The Experience of a Single NHS England Trust on the Impact of the COVID-19 Pandemic on Junior and Middle-Grade Doctors: What Is Next?
Abstract
:1. Introduction
2. Methods
2.1. Design and Sample
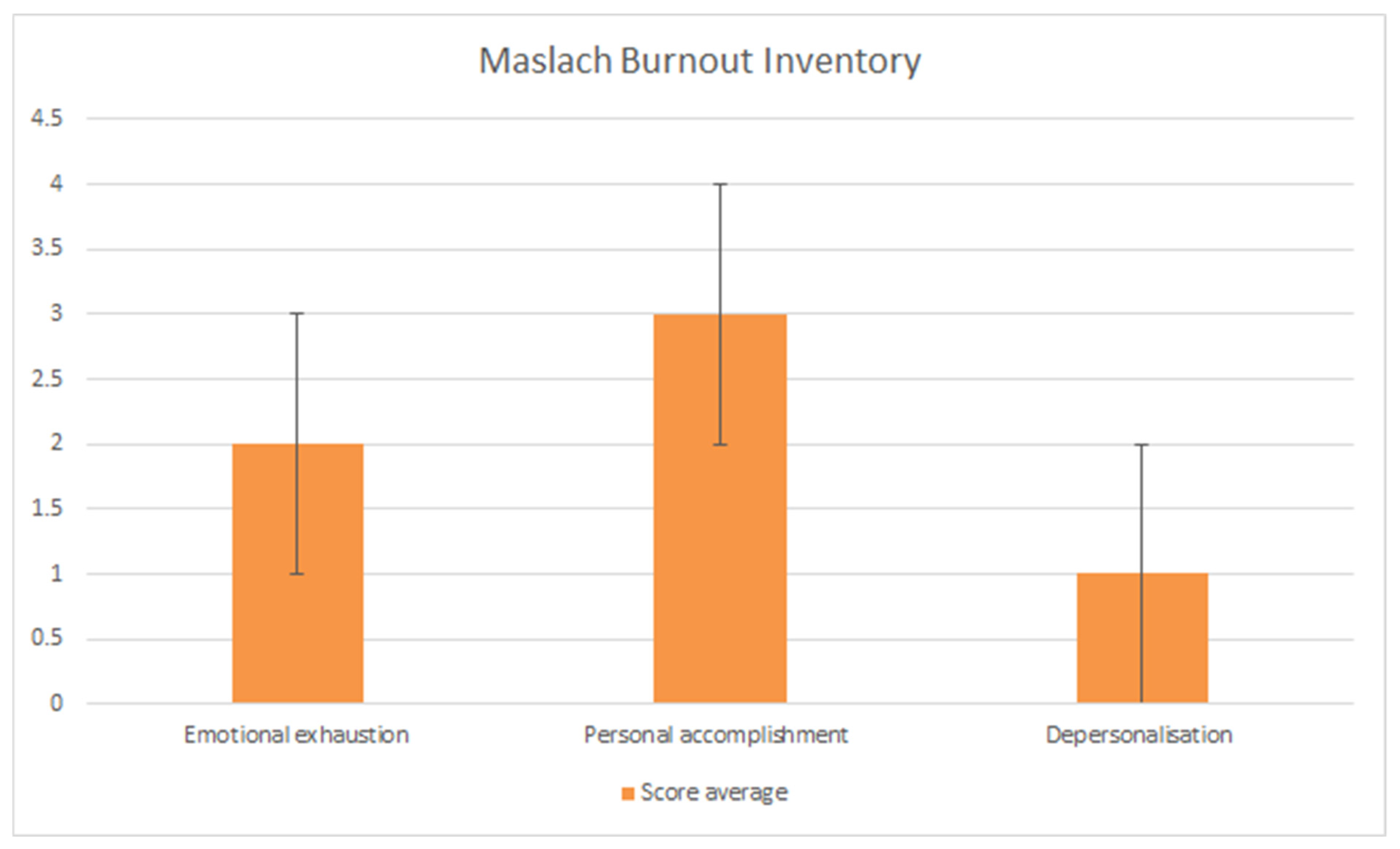
2.2. Measures
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| Demographics/Personal Information | |
| Are you | Male |
| Female | |
| Non-binary | |
| Prefer not to say | |
| Are you | 20–30 years old |
| 30–40 years old | |
| Over 40 years old | |
| Prefer not to say | |
| What describes your marital status? | Single |
| In a relationship | |
| Married | |
| Separated/Divorced | |
| Prefer not to answer | |
| Has the pandemic had an impact on your finances? | Yes, Positive |
| Yes, Negative | |
| No | |
| What best describes your role? | Foundation year 1 |
| Foundation year 2 | |
| SHO in training (CT, IMT, ACCS, ST1-ST2) | |
| SHO staff grade | |
| MTI | |
| SpR in training | |
| Specialty doctor/ SAS | |
| Working circumstances | |
| What specialty do you currently work in? | Medicine |
| Critical Care | |
| Emergency Medicine | |
| Surgery | |
| Other (please specify) | |
| Were you working during the first wave of COVID-19 (March 2020–June 2020)? | Yes |
| No | |
| Which hospital were you working at during the first wave of COVID-19? | Current Hospital |
| Other (please specify) | |
| During the second wave of the pandemic (November 2020–current), have you worked in a COVID-19 “hot” environment (managing suspected or confirmed cases)? | Yes |
| No | |
| Have you been redeployed during the first and second waves? | Yes—During the first wave |
| Yes—During the second wave | |
| Yes-Both waves | |
| No | |
| Do your feel that the workload has changed as a result of COVID-19? | Yes |
| No | |
| How busy do you feel your normal working days have been (during the first wave, between the waves, during the second wave)? | Light |
| Normal | |
| Busy | |
| How busy do you feel your on-call shifts have been (during the first wave, between the waves, during the second wave)? | Light |
| Normal | |
| Busy | |
| Please indicate your current level of satisfaction or dissatisfaction regarding your current work-life balance | Very dissatisfied |
| Somewhat dissatisfied | |
| Neither satisfied/not dissatisfied | |
| Somewhat satisfied | |
| Very satisfied | |
| Please indicate how often these statements are true for you | |
| I feel emotionally drained from work | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel used up at the end of the workday | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel fatigued when I get up in the morning and have to face another day on the job | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| Working with people all day is really a strain for me | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel burned out from my work | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel frustrated by my job? | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel I’m working too hard on my job | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| Working with people directly puts too much stress on me | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel like I am at the end of my rope | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I can easily understand how my patients feel about things | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I deal very effectively with the problems of my patients? | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel I am positively influencing other people’s lives through my work | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel very energetic | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I can easily create a relaxed atmosphere with my patients | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel exhilarated after working closely with my patients | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I have accomplished many worthwhile things in this job | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| In my work, I deal with emotional problems very calmly | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel I treat some patients as if they are impersonal objects | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I have become more callous toward people since I took this job | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I worry that this job is hardening me emotionally | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I do not really care what happens to some patients | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| I feel patients blame me for some of their problems | Never |
| Rarely | |
| Sometimes | |
| Frequently | |
| Always | |
| Would you answer the above questions more favourably before the second wave? | Yes |
| No | |
| Have you sought help of advice about your feelings? | No |
| Yes. If yes by whom? |
References
- British Medical Association. Caring for the Mental Health of the Medical Workforce. 2019. Available online: https://www.bma.org.uk/media/1365/bma-caring-for-the-mental-health-survey-oct-2019.pdf (accessed on 15 August 2021).
- Farrell, S.M.; Kadhum, M.; Lewis, T.; Singh, G.; Penzenstadler, L.; Molodynski, A. Wellbeing and burnout amongst medical students in England. Int. Rev. Psychiatry 2019, 31, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Wurm, W.; Vogel, K.; Holl, A.; Ebner, C.; Bayer, D.; Morkl, S.; Szilagyi, I.S.; Hotter, E.; Kapfhammer, H.P.; Hofmann, P. Depression-Burnout Overlap in Physicians. PLoS ONE 2016, 11, e0149913. [Google Scholar] [CrossRef] [PubMed]
- Rosenstein, A.H.; O’Daniel, M. Impact and implications of disruptive behavior in the perioperative arena. J. Am. Coll. Surg. 2006, 203, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Galbraith, N.; Boyda, D.; McFeeters, D.; Hassan, T. The mental health of doctors during the Covid-19 pandemic. BJPsych Bull. 2021, 45, 93–97. [Google Scholar] [CrossRef]
- Worldometer. COVID-19 Coronavirus Pandemic. Available online: https://www.worldometers.info/coronavirus/ (accessed on 19 August 2021).
- Cubitt, L.J.; Im, Y.R.; Scott, C.J.; Jeynes, L.C.; Molyneux, P.D. Beyond PPE: A mixed qualitative–quantitative study capturing the wider issues affecting doctors’ well-being during the COVID-19 pandemic. BMJ Open 2021, 11, e050223. [Google Scholar] [CrossRef]
- British Medical Association. BMA Survey Covid-19 Tracker Survey February 2021. Available online: https://www.bma.org.uk/media/3810/bma-covid-tracker-survey-february-2021.pdf (accessed on 21 February 2021).
- Chatterjee, S.S.; Bhattacharyya, R.; Bhattacharyya, S.; Gupta, S.; Das, S.; Banerjee, B.B. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian J. Psychiatry 2020, 62, 257–265. [Google Scholar]
- Salem, J.; Hawkins, L.; Sundaram, A.; Gates, J.; Suleman, S.; Mistry, M.; Ong, Y.E.; Fernando, A.; Snelgrove, H.; Chakravorty, I. COVID-19 and the Impact on Doctor Wellbeing and Training: A Mixed Methods Study. Physician 2021, 6, 1–8. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Schaufeli, W.B.; Schwab, R.L. Maslach Burnout Inventory Manual, 4th ed.; Carlson, J.F., Geisinger, K.F., Jonson, J.L., Eds.; Mind Garden, Inc.: Menlo Park, CA, USA, 2017. [Google Scholar]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Coughlan, C.; Nafde, C.; Khodatars, S.; Jeanes, A.L.; Habib, S.; Donaldson, E.; Besi, C.; Kooner, G.K. COVID-19: Lessons for junior doctors redeployed to critical care. Postgrad. Med. J. 2021, 97, 188–191. [Google Scholar] [CrossRef]
- Raza, A.; Matloob, S.; Abdul Rahim, N.F.; Abdul Halim, H.; Khattak, A.; Ahmed, N.H.; Nayab, D.E.; Hakeem, A.; Zubair, M. Factors Impeding Health-Care Professionals to Effectively Treat Coronavirus Disease 2019 Patients in Pakistan: A Qualitative Investigation. Front. Psychol. 2020, 11, 572450. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, J.; Malik, F.; Bin Arif, T.; Majid, Z.; Chaudhary, M.A.; Ahmad, J.; Malik, M.; Khan, T.M.; Khalid, M. Availability of personal protective equipment (PPE) among US and Pakistani doctors in COVID-19 pandemic. Cureus 2020, 12, e8550. [Google Scholar]
- Sultana, A.; Sharma, R.; Hossain, M.M.; Bhattacharya, S.; Purohit, N. Burnout among Healthcare Providers during COVID-19 Pandemic: Challenges and Evidence-based Interventions. Indian. J. Med. Ethics 2020, 4, 1–6. [Google Scholar]
- De Sio, S.; Buomprisco, G.; La Torre, G.; Lapteva, E.; Perri, R.; Greco, E.; Mucci, N.; Cedrone, F. The impact of COVID-19 on doctors’ well-being: Results of a web survey during the lockdown in Italy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7869–7879. [Google Scholar]
- General Medical Council. The State of Medical Education and Practice in the UK. 2020. Available online: https://www.gmc-uk.org/-/media/documents/somep-2020_pdf-84684244.pdf (accessed on 15 August 2021).
- Huo, L.; Zhou, Y.; Li, S.; Ning, Y.; Zeng, L.; Liu, Z.; Qian, W.; Yang, J.; Zhou, X.; Liu, T.; et al. Burnout and Its Relationship with Depressive Symptoms in Medical Staff during the COVID-19 Epidemic in China. Front. Psychol. 2021, 12, 616369. [Google Scholar] [CrossRef]
- Dugani, S.; Afari, H.; Hirschhorn, L.R.; Ratcliffe, H.; Veillard, J.; Martin, G.; Lagomarsino, G.; Basu, L.; Bitton, A. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: A systematic review. Gates Open Res. 2018, 2, 4. [Google Scholar] [CrossRef] [Green Version]
- HM Government. COVID-19 Response—Spring 2021. 2021. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/963491/COVID-19_Response_-_Spring_2021.pdf (accessed on 15 August 2021).
- Peng, Q.Y.; Wang, X.T.; Zhang, L.N. Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020, 46, 849–850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shoja, E.; Aghamohammadi, V.; Bazyar, H.; Moghaddam, H.R.; Nasiri, K.; Dashti, M.; Choupani, A.; Garaee, M.; Aliasgharzadeh, S.; Asgari, A. Covid-19 effects on the workload of Iranian healthcare workers. BMC Public Health 2020, 20, 1636. [Google Scholar] [CrossRef] [PubMed]
- Long, D.; Long, D.; Turner, W.; Lambert, C.C.; Creger, T.; Mugavero, M.J.; Burkholder, G.A. Economic and workload impact of COVID-19 pandemic on physicians in the United States: Results of a national survey. Open Forum Infect. Dis. 2020, 7, S850. [Google Scholar] [CrossRef]
- Hoonakker, P.; Carayon, P.; Gurses, A.; Brown, R.; McGuire, K.; Khunlertkit, A.; Walker, J.M. Measuring workload of ICU nurses with a questionnaire survey: The NASA Task Load Index (TLX). IIE. Trans. Healthc. Syst. Eng. 2011, 1, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Griffiths, P.; Ball, J.; Simon, M.; Aiken, L.H. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: Findings from a cross-sectional study of 12 European countries. BMJ Open 2015, 5, e008331. [Google Scholar] [CrossRef] [Green Version]
- Al-Ghunaim, T.A.; Johnson, J.; Biyani, C.S.; O’Connor, D. Psychological and occupational impact of the COVID-19 pandemic on UK surgeons: A qualitative investigation. BMJ Open 2021, 11, e045699. [Google Scholar] [CrossRef]
- Creese, J.; Byrne, J.P.; Conway, E.; Barrett, E.; Prihodova, L.; Humphries, N. “We All Really Need to Just Take a Breath”: Composite Narratives of Hospital Doctors’ Well-Being during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2051. [Google Scholar] [CrossRef] [PubMed]
- Søreide, K.; Hallet, J.; Matthews, J.B.; Schnitzbauer, A.A.; Line, P.D.; Lai, P.B.S.; Otero, J.; Callegaro, D.; Warner, S.G.; Baxter, N.N.; et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br. J. Surg. 2020, 107, 1250–1261. [Google Scholar] [CrossRef] [PubMed]
- Mallick, R.; Odejinmi, F.; Sideris, M.; Egbase, E.; Kaler, M. The impact of COVID-19 on obstetrics and gynaecology trainees; how do we move on? Facts Views Vis. Obgyn 2021, 13, 9–14. [Google Scholar] [CrossRef]
- Mehta, S.; Machado, F.; Kwizera, A.; Papazian, L.; Moss, M.; Azoulay, É.; Herridge, M. COVID-19: A heavy toll on health-care workers. Lancet Respir. Med. 2021, 9, 226–228. [Google Scholar] [CrossRef]
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef] [Green Version]
- Nap, R.E.; Andriessen, M.P.; Meessen, N.E.; Miranda Ddos, R.; van der Werf, T.S. Pandemic Influenza and Excess Intensive-Care Workload. Emerg. Infect. Dis. 2008, 14, 1518–1525. [Google Scholar] [CrossRef] [PubMed]
- Ferry, A.V.; Wereski, R.; Strachan, F.E.; Mills, N.L. Predictors of UK healthcare worker burnout during the COVID-19 pandemic. QJM 2021, hcab065. [Google Scholar] [CrossRef]
- Denning, M.; Goh, E.T.; Tan, B.; Kanneganti, A.; Almonte, M.; Scott, A.; Martin, G.; Clarke, J.; Sounderajah, V.; Markar, S.; et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: A multinational cross-sectional study. PLoS ONE 2021, 16, e0238666. [Google Scholar] [CrossRef] [PubMed]
- Gemine, R.; Davies, G.R.; Tarrant, S.; Davies, R.M.; James, M.; Lewis, K. Factors associated with work-related burnout in NHS staff during COVID-19: A cross-sectional mixed methods study. BMJ Open 2021, 11, e042591. [Google Scholar] [CrossRef]

| Age Group (Years) | Participants (n = 61) |
|---|---|
| 20–29 | 31 |
| 30–39 | 22 |
| Over 40 | 6 |
| Prefer not to say | 2 |
| Relationship status | |
| Single | 23 |
| In a relationship | 19 |
| Married | 18 |
| Prefer not to answer | 1 |
| Level of training | |
| F1 | 17 |
| F2 | 13 |
| SHO in training (CT, IMT, ACCS, ST1-ST2) | 13 |
| SpR in training (ST3 and above) | 9 |
| SHO staff grade | 5 |
| MTI and Specialty Doctors | 4 |
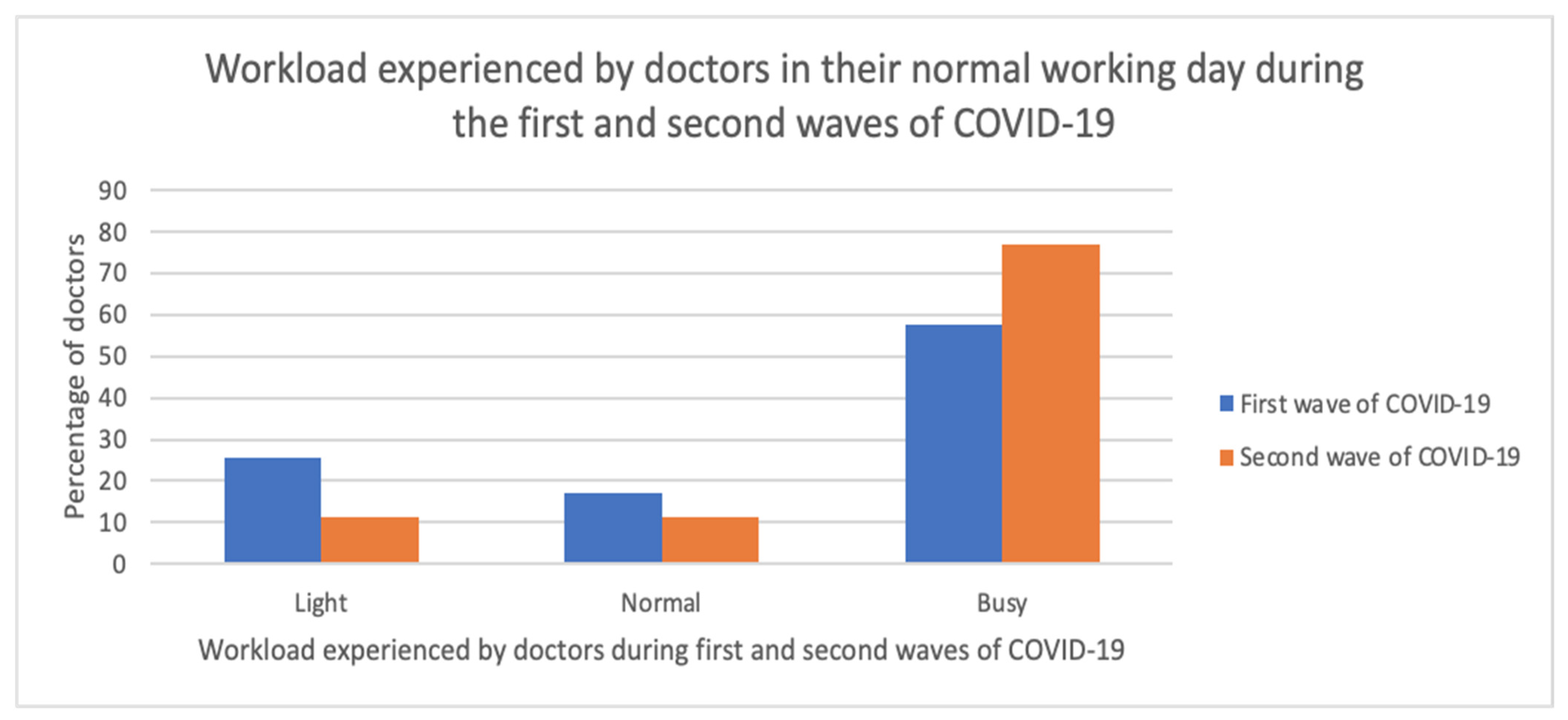
| Has Workload Changed due to COVID-19? | Participants (n = 61) |
|---|---|
| No | 4 |
| Yes | 57 |
| How busy were the normal days during the 1st wave of the pandemic? | |
| Busy | 34 |
| Light | 15 |
| Normal | 10 |
| Skipped | 2 |
| How busy were the on-call shifts during the 1st wave of the pandemic? | |
| Busy | 29 |
| Light | 10 |
| Normal | 20 |
| Skipped | 2 |
| Level of satisfaction/dissatisfaction on current work/life balance | |
| Very or somewhat dissatisfied | 46 |
| Neither satisfied nor dissatisfied | 11 |
| Very or somewhat satisfied | 5 |
| Working during the COVID-19 First Wave | Participants (n = 61) |
|---|---|
| No | 10 |
| Yes | 51 |
| Working in “hot’’ environments during second COVID-19 wave | |
| No | 5 |
| Yes | 56 |
| Have you been redeployed? | |
| No | 27 |
| Yes—both waves | 6 |
| Yes—during the first wave | 16 |
| Yes—during the second wave | 12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Revythis, A.; Shah, S.; Enyioma, S.; Ghose, A.; Patel, M.; Karathanasi, A.; Sanchez, E.; Boussios, S. The Experience of a Single NHS England Trust on the Impact of the COVID-19 Pandemic on Junior and Middle-Grade Doctors: What Is Next? Int. J. Environ. Res. Public Health 2021, 18, 10413. https://doi.org/10.3390/ijerph181910413
Revythis A, Shah S, Enyioma S, Ghose A, Patel M, Karathanasi A, Sanchez E, Boussios S. The Experience of a Single NHS England Trust on the Impact of the COVID-19 Pandemic on Junior and Middle-Grade Doctors: What Is Next? International Journal of Environmental Research and Public Health. 2021; 18(19):10413. https://doi.org/10.3390/ijerph181910413
Chicago/Turabian StyleRevythis, Antonios, Sidrah Shah, Synthia Enyioma, Aruni Ghose, Meenash Patel, Afroditi Karathanasi, Elisabet Sanchez, and Stergios Boussios. 2021. "The Experience of a Single NHS England Trust on the Impact of the COVID-19 Pandemic on Junior and Middle-Grade Doctors: What Is Next?" International Journal of Environmental Research and Public Health 18, no. 19: 10413. https://doi.org/10.3390/ijerph181910413
APA StyleRevythis, A., Shah, S., Enyioma, S., Ghose, A., Patel, M., Karathanasi, A., Sanchez, E., & Boussios, S. (2021). The Experience of a Single NHS England Trust on the Impact of the COVID-19 Pandemic on Junior and Middle-Grade Doctors: What Is Next? International Journal of Environmental Research and Public Health, 18(19), 10413. https://doi.org/10.3390/ijerph181910413








