Civil Liability of Regional Health Services: The Case of the Piedmont Region
Abstract
:1. Introduction
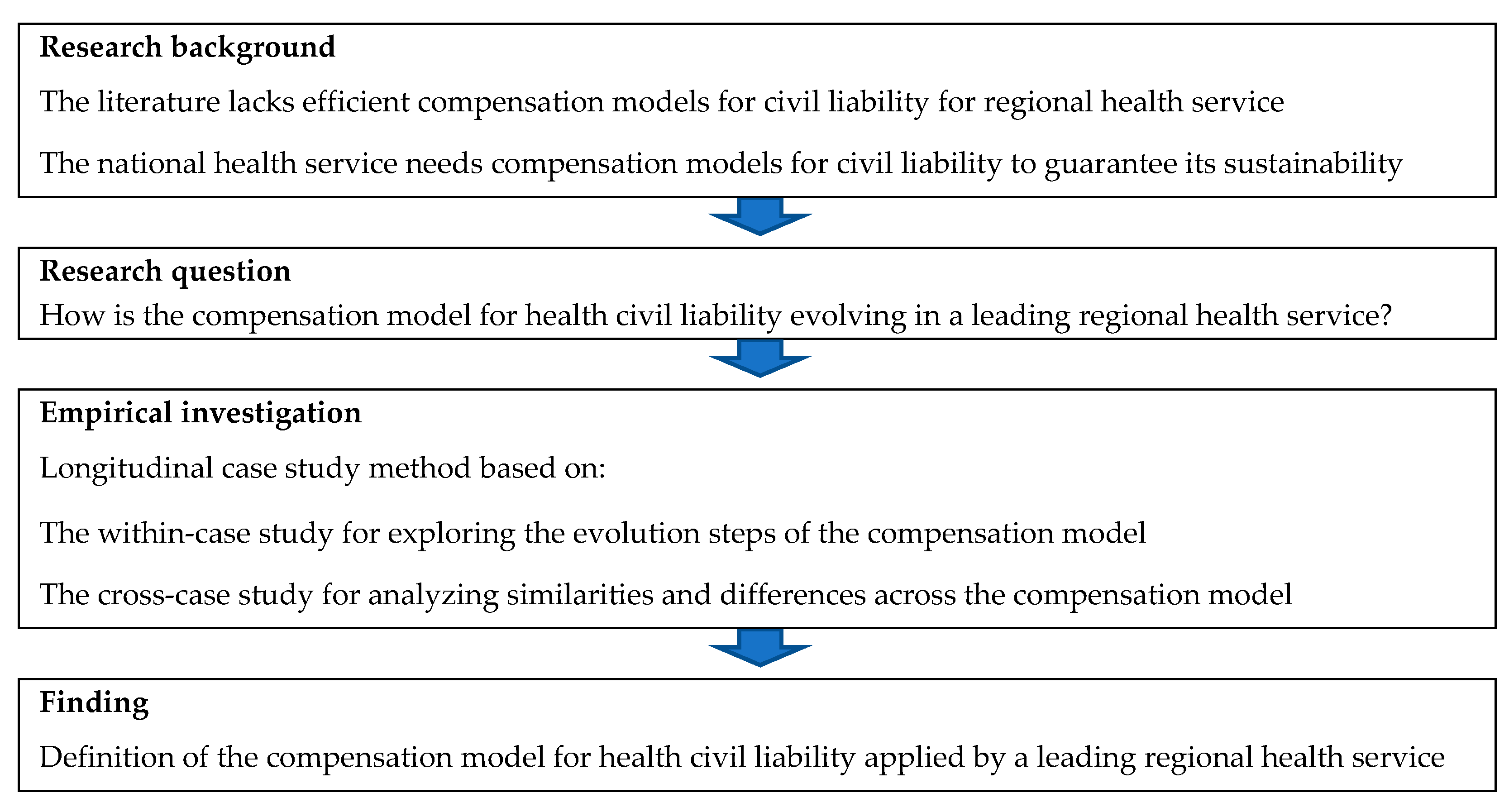
- How is the compensation model for health civil liability evolving in a leading regional health service?
2. Research Background
- ➢
- insurance model = insurance companies cover the risk and any damage
- ➢
- direct model = health authorities self-cover the risk and any damage
- ➢
- mixed-model = a mix of the two models described above.
3. Method
- Score of the Essential Levels of Assistance Grid
- % incidence of surplus/deficit on ordinary operations
- Average pre-operative hospital days
- % of operations for fracture of the femur operated within two days
- % discharged from surgical wards with medical Diagnosis Related Groups (DRGs)
- % of hospitalizations with surgical DRGs out of total hospitalizations
- % of ordinary hospitalizations with DRGs at high risk of inappropriateness
- % of diagnostic daytime hospitalizations out of total daytime hospitalizations with medical DRGs
- % of medical cases with hospitalization beyond the threshold for patients with age ≥ 65 years out of the total medical hospitalizations with age ≥ 65 years
- Deviation from the standard envisaged for the incidence of expenditure for collective assistance on the total expenditure (5%)
- Deviation from the expected standard for the incidence of district assistance expenditure on the total expenditure (51%)
- Deviation from the expected standard for the incidence of hospital care expenditure on the total expenditure (44%)
- Expenditure per capita for basic healthcare
- Expenditure per capita for drugs
- Average cost of hospitalization for acute cases in ordinary hospitalization
- Average cost for post-acute hospitalization
- Expenditure for clinical activity
- Expenditure for laboratory
- Expenditure for diagnostics.
- ✓
- ✓
- ✓
- ✓
- ✓
- ✓
- ➢
- The main National and Regional Rules to identify the main regulations of the Italian National Health Service and Piedmont Health Service
- ➢
- The main information on Piedmont Region to identify the main characteristics of Piedmont Health Service
- ➢
- The main evolution steps of the compensation model for health civil liability.
- ➢
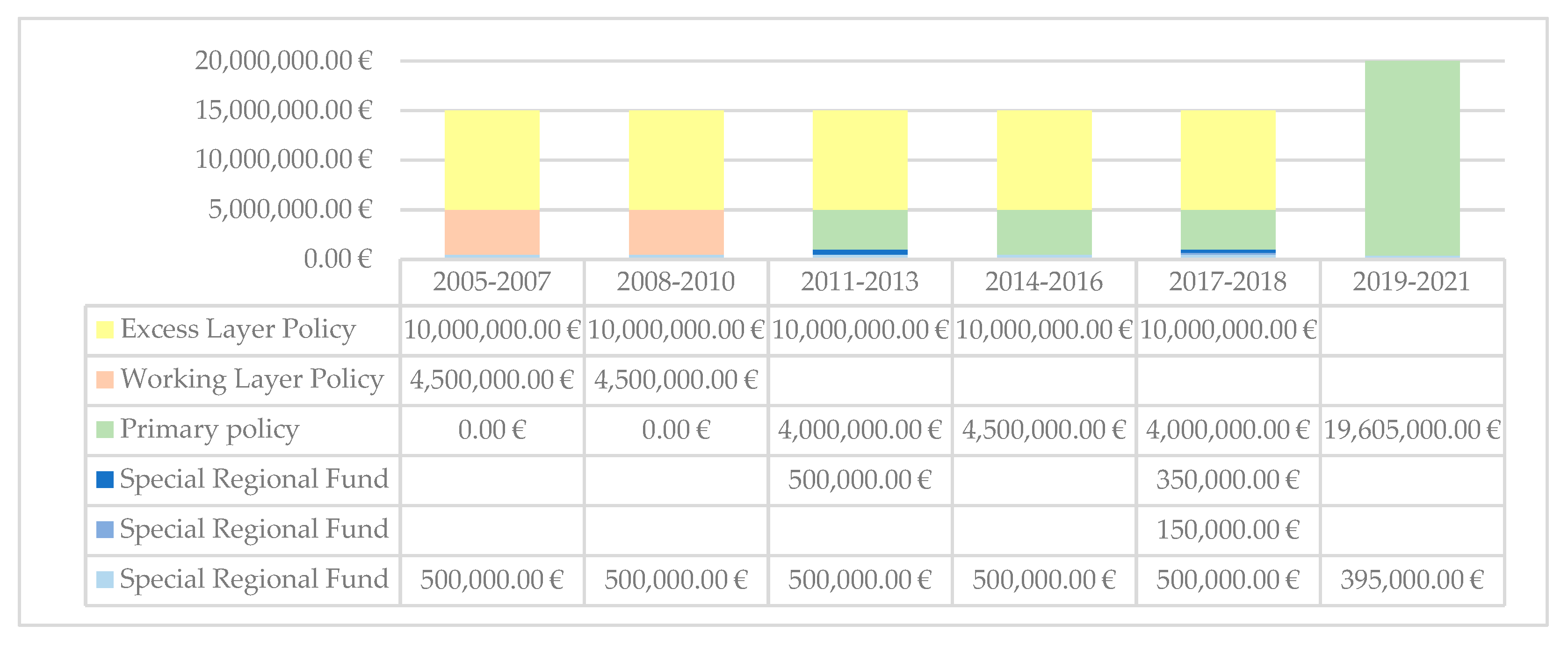
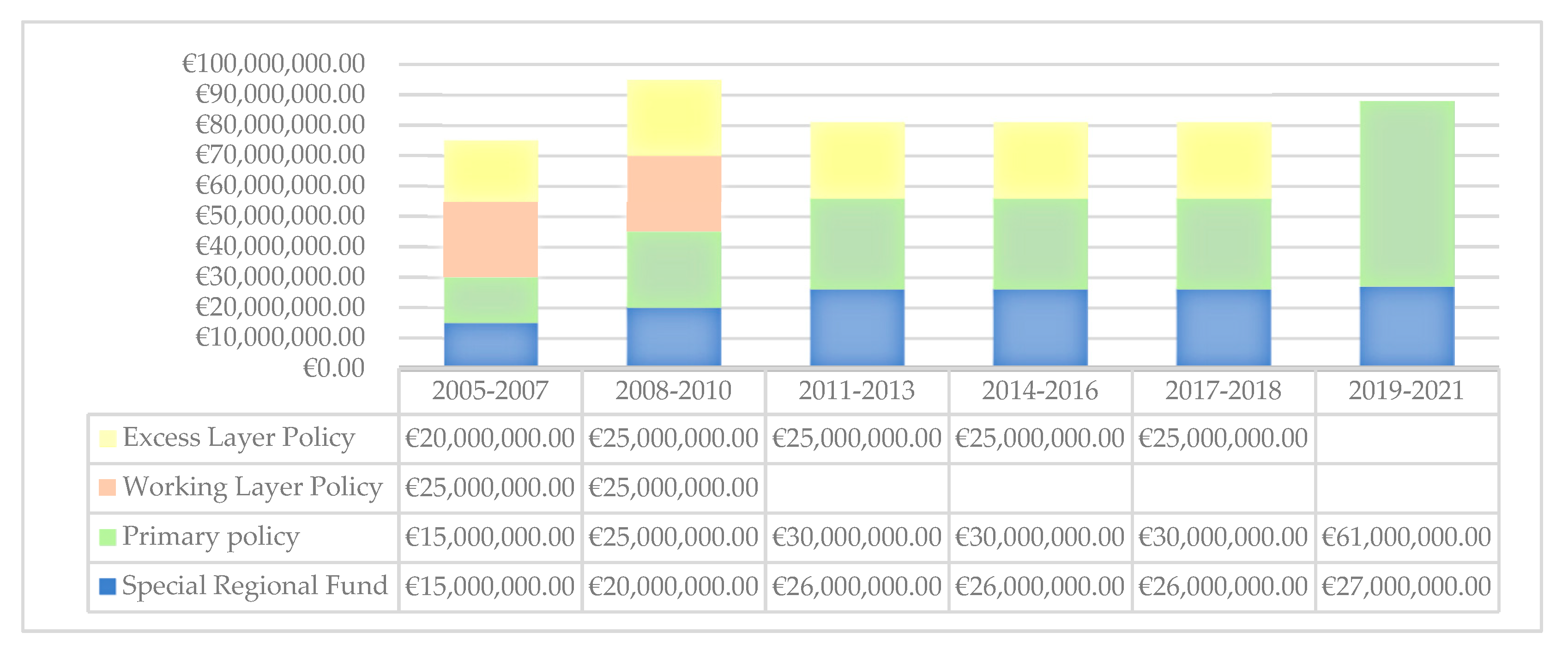
- Maximum amount and deductible for a single claim
- ➢
- Maximum amount for total claims per year
- ➢
- Paying Entity
- ➢
- Management entity of claims
- ➢
- Special regional fund.
4. Results
- Average previous claims of the Health Authorities calculated on a 10-year of the claims paid (weight 80%).
- Dimension healthcare facilities calculated based on the total salaries of healthcare personnel (weight 20%).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Sardi, A.; Sorano, E.; Guerrieri, A.; Fiandra, U. Improvement of health performance through clinical risk management: The maternal and child pathway. Meas. Bus. Excell. 2020. [Google Scholar] [CrossRef]
- Donaldson, L.; Ricciardi, W.; Sheridan, S.; Tartaglia, R. Textbook of Patient Safety and Clinical Risk Management; Springer Nature: Cham, Switzerland, 2021; ISBN 9783030594039. [Google Scholar]
- Khon, L.; Corrigan, J.; Donaldson, M. To Err is Human: Building a Safer Health System; National Academies Press (US): Washington, DC, USA, 2000; ISBN 9780309068376. [Google Scholar]
- The Institute for Healthcare Improvement Launches National Campaign to Reduce Medical Harm in U.S. Available online: http://http://www.ihi.org/about/news/Documents/IHIPressRelease_IHILaunchesCampaigntoReduceHarm_Dec06.pdf (accessed on 10 August 2021).
- Patient Safety: Global Action on Patient Safety: Report by the Director-General. Available online: https://apps.who.int/iris/handle/10665/327526 (accessed on 10 August 2021).
- The Bill & Melinda Gates Foundation Patient Safety. A grand challenge for healthcare professionals and policymakers alike. In Proceedings of the A roundtable at the Grand Challenges Meeting, Berlin, Germany, 19–21 October 2018. [Google Scholar]
- Slawomirski, L.; Auraaen, A.; Klazinga, N.S. The economics of patient safety: Strengthening a value-based approach to reducing patient harm at national level. In Proceedings of the OECD Health Working Papers, Paris, France, 26 June 2017. [Google Scholar]
- Slawomirski, L.; Auraaen, A.; Klazinga, N. The Economics of Patient Safety in Primary and Ambulatory Care: Flying Blind; OECD Health Working Papers, No. 106; OECD Publishing: Paris, France, 2018. [Google Scholar]
- Medication Without Harm-Global Patient Safety Challenge on Medication Safety. Available online: file:///C:/Users/User/Downloads/WHO-HIS-SDS-2017.6-eng.pdf (accessed on 10 August 2021).
- Borgonovi, E.; Compagni, A. Sustaining universal health coverage: The interaction of social, political, and economic sustainability. Value Health 2013, 16, 34–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sardi, A.; Sorano, E.; Agostini, L.; Guerrieri, A.; Angaramo, M.; Ripa, F. L’analisi a priori del rischio sanitario in Regione Piemonte: Applicazione del metodo Cartorisk sull’area materno-infantile. Mecosan 2020, 114, 67–88. [Google Scholar] [CrossRef]
- Bizzarri, G.; Farina, M.; Canciani, M. Strategia e Gestione del Rischio Clinico Nelle Organizzazioni Sanitarie: Approcci, Modalità, Strumenti e Risultati; Franco Angeli: Milano, Italy, 2018; ISBN 9788891760098. [Google Scholar]
- Brennan, T.A.; Leape, L.L.; Laird, N.M.; Hebert, L.; Localio, A.R.; Lawthers, A.G.; Newhouse, J.P.; Weiler, P.C.; Hiatt, H.H. Incidence of Adverse Events and Negligence in Hospitalized Patients. N. Engl. J. Med. 1991, 324, 370–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobs, J.P. Introduction--databases and the assessment of complications associated with the treatment of patients with congenital cardiac disease. Cardiol. Young 2008, 18 (Suppl. S2), 1–37. [Google Scholar] [CrossRef] [PubMed]
- AGENAS. Monitoraggio Dell’implementazione Delle Raccomandazioni per la Prevenzione Degli Eventi Sentinella. Available online: https://www.agenas.gov.it/aree-tematiche/qualita-e-sicurezza/rischio-clinico-e-sicurezza-del-paziente/monitoraggio-delle-raccomandazioni (accessed on 10 August 2021).
- Tartaglia, R.; Vannucci, A. Prevenire Gli Eventi Avversi Nella Pratica Clinica; Springer: New York, NY, USA, 2013; ISBN 978-88-470-5450-9. [Google Scholar]
- Crema, M.; Verbano, C. Identification and development of Lean and Safety projects. Saf. Sci. 2016, 89, 319–337. [Google Scholar] [CrossRef]
- Howell, A.-M.; Burns, E.M.; Hull, L.; Mayer, E.; Sevdalis, N.; Darzi, A. International recommendations for national patient safety incident reporting systems: An expert Delphi consensus-building process. BMJ Qual. Saf. 2017, 26, 150–163. [Google Scholar] [CrossRef] [PubMed]
- Grote, G. Safety management in different high-risk domains—All the same? Saf. Sci. 2012, 50, 1983–1992. [Google Scholar] [CrossRef]
- Ministero della Salute. Protocollo di Monitoraggio degli eventi sentinella 5° Rapporto. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_2353_allegato.pdf (accessed on 10 August 2021).
- Nicolini, D.; Waring, J.; Mengis, J. Policy and practice in the use of root cause analysis to investigate clinical adverse events: Mind the gap. Soc. Sci. Med. 2011, 73, 217–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peerally, M.F.; Carr, S.; Waring, J.; DIxon-Woods, M. The problem with root cause analysis. BMJ Qual. Saf. 2017, 26, 417–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, C.-H.; Chou, C.-J.; Wang, P.-C.; Lin, H.-Y.; Kao, C.-L.; Su, C.-T. Applying HFMEA to prevent chemotherapy errors. J. Med. Syst. 2012, 36, 1543–1551. [Google Scholar] [CrossRef] [PubMed]
- Intra, G.; Alteri, A.; Corti, L.; Rabellotti, E.; Papaleo, E.; Restelli, L.; Biondo, S.; Garancini, M.P.; Candiani, M.; Viganò, P. Application of failure mode and effect analysis in an assisted reproduction technology laboratory. Reprod. Biomed. Online 2016, 33, 132–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rienzi, L.; Bariani, F.; Dalla Zorza, M.; Romano, S.; Scarica, C.; Maggiulli, R.; Nanni Costa, A.; Ubaldi, F.M. Failure mode and effects analysis of witnessing protocols for ensuring traceability during IVF. Reprod. Biomed. Online 2015, 31, 516–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Comite, U.; Dong, K.; Li, R.Y.; Crabbe, M.J.C.; Shao, X.-F.; Yue, X.-G. An Economic–Business Approach to Clinical Risk Management. J. Risk Financ. Manag. 2020, 13, 135. [Google Scholar] [CrossRef]
- Ministero delle Salute. La Sicurezza dei Pazienti e la Gestione del Rischio Clinico. Glossario. Available online: https://www.asprc.it/files/asp/gestione%20rischio%20clinico/GLOSSARIO_26luglio2006.pdf (accessed on 10 August 2021).
- Dionisi, S.; Di Muzio, M.; Giannetta, N.; Di Simone, E.; Gallina, B.; Napoli, C.; Orsi, G.B. Nursing students’ experience of risk assessment, prevention and management: A systematic review. Nursing (Lond) 2021, 62, E122–E131. [Google Scholar]
- Colaianni, P.; Galanti, E.; Giusti, E.; Landini, S.; Manzato, R.; Marchi, M.; Romagnoli, G.; Tanimoto, K.; Panarelli, P. Autoassicurazione e Gestione del Rischio; Fondazione Cesifin Alberto Predieri: Milano, Italy, 2015; ISBN 9788898742035. [Google Scholar]
- Vainieri, M.; Flore, E.; Tartaglia, R.; Bellandi, T. Comparative analysis of models of the management of claims in healthcare. First empirical evidence on costs of claims. Mecosan 2014, 92, 27–53. [Google Scholar]
- Yin, R. Case Study Research: Design and Methods, 6th ed.; Sage: Los Angeles, CA, USA, 2017; ISBN 9781506336169. [Google Scholar]
- Eisenhardt, K.M.; Graebner, M.E. Theory building from cases: Opportunities and challenges. Acad. Manag. J. 2007, 50, 25–32. [Google Scholar] [CrossRef]
- Easterby-Smith, M.; Thorpe, R.; Lowe, A. Management and Business Research; Sage: London, UK, 2021; ISBN 9781529734522. [Google Scholar]
- Mills, A.; Durepos, G.; Wiebe, E. Encyclopedia of Case Study Research; Sage: London, UK, 2010. [Google Scholar]
- Mathison, S. Encyclopedia of Evaluation; Sage: London, UK, 2005. [Google Scholar]
- Garengo, P.; Biazzo, S. From ISO quality standards to an integrated management system: An implementation process in SME. Total Qual. Manag. Bus. Excell. 2013, 24, 310–335. [Google Scholar] [CrossRef]
- Sardi, A.; Sorano, E.; Ferraris, A.; Garengo, P. Evolutionary Paths of Performance Measurement and Management System: The Longitudinal Case Study of a Leading SME. Meas. Bus. Excell. 2020, 24, 495–510. [Google Scholar] [CrossRef]
- Enrichens, N. Responsabilità civile sanitaria e assicurazione. Sanità Pubblica e Priv. 2019, 1, 51–57. [Google Scholar]
| Region | Insurance Model | Direct Model | Mixed Model |
|---|---|---|---|
| Abruzzo | X | X | |
| Basilicata | X | ||
| Calabria | X | ||
| Campagna | X | X | |
| Emilia Romagna | X | ||
| Friuli Venezia Giulia | X | ||
| Lazio | X | X | X |
| Liguria | X | ||
| Lombardy | X | ||
| Marche | X | X | |
| Molise | X | ||
| Piedmont | X | ||
| Puglia | X | X | X |
| Sardinia | X | X | X |
| Sicily | X | ||
| Tuscany | X | ||
| Umbria | X | ||
| Valle d’Aosta | X | ||
| Veneto | X |
| Main Regulations | Description |
|---|---|
| Art. 32 of 1948 Constitution | Protect health as a right of the individual and a collective interest |
| Law No. 833 of 1978 | Establish the National Health Service and guaranteed health protection |
| Law No. 421 of 1992 | Reorganize the National Health Service by corporatization |
| Leg. Decree No. 229 of 1999 | Define the criteria of appropriateness, economy and scientific evidence in the choices of resources |
| DPCM No. 29 of 2001 | Define the Essential Levels of Assistance |
| Regional Law No. 9 of 2004 | Introduce the Special Regional Found for claim settlement |
| Min. Decree of 2009 | Establish Information System for Monitoring Errors in National Health Service |
| Law No. 15 of 2009 | Introduce a performance measurement system to improve the productivity of public employees |
| Leg. Decree No. 158 of 2012 | Introduce the monitoring of health risks to prevent litigation and reduce insurance charges |
| Min. Decree No. 70 of 2015 | Define the qualitative, structural, technological and quantitative standards relating to health care |
| Stability Law 2016 | Introduce the clinical risk management in the National Health Service |
| Law No. 24 of 2017 | Introduce the patient safety, the assisted person and the responsibility of healthcare operators |
| Piedmont Population 2021 | Data Population |
| Total | 4.3 million |
| Province | No. 8 * |
| Land area | 25,400 km2 |
| Density | 168/km2 |
| Regional Healthcare Service | Data regional Healthcare Service |
| Turnover | €8.5 billion approximately |
| Healthcare expenditure | €2000 per capita |
| Employees | 55,000 approximately |
| Local Health Authorities | No. 12 |
| University Hospitals | No. 3 |
| Hospitals Authorities | No. 48 |
| Healthcare beds | No. 11.472 |
| Period | Steps of the Mixed Model Development |
|---|---|
| 1990–2004 | Piedmont Health Service adopted an insurance model |
| 1990–2004 | Patients increased the compensation claims and the insurance companies paid more settlements |
| 1990–2004 | Insurance companies increased premiums and reduced guarantees |
| 2000–2002 | Piedmont installed defective heart valves; this event caused an increase in compensation claims |
| 2005–today | Piedmont adopted a mixed model; it included the creation of a Special regional fund |
| 2005–today | Special regional fund increased steadily |
| 2009–2015 | Calls of patients damaged for judgment had increased steadily |
| 2010–2019 | Piedmont Health Service increased the number of claims managed |
| Period | Max for Claim—Deductible for Claim | Max Claims/Year | Paying Entity | Management Entity |
|---|---|---|---|---|
| 2005–2007 | Up to €1500 | Unlimited | Health Authority | Health Authority |
| Up to €500,000—deductible €1500 | €15 million * | Piedmont Health Service | Loss Adjuster | |
| Up to €500,000—deductible €1500 if Special regional fund is exhausted | €15 million | Insurance Company by Policy, namely Primary Policy | Insurance Company | |
| Up to €5 million—deductible €500,000 only for claims > € 500,000 | €25 million | Insurance Company by Policy, namely Working Layer Policy | Insurance Company | |
| Up to €15 million—deductible €5 million only for catastrophic damage | €20 million | Insurance Company by Policy, namely Excess Layer Policy | Insurance Company | |
| 2008–2010 | Up to €1500 | Unlimited | Health Authority | Health Authority |
| Up to €500,000—deductible €1500 | €20 million * | Piedmont Health Service | Loss Adjuster Claim Committee | |
| Up to €500,000—deductible €1500 if Special regional fund is exhausted | €25 million | Insurance Company by Policy, namely Primary Policy | Insurance Company | |
| Up to €5 million—deductible €500,000 only for claims > €500,000 | €25 million | Insurance Company by Policy, namely Working Layer Policy | Insurance Company | |
| Up to €15 million—deductible €5 million only for catastrophic damage | €25 million | Insurance Company by Policy, namely Excess Layer Policy | Insurance Company | |
| 2011–2013 | Up to €5000 | Unlimited | Health Authority | Health Authority |
| Up to €1 million—deductible €5000 for childbirth and sentinel events claims Up to €500,000—deductible €5000 for different claims | €26 million * | Piedmont Health Service | Loss Adjuster Claim Committee | |
| Up to €5 million—deductible €1 million for childbirth and sentinel events claims Up to €5 million—deductible €500,000 for different claims | €30 million | Insurance Company by Policy, namely Primary Policy | Insurance Company | |
| Up to €15 million—deductible €5 million only for catastrophic damage | €25 million | Insurance Company by Policy, namely Excess Layer Policy | Insurance Company | |
| 2014–2016 | Up to €5000 | Unlimited | Health Authority | Health Authority |
| Up to €1 million—deductible €5000 for childbirth and sentinel events claims Up to €500,000—deductible €5000 for different claims | €26 million * | Piedmont Health Service | Loss Adjuster until 30 June 2016 | |
| Up to €5 million—deductible €1 million for childbirth and sentinel events claimUp to €5 million—deductible €500,000 € for different claims | €30 million | Insurance Company by Policy, namely Primary Policy | Insurance Company | |
| Up to €15 million—deductible €5 million only for catastrophic damage | €25 million | Insurance Company by Policy, namely Excess Layer Policy | Insurance Company | |
| 2017–2018 | Up to €5000 | Unlimited | Health Authority | Health Authority |
| Up to €1 million—deductible €5000 for childbirth and sentinel events claims Up to €650,000—deductible €5000 for death claimsUp to €500,000—deductible €5000 for difference claims | €26 million * | Piedmont Health Service | Claim Committee Insurance Company | |
| Up to €5 million—deductible €1 million for childbirth and sentinel events claims Up to €5 million—deductible €650,000 for death claims Up to €5 million—deductible €500,000 for difference claims | €30 million | Insurance Company by Policy, namely Primary Policy | Claim Committee Insurance Company Health Authority | |
| €15 million deductible €5 million only for catastrophic damage | €25 million | Insurance Company by Policy, namely Excess Layer Policy | Insurance Company | |
| 2019–2021 | Up to €5000 | Unlimited | Health Authority | Health Authority |
| Up to €395,000 deductible €5000 and SIR of 39% up to €500,000 | €27 million * | Piedmont Health Service | Claim Committee Insurance Company | |
| Up to €20 million—deductible SIR of 39% up to €500,000 | €61 million | Insurance Company by Policy, namely Primary Policy | Claim Committee Insurance Company Health Authority |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rizzi, A.; Sorano, E.; Cerrato, S.A.; Riganti, F.; Stiari, A.; Macrì, E.; Sardi, A. Civil Liability of Regional Health Services: The Case of the Piedmont Region. Int. J. Environ. Res. Public Health 2021, 18, 9954. https://doi.org/10.3390/ijerph18199954
Rizzi A, Sorano E, Cerrato SA, Riganti F, Stiari A, Macrì E, Sardi A. Civil Liability of Regional Health Services: The Case of the Piedmont Region. International Journal of Environmental Research and Public Health. 2021; 18(19):9954. https://doi.org/10.3390/ijerph18199954
Chicago/Turabian StyleRizzi, Alessandro, Enrico Sorano, Stefano A. Cerrato, Federico Riganti, Alessandro Stiari, Ernesto Macrì, and Alberto Sardi. 2021. "Civil Liability of Regional Health Services: The Case of the Piedmont Region" International Journal of Environmental Research and Public Health 18, no. 19: 9954. https://doi.org/10.3390/ijerph18199954
APA StyleRizzi, A., Sorano, E., Cerrato, S. A., Riganti, F., Stiari, A., Macrì, E., & Sardi, A. (2021). Civil Liability of Regional Health Services: The Case of the Piedmont Region. International Journal of Environmental Research and Public Health, 18(19), 9954. https://doi.org/10.3390/ijerph18199954








