Comparison between Three Therapeutic Options for the Treatment of Balance and Gait in Stroke: A Randomized Controlled Trial
Abstract
1. Introduction
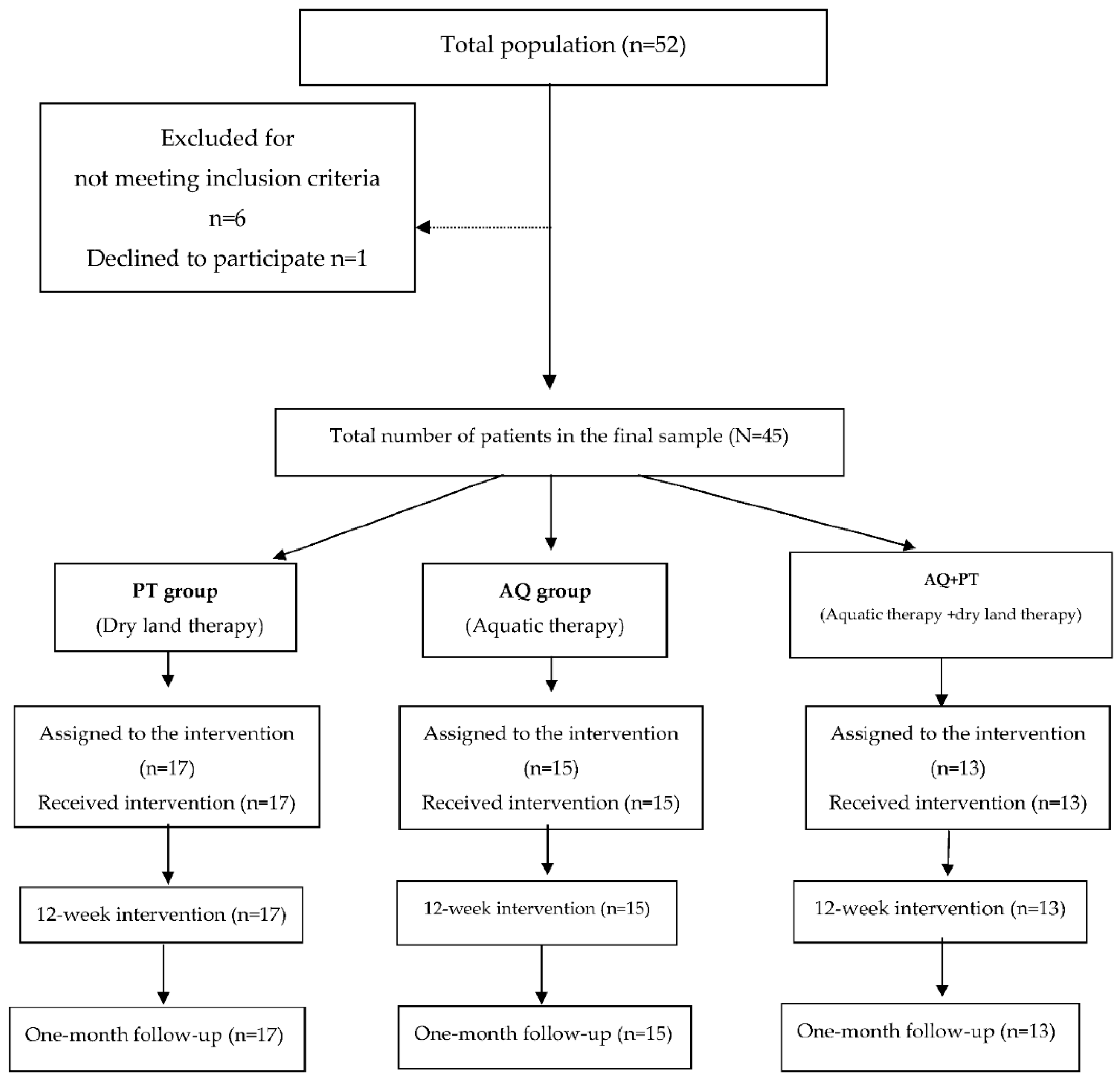
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Outcome Measures
2.4. Intervention
2.4.1. Dry Land Therapy (PT Group)
2.4.2. Aquatic Ai Chi (AQ Group)
2.4.3. Combined Group (AQ + PT Group)
2.5. Statistical Analysis
3. Results
4. Discussion
Study Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Langhorne, P.; Stott, D.J.; Robertson, L. Medical complications after stroke: A multicenter study. Stroke 2000, 31, 1223–1229. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Tyson, S.F.; Hanley, M.; Chillala, J.; Selley, A.; Tallis, R.C. Balance disability after stroke. Phys. Ther. 2006, 86, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Whitney, J.C.; Lord, S.R. Effective exercise for the prevention of falls: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2008, 56, 2234–2243. [Google Scholar] [CrossRef] [PubMed]
- Kenny, R.A.; Rubenstein, L.Z.; Tinetti, M.E. Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society: Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar]
- Morer, C.; Boestad, C.; Zuluaga, P.; Álvarez-Badillo, A.; Maraver, F. Effects of an intensive thalassotherapy and aquatic therapy program in stroke patients. A pilot study. Rev. Neurol. 2017, 16, 249–256. [Google Scholar]
- Lee, M.E.; Jo, G.Y.; Do, H.K.; Choi, H.E.; Kim, W.J. Efficacy of Aquatic Treadmill Training on Gait Symmetry and Balance in Subacute Stroke Patients. Ann. Rehabil. Med. 2017, 41, 376–386. [Google Scholar] [CrossRef]
- Kim, K.; Lee, D.K.; Kim, E.K. Effect of aquatic dual-task training on balance and gait in stroke patients. J. Phys. Ther. Sci. 2016, 28, 2044–2047. [Google Scholar] [CrossRef][Green Version]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A. American College of Sports Medicine: American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- Bommer, A.; Lambeck, J.F. Ai chi: Applications in clinical practice. Chapter 7. In Comprehensive Aquatic Therapy, 3rd ed.; Becker, B.E., Cole, A.J., Eds.; Washington State University Press: Washington, DC, USA, 2011; pp. 171–191. [Google Scholar]
- Pérez-de la Cruz, S.; García- Luengo, A.V.; Lambeck, J. Effects of an Ai Chi fall prevention programme for patients with Parkinson’s disease. Neurología 2016, 31, 176–182. [Google Scholar] [CrossRef]
- Bayraktar, D.; Guclu-Gunduz, A.; Yazici, G.; Lambeck, J.; Batur-Caglayan, H.Z.; Irkec, C.; Nazliel, B. Effects of Ai-Chi on balance, functional mobility, strength and fatigue in patients with multiple sclerosis: A pilot study. NeuroRehabilitation 2013, 33, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health 1992, 83, 7–11. [Google Scholar]
- Fernandez-Alonso, L.; Muñoz-García, T.; Fernandez-Alonso, L.; Muñoz-García, D.; Touche, R.L. The level of physical activity affects the health of older adults despite being active. J. Exerc. Rehabil. 2016, 12, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Briggs, R.; Gossman, M.; Birch, R.; Drews, J.; Shaddeau, S. Balance performance among noninstitutionalized elderly women. Phys. Ther. 1989, 69, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Broetz, D.; Fichner, M.; Gasser, T.; Weller, M.; Steinbach, J.P. Radicular and nonradicular back pain in Parkinson’s disease: A controlled study. Mov. Disord. 2007, 22, 853–856. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “Up & go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Salinet, A.S.M. Hidroterapia e Reabilitação Car-diorrespiratória após Acidente Vascular Cerebral. Rev. Neurocienc. 2012, 20, 183–184. [Google Scholar] [CrossRef]
- Batistela, A.C.T.; Junior, L.C.F.; Leonello, L.A.; Carraro, L.; Meneghetti, C.H.Z. A influência da fisioterapia aquática na função e equilíbrio no acidente vascular cerebral. Rev. Neurocienc. 2012, 20, 410–414. [Google Scholar]
- Borges, M.A.; Paizan, N.L.M.; Da Silva, R. Hidrotherapy: Coadjuvant treatment to kinesiotherapy in patients with sequels after stroke. Rev. Neurocienc. 2009, 17, 314–318. [Google Scholar]
- Lee, D.; Ko, T.; Cho, Y. Effect on static or dynamic balance of task-oriented training for patients in water or on land. J. Phys. Ther. Sci. 2010, 22, 331–336. [Google Scholar] [CrossRef]
- Xie, G.; Wang, T.; Jiang, B.; Su, Y.; Tang, X.; Guo, Y.; Liao, J. Effects of hydrokinesitherapy on balance and walking ability in stroke survivors: A systematic review and meta-analysis of randomized controlled studies. Eur. Rev. Aging Phys. Act 2019, 13, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Montagna, J.C.; Santos, B.C.; Battistuzzo, C.R.; Loureiro, A.P.C. Effects of aquatic physiotherapy on the improvement of balance and corporal symmetry in stroke. Int. J. Clin. Exp. Med. 2014, 7, 1182–1187. [Google Scholar] [PubMed]
- Dong Koog, N.; Lim, J.-Y.; Shin, H.-I.; Paik, N.-J. The effect of aquatic therapy on postural balance and muscle strength in stroke survivors—A randomized controlled pilot trial. Clin. Rehabil. 2008, 22, 966–976. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Gramage, J.; Sebastián-Mengod, A.; Amer-Cuenca, J.J.; Barcia-González, J. Efectos de un programa combinado de ejercicio físico y Halliwick sobre la hipertonía en personas adultas con lesión cerebral. Estudio piloto. Fisioterapia 2010, 32, 139–144. [Google Scholar] [CrossRef]
- Tripp, F.; Krakow, K. Effects of an aquatic therapy approach (Halliwick-Therapy) on functional mobility in subacute stroke patients: A randomized controlled trial. Clin. Rehabil. 2014, 28, 432–439. [Google Scholar] [CrossRef]
- Pérez-de la Cruz, S. A bicentric controlled study on the effects of aquatic Ai Chi in Parkinson disease. Complement. Ther. Med. 2018, 36, 147–153. [Google Scholar] [CrossRef]
- Temperoni, G.; Curcio, A.; Iosa, M.; Mangiarotti, M.A.; Morelli, D.; De Angelis, S.; Vergano, S.; Tramontano, M. A Water-Based Sequential Preparatory Approach vs. Conventional Aquatic Training in Stroke Patients: A Randomized Controlled Trial With a 1-Month Follow-Up. Front Neurol. 2020, 11, 466. [Google Scholar] [CrossRef]
- Skinner, E.H.; Dinh, T.; Hewitt, M.; Piper, R.; Thwaites, C. An Ai Chi-based aquatic group improves balance and reduces falls in community-dwelling adults: A pilot observational cohort study. Physiother. Theory Pract. 2016, 32, 581–590. [Google Scholar] [CrossRef]
- Zhu, Z.; Cui, L.; Yin, M. Hydrotherapy vs. conventional land-based exercise for improving walking and balance after stroke: A randomized controlled trial. Clin. Rehabil. 2015, 30, 587–593. [Google Scholar] [CrossRef]
- Cronin, N.J.; Valtonen, A.M.; Waller, B.; Pöyhönen, T.; Avela, J. Effects of short term water immersion on peripheral reflex excitability in hemiplegic and healthy individuals: A preliminary study. J. Musculoskelet. Neuronal Interact. 2016, 16, 58–62. [Google Scholar]
- Yang, Y.R.; Chen, Y.C.; Lee, C.S. Dual-task-related gait changes in individuals with stroke. Gait Posture 2007, 25, 185–190. [Google Scholar] [CrossRef] [PubMed]
- An, H.J.; Kim, J.I.; Kim, Y.R. The effect of various dual task training methods with gait on the balance and gait of patients with chronic stroke. J. Phys. Ther. Sci. 2014, 26, 1287–1291. [Google Scholar] [CrossRef]
- Han, S.K.; Kim, M.C.; An, C.S. Comparison of effects of a proprioceptive exercise program in water and on land the balance of chronic stroke patients. J. Phys. Ther. Sci. 2013, 25, 1219–1222. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cider, A.; Schaufelberger, M.; Sunnerhagen, K.S. Hydrotherapy—A new approach to improve function in the older patient with chronic heart failure. Eur. J. Heart Fail. 2003, 5, 527–535. [Google Scholar] [CrossRef]
- Arnold, C.M.; Busch, A.J.; Schachter, C.L. A randomized clinical trial of aquatic versus land exercise to improve balance, function, and quality of life in older women with osteoporosis. Physiother. Can. 2008, 60, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Dean, C.M.; Richards, C.L.; Malouin, F. Task-related circuit training improves performance of locomotor tasks in chronic stroke: A randomized, controlled pilot trial. Arch. Phys. Med. Rehabil. 2000, 81, 409–417. [Google Scholar] [CrossRef] [PubMed]
| Participants | p | |||
|---|---|---|---|---|
| AQ + PT Group (n = 13) | PT Group (n = 17) | AQ Group (n = 15) | ||
| Age (years) | 61.4 (13.9) | 62.7 (13.4) | 63.8 (13.6) | 0.896 |
| Sex | 0.672 | |||
| Females | 5 (38.5) | 9 (52.9) | 8 (53.3) | |
| Males | 8 (61.5) | 8 (47.1) | 7 (46.7) | |
| Clinical history | 0.754 | |||
| No | 10 (76.9) | 11 (64.7) | 10 (66.7) | |
| Yes | 3 (23.1) | 6 (35.3) | 5 (33.3) | |
| Surgical interventions | 0.254 | |||
| No | 3 (23.1) | 9 (52.9) | 6 (40) | |
| Yes | 10 (76.9) | 8 (47.1) | 9 (60) | |
| Medication | 0.059 | |||
| No | 4 (30.8) | 0 (0) | 3 (20) | |
| Yes | 9 (69.2) | 17 (100) | 12 (80) | |
| BMI (kg/m2) | 25.4 (2.7) | 24.6 (2.3) | 25.1 (3.3) | 0.708 |
| Time since the lesion (years) | 5.6 (3.1) | 5.2 (2.7) | 5.1 (4.2) | 0.113 |
| Variables | Mean Values (SD) | Intra-Subject Effects † | |||
|---|---|---|---|---|---|
| Pre | Post | Post-2 (1 Month) | Time | Treatment Time | |
| F (d.f.); p-Value (eta2) | F (d.f.); p-Value (eta2) | ||||
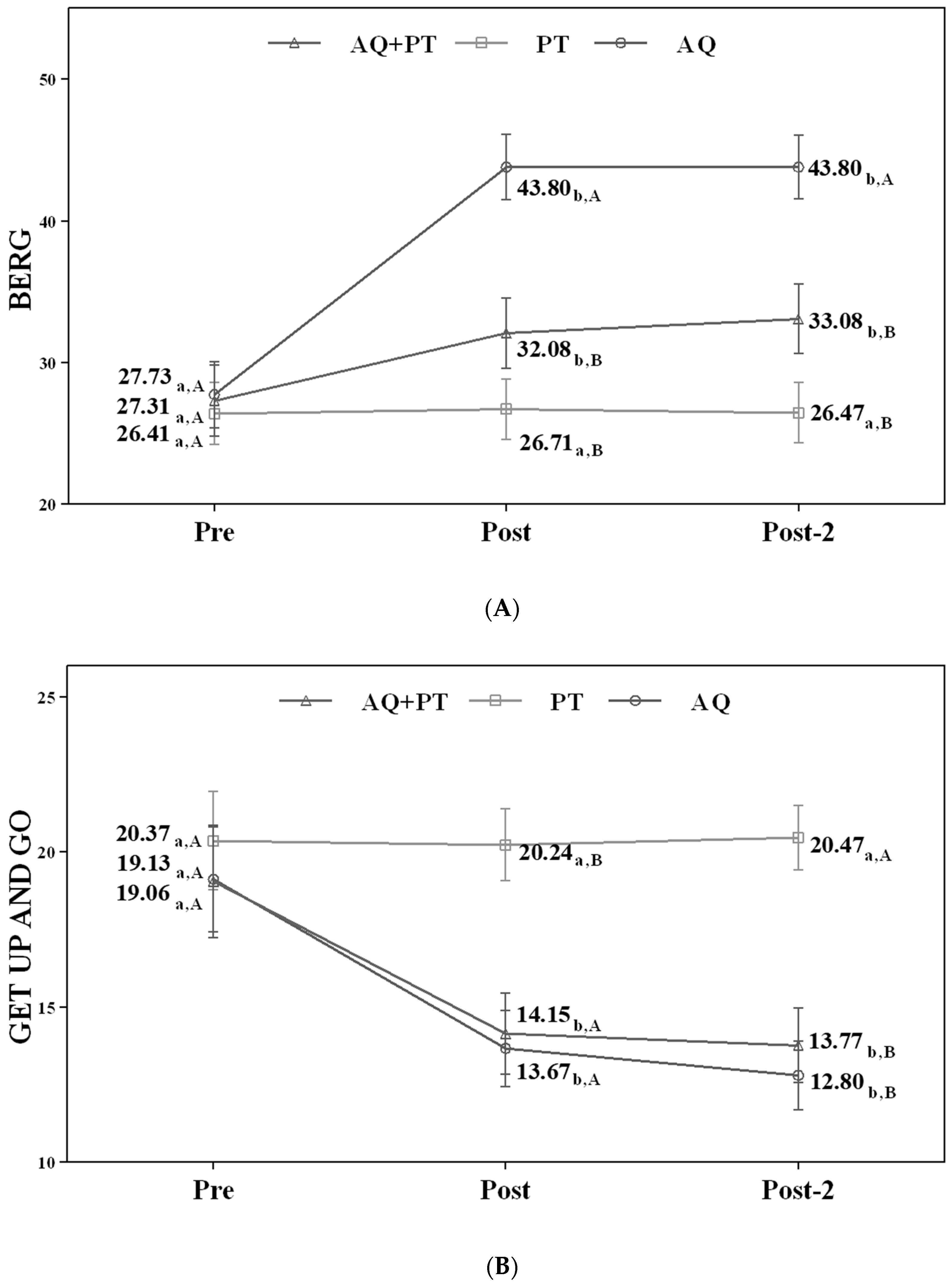
| Berg balance scale (points) | F(1.0; 43.1) = 66.42; p < 0.001 (0.613) | F(2.1; 43.1) = 30.08; p < 0.001 (0.589) | |||
| AQ + PT group (13) | 27.31 (11.7) | 32.08 (10.4) | 33.08 (10.4) | ||
| PT group (17) | 26.41 (6.5) | 26.71 (6.3) | 26.47 (6.1) | ||
| AQ group (15) | 27.73 (9.0) | 43.80 (9.9) | 43.80 (9.9) | ||
| Timed up and go test (seconds) | F(1.2; 48.4) = 47.29; p < 0.001 (0.530) | F(2.3; 48.4) = 5.91; p = 0.004 (0.219) | |||
| AQ + PT group (13) | 19.06 (5.3) | 14.15 (3.8) | 13.77 (3.8) | ||
| PT group (17) | 20.37 (6.1) | 20.24 (4.9) | 20.47 (4.9) | ||
| AQ group (15) | 19.13 (7.9) | 13.67 (5.2) | 12.80 (3.9) | ||
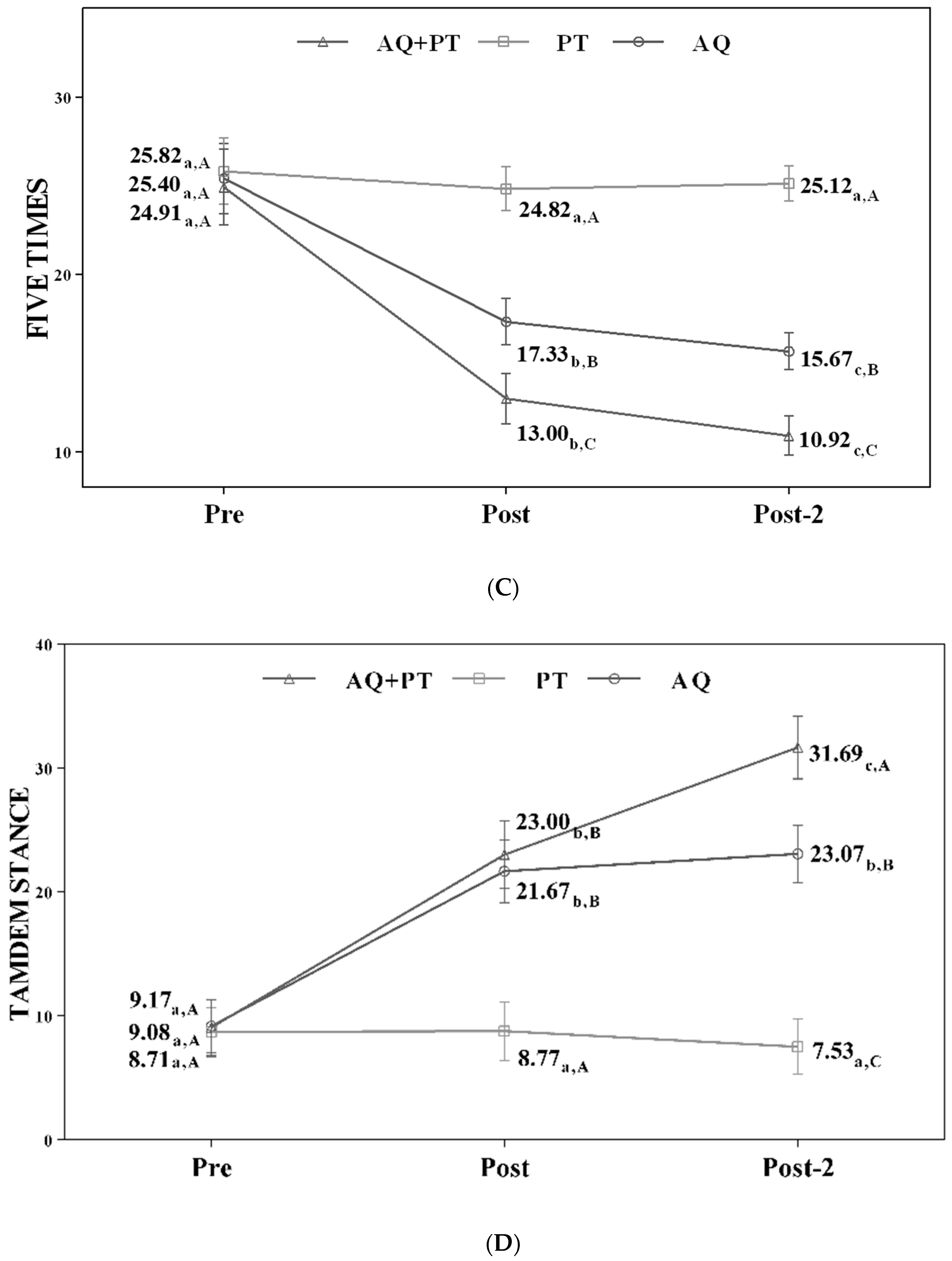
| Five times sit-to-stand (seconds) | F(1.2; 49.8) = 41.85; p < 0.001 (0.499) | F(2.4; 49.8) = 9.06; p < 0.001 (0.301) | |||
| AQ + PT group (13) | 24.91 (4.4) | 13.00 (3.8) | 11.92 (2.8) | ||
| PT group (17) | 25.82 (6.4) | 24.82 (5.5) | 25.12 (4.5) | ||
| AQ group (15) | 25.40 (10.7) | 17.33 (5.7) | 15.67 (4.3) | ||
| Tandem stance (seconds) | F(1.6; 68.4) = 93.98; p < 0.001 (0.691) | F(3.3; 68.4) = 33.79; p < 0.001 (0.617) | |||
| AQ + PT group (13) | 9.08 (8.8) | 23.00 (14.4) | 31.69 (14.3) | ||
| PT group (17) | 8.71 (6.8) | 8.77 (6.2) | 7.53 (4.4) | ||
| AQ group (15) | 9.17 (9.0) | 21.67 (7.9) | 23.07 (7.3) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-de la Cruz, S. Comparison between Three Therapeutic Options for the Treatment of Balance and Gait in Stroke: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 426. https://doi.org/10.3390/ijerph18020426
Pérez-de la Cruz S. Comparison between Three Therapeutic Options for the Treatment of Balance and Gait in Stroke: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(2):426. https://doi.org/10.3390/ijerph18020426
Chicago/Turabian StylePérez-de la Cruz, Sagrario. 2021. "Comparison between Three Therapeutic Options for the Treatment of Balance and Gait in Stroke: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 2: 426. https://doi.org/10.3390/ijerph18020426
APA StylePérez-de la Cruz, S. (2021). Comparison between Three Therapeutic Options for the Treatment of Balance and Gait in Stroke: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(2), 426. https://doi.org/10.3390/ijerph18020426





