions and the Internet Australia in Transnational Perspective; Routledge: Oxfordshire, UK, 2013. [Google Scholar]
- Dodd, V. Social Capital and Subjective Well-Being: The Case of Rural Ethiopia; Clemson University: Clemson, SC, USA, 2012. [Google Scholar]
- Jeffrey, C. Civil Society, NGOs, and Development in Ethiopia; The International Bank for Reconstruction and Development/THE WORLD BANK: New York, NY, USA, 2000. [Google Scholar]
- Dawson, E.L. Gender, diversity, and sustainable civil society strengthening: Lessons from Ethiopia. Dev. Pract. 2016, 26, 629–636. [Google Scholar] [CrossRef]
- ABS (Australian Bureau of Statistics). Disability, Ageing and Carers, Australia: Summary of Findings; Australian Bureau of Statistics, Ed.; Australian Government: Canberra, Australia, 2016.
- Mohanty, I.; Niyonsenga, T. A longitudinal analysis of mental and general health status of informal carers in Australia. BMC Public Health 2019, 19, 1436. [Google Scholar] [CrossRef]
- IES, The Cultural Atlas. Ethiopian Culture. In SBS Australia; IES: Canberra, Australia, 2020. [Google Scholar]
- Brides, G.N. What’s The Child Marriage Rate? How Big of an Issue Is Child Marriage? Available online: https://www.girlsnotbrides.org/child-marriage/ethiopia/ (accessed on 19 October 2020).
- Swain, S. Single Mothers and Their Children: Disposal, Punishment and Survival in Australia; Cambridge University Press: Melbourne, Australia, 1995. [Google Scholar]
- Luke Henriques-Gomes. Demeaning’ Welfare Crackdown on Single Parents Finds Only 1.3% Were Breaking Rules. Available online: https://www.theguardian.com/australia-news/2020/jan/23/coalitions-demeaning-parenting-payment-crackdown-falling-short-of-estimated-savings (accessed on 13 January 2021).
- Sen, G.; Östlin, P.; George, A. Unequal, Unfair, Ineffective and Inefficient Gender Inequity in Health: Why It Exists And how We Can Change It. Final Report to the WHO Commission on Social Determinants of Health. Women and Gender Equity Knowledge Network; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- AIHW (Australian Institute of Health and Welfare). The Health of Australia’s Females; AIHW: Canberra, Australia, 2019.
- Haile, R.T.; Kebeta, N.D.; Kassie, G.M. Prevalence of sexual abuse of male high school students in Addis Ababa, Ethiopia. BMC Int. Health Hum. Rights 2013, 13, 24. [Google Scholar] [CrossRef]
- Ayano, G.; Yohannis, K.; Abraha, M.; Duko, B. The epidemiology of alcohol consumption in Ethiopia: A systematic review and meta-analysis. Subst. Abus. Treat. Prev. Policy 2019, 14, 26. [Google Scholar] [CrossRef] [PubMed]
- Mokdad A, Bcheraoui C, Wang H; Murray, C.J.L. Trends in HIV/AIDS morbidity and mortality in Eastern Mediterranean countries, 1990-2015: Findings from the Global Burden of Disease 2015 Study. Available online: http://www.healthdata.org/research-article/trends-hivaids-morbidity-and-mortality-eastern-mediterranean-countries-1990-2015 (accessed on 13 January 2021).
- Prina, A.M.; Cosco, T.D.; Dening, T.; Beekman, A.; Brayne, C.; Huisman, M. The association between depressive symptoms in the community, non-psychiatric hospital admission and hospital outcomes: A systematic review. J. Psychosom. Res. 2015, 78, 25–33. [Google Scholar] [CrossRef]
- Greenhalgh, E.; Bayly, M.; Winstanley, M. Tobacco in Australia: Facts and Issues; Cancer Council Victoria: Melbourne, Australia, 2020. [Google Scholar]
- Oksuzyan, A.; Juel, K.; Vaupel, J.W.; Christensen, K. Men: Good health and high mortality. Sex differences in health and aging. Aging Clin. Exp. Res. 2008, 20, 91–102. [Google Scholar] [CrossRef]
- Wolfinger, E. Stereotyping Single Mothers Is Not New—Its History, and How to Challenge It; Council of Single Mothers and their children, State Government Victoria: Melbourne, Australia, 2017; Volume 2020.
- Gough, B. Try to be healthy, but don’t forgo your masculinity: Deconstructing men’s health discourse in the media. Soc. Sci. Med. 2006, 63, 2476–2488. [Google Scholar] [CrossRef] [PubMed]
- Flood, M. Gender equality: Engaging men in change. Lancet 2019, 393, 2386–2387. [Google Scholar] [CrossRef]
- ABS (Australian Bureau of Statistics). National Aboriginal and Torres Strait Islander Health Survey, 2018–2019: Smoking; ABS: Canberra, Australia, 2019.
- Pocock, B. All change, still gendered: The Australian labour market in the 1990s. J. Ind. Relat. 1998, 40, 580–604. [Google Scholar] [CrossRef]
- Lopez, A.D.; Adair, T. Slower increase in life expectancy in Australia than in other high income countries: The contributions of age and cause of death. Med. J. Aust. 2019, 210, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Crenshaw, K. Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ. Chic. Leg. Forum 1989, 1989, 139–167. [Google Scholar]
- Hankivsky, O.; Christoffersen, A. Intersectionality and the determinants of health: A Canadian perspective. Crit. Public Health 2008, 18, 271–283. [Google Scholar] [CrossRef]
- Robinson, Z.F. Intersectionality and Gender Theory. In Handbook of the Sociology of Gender, 2nd ed.; Risman, B.J., Froyum, C.M., Scarborough, W.J., Eds.; Springer Nature: Cham, Switzerland, 2018; pp. 69–81. [Google Scholar]
- Van Daalen, K.R.; Bajnoczki, C.; Chowdhury, M.; Dada, S.; Khorsand, P.; Socha, A.; Lal, A.; Jung, L.; Alqodmani, L.; Torres, I.; et al. Symptoms of a broken system: The gender gaps in COVID-19 decision-making. BMJ Glob. Health 2020, 5, e003549. [Google Scholar] [CrossRef]
- Hill, S.E.; Friel, S. ‘As Long as It Comes off as a Cigarette Ad, Not a Civil Rights Message’: Gender, Inequality and the Commercial Determinants of Health. Int. J. Environ. Res. Public Health 2020, 17, 7902. [Google Scholar] [CrossRef] [PubMed]
- Freudenberg, N. Lethal but Legal: Corporations, Consumption, and Protecting Public Health; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Busse, H.; Azazh, A.; Teklu, S.; Tupesis, J.P.; Woldetsadik, A.; Wubben, R.J.; Tefera, G. Creating change through collaboration: A twinning partnership to strengthen emergency medicine at Addis Ababa University/Tikur Anbessa Specialized Hospital—A model for international medical education partnerships. Acad. Emerg. Med. 2013, 20, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Perez, C.C. Invisible Women: Exposing Data Bias ina World Designed for Men; Vintage: London, UK, 2019. [Google Scholar]
- Global Health 5050 Our Mission, Vision and Values. Available online: https://globalhealth5050.org/mission-vision-values/ (accessed on 13 January 2021).
| Countries Grouped by Income Level | Life Expectancy, Total, at Birth | Life Expectancy, Female, at Birth | Life Expectancy, Male, at Birth | Gender Life Expectancy Difference |
|---|---|---|---|---|
| Low-income | 63.49 | 65.41 | 61.59 | 3.82 |
| Middle-income | 71.86 | 74.11 | 69.75 | 4.36 |
| High-income | 80.66 | 83.35 | 78.13 | 5.22 |
| World | 72.56 | 74.87 | 70.39 | 4.48 |
| Rank | Cause of Death (Male), Australia, (%) | Cause of Death (Female), Australia, (%) | Cause of Death (Male), Ethiopia, (%) | Cause of Death (Female), Ethiopia, (%) |
|---|---|---|---|---|
| 1st | Coronary heart disease (12.5) | Dementia including Alzheimer disease (11.8) | Infectious and Parasite disease (29) | Infectious and Parasite disease (41) |
| 2nd | Lung cancer (6.1) | Coronary heart disease (9.5) | External cause of death (16) 1 | Indeterminate [51] |
| 3rd | Dementia including Alzheimer disease (6.1) | Cerebrovascular disease (7.6) | Cardiac related disease (14) 2 | Cardiac related disease (14) |
| 4th | Cerebrovascular disease (5.1) | Lung cancer (4.7) | Indeterminate (13) | External cause of death (8) |
| 5th | Chronic obstructive pulmonary disease (COPD) (4.6) | Chronic obstructive pulmonary disease (COPD) (4.4) | Neoplasm (6) 3 | Neoplasm (6) |
| 6th | Prostate cancer (4) | Breast cancer (3.9) | Mental and nervous system disorder (6) 4 | Renal disorders (4) |
| 7th | Colorectal cancer (3.5) | Colorectal cancer (3.2) | Gastrointestinal disorder (6) 5 | Mental and nervous system disorder (4) |
| 8th | Diabetes (3.1) | Diabetes (2.8) | Nutritional and endocrine disorder (4) 6 | Nutritional and endocrine disorder (4) |
| 9th | Suicide (2.8) | Heart failure and complications and ill-defined heart disease (2.4) | Renal disorders (3) 7 | Gastrointestinal disorder (3) |
| 10th | Cancer of unknown (2) | Influenza and pneumonia (2.2) | Respiratory disorder (1) 8 | Unspecified (3) |
| GII 1 | 2000 | 2005 | 2010 | 2015 | 2018 |
|---|---|---|---|---|---|
| Australia | 0.160 | 0.139 | 0.138 | 0.110 | 0.103 |
| Ethiopia | 0.614 | 0.580 | 0.519 | 0.508 | |
| GDI 2 | 2000 | 2005 | 2010 | 2015 | 2018 |
| Australia | 0.961 | 0.969 | 0.975 | 0.975 | 0.975 |
| Ethiopia | 0.741 | 0.759 | 0.817 | 0.841 | 0.844 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baum, F.; Musolino, C.; Gesesew, H.A.; Popay, J. New Perspective on Why Women Live Longer Than Men: An Exploration of Power, Gender, Social Determinants, and Capitals. Int. J. Environ. Res. Public Health 2021, 18, 661. https://doi.org/10.3390/ijerph18020661
Baum F, Musolino C, Gesesew HA, Popay J. New Perspective on Why Women Live Longer Than Men: An Exploration of Power, Gender, Social Determinants, and Capitals. International Journal of Environmental Research and Public Health. 2021; 18(2):661. https://doi.org/10.3390/ijerph18020661
Chicago/Turabian StyleBaum, Fran, Connie Musolino, Hailay Abrha Gesesew, and Jennie Popay. 2021. "New Perspective on Why Women Live Longer Than Men: An Exploration of Power, Gender, Social Determinants, and Capitals" International Journal of Environmental Research and Public Health 18, no. 2: 661. https://doi.org/10.3390/ijerph18020661
APA StyleBaum, F., Musolino, C., Gesesew, H. A., & Popay, J. (2021). New Perspective on Why Women Live Longer Than Men: An Exploration of Power, Gender, Social Determinants, and Capitals. International Journal of Environmental Research and Public Health, 18(2), 661. https://doi.org/10.3390/ijerph18020661





