A Realist Inquiry to Identify the Contribution of Lean Six Sigma to Person-Centred Care and Cultures
Abstract
:1. Introduction
1.1. Background
1.1.1. Lean Six Sigma
1.1.2. Person Centredness
1.1.3. The Problem
1.1.4. Study Aim
2. Materials and Methods
2.1. Study Design
2.1.1. Study Setting
2.1.2. Study Design
2.1.3. Reference Group
2.1.4. Initial Programme Theory Development
2.1.5. Realist Review
- Key search terms used in combination for the first strand were: ‘Lean’, ‘Six Sigma’, ‘Lean Six Sigma’, ‘process improvement’, ‘quality improvement’, and ‘healthcare’.
- The second strand search utilised the key words ‘person-centred’, ‘person-centredness’, ‘person-centred cultures’, ‘patient-centred’, and ‘patient-centredness’.
- The third strand of the search utilised a combination of the keywords from strands one and two to fully address the research questions.
- Work published relating to LSS in healthcare in the English language between 2000 and 2017, the rationale for this being that LSS was first introduced into healthcare settings early in the decade.
- Work relating to LSS that discusses the concept of patient-centred care but also references person-centred care or person-centred cultures.
- Work relating to person-centred care and person-centred cultures from 1995 to 2017, the rationale being that this was a period of ‘strong academic momentum and practice emergence’ [50].
- Work meeting criteria 1–3 that was peer-reviewed and available as full-text journal articles with a complete bibliography.
- The outcomes for the CMOc relating to patients were dependent on the CMOc relating to staff, in that staff proficiency and knowledge of LSS are mechanisms for patient outcomes.
- The CMOc relating to organisational influences addressed organisational support; however, the CMOc relating to staff addressed where and how staff worked with LSS in their everyday practice. To truly capture the staff voice, the logical choice for further research was the CMOc that related to them.
- Much of the literature talked about organisational gains in relation to Key Performance Indicators (KPIs) but little referred to how staff felt about their interactions with LSS. As this study was based on the concept of person-centred cultures, there was a need to focus this research on staff as a key component of the impact of LSS.
- There was a large population of staff who were trained in, led and worked on LSS initiatives within the study site, and who were willing to participate in the study.
2.1.6. Realist Evaluation
- A series of facilitated workshops with study participants (n = 20) to adjudicate the CMOc, relating to staff. The person-centred principles of Collaborative, Inclusive, and Participative (CIP) ways of working [51,52] underpinned the approach to these workshops to gather participants’ views and experiences as LSS practitioners. A range of creative approaches were used to achieve these collaborative and inclusive ways of working including the use of pictures and creative constructs [53] and other means, such as the use of painting and collage [54,55]. These approaches facilitated participant feedback and adjudication of the programme theory, adjudication being the interrogation of underlying causal processes [40], and further facilitated thematic analysis. The ultimate purpose of data analysis through adjudication is related to theory development and refinement of the programme theory [56].
- Individual interviews with workshop participants (n = 20) to further explore the themes that were developed in their first workshop and to refine the initial programme theory through individual adjudication of the CMOc. These were semi-structured realist interviews [57].
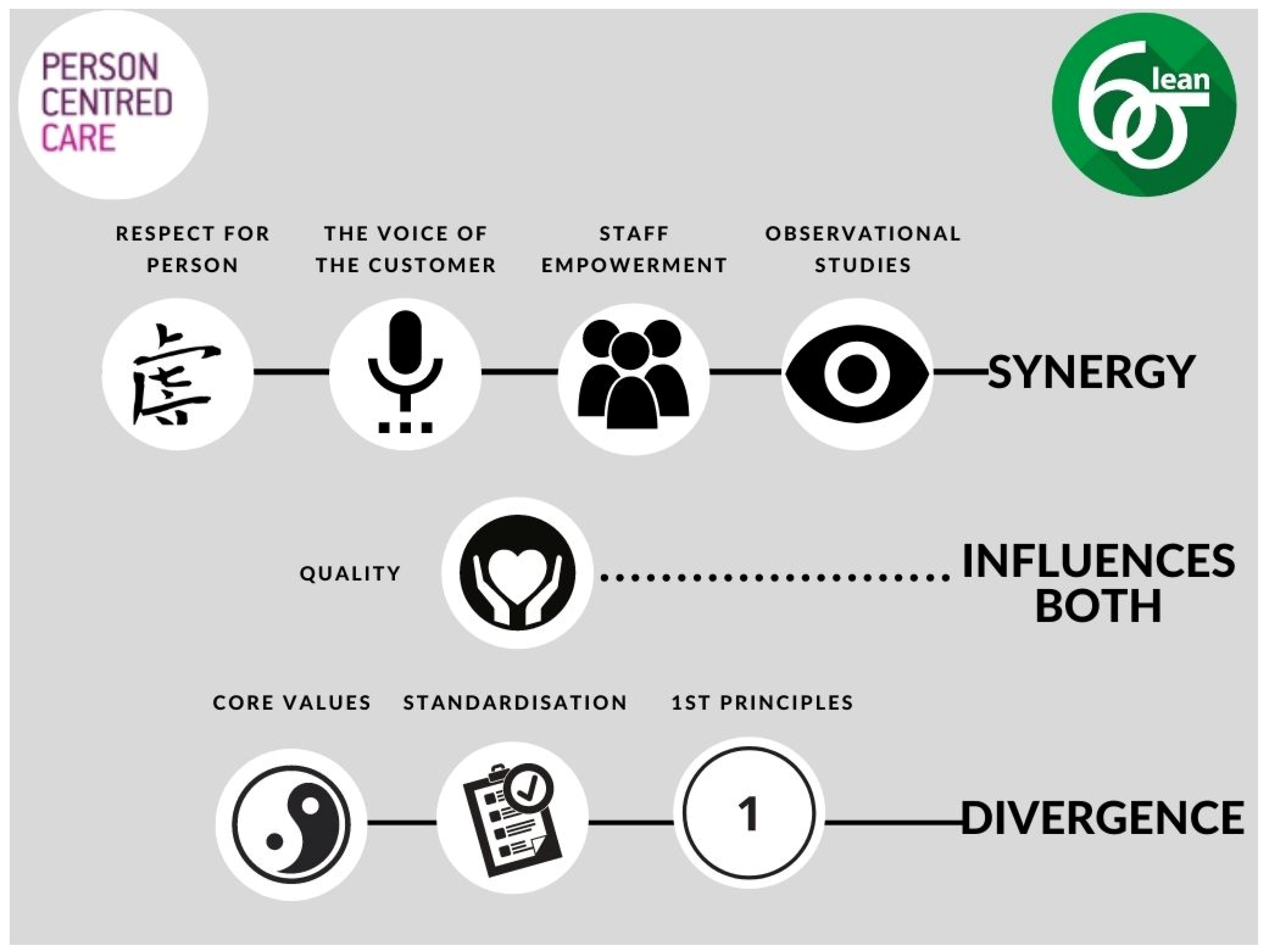
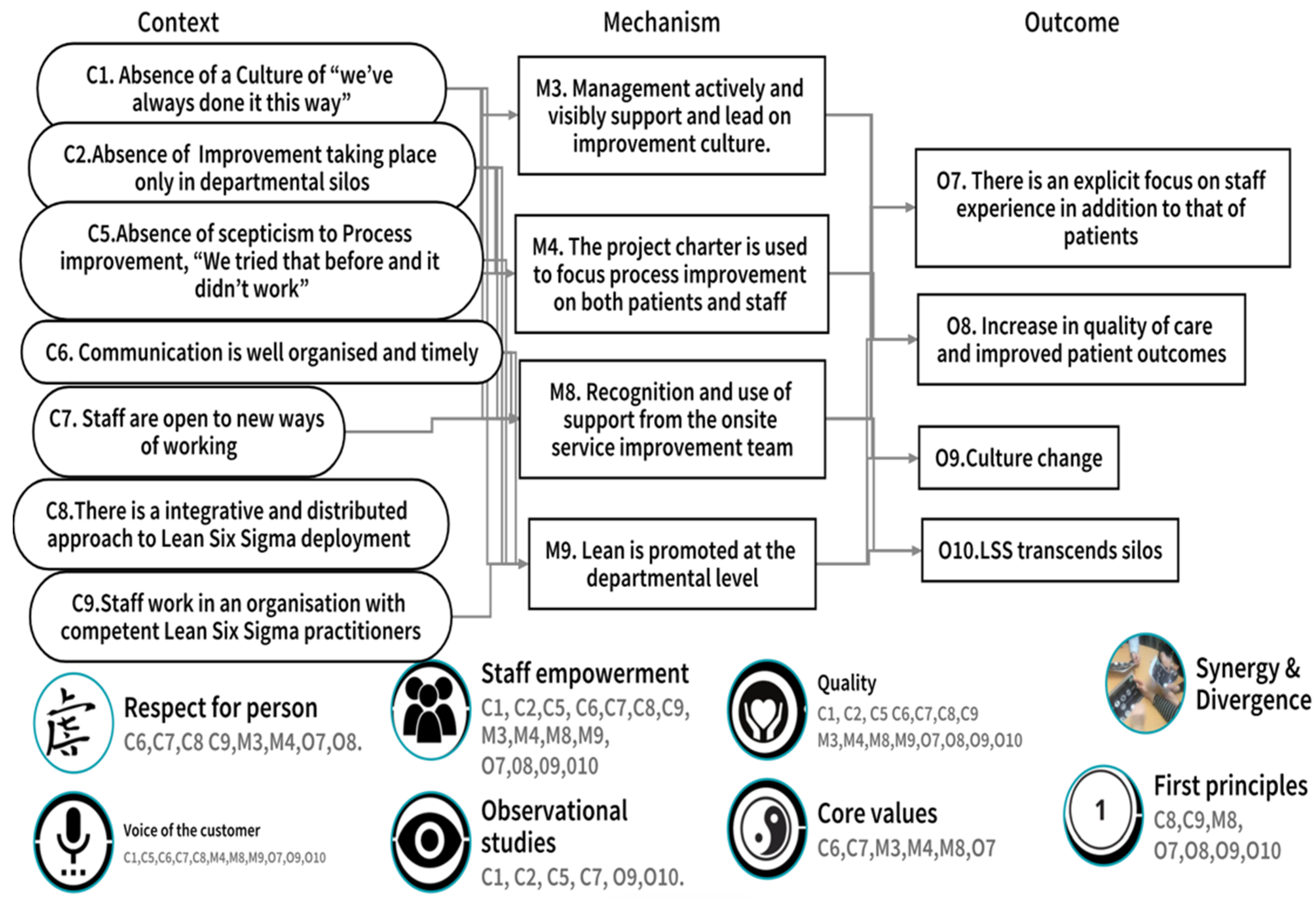
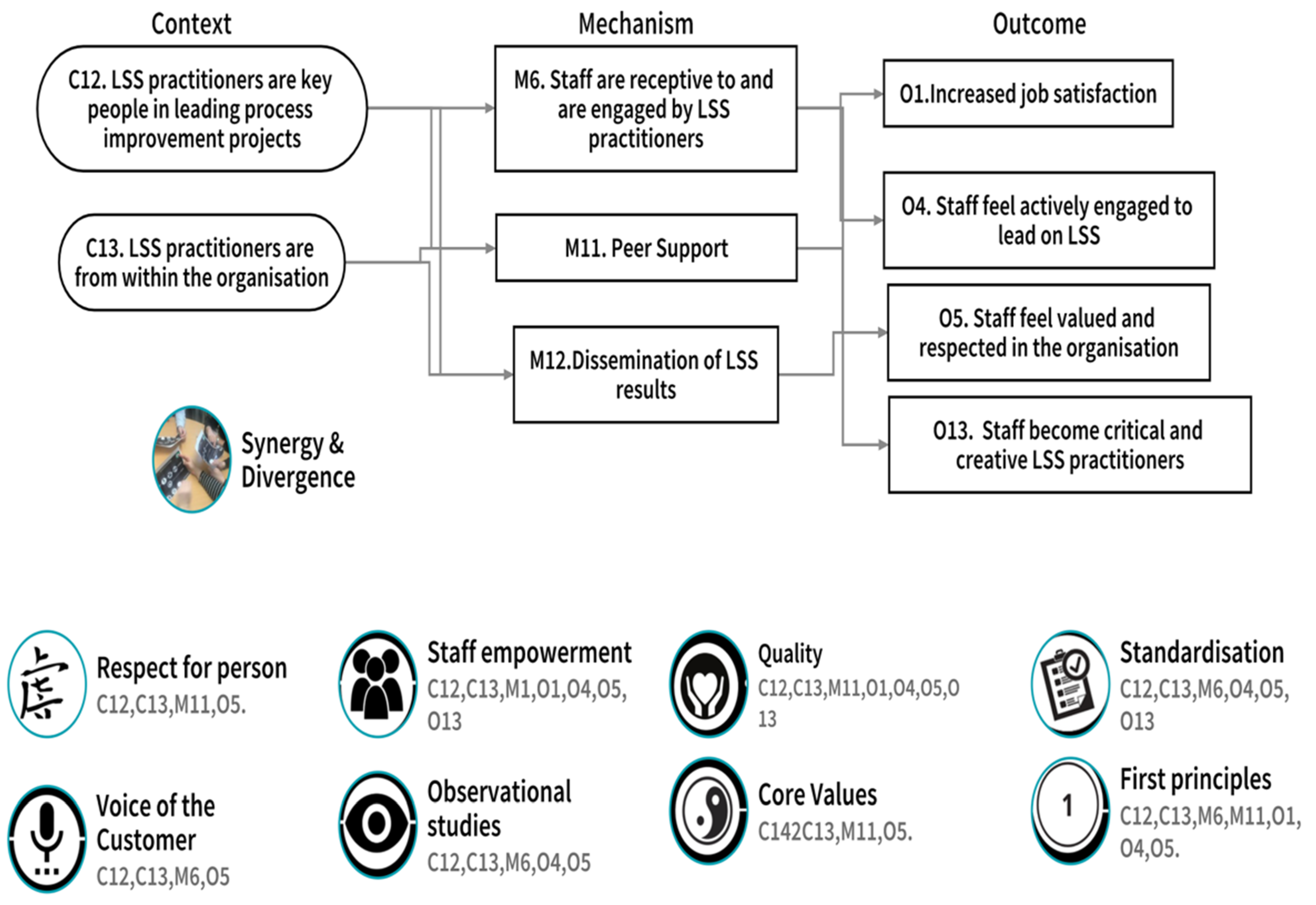
- A second series of facilitated workshops with study participants to arrive at a final adjudication of the CMOc as refined in workshop one and further refined in the individual interviews. Participants worked with the researchers to consider the data from the realist review, from LSS poster presentations and from their own workshop and individual interviews and to use that information to adjudicate the existing CMOc. Finally, participants located the adjudicated CMOc within the synergies and divergences identified between LSS, person-centred care, and person-centred cultures located in a previous review of the literature by the authors of this study [18]. These synergy and divergences are represented in Figure 3.
- The results of study participants’ LSS projects, already in the public domain, provided supporting evidence for the outcomes of their LSS work in their area of practice and provided evidence of improved patient and staff experiences, and patient outcomes. Results reviewed were represented in scientific poster presentations and peer-reviewed publications.
2.1.7. Study Participants
- Graduate of the LSS education and training programme (2014–2017).
- Current member of staff within the study site.
- Graduates of the LSS education and training programme (2014–2017) who no longer worked in the hospital (as their LSS practice did not relate to the study site).
- Non-study site staff who undertook the programme.
- Graduates currently involved in another research project (so as not to detract from their work on that project or place additional demands on their time).
3. Results
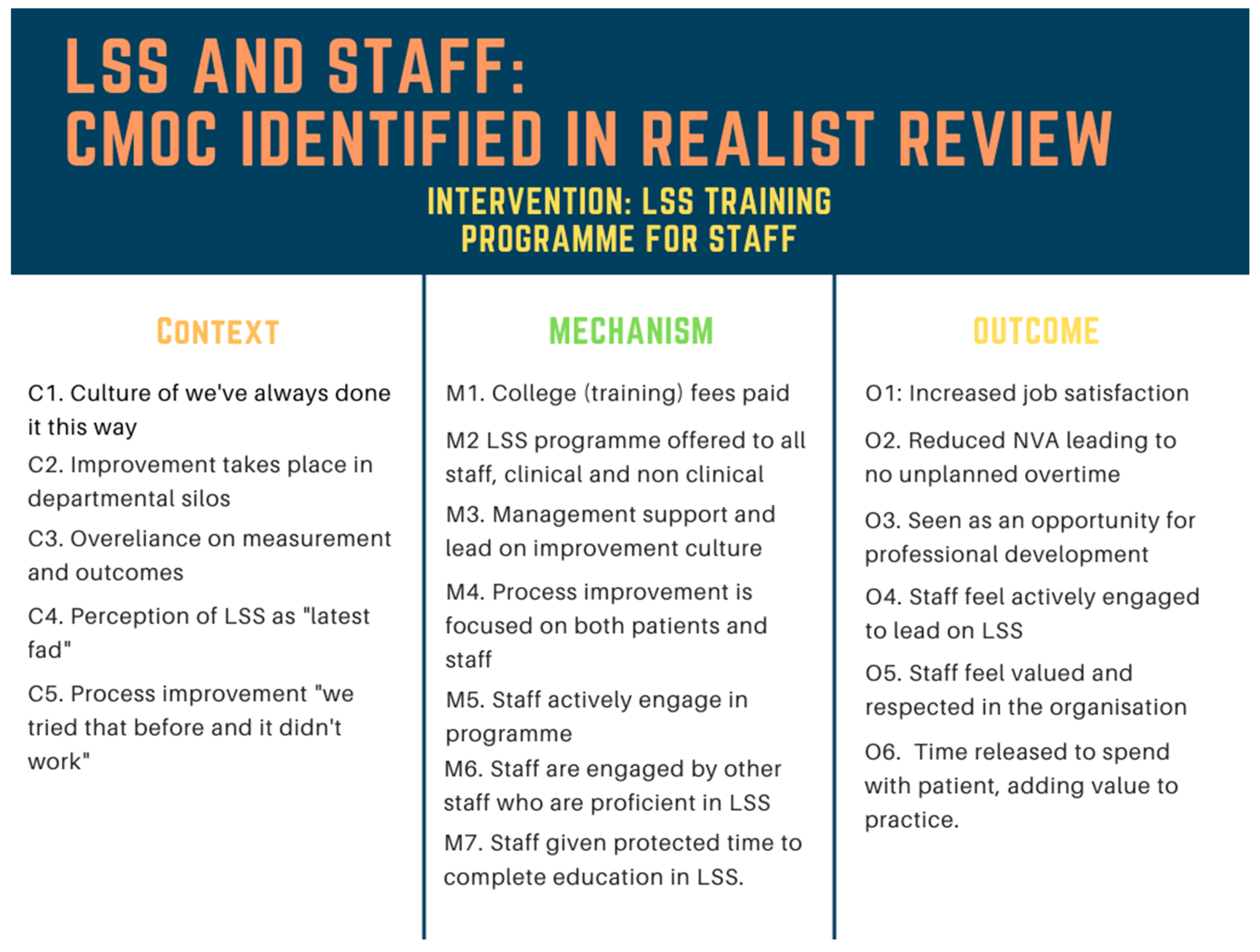
3.1. Results of the Realist Review
3.2. Results of the Realist Evaluation
- CMOc 1. LSS and aspects of organisational culture;
- CMOc 2. The organisation’s receptivity to LSS;
- CMOc 3. Participants’ self-perception as LSS practitioners.
3.2.1. CMOc 1. LSS and Aspects of Organisational Culture
3.2.2. CMOc 2. The Organisation’s Receptivity to LSS
3.2.3. CMOc 3. Participants’ Self-Perception as LSS Practitioners
4. Discussion
- Contextual factors (C) that facilitated or hindered their LSS practice work.
- The outcomes (O) that emerged because of the action of underlying mechanisms (M), which they identified that were active when the contextual factors (C) were present.
- The synergies, influencers, and divergences between their LSS practice and person-centred care and cultures.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abu Bakar, F.A.; Subari, K.; Daril, M.A.M. Critical success factors of Lean Six Sigma deployment: A current review. Int. J. Lean Six Sigma 2015, 6, 339–348. [Google Scholar] [CrossRef]
- Zidel, T.G. A Lean Guide to Transforming Healthcare: How to Implement Lean Principles in Hospitals, Medical Offices, Clinics and Other Healthcare Organisations; American Society for Quality, Quality Press: Milwaukee, WI, USA, 2006. [Google Scholar]
- Aherne, J.; Whelton, J. Applying Lean in Healthcare: A Collection of International Case Studies; Productivity Press: New York, NY, USA, 2010. [Google Scholar]
- Pande, P.S.; Neuman, R.P.; Cavanagh, R.R. The Six Sigma Way Team Fieldbook: An Implementation Guide for Process Improvement; McGraw-Hill: New York, NY, USA, 2002. [Google Scholar]
- Rath, S. Six Sigma Pocket Guide; McGraw-Hill: New York, NY, USA, 2002. [Google Scholar]
- George, M.L.; Rowlands, D.; Price, M.; Maxey, J. The Lean Six Sigma Pocket Toolbook; McGraw-Hill: New York, NY, USA, 2005. [Google Scholar]
- Vijaya Sunder, M. Synergies of lean six Sigma the IUP. J. Oper. Manag. 2013, 12, 21–31. [Google Scholar]
- Taner, M.T.; Sezen, B.; Antony, J. An overview of six sigma applications in healthcare industry. Int. J. Health Care Qual. Assur. 2007, 20, 329–340. [Google Scholar] [CrossRef]
- Graban, M. Lean Hospitals Improving Quality, Patient Safety, and Employee Engagement, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Fillingham, D. Can lean save lives? Leadersh. Health Serv. 2007, 20, 231–241. [Google Scholar] [CrossRef] [Green Version]
- BRANDAO, D.S.L. Trends and approaches in lean healthcare. Leadersh. Health Serv. 2009, 22, 121–139. [Google Scholar] [CrossRef]
- Mazzocato, P.; Stenfors, T.; Schwarz, U.V.T.; Hasson, H.; Nyström, M.E. Kaizen practice in healthcare: A qualitative analysis of hospital employees’ suggestions for improvement. BMJ Open 2016, 6, e012256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burgess, N.; Radnor, Z. Evaluating Lean in healthcare. Int. J. Health Care Qual. Assur. 2013, 26, 220–235. [Google Scholar] [CrossRef]
- Aboelmaged, M. Six Sigma quality: A structured review and implications for future research. Int. J. Qual. Reliab. Manag. 2010, 27, 268–317. [Google Scholar] [CrossRef]
- Radnor, Z.; Osborne, S.P. Lean: A failed theory for public services? Public Manag. Rev. 2013, 15, 265–287. [Google Scholar] [CrossRef]
- Williams, S. Lean and Person-Centred Care: Are They at Odds? Available online: http://www.pomsmeetings.org/ConfProceedings/051/FullPapers/Final%20Full%20length%20Papers/051-0066.pdf (accessed on 27 November 2015).
- Jorma, T.; Tiirinki, H.; Bloigu, R.; Turkki, L. LEAN thinking in Finnish healthcare. Leadersh. Health Serv. 2016, 29, 9–36. [Google Scholar] [CrossRef] [PubMed]
- Teeling, S.P.; Dewing, J.; Baldie, D. A discussion of the synergy and divergence between lean six sigma and person-centred improvement sciences. Int. J. Res. Nurs. 2020, 11, 10–23. [Google Scholar] [CrossRef] [Green Version]
- Bartz, C.C. International Council of Nurses and person-centered care. Int. J. Integr. Care 2010, 10, e010. [Google Scholar] [CrossRef] [PubMed]
- Toro, N. Who global strategy on integrated people-centred health services (IPCHS)/Estrategia mundial en servicios de salud integrada centrado en las personas (IPCHS). Int. J. Integr. Care 2015, 15. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Framework on Integrated, People-Centred Health Services; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Van Weel, C. Person-centred medicine in the context of primary care: A view from the World Organization of Family Doctors (Wonca). J. Eval. Clin. Pract. 2011, 17, 337–338. [Google Scholar] [CrossRef]
- Nolte, E. Implementing person centred approaches. BMJ 2017, 358, j4126. [Google Scholar] [CrossRef] [PubMed]
- Hardiman, M.; Dewing, J. Using two models of workplace facilitation to create conditions for development of a person-centred culture: A participatory action research study. J. Clin. Nurs. 2019, 28, 2769–2781. [Google Scholar] [CrossRef]
- McCormack, B.; McCance, T.; Klopper, H. Person-Centred Practice in Nursing and Health Care: Theory and Practice, 2nd ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2017. [Google Scholar]
- McCormack, B.; Borg, M.; Cardiff, S.; Dewing, J.; Jacobs, G.; Janes, N.; Karlsson, B.; McCance, T.; Mekki, T.E.; Porock, D.; et al. “Person-centredness—The ‘State’ of the Art. Int. Pract. Dev. J. 2015, 5, 1–15. [Google Scholar] [CrossRef]
- McCormack, B.; McCance, T. Development of a framework for person-centred nursing. J. Adv. Nurs. 2006, 56, 472–479. [Google Scholar] [CrossRef]
- McCormack, B.; McCance, T. Person-Centred Nursing Theory and Practice; Wiley-Blackwell: Hoboken, NJ, USA, 2010. [Google Scholar]
- McCormack, B. Person-Centredness and Person-Centred Practice Masterclass on Person Centred Cultures; Health Service Executive: Dublin, Ireland, 2017. [Google Scholar]
- McCormack, B.; Dewing, J.; Breslin, L.; Coyne-Nevin, A.; Kennedy, K.; Manning, M.; Peelo-Kilroe, L.; Tobin, C.; Slater, P. Developing person-centred practice: Nursing outcomes arising from changes to the care environment in residential settings for older people. Int. J. Older People Nurs. 2010, 5, 93–107. [Google Scholar] [CrossRef]
- Dixon-Woods, M. How to improve healthcare improvement—An essay by Mary Dixon-Woods. BMJ 2019, 367, l5514. [Google Scholar] [CrossRef] [Green Version]
- McNamara, M.; Teeling, S.P. Developing a university-accredited lean six sigma curriculum to overcome system blindness. Int. J. Qual. Health Care 2019, 31, 3–5. [Google Scholar] [CrossRef] [Green Version]
- Pawson, R. Evidence-Based Policy A Realist Perspective; SAGE: London, UK, 2006. [Google Scholar]
- Pawson, R.; Greenhalgh, T.; Harvey, G.; Walshe, K. Realist review—A new method of systematic review designed for complex policy interventions. J. Health Serv. Res. Policy 2005, 10, 21–34. [Google Scholar] [CrossRef]
- Pawson, R.; Tilley, N. Realistic Evaluation; SAGE: London, UK, 1997. [Google Scholar]
- Pawson, R.; Tilley, N. Realistic evaluation bloodlines. Am. J. Eval. 2001, 22, 317–324. [Google Scholar] [CrossRef]
- Pawson, R. Middle-range realism. Arch. Eur. Sociol. 2000, 41, 283–325. [Google Scholar] [CrossRef]
- Pawson, R. Evidence-based policy: The promise of ‘Realist Synthesis’. Evaluation 2002, 8, 340–358. [Google Scholar] [CrossRef] [Green Version]
- Pawson, R. How ‘Bad’ Research Can Yield ‘Good’ Evidence. Int. J. Soc. Res. Methodol. 2006, 9, 127–142. [Google Scholar] [CrossRef]
- Pawson, R. The Science of Evaluation: A Realist Manifesto; Sage: London, UK, 2013. [Google Scholar]
- Tilley, N. Applying theory-driven evaluation to the British crime reduction programme: The theories of the programme and of its evaluations. Crim. Justice 2004, 4, 255–276. [Google Scholar] [CrossRef]
- Tilley, C. Explaining Social Processes, 1st ed.; Taylor & Francis: London, UK, 2008. [Google Scholar]
- Manzano-Santaella, A. A realistic evaluation of fines for hospital discharges: Incorporating the history of programme evaluations in the analysis. Evaluation 2011, 17, 21–36. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Macfarlane, F.; Barton-Sweeney, C.; Woodard, F. “If we build it, will it stay?” A case study of the sustainability of whole-system change in London. Milbank Q. 2012, 90, 516–547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazzocato, P.; Holden, R.J.; Brommels, M.; Aronsson, H.; Bäckman, U.; Elg, M.; Thor, J. How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children’s hospital, Stockholm, Sweden. BMC Health Serv. Res. 2012, 12, 28. [Google Scholar] [CrossRef] [Green Version]
- Mazzocato, P.; Thor, J.; Bäckman, U.; Brommels, M.; Carlsson, J.; Jonsson, F.; Hagmar, M.; Savage, C. Complexity complicates lean: Lessons from seven emergency services. J. Health Organ. Manag. 2014, 28, 266–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Buckingham, J.; Pawson, R. RAMESES publication standards. BMC Med. 2013, 11, 20. [Google Scholar] [CrossRef] [Green Version]
- Birckmayer, J.D.; Weiss, C.H. Theory-based evaluation in practice. What do we learn? Eval. Rev. 2000, 24, 407–431. Available online: http://erx.sagepub.com/content/24/4/407.short (accessed on 18 February 2016). [CrossRef] [PubMed]
- Wong, G.; Westhorp, G.; Greenhalgh, J.; Manzano, A.; Jagosh, J.; Greenhalgh, T. Quality and reporting standards, resources, training materials and information for realist evaluation: The RAMESES II project. Health Serv. Deliv. Res. 2017, 5, 1–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edvardsson, D.; Fetherstonhaugh, D.; Nay, R. Promoting a continuation of self and normality: Person-centred care as described by people with dementia, their family members and aged care staff. J. Clin. Nurs. 2010, 19, 2611–2618. [Google Scholar] [CrossRef] [PubMed]
- Manley, K.; O’Keefe, H.; Jackson, C.; Pearce, J.; Smith, S. A shared purpose framework to deliver person-centred, safe and effective care: Organisational transformation using practice development methodology. Int. Pract. Dev. J. 2014, 4, 1–31. [Google Scholar] [CrossRef]
- Dewing, J.; McCormack, B.; Titchen, A. Developing a Shared Vision for Person-Centred Care. In Practice Development for Nursing, Health and Social Care Teams; John Wiley & Sons Ltd.: Chichester, UK, 2015. [Google Scholar]
- Coats, E.; Dewing, J.; Titchen, A. Opening Doors on Creativity: Resources to Awaken Creative Working; Royal College of Nursing: London, UK, 2006. [Google Scholar]
- McCormack, B.; Dewar, B.; Wright, J.; Garbett, R.; Harvey, G.; Ballantine, K. A Realist Synthesis of Evidence Relating to Practice Development; National Health Service Scotland: Edinburgh, UK, 2006. [Google Scholar]
- Foster, V. The art of empathy: Employing the arts in social inquiry with poor, working class women. Soc. Justice 2007, 34, 12–27. [Google Scholar]
- Rycroft-Malone, J.; McCormack, B.; Hutchinson, A.M.; DeCorby, K.; Bucknall, T.K.; Kent, B.; Schultz, A.; Snelgrove-Clarke, E.; Stetler, C.B.; Wilson, V.; et al. Realist synthesis: Illustrating the method for implementation research. Implement. Sci. 2012, 7, 33. [Google Scholar] [CrossRef] [Green Version]
- Manzano, A. The craft of interviewing in realist evaluation. Evaluation 2016, 22, 342–360. [Google Scholar] [CrossRef] [Green Version]
- Kemper, E.A.; Stringfield, S.; Teddlie, C. Mixed methods sampling strategies in social science research. In Handbook of Mixed Methods in the Social and Behavioral Science; Tashakkori, A., Teddlie, C., Eds.; SAGE: Thousand Oaks, CA, USA, 2003; pp. 273–296. [Google Scholar]
- Wong, G.; Westhorp, G.; Manzano, A.; Greenhalgh, J.; Jagosh, J.; Greenhalgh, T. RAMESES II reporting standards for realist evaluations. BMC Med. 2016, 14, 96. [Google Scholar] [CrossRef] [Green Version]
- Graban, M. Fighting against ‘The Way We’ve Always Done It’—Before Lean or with Lean. 2015. Available online: https://www.leanblog.org/2015/11/fighting-against-the-way-weve-always-done-it-before-lean-or-with-lean/ (accessed on 13 August 2017).
- Del Marmol, L. Applying Lean and Agile in an Age of Rapid Change. 2018. Available online: https://leansixsigmabelgium.com/blog/applying-lean-and-agile-in-an-age-of-rapid-change/ (accessed on 13 January 2020).
- Seddon, J.; O’Donovan, B.; Zokaei, K. Lean is a waning fad. Manag. Serv. J. 2011, 55, 34. [Google Scholar]
- McIntosh, B.; Cookson, G. Lean management in the NHS: Fad or panacea. Br. J. Health Care Manag. 2012, 18, 130–135. [Google Scholar] [CrossRef] [Green Version]
- Flynn, R.; Newton, A.S.; Rotter, T.; Hartfield, D.; Walton, S.; Fiander, M.; Scott, S.D. The sustainability of Lean in pediatric healthcare: A realist review. Syst. Rev. 2018, 7, 137. [Google Scholar] [CrossRef]
- Roussel, J. Common Excuses for Neglecting the Continuous Improvement Cycle. 2019. Available online: https://blog.kainexus.com/continuous-improvement/continuous-improvement-cycle/common-excuses-for-neglecting-the-continuous-improvement-cycle (accessed on 13 January 2020).
- Antony, J.; Downey-Ennis, K.; Antony, F.; Seow, C. Can Six Sigma be the “cure” for our “ailing” NHS? Leadersh. Health Serv. 2007, 20, 242–253. [Google Scholar] [CrossRef]
- Antony, J. A SWOT analysis on Six Sigma: Some perspectives from leading academics and practitioners. Int. J. Prod. Perform. Manag. 2012, 61, 691–698. [Google Scholar] [CrossRef]
- Hilton, R.J.; Sohal, A. A conceptual model for the successful deployment of lean six sigma. Int. J. Qual. Reliab. Manag. 2012, 29, 54–70. [Google Scholar] [CrossRef]
- Antony, J.; Krishan, N.; Cullen, D.; Kumar, M. Lean Six Sigma for higher education institutions (HEIs): Challenges, Barriers, success factors, tools/techniques. Int. J. Prod. Perform. Manag. 2012, 61, 940–948. [Google Scholar] [CrossRef]
- Honda, A.C.; Bernardo, V.Z.; Gerolamo, M.C.; Davis, M.M. How lean six sigma principles improve hospital performance. Qual. Manag. J. 2018, 25, 70–82. [Google Scholar] [CrossRef]
- Jones, D. Dan Jones Shares Four Lessons on Lean Healthcare Reducing Waste and Errors: Piloting Lean Principles at Inter-mountain Healthcare Methods, Tools, and Strategies.2017. Available online: http://planet-lean.com/lowdown-on-lean-management-principles-applied-to-healthcare (accessed on 3 February 2017).
- Andersen, H.; Røvik, K.A.; Ingebrigtsen, T. Lean thinking in hospitals: Is there a cure for the absence of evidence? A systematic review of reviews. BMJ Open 2014, 4, e003873. [Google Scholar] [CrossRef] [Green Version]
- Fine, B.A.; Golden, B.; Hannam, R.; Morra, D. Leading lean: A Canadian healthcare leader’s guide. Healthc. Q. 2009, 12, 32–41. [Google Scholar] [CrossRef]
- Cima, R.R.; Brown, M.J.; Hebl, J.R.; Moore, R.; Rogers, J.C.; Kollengode, A.; Amstutz, G.J.; Weisbrod, C.A.; Narr, B.J.; Deschamps, C.; et al. Use of lean and six sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center. J. Am. Coll. Surg. 2011, 213, 83–92. [Google Scholar] [CrossRef]
- Hydes, T.; Hansi, N.; Trebble, T.M. Lean thinking transformation of the unsedated upper gastrointestinal endoscopy pathway improves efficiency and is associated with high levels of patient satisfaction. BMJ Qual. Saf. 2012, 21, 63–69. [Google Scholar] [CrossRef]
- Ben-Tovim, D.I.; Bassham, J.E.; Bolch, D.; Martin, M.A.; Dougherty, M.; Szwarcbord, M. Lean thinking across a hospital: Redesigning care at the Flinders Medical Centre. Aust. Health Rev. 2007, 31, 10–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kollberg, B.; Dahlgaard, J.J.; Brehmer, P. Measuring lean initiatives in health care services: Issues and findings. Int. J. Prod. Perform. Manag. 2006, 56, 7–24. [Google Scholar] [CrossRef]
- Mazzocato, P.; Savage, C.; Brommels, M.; Aronsson, H.; Thor, J. Lean thinking in healthcare: A realist review of the literature. Qual. Saf. Healthc. 2010, 19, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Abo-Hamad, W.; Crowe, J.; Arisha, A. Towards leaner healthcare facility: Application of simulation modelling and value stream mapping. In Proceedings of the International Workshop on Innovative Simulation in Healthcare (I-WISH), Vienna, Austria, 21 September 2012. [Google Scholar]
- Kieran, M.; Cleary, M.; De Brún, A.; Igoe, A. Supply and demand: Application of Lean Six Sigma methods to improve drug round efficiency and release nursing time. Int. J. Qual. Health Care 2017, 29, 803–809. [Google Scholar] [CrossRef] [Green Version]
- Creed, M.; McGuirk, M.; Buckley, R.; De Brún, A.; Kilduff, M. Using lean six sigma to improve controlled drug processes and release nursing time. J. Nurs. Care Qual. 2019, 34, 236–241. [Google Scholar] [CrossRef]
- Davies, C.; Lyons, C.; Whyte, R. Optimizing nursing time in a day care unit: Quality improvement using lean six sigma methodology. Int. J. Qual. Health Care 2019, 31, 22–28. [Google Scholar] [CrossRef]
- Teeling, S.P.; Coetzee, H.; Phillips, M.; McKiernan, M.; NÍ ShÉ, É.; Igoe, A. Reducing risk of development or exacerbation of nutritional deficits by optimizing patient access to mealtime assistance. Int. J. Qual. Health Care 2019, 31, 6–13. [Google Scholar] [CrossRef]
- O’Hora, L.; Stanley, J.; Fox, L.; Murphy, K. An investigation of the effectiveness of lean six sigma strategies in reducing computed tomography order to report time. Radiogr. Irel. 2015, 18, 13–17. [Google Scholar]
- Castle, A.; Harvey, R. Lean information management: The use of observational data in health care. Int. J. Prod. Perform. Manag. 2009, 58, 280–299. [Google Scholar] [CrossRef]
- Deihl, B. Sharpening Coordinated Care Processes; Institute of Industrial and Systems Engineers (IISE): Norcross, Georgia, 2011. [Google Scholar]
- Brown, R.; Grehan, P.; Brennan, M.; Carter, D.; Brady, A.; Moore, E.; Teeling, S.P.; Ward, M.; Eaton, D. Using lean six sigma to improve rates of day of surgery admission in a national thoracic surgery department. Int. J. Qual. Health Care 2019, 31, 14–21. [Google Scholar] [CrossRef]
- McGrath, K.; Casserly, M.; O’mara, F.; Mulsow, J.; Shields, C.; Staunton, O.; Ward, M. Zap it track it: The application of Lean Six Sigma methods to improve the screening system of low-grade mucinous neoplasms of the appendix in an acute hospital setting. Int. J. Qual. Health Care 2019, 31, 35–44. [Google Scholar] [CrossRef]
- Murphy, C.; Mullen, E.; Hogan, K.; O’Toole, R.; Teeling, S.P. Streamlining an existing hip fracture patient pathway in an acute tertiary adult Irish hospital to improve patient experience and outcomes. Int. J. Qual. Health Care 2019, 31, 45–51. [Google Scholar] [CrossRef]
- Ryan, P.; McGrath, C.; Lawrie, I.; Fitzsimons, C.; O’Shea, J.; De BrÚn, A. Enhancing efficiency in a cardiac investigations department by increasing remote patient monitoring. Int. J. Qual. Health Care 2019, 31, 29–34. [Google Scholar] [CrossRef]
- Connolly, K.; Teeling, S.P.; McNamara, M. Live well after stroke. Int. Pract. Dev. J. 2020, 10. [Google Scholar] [CrossRef]
- Donegan, D.; Teeling, S.P.; McNamara, M.; McAweeney, E.; McGrory, L.; Mooney, R. How collaborative working reduced older persons’ length of stay in acute care and increased home discharge: Calling time on the ‘dance of the blind reflex’. Int. Pract. Dev. J. 2021, 11, 1–14. [Google Scholar] [CrossRef]
- Joosten, T.; Bongers, I.; Janssen, R. Application of lean thinking to health care: Issues and observations. Int. J. Qual. Health Care 2009, 21, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Veech, D.S. A Person-Centered Approach to Sustaining a Lean Environment-Job Design for Self-Efficacy; Office of Under Secretary of Defence for Acquisition Technology and Logistics: Washington, DC, USA, 2004. [Google Scholar]
- Liker, J.K. The Toyota Way; Simon & Schuster: New York, NY, USA, 2004. [Google Scholar]
- McCormack, B. A conceptual framework for person-centred practice with older people. Int. J. Nurs. Pract. 2003, 9, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Barraza, M.F.; Ramis-Pujol, J.; Kerbache, L. Thoughts on kaizen and its evolution. Lean Six Sigma J. 2011, 2, 288–308. [Google Scholar] [CrossRef]
- Breckenridge, J.P.; Gray, N.; Toma, M.; Ashmore, S.; Glassborow, R.; Stark, C.; Renfrew, M. Motivating Change: A grounded theory of how to achieve large-scale, sustained change, co-created with improvement organisations across the UK. BMJ Open Qual. 2019, 8, e000553. [Google Scholar] [CrossRef] [Green Version]
- Collins, K.F.; Muthusamy, S.K. Applying the Toyota production system to a healthcare organisation: A case study on a rural community healthcare provider. Qual. Manag. J. 2007, 14, 41–52. [Google Scholar] [CrossRef]
- Found, P.; Harrison, R. Understanding the lean voice of the customer. Int. J. Lean Six Sigma 2012, 3, 251–267. [Google Scholar] [CrossRef]
- Langabeer, J.R.; DelliFraine, J.L.; Heineke, J.; Abbass, I. Implementation of lean and six sigma quality initiatives in hospitals: A goal theoretic perspective. Oper. Manag. Res. 2009, 2, 13–27. [Google Scholar] [CrossRef]
- Arthur, J. Lean Six Sigma for Hospitals: Improving Patient Safety, Patient Flow and the Bottom Line, 2nd ed.; McGrath Hill Education: New York, NY, USA, 2016. [Google Scholar]
- Lipley, N. Productive wards hailed for transforming care. Nurs. Manag. 2009, 16, 4. [Google Scholar] [CrossRef] [PubMed]
- Laloux, F. Reinventing Organisations: A Guide to Creating Organisations Inspired by the Next Stage of Human Consciousness, 1st ed.; Nelson Publishing: Brussels, Belgium, 2014. [Google Scholar]
- Ballé, M.; Régnier, A. Lean as a learning system in a hospital ward. Leadersh. Health Serv. 2007, 20, 33–41. [Google Scholar] [CrossRef] [Green Version]
- Dewing, J.; McCormack, B. Editorial: Tell me, how do you define person-centredness? J. Clin. Nurs. 2017, 26, 2509–2510. [Google Scholar] [CrossRef] [PubMed]
- Ohno, T.; Bodek, N. The Toyota Production System: Beyond Large-Scale Production; Productivity Press: New York, NY, USA, 1988. [Google Scholar]
- Elgar, T.; Smith, C. Global Japanization: The Transnational Transformation for the Labour Process; Routledge: London, UK, 1994. [Google Scholar]
- Wilson, V.; Dewing, J.; Cardiff, S.; Mekki, T.E.; Øye, C.; McCance, T. A person-centred observational tool: Devising the workplace culture critical analysis tool. Int. Pract. Dev. J. 2020, 10, 1–15. [Google Scholar] [CrossRef]
- Radnor, Z.J.; Holweg, M.; Waring, J. Lean in healthcare: The unfilled promise? Soc. Sci. Med. 2012, 74, 364–371. [Google Scholar] [CrossRef] [Green Version]
- Stone, K. Four decades of lean: A systematic literature review. Lean Six Sigma J. 2012, 3, 112–132. [Google Scholar] [CrossRef]
- Lawal, A.K.; Rotter, T.; Kinsman, L.; Sari, N.; Harrison, L.; Jeffery, C.; Kutz, M.; Khan, M.F.; Flynn, R. Lean management in health care: Definition, concepts, methodology and effects reported (systematic review protocol). Syst. Rev. 2014, 3, 103. [Google Scholar] [CrossRef] [Green Version]
- Wackerbarth, S.B.; Bishop, S.S.; Aroh, A.C. Lean in healthcare: Time for evolution or revolution? J. Healthc. Qual. 2021, 43, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Deming, W.E. The New Economics for Industry, Government, Education, 2nd ed.; MIT Press: Cambridge, UK, 2000. [Google Scholar]
- Marriott-Statham, K.; Mackay, M.; Brennan, N.; Mackay, J. Empowering aged care nurses to deliver person-centred care: Enabling nurses to shine. Nurse Educ. Pract. 2018, 31, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, D.; Westhorp, G.; Rotter, T.; Dobson, R.; Bath, B. Lean and leadership practices: Development of an initial realist program theory. BMC Health Serv. Res. Engl. BioMed Cent. 2015, 15, 362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, J. Transforming the patient care environment with lean six sigma and realistic evaluation. J. Healthc. Qual. 2009, 31, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Drotz, E.; Poksinska, B. Lean in healthcare from employees’ perspectives. J. Health Organ. Manag. 2014, 28, 177–195. [Google Scholar] [CrossRef]
- Schattenkirk, D. Building sustainable internal capacity for quality within a healthcare environment. TQM J. 2012, 24, 374–382. [Google Scholar] [CrossRef]
- Amran, M.M.; Januddi, F.; Nuraina, S.; Ikbar, A.M.; Khairanum, S. The barriers in lean healthcare implementation. Test Eng. Manag. 2020, 82, 1972–1981. [Google Scholar]
- Imai, M. Kaizen—The Key to Japan’s Competitive Success; Random House: New York, NY, USA, 1986. [Google Scholar]
- Wittenberg, G. Kaizen—The many ways of getting better. Assem. Autom. 1994, 14, 12–17. [Google Scholar] [CrossRef]
- Gondhalekar, S.; Babu, A.S.; Godrej, N.B. Towards TQM using kaizen process dynamics: A case study. Int. J. Qual. Reliab. Manag. 1995, 12, 192–209. [Google Scholar] [CrossRef]
- Polit, D.; Beck, C. Nursing Research: Principles and Methods, 8th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Costley, C.; Elliott, G.; Gibbs, P. Doing Work Based Research: Approaches to Enquiry for Insider-Researchers; SAGE: London, UK, 2010. [Google Scholar]
- Wilson, V.; McCormack, B. Critical realism as emancipatory action: The case for realistic evaluation in practice development. Nurs. Philos. 2006, 7, 45–57. [Google Scholar] [CrossRef]
- Hochman, M.; Briggs-Malonson, M.; Wilkes, E.; Bergman, J.; Daskivich, L.P.; Moin, T.; Brook, I.; Ryan, G.W.; Brook, R.H.; Mangione, C.M. Fostering a Commitment to Quality: Best Practices in Safety-net Hospitals. J. Health Care Poor Underserved 2016, 27, 293–307. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, G.S.; Patterson, S.H.; Ching, J.M.; Blackmore, C.C. Why Lean doesn’t work for everyone. BMJ Qual. Saf. 2014, 23, 970–973. [Google Scholar] [CrossRef] [Green Version]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teeling, S.P.; Dewing, J.; Baldie, D. A Realist Inquiry to Identify the Contribution of Lean Six Sigma to Person-Centred Care and Cultures. Int. J. Environ. Res. Public Health 2021, 18, 10427. https://doi.org/10.3390/ijerph181910427
Teeling SP, Dewing J, Baldie D. A Realist Inquiry to Identify the Contribution of Lean Six Sigma to Person-Centred Care and Cultures. International Journal of Environmental Research and Public Health. 2021; 18(19):10427. https://doi.org/10.3390/ijerph181910427
Chicago/Turabian StyleTeeling, Seán Paul, Jan Dewing, and Deborah Baldie. 2021. "A Realist Inquiry to Identify the Contribution of Lean Six Sigma to Person-Centred Care and Cultures" International Journal of Environmental Research and Public Health 18, no. 19: 10427. https://doi.org/10.3390/ijerph181910427
APA StyleTeeling, S. P., Dewing, J., & Baldie, D. (2021). A Realist Inquiry to Identify the Contribution of Lean Six Sigma to Person-Centred Care and Cultures. International Journal of Environmental Research and Public Health, 18(19), 10427. https://doi.org/10.3390/ijerph181910427






