A Mixed-Methods Systematic Review of the Impacts of Coronavirus on Society and Culture
Abstract
1. Introduction
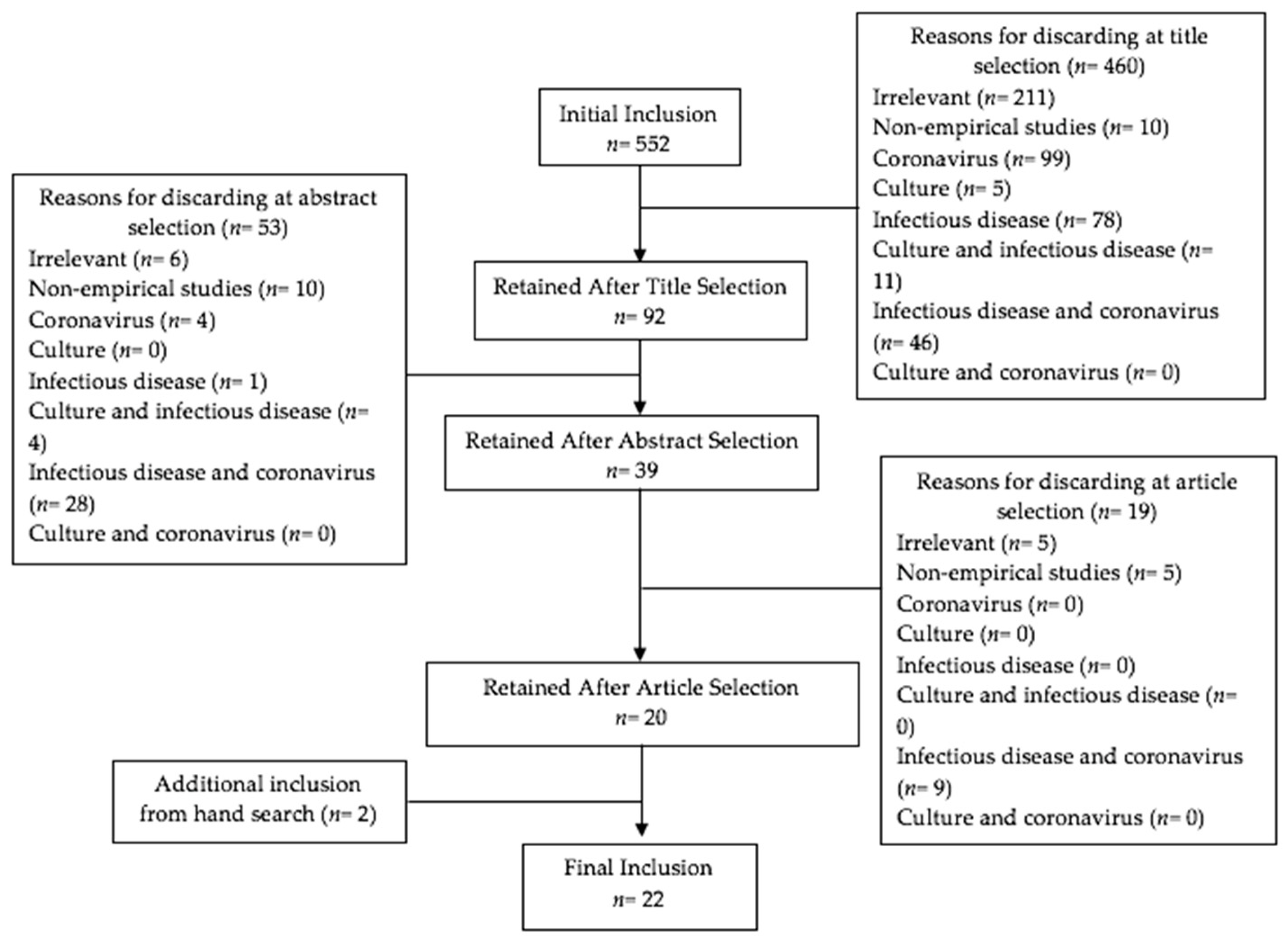
2. Methods
2.1. Search Strategy and Selection Criteria
2.2. Data Sources and Data Abstraction
3. Results
3.1. Characteristics of the Reviewed Studies
3.1.1. Study Sites and Publication Period
3.1.2. Study Design and Target Population
3.2. Theme
3.2.1. Governance
3.2.2. Crisis Communication and Public Knowledge
3.2.3. Stigma and Discrimination
3.2.4. Social Compliance of Preventive Measures
3.2.5. Social Experience as Healthcare Workers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Napier, A.D.; Ancarno, C.; Butler, B.; Calabrese, J.; Chater, A.; Chatterjee, H.; Guesnet, F.; Horne, R.; Jacyna, S.; Jadhav, S.; et al. Culture and Health. Lancet 2014, 384, 1607–1639. [Google Scholar] [CrossRef]
- Affonso, D.D.; Andrews, G.J.; Jeffs, L. The Urban Geography of SARS: Paradoxes and Dilemmas in Toronto’s Health Care. J. Adv. Nurs. 2004, 45, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Eichelberger, L. SARS and New York’s Chinatown: The Politics of Risk and Blame during an Epidemic of Fear. Soc. Sci. Med. 2007, 65, 1284–1295. [Google Scholar] [CrossRef] [PubMed]
- Siu, Y.M.J. The Sars-Associated Stigma of SARS Victims in the Post-Sars Era of Hong Kong. Qual. Health Res. 2008, 18, 729–738. [Google Scholar] [CrossRef] [PubMed]
- Patrick, W.; Nerlich, B. Disease Metaphors in New Epidemics: The UK Media Framing of the 2003 SARS Epidemic. Soc. Sci. Med. 2005, 60, 2629–2639. [Google Scholar] [CrossRef]
- O’Sullivan, T.L.; Amaratunga, C.A.; Hardt, J.; Dow, D.; Phillips, K.P.; Corneil, W. Are We Ready? Evidence of Support Mechanisms for Canadian Health Care Workers in Multi-Jurisdictional Emergency Planning. Can. J. Public Health 2007, 98, 358–363. [Google Scholar] [CrossRef]
- Park, J.S.; Lee, E.H.; Park, N.R.; Choi, Y.H. Mental Health of Nurses Working at a Government-Designated Hospital during a MERS-CoV Outbreak: A Cross-Sectional Study. Arch. Psychiatr. Nurs. 2018, 32, 2–6. [Google Scholar] [CrossRef]
- Almutairi, K.M.; Al Helih, E.M.; Moussa, M.; Boshaiqah, A.E.; Alajilan, A.S.; Vinluan, J.M.; Almutairi, A. Awareness, Attitudes, and Practices Related to Coronavirus Pandemic among Public in Saudi Arabia. Fam. Community Health 2015, 38, 332–340. [Google Scholar] [CrossRef]
- Ludolph, R.; Schulz, P.J.; Chen, L. Investigating the Effects of Mass Media Exposure on the Uptake of Preventive Measures by Hong Kong Residents during the 2015 MERS Outbreak: The Mediating Role of Interpersonal Communication and the Perception of Concern. J. Health Commun. 2018, 23, 1–8. [Google Scholar] [CrossRef]
- Yoo, W.; Choi, D.H.; Park, K. The Effects of SNS Communication: How Expressing and Receiving Information Predict MERS-Preventive Behavioral Intentions in South Korea. Comput. Hum. Behav. 2016, 62, 34–43. [Google Scholar] [CrossRef]
- Choi, J.S.; Kim, J.S. Factors Influencing Emergency Nurses’ Ethical Problems during the Outbreak of MERS-CoV. Nurs. Ethics 2018, 25, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, A.S.; Wiley, K.E.; Tashani, M.; Willaby, H.W.; Heywood, A.E.; BinDhim, N.F.; Booy, R.; Rashid, H. Exploring Barriers to and Facilitators of Preventive Measures against Infectious Diseases among Australian Hajj Pilgrims: Cross-Sectional Studies before and after Hajj. Int. J. Infect. Dis. 2016, 47, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.; Chun, B.C. An Interim Review of the Epidemiological Characteristics of 2019 Novel Coronavirus. Epidemiol. Health 2020, 42, e2020006. [Google Scholar] [CrossRef] [PubMed]
- Badawi, A.; Ryoo, S.G. Prevalence of Comorbidities in the Middle East Respiratory Syndrome Coronavirus (MERS-CoV): A Systematic Review and Meta-Analysis. Int. J. Infect. Dis. 2016, 49, 129–133. [Google Scholar] [CrossRef]
- Momattin, H.; Mohammed, K.; Zumla, A.; Memish, Z.A.; Al-Tawfiq, J.A. Therapeutic Options for Middle East Respiratory Syndrome Coronavirus (MERS-CoV)—Possible Lessons from a Systematic Review of SARS-CoV Therapy. Int. J. Infect. Dis. 2013, 17, e792–e798. [Google Scholar] [CrossRef]
- Petersen, E.; Memish, Z.A.; Zumla, A.; Al Maani, A. Transmission of Respiratory Tract Infections at Mass Gathering Events. Curr. Opin. Pulm. Med. 2020, 26, 197–202. [Google Scholar] [CrossRef]
- Barasheed, O.; Alfelali, M.; Mushta, S.; Bokhary, H.; Alshehri, J.; Attar, A.A.; Booy, R.; Rashid, H. Uptake and Effectiveness of Facemask against Respiratory Infections at Mass Gatherings: A Systematic Review. Int. J. Infect. Dis. 2016, 47, 105–111. [Google Scholar] [CrossRef]
- Denzin, N.K.; Lincoln, Y.S. (Eds.) The SAGE Handbook of Qualitative Research; Sage: Thousand Oaks, CA, USA, 2005. [Google Scholar]
- Tashakkori, A.; Creswell, J.W. Envisioning the Future Stewards of the Social-Behavioural Research Enterprise. J. Mix. Methods Res. 2008, 2, 291–295. [Google Scholar] [CrossRef]
- De Zwart, O.; Veldhuijzen, I.K.; Elam, G.; Aro, A.R.; Abraham, T.; Bishop, G.D.; Voeten, H.A.; Richardus, J.H.; Brug, J. Perceived Threat, Risk Perception, and Efficacy Beliefs Related to SARS and Other (Emerging) Infectious Diseases: Results of an International Survey. Int. J. Behav. Med. 2009, 16, 30–40. [Google Scholar] [CrossRef]
- Park, M. Infectious Disease-Related Laws: Prevention and Control Measures. Epidemiol. Health 2017, 39, e2017033. [Google Scholar] [CrossRef][Green Version]
- Gautret, P.; Benkouiten, S.; Al-Tawfiq, J.A.; Memish, Z.A. The Spectrum of Respiratory Pathogens among Returning Hajj Pilgrims: Myths and Reality. Int. J. Infect. Dis. 2016, 47, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Alhomoud, F.; Alhomoud, F. ‘Your Health Essential for Your Hajj’: Muslim Pilgrims’ Knowledge, Attitudes and Practices Regarding Middle East Respiratory Syndrome Coronavirus (MERS-CoV) during Hajj Season. J. Infect. Chemother. 2017, 23, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Des Jarlais, D.C.; Stuber, J.; Tracy, M.; Tross, S.; Galea, S. Social Factors Associated with AIDS and SARS. Emerg. Infect. Dis. 2005, 11, 1767. [Google Scholar] [CrossRef] [PubMed]
- Cava, M.A.; Fay, K.E.; Beanlands, H.J.; McCay, E.A.; Wignall, R. The Experience of Quarantine for Individuals Affected by SARS in Toronto. Public Health Nurs. 2005, 22, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Crawford, R.; Rutz, D.C.; Evans, D.P. ‘Between Combat Boots and Birkenstocks’–Lessons from HIV/AIDS, SARS, H1N1 and Ebola. Public Health 2016, 141, 186–191. [Google Scholar] [CrossRef]
- Voeten, H.A.C.M.; de Zwart, O.; Veldhuijzen, I.K.; Yuen, C.; Jiang, X.; Elam, G.; Abraham, T.; Brug, J. Sources of Information and Health Beliefs Related to SARS and Avian Influenza among Chinese Communities in the United Kingdom and the Netherlands, Compared to the General Population in These Countries. Int. J. Behav. Med. 2009, 16, 49–57. [Google Scholar] [CrossRef]
- Oh, S.H.; Lee, S.Y.; Han, C. The Effects of Social Media Use on Preventive Behaviors during Infectious Disease Outbreaks: The Mediating Role of Self-Relevant Emotions and Public Risk Perception. Health Commun. 2020. [Google Scholar] [CrossRef]
- Qiu, W.; Chu, C.; Mao, A.; Wu, J. The Impacts on Health, Society, and Economy of SARS and H7N9 Outbreaks in China: A Case Comparison Study. J. Environ. Public Health 2018, 2018, 2710185. [Google Scholar] [CrossRef]
- Straus, S.E.; Wilson, K.; Rambaldini, G.; Rath, D.; Lin, Y.; Gold, W.L.; Kapral, M.K. Severe Acute Respiratory Syndrome and Its Impact on Professionalism: Qualitative Study of Physicians’ Behaviour during an Emerging Healthcare Crisis. Br. Med. J. 2004, 329, 83–85. [Google Scholar] [CrossRef]
- Kang, M.; Kim, J.R.; Cha, H. From Concerned Citizens to Activists: A Case Study of 2015 South Korean MERS Outbreak and the Role of Dialogic Government Communication and Citizens’ Emotions on Public Activism. J. Public Relat. Res. 2018, 30, 202–229. [Google Scholar] [CrossRef]
- Han, X.; Wang, J.; Zhang, M.; Wang, X. Using Social Media to Mine and Analyze Public Opinion Related to COVID-19 in China. Int. J. Environ. Res. Public Health 2020, 17, 2788. [Google Scholar] [CrossRef] [PubMed]
- La, V.-P.; Pham, T.-H.; Ho, M.-T.; Nguyen, M.-H.; Nguyen, P.K.-L.; Vuong, T.-T.; Nguyen, H.-K.T.; Tran, T.; Khuc, Q.; Ho, M.-T.; et al. Policy Response, Social Media and Science Journalism for the Sustainability of the Public Health System Amid the COVID-19 Outbreak: The Vietnam Lessons. Sustainability 2020, 12, 2931. [Google Scholar] [CrossRef]
- Nguyen, N.H.; Van Nguyen, T.; Nguyen, A.Q.; Van Nguyen, P.; Nguyen, T.N.M. The first cohort of the COVID-19 patients in Vietnam and the national response to the pandemic. Int. J. Med. Sci. 2020, 17, 2449–2453. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. COVID-19 and the Consequences of Isolating the Elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef]
- Galmés, S.; Serra, F.; Palou, A. Current State of Evidence: Influence of Nutritional and Nutrigenetic Factors on Immunity in the COVID-19 Pandemic Framework. Nutrients 2020, 12, 2738. [Google Scholar] [CrossRef]
- Atabani, S.F.; Wilson, S.; Overton-Lewis, C.; Workman, J.; Kidd, I.M.; Petersen, E.; Zumla, A.; Smit, E.; Osman, H. Active Screening and Surveillance in the United Kingdom for Middle East Respiratory Syndrome Coronavirus in Returning Travellers and Pilgrims from the Middle East: A Prospective Descriptive Study for the Period 2013–2015. Int. J. Infect. Dis. 2016, 47, 10–14. [Google Scholar] [CrossRef]
- AlAfnan, M.A. COVID 19-The Foreign Virus: Media Bias, Ideology and Dominance in Chinese and American Newspaper Articles. Int. J. Appl. Linguist. Engl. Lit. 2020, 9, 56. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental Health Problems and Social Media Exposure during COVID-19 Outbreak. PLoS ONE 2020, 15, e231924. [Google Scholar] [CrossRef]
- Oh, N.; Hong, N.S.; Ryu, D.H.; Bae, S.G.; Kam, S.; Kim, K.Y. Exploring Nursing Intention, Stress, and Professionalism in Response to Infectious Disease Emergencies: The Experience of Local Public Hospital Nurses During the 2015 MERS Outbreak in South Korea. Asian Nurs. Res. 2017, 11, 230–236. [Google Scholar] [CrossRef]
- Lee, S.M.; Kang, W.S.; Cho, A.R.; Kim, T.; Park, J.K. Psychological Impact of the 2015 MERS Outbreak on Hospital Workers and Quarantined Hemodialysis Patients. Compr. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef]
- Budhwani, H.; Sun, R. Referencing the Novel Coronavirus as the ‘Chinese Virus’ or ‘China Virus’ on Twitter: COVID-19 Stigma (Preprint). J. Med. Internet Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.O.; Bayer, R.; Fairchild, A.L. Ethical and Legal Challenges Posed by Severe Acute Respiratory Syndrome: Implications for the Control of Severe Infectious Disease Threats. J. Am. Med Assoc. 2003, 290, 3229–3237. [Google Scholar] [CrossRef] [PubMed]
| Authors (Year) | Ref # | Theme 1 Governance | Theme 2 Communication and Public Knowledge | Theme 3 Stigma and Discrimination | Theme 4 Social Compliance | Theme 5 Health Workers | Study Site | Study Sample and Size | Study Design |
|---|---|---|---|---|---|---|---|---|---|
| O’Sullivan et al. (2007) | 6 | Governance | Health Workers | Canada | 12 emergency plans | Qualitative content analysis | |||
| Almutairi et al. (2015) | 8 | Communication and Public Knowledge | Social Compliance | Riyadh, Saudi Arabia | 1147 male and female Saudis and expatriates 18 years and older in shopping malls | Quantitative Cross-sectional | |||
| Wallis & Nerlich (2005) | 5 | Communication and Public Knowledge | Stigma and discrimination | United Kingdom | 5 UK newspapers | Qualitative linguistic method | |||
| Alqahtani et al. (2016) | 12 | Communication and Public Knowledge | Social Compliance | Australia | 356 Australian Hajj pilgrims | Quantitative Two Cross-sectional surveys | |||
| Choi & Kim (2018) | 11 | Stigma and discrimination | Health Workers | South Korea (3 cities) | 169 emergency nurses | Quantitative Cross-sectional | |||
| Park (2017) | 21 | Governance | South Korea | Legislative procedure of the Infectious Disease Control and Prevention Act | N/A | ||||
| Ludolph et al. (2018) | 9 | Communication and Public Knowledge | Hong Kong, China | 533 Hong Kong residents | Quantitative Cross-sectional survey | ||||
| Park et al. (2018) | 7 | Governance | Stigma and discrimination | Health Workers | Gyeonggi, South Korea | 187 nurses | Quantitative Cross-sectional exploratory | ||
| de Zwart et al. (2009) | 20 | Communication and Public Knowledge | Europe (5 countries) and Asia (3 countries) | 3436 respondents interviewed over the phone | Quantitative Survey | ||||
| Eichelberger (2007) | 3 | Stigma and discrimination | New York City, NY | 37 community members of New York’s Chinatown | Qualitative Participant observation | ||||
| Straus et al. (2004) | 29 | Health Workers | Toronto, Canada | 14 physicians in specialties involving SARS patients | Qualitative interviews | ||||
| Des Jarlais et al. (2005) | 24 | Communication and Public Knowledge | Stigma and discrimination | New York City, NY | 1832 New York City residents | Quantitative Phone interview | |||
| Voeton et al. (2009) | 27 | Communication and Public Knowledge | United Kingdom and The Netherlands | 299 British and Dutch Chinese people’s knowledge of SARS compared to 804 British and Dutch non-Chinese people | Quantitative Computer assisted phone survey | ||||
| Yoo et al. (2016) | 10 | Communication and Public Knowledge | Social Compliance | South Korea | 1000 Korean adults 19 or older of nationally represented demographics | Quantitative Online survey | |||
| Oh et al. (2020) | 28 | Communication and Public Knowledge | South Korea | 400 individuals chosen based on age, gender, and region | Quantitative Online survey | ||||
| Cava et al. (2005) | 25 | Stigma and discrimination | Toronto, Canada | 21 English speaking individuals exposed to SARS during the outbreak in Toronto | Qualitative | ||||
| Qiu et al. (2018) | 30 | Stigma and discrimination | China | Literature review, document analysis, and 26 in-depth interviews with key stakeholders were conducted. | Qualitative case study | ||||
| Siu (2008) | 4 | Stigma and discrimination | Hong Kong, China | 200 members of a self-help group for SARS victims, 30 participated in in-depth semi-structured interviews. | Qualitative participant observation | ||||
| Gautret et al. (2016) | 22 | Social Compliance | Middle East | Large scale surveillance study of people traveling back to the Middle East. | Quantitative Surveillance study | ||||
| Affonso et al. (2003) | 2 | Health Workers | Toronto, Canada | Reviewed public health records, governmental and non-governmental health statements, initial epidemiological research done on SARS, and firsthand experiences of healthcare systems. | N/A | ||||
| Crawford et al. (2016) | 26 | Governance | N/A | 21 individuals who were key responders in recent epidemics participated in interviews. | Qualitative Non-systematic review | ||||
| Alhomoud and Alhomoud (2017) | 23 | Social Compliance | Mecca, Saudi Arabia | 257 pilgrims that participated in Hajj 2015 who were 18+ and spoke English or Arabic | Quantitative Cross-sectional study |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, Y.J.; Park, Y.S.; Keller, A.; Noh, J.-W.; Cha, J. A Mixed-Methods Systematic Review of the Impacts of Coronavirus on Society and Culture. Int. J. Environ. Res. Public Health 2021, 18, 491. https://doi.org/10.3390/ijerph18020491
Yu YJ, Park YS, Keller A, Noh J-W, Cha J. A Mixed-Methods Systematic Review of the Impacts of Coronavirus on Society and Culture. International Journal of Environmental Research and Public Health. 2021; 18(2):491. https://doi.org/10.3390/ijerph18020491
Chicago/Turabian StyleYu, Yeon Jung, Young Su Park, Alison Keller, Jin-Won Noh, and Jiho Cha. 2021. "A Mixed-Methods Systematic Review of the Impacts of Coronavirus on Society and Culture" International Journal of Environmental Research and Public Health 18, no. 2: 491. https://doi.org/10.3390/ijerph18020491
APA StyleYu, Y. J., Park, Y. S., Keller, A., Noh, J.-W., & Cha, J. (2021). A Mixed-Methods Systematic Review of the Impacts of Coronavirus on Society and Culture. International Journal of Environmental Research and Public Health, 18(2), 491. https://doi.org/10.3390/ijerph18020491






