Abstract
The aim of this study was to demonstrate the effects of motor imagery training on balance and gait abilities in older adults and to investigate the possible application of the training as an effective intervention against fall prevention. Subjects (n = 34) aged 65 years and over who had experienced falls were randomly allocated to three groups: (1) motor imagery training group (MITG, n = 11), (2) task-oriented training group (TOTG, n = 11), and (3) control group (CG, n = 12). Each group performed an exercise three times a week for 6 weeks. The dependent variables included Path Length of center of pressure (COP)-based static balance, Berg Balance Scale (BBS) score, Timed Up and Go Test (TUG) score, which assesses a person’s mobility based on changes in both static and dynamic balance, Falls Efficacy Scale (FES) score, which evaluates changes in fear of falls, and gait parameters (velocity, cadence, step length, stride length, and H-H base support) to evaluate gait. After the intervention, Path Length, BBS, TUG, velocity, cadence, step length, and stride length showed significant increases in MITG and TOTG compared to CG (p < 0.05). Post hoc test results showed a significantly greater increase in BBS, TUG, and FES in MITG compared with TOTG and CG (p < 0.05). Our results suggest that motor imagery training combined with functional training has positive effects on balance, gait, and fall efficacy for fall prevention in the elderly.
1. Introduction
As the life expectancy of the elderly increases due to the effects of medical technology and increased living standards, physical changes and health challenges due to aging become a primary concern. Advanced age is associated with decreased flexibility, coordination, and muscle strength, and increased physical response time due to neuronal degeneration. Therefore, the elderly are not capable of rapid response to sudden changes in the environment [1]. These changes in the elderly reduce cognitive motor responses and postural control, thereby increasing the incidence of trauma and death due to falls [2,3]. It has been reported that 30% of the elderly aged at least 65 years residing in the community sustain a fall injury at least once a year. The risks and economic costs of falls increase along with age, and nearly 40% of those who sustain an initial fall injury experience recurrent falls [4,5].
Falls occur due to intrinsic factors related to physiological changes associated with aging or disease as well as extrinsic environmental factors, such as slippery grounds, poor lighting and obstacles [6]. These factors can be independent or related to each other in complex and diverse ways. Decreased ability to maintain posture, increased postural sway, decreased walking speed and dynamic balance may be closely related to the occurrence of falls [7]. The incidence of falls is reported to be the highest during walking, followed by descending stairs, standing up, and changing direction, and is higher among women than men [8].
Recently, various interventions have been attempted to prevent falls in the elderly and improve their daily living activities and ability to balance. Motor imagery training and task-oriented training are being used as evidence-based interventions in diverse fields of rehabilitation [9,10].
Motor imagery training is a learning process in which movements are only internally imagined without being physically carried out [11]. Imagery training engages the same areas of the brain that are activated during exercise, suggesting that the activity of imaginary muscles is increased and resulting in increased muscle strength and speed [12]. For this reason, motor imagery has been used to improve performance in athletes and promote functional recovery in patients at reduced burden and cost, without the need for exercise equipment or therapists [13,14]. In addition, since it can be done at home, it serves as an appropriate intervention in the elderly and patients who cannot participate in daily exercise programs [15]. Multiple forms of motor imagery training exist. However, it is important to include familiar and task-oriented exercise in motor imagery training because the motor neurons are activated further by meaningful exercise-related tasks based on clear-cut goals and motivation [16]. Motor imagery training combined with other therapeutic interventions enhances the recovery of daily living activities in the elderly [17]. Zapparoli et al. reported that the patient’s damaged motor function was recovered by combining motor imagery training and physical therapy [18].
Task-oriented training is based on motor behavior system theory and motor learning. It is an effective intervention in the field of rehabilitation medicine because it provides patients with the motivation to solve problems more actively via exercise programs that are focused on functional tasks rather than repeated and simple training movements. To maximize the effectiveness of task-oriented training, the form of the training task should be similar to that of a task seen in real-world situations, and it should be a meaningful and important task for the subjects. To this end, various forms, such as task-oriented circuit training and progressive resistance task-oriented training, are used as effective interventions in the field of rehabilitation medicine [19,20].
Thus, individual interventions via motor imagery training and task-oriented training are designed to improve balance and gait, respectively. However, most previous studies assessing these interventions involved athletes and patients rather than the elderly, and studies combining the two interventions to assess the risk of falls among the elderly have yet to be reported. Therefore, the purpose of this study was to evaluate the effect of these training on the balance and gait of the elderly after conducting motor imagery training combined with task-oriented training based on various real environments in which falls could occur to prevent falls.
2. Materials and Methods
2.1. Study Subjects
In this study, 36 healthy elderly persons aged at least 65 years residing at a senior citizen center in an apartment building in S-city, South Korea were assigned to a motor imagery training group (MITG), a task-oriented training group (TOTG), and a control group (CG (n = 12 subjects per group). The final study population consisted of 34 subjects after two dropped out (Table 1). The subjects were randomly assigned to the individual groups using a randomization program (http://www.randomization.com). The calculation was based on a significance level (α) of 0.05 and a power (1 − β) of 0.95 using the G-power 3.1 program, and the effect size was calculated based on the primary effect in previous studies [21].

Table 1.
General characteristics of the subjects (n = 34).
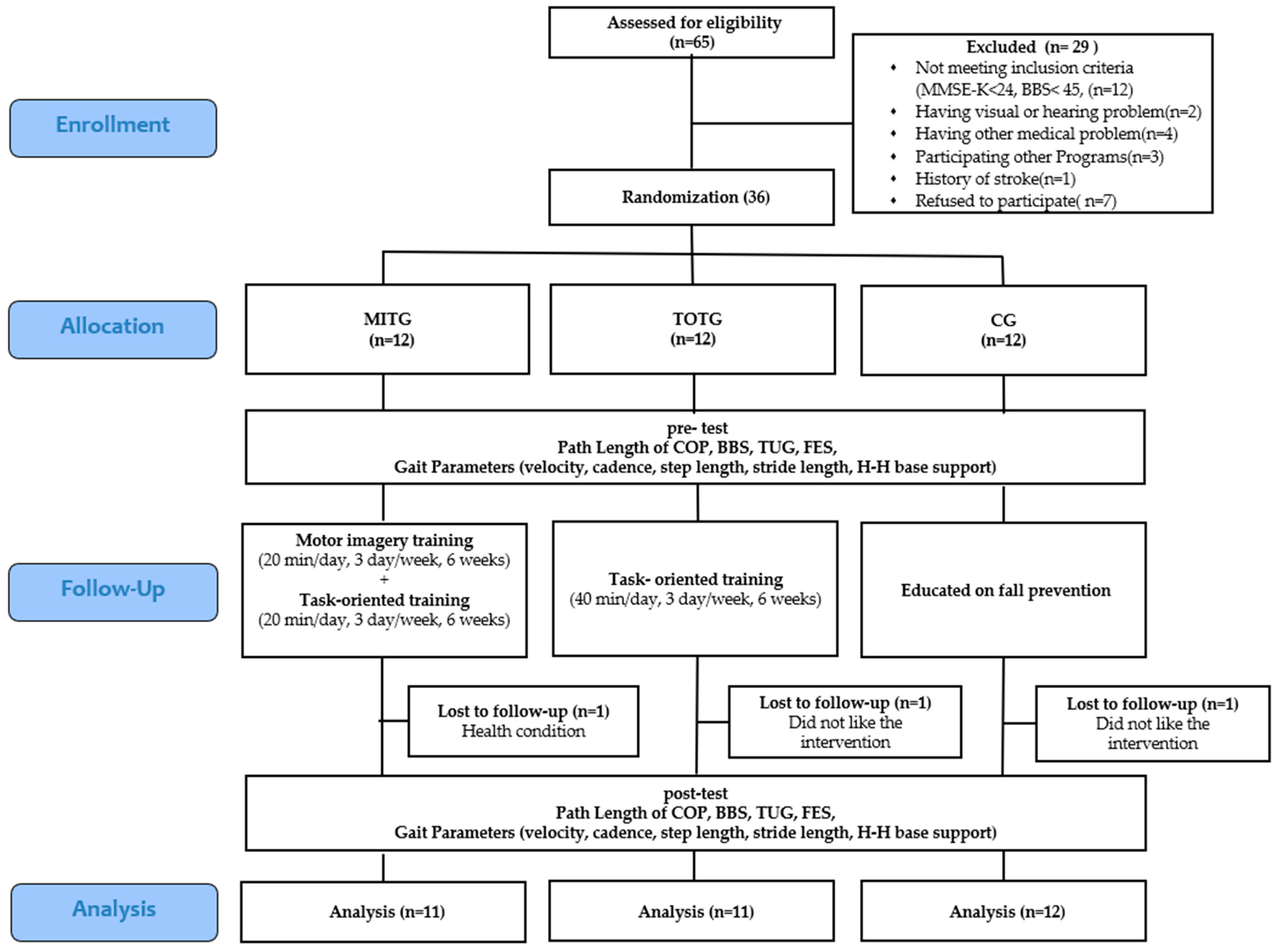
According to the calculations, a total of 33 subjects were deemed necessary for the study. The selection criteria were: a score of at least 24 points on the Mini-Mental State Examination-Korean (MMSE-K), a history of at least two falls within the one year prior to the study, adequate communication skills, ability to walk independently and to balance, and willingness to provide written informed consent to participate in the study. The exclusion criteria were: brain damage or neurological abnormalities, visual or hearing ailments, treatment with drugs related to walking or balance, participation in programs related to walking or balance at the time of the study, experimental participation rate lower than 80%, or study dropouts (Figure 1).
Figure 1.
Flow diagram of participant progress. Abbreviations: MITG: motor imagery training group, TOTG: task-oriented training group, CG: control group, MMSE-K: Mini Mental State Examination-Korean Version, COP: center of pressure, BBS: Berg Balance Scale, TUG: Timed Up and Go Test, FES: Falls Efficacy Scale.
2.2. Study Design and Procedure
The intervention period was 6 weeks long, and training was conducted in 40-min sessions three times per week. During the intervention period, MITG carried out task-oriented training following motor imagery training; TOTG performed only task-oriented training; and CG was educated on fall prevention and health using audio-visual materials. The balance and gait abilities of all subjects were evaluated before and after the intervention, and the Falls Efficacy Scale (FES) scores of the participants were evaluated in relation to these functional performance abilities. Path Length of Center of pressure (COP)-based static balance tests, the Berg Balance Scale (BBS), and timed up and go (TUG) tests were used to evaluate balance. H-H base supports were conducted using the GAITRite system to evaluate gait, velocity, cadence, step length, and stride length. This study was approved by the Institutional Bioethics Committee of Daejeon University (IRB1040647-201910-HR-010-03).
2.3. Intervention
2.3.1. Motor Imagery Training
The subjects were asked to relax their bodies and meditate while sitting comfortably in a chair with their eyes closed in a quiet room for 10 min before performing motor imagery training. The subjects then performed motor imagery training for 20 min by freely imagining movements that protected their body and prevented injuries in the event of falls in diverse real-world environments, such as in the bathroom, kitchen, on the stairs, and around obstacles that are frequently associated with falls. During the motor imagery training, a researcher briefly explained the situation verbally using a script that was prepared in advance (Table 2).

Table 2.
Motor imagery training.
2.3.2. Task-Oriented Training
The task-oriented training implemented in this study entailed balance training centered on activities of daily living in the real-life environment of the senior citizen center. In order to reduce the risk of falls and increase the subjects’ interest in the training, the assigned tasks changed over time (Table 3).

Table 3.
Task-oriented training.
2.4. Evaluation Tool
2.4.1. Mini-Mental State Examination-Korean (MMSE-K)
The MMSE-K is a tool designed to test cognitive dysfunction in the elderly. The MMSE is relatively easy to use and can be completed in 5 to 10 min. This tool can be used to monitor changes that take place over time because the learning effect of training is small and the tool enables repetitious measurements. The total MMSE score of 30 includes: 10 points for intellectual power, 3 points for memory registration, 3 points for memory recall, 5 points for attention and calculation, 7 points for language skills, and 2 points for understanding and judgment. In this study, additional points were assigned to compensate those who were not educated, though the total score of each individual sub-item never exceeded the full score for that sub-item (e.g., a participant could not receive more than 10 points for intellectual power). A normal (non-cognitively impaired) state is defined by a score of 25 or higher, whereas a score of 21–24 points indicates possible dementia and cognitive impairment is indicated by a score of 20 or lower [22].
2.4.2. Movement Imagery Questionnaire—Revised Second Version: MIQ-RS
The Movement Imagery Questionnaire (MIQ-RS) is designed to assess a subject’s ability to imagine the given tasks. It is composed of a total of 14 items: seven items to evaluate visualization and seven items to evaluate kinematic imagination. Each item is scored on a 7-point scale, ranging from 1 for tasks that are very easy to imagine or implement to 7 for very difficult tasks [23].
2.4.3. Path Length of Center of Pressure (COP)-Based Static Balance Test
Static balance was evaluated using a Wii fit force plate (Balance Board, Nintendo, Kyoto, Japan) and a Balancia software program (Balancia software ver. 2.0, Mintosys, Seoul, Korea). The subjects were asked to stand on the Wii fit force plate with their knees straight and their feet shoulder width apart and maintain a posture with both arms comfortably lowered.
In order to control for postural fluctuations due to eye movements, the subjects were asked to look straight ahead with their eyes open. The measurement was conducted for 30 s beginning with the participants standing on the force plate in stockinged feet with a stable posture. The test was conducted a total of three times and the average value was used. The test was conducted between 2 and 4 p.m. and 10 min of rest were given between each of the three measurements. The center of pressure for the X and Y axes was recorded using the Wii Fit force plate connected to the laptop and Bluetooth technology to measure the forward, backward, leftward, and rightward path length. The Valencia program was used to analyze the data. The sampling rates for data collection were 50 Hz and 12 Hz (using a low-pass filter). The intra-tester reliability of the Wii Fit force plate based on ICC was 0.92–0.98, while the intra-tester reliability of the Valencia program was r = 0.79–0.96 and the validity of the program was r = 0.8–0.96. The Wii Fit force plate and the Valencia program have been validated as useful tools for balance evaluation [24].
2.4.4. Berg Balance Scale (BBS)
BBS is used to evaluate static and dynamic balance. It can be used to predict the risk of falls in elderly subjects without neurological lesions living in the community. BBS is composed of three components: sitting, standing, and postural change. The total score on the BBS is 56 points; it consists of 14 items applicable to daily living activities, each of which is measured with a 5-point scale ranging from 0 to 4 points. A BBS score of 45 or lower indicates that an auxiliary tool such as a cane is necessary when walking, and that the risk of fall is high [25].
2.4.5. Timed Up and Go Test (TUG)
TUG can be used to measure a subject’s ability to balance and move. It entails measuring the time it takes for the subject to walk around an obstacle that is 3 m away from the chair in which he was originally seated and return to the chair as quickly and safely as possible. The test-retest reliability and intra-tester reliability were r = 0.99 [26]. The measurement was performed a total of three times for each participant and the average was used as the measured value. The test was conducted between 9 and 11 a.m. and 10 min of rest were given between each of the three measurements.
2.4.6. Gait Evaluation
To measure temporospatial gait, various gait-related variables including walking velocity, cadence, step length, stride length, double support time, and the base support between the heels of both feet (H-H base support) were measured using the GAITRite system (CIR Systems Inc. Peekskill, NY, USA), which has proven validity. The participants were asked to walk at a comfortable speed 2 m in front of a walking board and on a 4 m walking board according to the examiner’s verbal instructions [27]. The participants were measured indoors with their shoes off and socks on. The gait test was performed three times for each participant and the average value was used. The test was conducted between 1 and 4 p.m. and 10 min of rest were given between each of the three measurements.
2.4.7. Falls Efficacy Scale (FES)
The Falls Efficacy Scale (FES) measures the level of confidence associated with fall prevention. The FES score represents the fear associated with performing 10 actions necessary in daily life on a scale ranging from 1 to 10, and its reliability is r = 0.94. FES score is inversely proportional to the fear of falling and predicts the recurrence of falls. The higher the score, the greater the fear of falls, and the lower the fall efficacy [28].
2.5. Analytical Method
The SPSS ver. 21.0 program (IBM, Armonk, NY, USA) was used for all statistical analyses. The general characteristics of the subjects were tested for normality using the Sharpiro-Wilk test. The chi-square test and one-way analysis of variance (ANOVA) were used to test the homogeneity of the general characteristics between the groups and of the pre-experimental results. In order to comprehensively analyze the two factors (treatment application time, intervention method), a two-way ANOVA with repeated measures was performed to assess the effects of interaction between individual factors and each repeated measures factor. Paired t-tests or Wilcoxon signed rank tests were used to analyze changes between measurement time points (before and after intervention) in each group. One-way ANOVA was used to compare the degree of change between groups, and Scheffe tests were used for post-hoc analysis. The significance level was set at α = 0.05.
3. Results
3.1. Path Length of Center of Pressure (COP)-Based Static Balance Test
Path length of COP decreased significantly more in MITG and TOTG than in CG (p < 0.05). Path length was compared between the three groups before and after the intervention; the results indicated significant interactions between the groups and the times (F = 11.076, p < 0.05). The changes before and after the intervention in the three groups were significantly different (F = 4.930, p < 0.05). According to the results of post-hoc analysis, Path length decreased significantly more in MITG and TOTG than in CG (p < 0.05); however, no significant difference existed between the two intervention groups (p > 0.05) (Table 4).

Table 4.
Path Length in each group, pre- vs. post-test.
3.2. Berg Balance Scale (BBS)
Significant increases in BBS score were found in MITG and TOTG after the intervention (p < 0.05). The scores of the three groups were compared before and after the intervention, and significant interactions between the groups and the times were observed (F = 22.234, p < 0.05). The changes before and after the intervention in the three groups showed significant differences (F = 11.684, p < 0.05). According to the results of post-hoc analysis, the scores increased significantly more in MITG compared to the other two groups (p < 0.05) (Table 5).

Table 5.
BBS score in each group, pre- vs. post-test.
3.3. Timed Up and Go Test (TUG)
Significant increases in TUG were found in MITG and TOTG after the intervention (p < 0.05). The times of the three groups were compared before and after the intervention, and significant interactions between the groups and the times were observed (F = 12.277, p < 0.05). The changes before and after the intervention in the three groups were significantly different (F = 15.607, p < 0.05). The results of post-hoc analysis revealed that MITG showed the most significant decrease of all three groups (p < 0.05) (Table 6).

Table 6.
TUG in each group, pre- vs. post-test.
3.4. Gait Evaluation
Evaluation of gait before and after intervention revealed a significant increase in velocity, cadence, step length, and stride length in MITG and TOTG (p < 0.05). The H-H base of support decreased significantly after intervention only in MITG (p < 0.05). Analysis of the velocity, cadence, step length, stride length, and H-H base of support in the three groups revealed significant interactions between the groups and the times (F = 12.925, 9.489, 30.784, 23.134, and 16.016, respectively; p < 0.05). The changes in velocity, cadence, step length, stride length, and H-H base of support before and after the intervention in the three groups were compared, and the results showed significant differences (F = 8.788, 4.953, 3.596, 4.818, 7.027 p < 0.05). The results of post-hoc analysis showed a significant increase in the velocity, cadence, and stride length in MITG and TOTG compared with CG (p < 0.05), but no significant difference between MITG and TOTG (p > 0.05). According to the results of post-hoc analysis, step length increased significantly more in MITG compared with CG (p < 0.05), but no significant difference existed between MITG and TOTG (p > 0.05). The results of post-hoc analysis revealed a strongly significant decrease in the H-H base of support in MITG (p < 0.05) (Table 7).

Table 7.
Comparison of gait parameters in the three groups: pre- vs. post-test.
3.5. Falls Efficacy Scale (FES)
Significant differences in FES score between MITG and TOTG (p < 0.05) were found after intervention. The scores of the three groups were compared before and after the intervention, and the results revealed significant interactions between the groups and the times (F = 8.839, p < 0.05). The changes between the three groups before and after the intervention were significant (F = 14.017, p < 0.05). The results of post-hoc analysis revealed significant decreases in MITG and TOTG compared to CG (p < 0.05), and the most significant decrease was found in MITG (p < 0.05) (Table 8).

Table 8.
FES in each group, pre- vs. post-test.
4. Discussion
Motor imagery training is consistently reported to improve balance and gait in the elderly, and many studies have investigated falls in the elderly population. Thus, the current study conducted motor imagery training centered on activities of daily life that aimed to maintain balance and protect the body in the event of a fall in order to assess the effects of such training on balance and walking.
Malouin et al. stated that it is important to determine the extent to which subjects can concentrate on imagining movements because the quality of imagination during motor imagery training may differ across individuals [29,30]. This is an important factor that affects the outcome of motor imagery training. Several types of questionnaires that measure the ability to imagine have been developed for a variety of populations. Butler et al. tested whether the MIQ-RS, developed for healthy young adults, was valid for the elderly and stroke patients, and reported that it is useful for evaluating imagination among the elderly and stroke patients [31]. Therefore, in this study, MIQ-RS was used to determine the extent to which subjects imagine or execute movements. The method includes a first-person perspective, in which the person imagines movement by changing the position of the joint angles to coincide with a given activity, and a third-person perspective, in which the person visualizes his/her movements from the viewpoint of others, similar to a movie [32]. Dickstein and Deutsch stated that although the application of these viewpoints varies according to the task at hand, division of the two viewpoints may be academic and artificial [33]. However, Fery argued that the third-person perspective may be effective in imitating forms for writing but applying the first-person viewpoint to the proprioceptive sense is more effective [34]. A study in stroke patients conducted by Kim and Kim reported that the first-person point of view is more effective at enhancing balance than the third-person perspective [35]. Therefore, in this study, since the nature of the task is appropriate for a first-person perspective, the subjects were requested to perform training accordingly.
On the Path Length of COP-based static balance test, the Path Length after intervention decreased more in MITG and TOTG than in the control group, indicating that the ability to balance was improved to a greater extent in the intervention groups. Similar results were obtained on the BBS test, which is designed to evaluate both static and dynamic balances. The TUG, which is another dynamic balance test used to assess rapidity, speed, and agility, also yielded similar results, which are consistent with Hosseini et al.’s findings in stroke patients [36]. Haslinger et al. reported that application of task-oriented visual feedback training in the elderly improved the results of TUG [37]. Liu et al. reported that, in an elderly population, muscle strength and daily activities were improved by a task-oriented exercise program, which coincides with the results of the present study; together, these findings suggest that task-oriented training not only improves balance in the elderly, but also interacts with motor imagery training to result in more positive effects [38]. Whereas MITG and TOTG did not show different results on the static balance test, the group exposed to the combination of motor imagery training and task-oriented training showed more significant improvement than the group that performed only task-oriented training in the dynamic balance test. A study conducted by Shamsipour-Dehkordy et al. reported that combined motor imagery and physical training in the elderly produced more significant improvement in terms of static and dynamic balance than motor imagery training alone [39]. Lee et al. reported that a group of stroke patients exposed to both functional training and motor imagery training showed significantly greater improvement in dynamic balance than a group who performed only functional training [21]. These results are consistent with the results of the present study, indicating that motor imagery is more effective when used together with other interventions. However, according to Boraxbekk et al., neurological response tests in the elderly who learned a new task revealed that the group that combined functional movements with motor imagery showed no greater effect than the group exposed to a single intervention [40]. This phenomenon was explained by activation of mainly the premotor cortex in the movement group and activation of the secondary visual cortex in the motor imagery training group, suggesting that the activities interfered with each other in the combined group, leading to decreased brain activation. Therefore, although motor imagery training has positive effects on balance and gait in the elderly, the results differ depending on the type of task and method used. It may be difficult to activate motor sensation in the elderly when the imaginary movements are identical to actual movements [41], and the ability to learn and maintain new tasks may also decrease in an older population [42]. However, activation of the cerebral visual cortex via imagery training generates muscle tension through voluntary or involuntary movements of the eyes and brain when an object moves or a sudden change in eye direction occurs [43,44]. Also, Mattay et al. stated that, during the elderly learning movement tasks based on visual information, the brain forms more neural networks bilaterally than are formed in younger learners [44]. Therefore, motor imagery training has a positive effect on balance and gait. In addition, since the motor imagery training carried out in this study did not involve new tasks or tasks that included simple movements, but instead focused on tasks that were relatively familiar in daily life and were important in relation to falls, the participants’ motor imaging ability was strengthened to facilitate actual motor functions. In a study of motor imagery training combined with manual dexterity tasks, Ruffino et al. reported that motor ability was improved in the experimental compared to the control group [45]. Based on a systematic review, Nicholson et al. showed that motor imagery training can be an alternative means of improving balance and gait in the elderly who do not have any neurological issues [10].
The walking patterns of the elderly characteristically show reduced velocity, step length, and cadence, wide stride width, long stance phase, and short swing phase [46]. In this study, the GAITRite system was used to evaluate the gait of the elderly participants based on temporospatial variables. The results revealed that both MITG and TOTG showed increased velocity and cadence, which are temporal variables, and step length and stride length, which are spatial variables, compared to the control group. The H-H base support was significantly decreased in MITG. Dunlap et al. reported that the elderly who experience falls show increased width between the two feet when walking in a new environment due to the fear of falling [47]. The results of this study indicated that the H-H base support decreased the most in MITG, resulting in improved walking ability.
Scheffer et al. reported that elderly individuals who experience falls tend to decrease their physical activities due to their fear of falls, which reduces their motor functions, in turn leading to increased risk of falls [48]. Therefore, in this study, Falls Efficacy Scale (FES) tests were conducted to examine changes in the fear of falls in the elderly. The results suggest that the fear of falls decreased the most in MITG, which is consistent with the results of a study conducted by Chung et al. [49]. Kumar et al. reported that fall efficacy is closely related to balance and movement [50]. Therefore, the improvements in balance and walking ability in this study positively affected fall efficacy, and the repetitive learning about falls via motor imagery training further reduced the fear of falls.
Thus, motor imagery and task-oriented training had a positive effect on static and dynamic balance, walking, and fall efficacy in the elderly. Motor imagery training combined with task-oriented training improved functional abilities more than the single intervention. However, there are several problems in interpreting the results of this study. First, because the number of subjects is small, it is difficult to generalize the results to the entire elderly population. Second, no previous studies reported task-oriented training combined with motor imagery training in the elderly. Third, this study failed to evaluate the duration of the learning effect of motor imagery training. Therefore, additional studies are needed to address these limitations.
5. Conclusions
This study investigated the effect of motor imagery training on the balance and gait of individuals aged at least 65 years who experienced falls. The results suggest that motor imagery training combined with task-oriented training resulted in significant improvement in static and dynamic balance and walking ability in the elderly, and positively affected fall efficacy. These interventions are simple and cost-effective ways to prevent falls in the elderly. The results of this study represent basic data relevant to the elderly.
Author Contributions
Conceptualization, D.S.O.; methodology, J.D.C.; software, D.S.O.; validation, J.D.C.; formal analysis, J.D.C.; investigation, D.S.O.; resources, D.S.O.; data curation, D.S.O.; writing—original draft preparation, D.S.O.; writing—review and editing, D.S.O. and J.D.C.; visualization, D.S.O.; supervision, J.D.C.; project administration, J.D.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Daejeon University (1040647-201910-HR-010-03).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this article are available on request from the corresponding author.
Acknowledgments
The authors would like to acknowledge Shi-Jong Lee and Il-Ryang Wi for providing support on this project.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hiyamizu, M.; Morioka, S.; Shomoto, K.; Shimada, T. Effects of dual task balance training on dual task performance in elderly people: A randomized controlled trial. Clin. Rehabil. 2012, 26, 58–67. [Google Scholar] [CrossRef]
- Grundstrom, A.C.; Guse, C.E.; Layde, P.M. Risk factors for falls and fall-related injuries in adults 85 years of age and older. Arch. Gerontol. Geriatr. 2012, 54, 421–428. [Google Scholar] [CrossRef]
- Turusheva, A.; Frolova, E.; Kotovskaya, Y.; Petrosyan, Y.; Dumbadze, R. Association between arterial stiffness, frailty and fall-related injuries in older adults. Vasc. Health Risk Manag. 2020, 16, 307. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, L.D.; Gillespie, W.J.; Robertson, M.C.; Lamb, S.E.; Cumming, R.G.; Rowe, B.H. Interventions for preventing falls in elderly people. Physiotherapy 2003, 89, 692–693. [Google Scholar] [CrossRef]
- Tricco, A.C.; Thomas, S.M.; Veroniki, A.A.; Hamid, J.S.; Cogo, E.; Strifler, L.; Khan, P.A.; Robson, R.; Sibley, K.M.; MacDonald, H. Comparisons of interventions for preventing falls in older adults: A systematic review and meta-analysis. JAMA 2017, 318, 1687–1699. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z.; Josephson, K.R. Falls and their prevention in elderly people: What does the evidence show? Med. Clin. 2006, 90, 807–824. [Google Scholar] [CrossRef] [PubMed]
- Rogers, M.E.; Rogers, N.L.; Takeshima, N.; Islam, M.M. Methods to assess and improve the physical parameters associated with fall risk in older adults. Prev. Med. 2003, 36, 255–264. [Google Scholar] [CrossRef]
- Cuevas-Trisan, R. Balance problems and fall risks in the elderly. Phys. Med. Rehabil. Clin. 2017, 28, 727–737. [Google Scholar] [CrossRef]
- Kalicinski, M.; Lobinger, B.H. Benefits of motor and exercise imagery for older adults. J. Imag. Res. Sport Phys. Act. 2013, 8, 61–75. [Google Scholar] [CrossRef]
- Nicholson, V.; Watts, N.; Chani, Y.; Keogh, J.W. Motor imagery training improves balance and mobility outcomes in older adults: A systematic review. J. Physiother. 2019, 65, 200–207. [Google Scholar] [CrossRef]
- Jackson, P.L.; Lafleur, M.F.; Malouin, F.; Richards, C.; Doyon, J. Potential role of mental practice using motor imagery in neurologic rehabilitation. Arch. Phys. Med. Rehabil. 2001, 82, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Di Rienzo, F.; Blache, Y.; Kanthack, T.F.D.; Monteil, K.; Collet, C.; Guillot, A. Short-term effects of integrated motor imagery practice on muscle activation and force performance. Neuroscience 2015, 305, 146–156. [Google Scholar] [CrossRef]
- Schuster, C.; Hilfiker, R.; Amft, O.; Scheidhauer, A.; Andrews, B.; Butler, J.; Kischka, U.; Ettlin, T. Best practice for motor imagery: A systematic literature review on motor imagery training elements in five different disciplines. BMC Med. 2011, 9, 75. [Google Scholar] [CrossRef]
- Saimpont, A.; Malouin, F.; Tousignant, B.; Jackson, P.L. Motor imagery and aging. J. Mot. Behav. 2013, 45, 21–28. [Google Scholar] [CrossRef]
- Dunsky, A.; Dickstein, R.; Marcovitz, E.; Levy, S.; Deutsch, J. Home-based motor imagery training for gait rehabilitation of people with chronic poststroke hemiparesis. Arch. Phys. Med. Rehabil. 2008, 89, 1580–1588. [Google Scholar] [CrossRef]
- Kim, J.; Oh, D.; Kim, S.; Choi, J. Visual and kinesthetic locomotor imagery training integrated with auditory step rhythm for walking performance of patients with chronic stroke. Clin. Rehabil. 2011, 25, 134–145. [Google Scholar] [CrossRef]
- Carrasco, D.G.; Cantalapiedra, J.A. Effectiveness of motor imagery or mental practice in functional recovery after stroke: A systematic review. Neurologia 2016, 31, 43–52. [Google Scholar] [CrossRef]
- Zapparoli, L.; Sacheli, L.M.; Seghezzi, S.; Preti, M.; Stucovitz, E.; Negrini, F.; Pelosi, C.; Ursino, N.; Banfi, G.; Paulesu, E. Motor imagery training speeds up gait recovery and decreases the risk of falls in patients submitted to total knee arthroplasty. Sci. Rep. 2020, 10, 1–12. [Google Scholar] [CrossRef]
- Ghazal, J.; Malik, A.N.; Amjad, I. Task oriented training improves the balance outcome & reducing fall risk in diabetic population. Pak. J. Med. Sci. 2016, 32, 983–987. [Google Scholar]
- Rensink, M.; Schuurmans, M.; Lindeman, E.; Hafsteinsdóttir, T. Task-oriented training in rehabilitation after stroke: Systematic review. J. Adv. Nurs. 2009, 65, 737–754. [Google Scholar] [CrossRef]
- Lee, S.; Lee, G.; Song, C. Effectiveness of imagery training of functional training on the balance and gait in stroke patients. J. Coach. Dev. 2010, 12, 201–211. [Google Scholar]
- Park, J.H.; Kwon, Y.C. Modification of the mini-mental state examination for use in the elderly in a non-western society: Part I. development of korean version of mini-mental state examination. Int. J. Geriatr. Psychiatry 1990, 5, 381–387. [Google Scholar] [CrossRef]
- Gregg, M.; Hall, C.; Butler, A. The MIQ-RS: A suitable option for examining movement imagery ability. Evid. Based Complement. Altern. Med. 2010, 7, 249–257. [Google Scholar] [CrossRef]
- Park, D.; Lee, D.; Choi, S.; Shin, W. Reliability and validity of the balancia using wii balance board for assessment of balance with stroke patients. J. Korea Acad. Ind. Coop. Soc. 2013, 14, 2767–2772. [Google Scholar]
- Park, S.; Lee, Y. The diagnostic accuracy of the berg balance scale in predicting falls. West. J. Nurs. Res. 2017, 39, 1502–1525. [Google Scholar] [CrossRef]
- Nightingale, C.J.; Mitchell, S.N.; Butterfield, S.A. Validation of the timed up and go test for assessing balance variables in adults aged 65 and older. J. Aging Phys. Act. 2018, 27, 230–233. [Google Scholar] [CrossRef]
- Van Uden, C.J.; Besser, M.P. Test-retest reliability of temporal and spatial gait characteristics measured with an instrumented walkway system (GAITRite®). BMC Musculoskelet. Disord. 2004, 5, 13. [Google Scholar] [CrossRef]
- Figueiredo, D.; Santos, S. Cross-cultural validation of the falls efficacy scale-international (FES-I) in portuguese community-dwelling older adults. Arch. Gerontol. Geriatr. 2017, 68, 168–173. [Google Scholar] [CrossRef]
- Malouin, F.; Richards, C.L.; Jackson, P.L.; Lafleur, M.F.; Durand, A.; Doyon, J. The kinesthetic and visual imagery questionnaire (KVIQ) for assessing motor imagery in persons with physical disabilities: A reliability and construct validity study. J. Neurol. Phys. 2007, 31, 20–29. [Google Scholar] [CrossRef]
- Nakano, H.; Kodama, T.; Ukai, K.; Kawahara, S.; Horikawa, S.; Murata, S. Reliability and validity of the japanese version of the kinesthetic and visual imagery questionnaire (KVIQ). Brain Sci. 2018, 8, 79. [Google Scholar] [CrossRef]
- Butler, A.J.; Cazeaux, J.; Fidler, A.; Jansen, J.; Lefkove, N.; Gregg, M.; Hall, C.; Easley, K.A.; Shenvi, N.; Wolf, S.L. The movement imagery questionnaire-revised, (MIQ-RS) is a reliable and valid tool for evaluating motor imagery in stroke populations. Evid. Based Complement. Altern. Med. 2012, 2012, 1–11. [Google Scholar] [CrossRef]
- McAvinue, L.P.; Robertson, I.H. Measuring motor imagery ability: A review. Eur. J. Cogn. Psychol. 2008, 20, 232–251. [Google Scholar] [CrossRef]
- Dickstein, R.; Deutsch, J.E. Motor imagery in physical therapist practice. Phys. Ther. 2007, 87, 942–953. [Google Scholar] [CrossRef]
- Fery, Y.A. Differentiating visual and kinesthetic imagery in mental practice. Can. J. Exp. Psychol. 2003, 57, 1–10. [Google Scholar] [CrossRef]
- Kim, J.; Kim, K. Effect of motor imagery training with visual and kinesthetic imagery training on balance ability in post stroke hemiparesis. J. Korean Soc. Phys. Med. 2010, 5, 517–525. [Google Scholar]
- Hosseini, S.A.; Fallahpour, M.; Sayadi, M.; Gharib, M.; Haghgoo, H. The impact of mental practice on stroke patients’ postural balance. J. Neurol. Sci. 2012, 322, 263–267. [Google Scholar] [CrossRef]
- Haslinger, W.; Müller, L.; Sarabon, N.; Raschner, C.; Kern, H.; Löfler, S. A novel device to preserve physical activities of daily living in healthy older people. J. Aging Phys. Act. 2015, 23, 569–579. [Google Scholar] [CrossRef]
- Liu, C.; Jones, L.Y.; Formyduval, A.R.; Clark, D.O. Task-oriented exercise to reduce activities of daily living disability in vulnerable older adults: A feasibility study of the 3-step workout for life. J. Aging Phys. Act. 2016, 24, 384–392. [Google Scholar] [CrossRef]
- Shamsipour-Dehkordy, P.; Aslankhani, M.; Shams, A. Effects of physical, mental and mixed practices on the static and dynamic balance of aged people. J. Shahrekord Univ. Med. Sci. 2011, 12, 71–77. [Google Scholar]
- Boraxbekk, C.; Hagkvist, F.; Lindner, P. Motor and mental training in older people: Transfer, interference, and associated functional neural responses. Neuropsychologia 2016, 89, 371–377. [Google Scholar] [CrossRef]
- Zwergal, A.; Linn, J.; Xiong, G.; Brandt, T.; Strupp, M.; Jahn, K. Aging of human supraspinal locomotor and postural control in fMRI. Neurobiol. Aging 2012, 33, 1073–1084. [Google Scholar] [CrossRef] [PubMed]
- Kalicinski, M.; Kempe, M.; Bock, O. Motor imagery: Effects of age, task complexity, and task setting. Exp. Aging Res. 2015, 41, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Sturnieks, D.L.; St George, R.; Lord, S.R. Balance disorders in the elderly. Neurophysiol. Clin. 2008, 38, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Mattay, V.S.; Fera, F.; Tessitore, A.; Hariri, A.R.; Das, S.; Callicott, J.H.; Weinberger, D.R. Neurophysiological correlates of age-related changes in human motor function. Neurology 2002, 58, 630–635. [Google Scholar] [CrossRef]
- Ruffino, C.; Bourrelier, J.; Papaxanthis, C.; Mourey, F.; Lebon, F. The use of motor imagery training to retain the performance improvement following physical practice in the elderly. Exp. Brain Res. 2019, 237, 1375–1382. [Google Scholar] [CrossRef]
- Hollman, J.H.; McDade, E.M.; Petersen, R.C. Normative spatiotemporal gait parameters in older adults. Gait Posture 2011, 34, 111–118. [Google Scholar] [CrossRef]
- Dunlap, P.; Perera, S.; VanSwearingen, J.M.; Wert, D.; Brach, J.S. Transitioning to a narrow path: The impact of fear of falling in older adults. Gait Posture 2012, 35, 92–95. [Google Scholar] [CrossRef]
- Scheffer, A.C.; Schuurmans, M.J.; van Dijk, N.; van der Hooft, T.; de Rooij, S.E. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008, 37, 19–24. [Google Scholar] [CrossRef]
- Chung, J.; Jung, H.; Lee, C.; Yoo, E. Effects of mental practice on balance ability and fall efficacy in dwelling elderly population: Single subject design. J. Korean Soc. Community Based Occup. Ther. 2015, 5, 31–42. [Google Scholar] [CrossRef]
- Kumar, S.; Vendhan, G.V.; Awasthi, S.; Tiwari, M.; Sharma, V.P. Relationship between fear of falling, balance impairment and functional mobility in community dwelling elderly. Indian J. Phys. Med. Rehabil. 2008, 19, 48–52. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).