Influence of Fixed Orthodontic Therapy on Pharyngeal Airway Dimensions after Correction of Class-I, -II and -III Skeletal Profiles in Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Study Design and Grouping
2.3. Eligibility Criteria
2.4. Demographic Data
2.5. Fixed Orthodontic Therapy
2.6. Study Sample (Cephalometric Analysis)
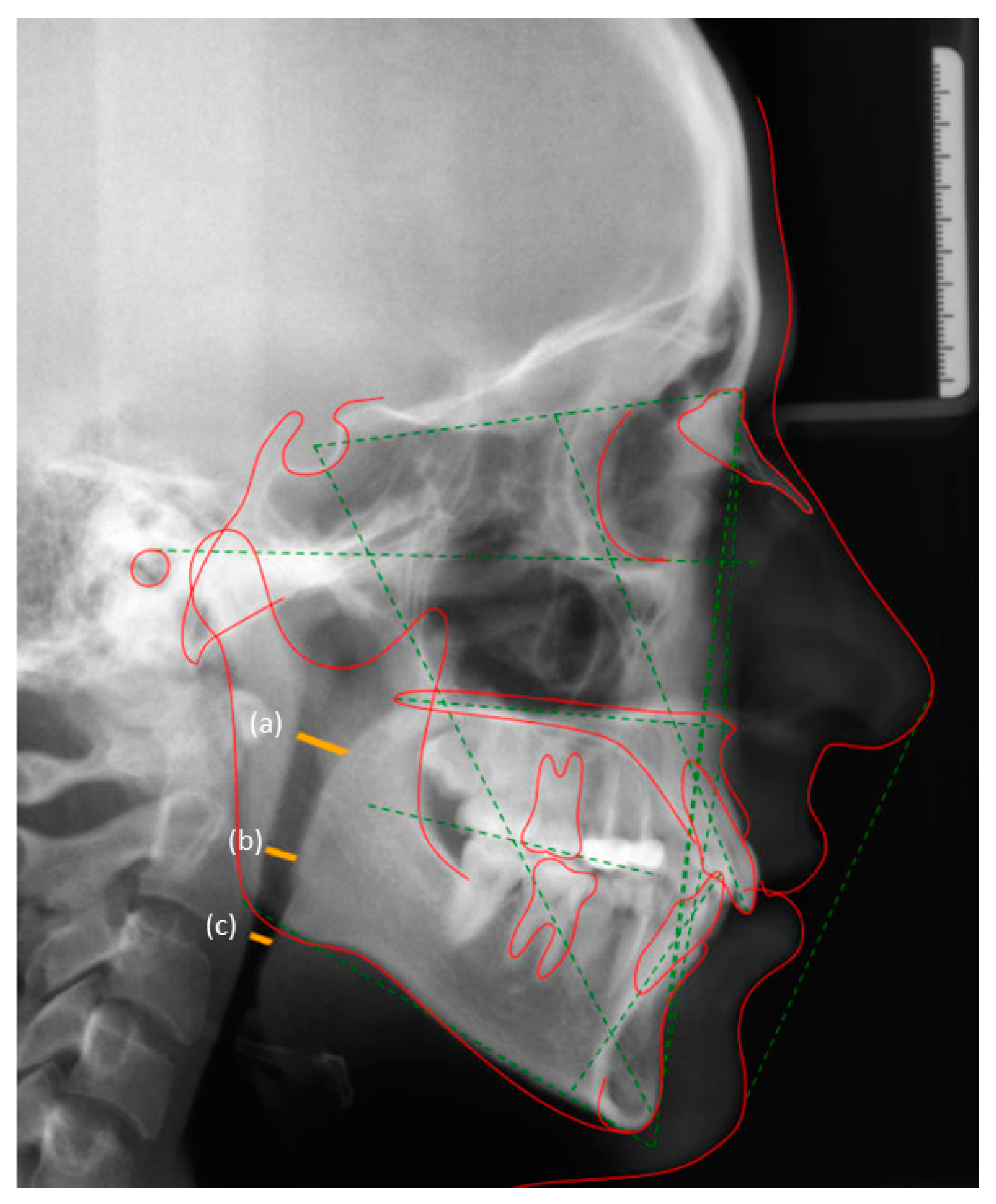
2.7. Cephalometric Measurements
2.8. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Airway Dimensions in Relation to Skeletal Profile
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Stoohs, R.; Guilleminault, C. Obstructive sleep apnea syndrome or abnormal upper airway resistance during sleep? J. Clin. Neurophysiol. 1990, 7, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Chuang, L.C.; Hwang, Y.J.; Lian, Y.C.; Hervy-Auboiron, M.; Pirelli, P.; Huang, Y.S.; Guilleminault, C. Changes in craniofacial and airway morphology as well as quality of life after passive myofunctional therapy in children with obstructive sleep apnea: A comparative cohort study. Sleep Breath 2019, 23, 1359–1369. [Google Scholar] [CrossRef] [PubMed]
- Chambi-Rocha, A.; Cabrera-Domínguez, M.E.; Domínguez-Reyes, A. Breathing mode influence on craniofacial development and head posture. J. Pediatr. 2018, 94, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.S.; Almashraqi, A.A.; Helboub, E.; Almahdi, S.; Jali, T.; Atafi, A.; Alomar, F. Pharyngeal airway spaces in different skeletal malocclusions: A CBCT 3D assessment. Cranio 2019, 1–10. [Google Scholar] [CrossRef] [PubMed]
- AlKawari, H.M.; AlBalbeesi, H.O.; Alhendi, A.A.; Alhuwaish, H.A.; Al Jobair, A.; Baidas, L. Pharyngeal airway dimensional changes after premolar extraction in skeletal class II and class III orthodontic patients. J. Orthod. Sci. 2018, 7, 10, PMC6004743. [Google Scholar] [CrossRef]
- Becker, O.E.; Avelar, R.L.; Göelzer, J.G.; Dolzan Ado, N.; Haas, O.L., Jr.; De Oliveira, R.B. Pharyngeal airway changes in Class III patients treated with double jaw orthognathic surgery—Maxillary advancement and mandibular setback. J. Oral. Maxillofac. Surg. 2012, 70, e639–e647. [Google Scholar] [CrossRef]
- Lee, W.C.; Tu, Y.K.; Huang, C.S.; Chen, R.; Fu, M.W.; Fu, E. Pharyngeal airway changes following maxillary expansion or protraction: A meta-analysis. Orthod. Craniofac. Res. 2018, 21, 4–11. [Google Scholar] [CrossRef]
- Hourfar, J.; Kinzinger, G.S.M.; Feifel, H.; Vehr, V.M.; Lisson, J.A. Effects of combined orthodontic-orthognathic treatment for class II and III correction on posterior airway space: Comparison of mono- and bignathic osteotomies. J. Orofac. Orthop. Fortschr. Kieferorthopadie 2017, 78, 455–465. [Google Scholar] [CrossRef]
- Kavaliauskienė, A.; Šidlauskas, A.; Zaborskis, A. Relationship Between Orthodontic Treatment Need and Oral Health-Related Quality of Life among 11–18-Year-Old Adolescents in Lithuania. Int. J. Environ. Res. Public Health 2018, 15. PMC5982051. [Google Scholar]
- Downs, W.B. Variations in facial relationships; their significance in treatment and prognosis. Am. J. Orthod. 1948, 34, 812–840. [Google Scholar] [CrossRef]
- Arnett, G.W.; Bergman, R.T. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am. J. Orthod. Dentofac. Orthop 1993, 103, 299–312. [Google Scholar] [CrossRef]
- Plaza, S.P.; Reimpell, A.; Silva, J.; Montoya, D. Relationship between skeletal Class II and Class III malocclusions with vertical skeletal pattern. Dental Press J. Orthod. 2019, 24, 63–72, PMC6733235. [Google Scholar] [CrossRef]
- Michelogiannakis, D.; Rossouw, P.E.; Khan, J.; Akram, Z.; Menenakos, E.; Javed, F. Influence of increased body mass index on orthodontic tooth movement and related parameters in children and adolescents: A systematic review of longitudinal controlled clinical studies. J. Orthod. 2019, 46, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, I.S.; Topolski, F.; França, S.N.; Brücker, M.R.; Fernandes, Â. Assessment of skeletal and dental ages of children and adolescents with type 1 diabetes mellitus. Braz. Oral. Res. 2015, 29. [Google Scholar] [CrossRef] [PubMed]
- Daraze, A.; Delatte, M.; Liistro, G.; Majzoub, Z. Cephalometrics of Pharyngeal Airway Space in Lebanese Adults. Int. J. Dent. 2017, 2017, 3959456, PMC5241489 of this paper. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A. Influence of respiratory pattern on craniofacial growth. Angle Orthod 1981, 51, 269–300. [Google Scholar]
- Kirjavainen, M.; Kirjavainen, T. Upper airway dimensions in Class II malocclusion. Effects of headgear treatment. Angle Orthod. 2007, 77, 1046–1053. [Google Scholar] [CrossRef]
- Ortu, E.; Giannoni, M.; Ortu, M.; Gatto, R.; Monaco, A. Oropharyngeal airway changes after rapid maxillary expansion: The state of the art. Int. J. Clin. Exp. Med. 2014, 7, 1632–1638, PMC4132123. [Google Scholar]
- Stefanovic, N.; El, H.; Chenin, D.L.; Glisic, B.; Palomo, J.M. Three-dimensional pharyngeal airway changes in orthodontic patients treated with and without extractions. Orthod. Craniofac. Res. 2013, 16, 87–96. [Google Scholar] [CrossRef]
- Sun, F.C.; Yang, W.Z.; Ma, Y.K. Effect of incisor retraction on three-dimensional morphology of upper airway and fluid dynamics in adult class patients with bimaxillary protrusion. Zhonghua. Kou. Qiang. Yi Xue Za Zhi 2018, 53, 398–403. [Google Scholar]
- Oliveira, P.M.; Cheib-Vilefort, P.L.; de Parsia Gontijo, H.; Melgaco, C.A.; Franchi, L.; McNamara, J.A., Jr.; Souki, B.Q. Three-dimensional changes of the upper airway in patients with Class II malocclusion treated with the Herbst appliance: A cone-beam computed tomography study. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.A.; Park, Y.H. Does upper premolar extraction affect the changes of pharyngeal airway volume after bimaxillary surgery in skeletal class III patients? J. Oral. Maxillofac. Surg. 2014, 72, 165. e1–165. e10. [Google Scholar] [CrossRef] [PubMed]
- Valiathan, M.; El, H.; Hans, M.G.; Palomo, M.J. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010, 80, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Obelenis Ryan, D.P.; Bianchi, J.; Ignácio, J.; Wolford, L.M.; Gonçalves, J.R. Cone-beam computed tomography airway measurements: Can we trust them? Am. J. Orthod. Dentofac. Orthop. 2019, 156, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Niu, X.; Di Carlo, G.; Cornelis, M.A.; Cattaneo, P.M. Three-dimensional analyses of short- and long-term effects of rapid maxillary expansion on nasal cavity and upper airway: A systematic review and meta-analysis. Orthod. Craniofac. Res. 2020, 23, 250–276. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Jiao, D.; Wang, X.; Liu, J.; Martin, D.; Guo, J. Changes in maxillary width and upper airway spaces in young adults after surgically assisted rapid palatal expansion with surgically facilitated orthodontic therapy. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2019, 127, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Ikoma, M.; Arai, K. Craniofacial morphology in women with Class I occlusion and severe maxillary anterior crowding. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Shivaprakash, G. To Evaluate the Correlation Between Skeletal and Dental Parameters to the Amount of Crowding in Class II Div. 1 Malocclusions. J. Clin. Diagn. Res. 2017, 11, Zc22–Zc27, PMC5713849. [Google Scholar] [CrossRef] [PubMed]
- Tseng, L.L.; Chang, C.H.; Roberts, W.E. Diagnosis and conservative treatment of skeletal Class III malocclusion with anterior crossbite and asymmetric maxillary crowding. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 555–566. [Google Scholar] [CrossRef] [PubMed]
- Kurosawa, M.; Ando, K.; Goto, S. Class II Division 1 malocclusion with a high mandibular plane angle corrected with 2-phase treatment. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Xia, S.; Dai, H.W.; Zhang, Y.; Wang, C.; Wang, H.Q. Changes of upper airway in ClassⅡchildren with high mandibular plane angle before and after functional treatment by high headgear-activator. Shanghai Kou Qiang Yi Xue 2018, 27, 270–274. [Google Scholar] [PubMed]
- Hu, Z.; Yin, X.; Liao, J.; Zhou, C.; Yang, Z.; Zou, S. The effect of teeth extraction for orthodontic treatment on the upper airway: A systematic review. Sleep Breath 2015, 19, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Yuan, L.; Wang, B.; Zhang, L.; Shen, G.; Fang, B. Changes of alveolar bone dehiscence and fenestration after augmented corticotomy-assisted orthodontic treatment: A CBCT evaluation. Prog. Orthod. 2019, 20, 7, PMC6378319. [Google Scholar] [CrossRef] [PubMed]
- Crimi, S.; Defila, L.; Nanni, M.; Cicciù, M.; Fiorillo, L.; Cervino, G.; Marchetti, C.; Bianchi, A. Three-Dimensional Evaluation on Cortical Bone During Orthodontic Surgical Treatment. J. Craniofac. Surg. 2020, 31, 1637–1646. [Google Scholar] [CrossRef] [PubMed]
- Al-Okshi, A.; Lindh, C.; Salé, H.; Gunnarsson, M.; Rohlin, M. Effective dose of cone beam CT (CBCT) of the facial skeleton: A systematic review. Br. J. Radiol. 2015, 88, 20140658, PMC4277388. [Google Scholar] [CrossRef]
- Lenza, M.G.; Lenza, M.M.; Dalstra, M.; Melsen, B.; Cattaneo, P.M. An analysis of different approaches to the assessment of upper airway morphology: A CBCT study. Orthod. Craniofac. Res. 2010, 13, 96–105. [Google Scholar] [CrossRef]
| Skeletal Profiles | ||||
|---|---|---|---|---|
| Parameters | Skeletal Class-I | Skeletal Class-II | Skeletal Class-III | Control Individuals |
| Number of participants/lateral cephalograms (n) | 58 | 58 | 58 | 29 |
| Gender (male:female) | 28:30 | 29:29 | 27:31 | 14:15 |
| Overall age in years (mean ± SD) | 15.6 ± 0.7 years | 15.3 ± 0.5 years | 15.8 ± 0.5 years | 15.6 ± 0.6 years |
| Males | 15.9 ± 0.3 years | 15.2 ± 0.2 years | 15.5 ± 0.4 years | 15.2 ± 0.3 years |
| Females | 15.4 ± 0.4 years | 15.5 ± 0.3 years | 16 ± 0.1 years | 15.8 ± 0.2 years |
| Skeletal Pattern | Airway Dimensions | |||
|---|---|---|---|---|
| Airway Space | Pre-Treatment (T0) | Post-Treatment (T1) | No Treatment | |
| Class-I | Nasopharynx | 22.51 ± 2.08 | 22.75 ± 1.3 | NA |
| Oropharynx | 19.33 ± 0.95 | 19.35 ± 0.88 | NA | |
| Hypopharynx | 20.15 ± 1.54 | 20.18 ± 1.25 | NA | |
| Class-II | Nasopharynx | 23.44 ± 2.64 | 24.05 ± 3.61 | NA |
| Oropharynx | 19.46 ± 3.36 | 19.52 ± 3.19 | NA | |
| Hypopharynx | 20.25 ± 4.11 | 20.22± 4.15 | NA | |
| Class-III | Nasopharynx | 23.58 ± 4.64 | 23.33 ± 4.28 | NA |
| Oropharynx | 21.5 ± 3.17 | 21.61 ± 3.42 | NA | |
| Hypopharynx | 21.28 ± 4.47 | 21.32 ± 4.08 | NA | |
| Control group | Nasopharynx | NA | NA | 21.32 ± 1.64 |
| Oropharynx | NA | NA | 20.27 ± 1.16 | |
| Hypopharynx | NA | NA | 20.52 ± 3.6 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Senani, Y.; Al Shammery, A.J.; Al Nafea, A.; Al Absi, N.; Al Kadhi, O.; Al-Shammery, D. Influence of Fixed Orthodontic Therapy on Pharyngeal Airway Dimensions after Correction of Class-I, -II and -III Skeletal Profiles in Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 517. https://doi.org/10.3390/ijerph18020517
Al Senani Y, Al Shammery AJ, Al Nafea A, Al Absi N, Al Kadhi O, Al-Shammery D. Influence of Fixed Orthodontic Therapy on Pharyngeal Airway Dimensions after Correction of Class-I, -II and -III Skeletal Profiles in Adolescents. International Journal of Environmental Research and Public Health. 2021; 18(2):517. https://doi.org/10.3390/ijerph18020517
Chicago/Turabian StyleAl Senani, Yara, Al Jouharah Al Shammery, Abeer Al Nafea, Nisreen Al Absi, Omar Al Kadhi, and Deema Al-Shammery. 2021. "Influence of Fixed Orthodontic Therapy on Pharyngeal Airway Dimensions after Correction of Class-I, -II and -III Skeletal Profiles in Adolescents" International Journal of Environmental Research and Public Health 18, no. 2: 517. https://doi.org/10.3390/ijerph18020517
APA StyleAl Senani, Y., Al Shammery, A. J., Al Nafea, A., Al Absi, N., Al Kadhi, O., & Al-Shammery, D. (2021). Influence of Fixed Orthodontic Therapy on Pharyngeal Airway Dimensions after Correction of Class-I, -II and -III Skeletal Profiles in Adolescents. International Journal of Environmental Research and Public Health, 18(2), 517. https://doi.org/10.3390/ijerph18020517






