Global Gender Disparities in Premature Death from Cardiovascular Disease, and Their Associations with Country Capacity for Noncommunicable Disease Prevention and Control
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Materials
2.1.1. Global Health Estimates Country-Specific CVD Mortality
2.1.2. Country Capacity for the Prevention and Control of NCDs
2.1.3. Other Variables
2.2. Statistical Analysis
3. Results
3.1. Regional and Temporal Trends in Total Age-Standardized Premature Death Rates
3.2. Gender Disparities among Geographic Regions and Income Groups
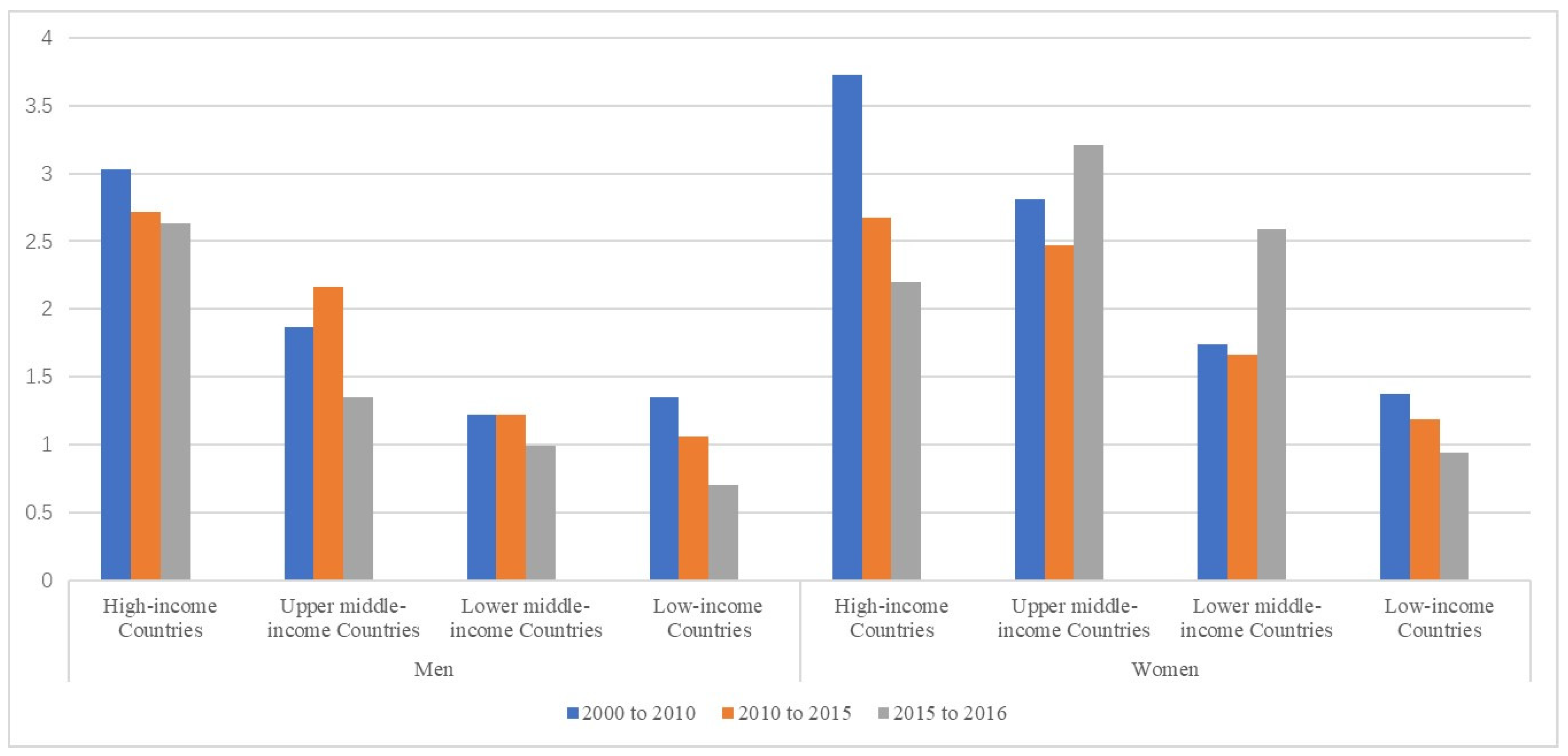
3.3. Premature Death Rates and Gender Differences Associated with National NCD Capacity of Prevention
4. Discussion
4.1. Overall Trends in Global Premature CVD-Related Deaths
4.2. Gender Differences in CVD-Related Premature Mortality
4.3. National Capacity for the Prevention and Control of NCDs
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- GBD Causes of Death Collaborator. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Dis-ease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Vogel, B.; Acevedo, M.; Appelman, Y.; Merz, C.N.B.; Chieffo, A.; Figtree, G.A.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.H.E.M.; et al. The Lancet women and cardiovascular disease Commission: Reducing the global burden by 2030. Lancet 2021. [Google Scholar] [CrossRef]
- Bhatnagar, P.; Wickramasinghe, K.; Williams, J.; Rayner, M.; Townsend, N. The epidemiology of cardiovascular disease in the UK 2014. Heart 2015, 101, 1182–1189. [Google Scholar] [CrossRef]
- National Center for Cardiovascular Diseases of China. Report on Cardiovascular Diseases in China 2018; Encyclopedia of China Publishing House: Beijing, China, 2019. [Google Scholar]
- Gheorghe, A.; Griffiths, U.; Murphy, A.; Legido-Quigley, H.; Lamptey, P.; Perel, P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: A systematic review. BMC Public Health 2018, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- WHO. The Nine Voluntary Global Targets and 25 Indicators Aimed at Combatting Global Mortality from the Four Main NCDs. 2013. Available online: https://www.who.int/nmh/global_monitoring_framework/2013-11-06-who-dc-c268-whp-gap-ncds-techdoc-def3.pdf?ua=1 (accessed on 8 February 2019).
- Roth, G.A.; Huffman, M.D.; Moran, A.E.; Feigin, V.; Mensah, G.A.; Naghavi, M.; Murray, C.J. Global and Regional Patterns in Cardiovascular Mortality from 1990 to 2013. Circulation 2015, 132, 1667–1678. [Google Scholar] [CrossRef] [PubMed]
- Hyun, K.K.; Redfern, J.; Patel, A.; Peiris, D.; Brieger, D.; Sullivan, D.; Harris, M.; Usherwood, T.; MacMahon, S.; Lyford, M.; et al. Gender inequalities in cardiovascular risk factor assessment and management in primary healthcare. Heart 2017, 103, 492–498. [Google Scholar] [CrossRef]
- Clemens, K.K.; Woodward, M.; Neal, B.; Zinman, B. Sex Disparities in Cardiovascular Outcome Trials of Populations with Diabetes: A Systematic Review and Meta-analysis. Diabetes Care 2020, 43, 1157–1163. [Google Scholar] [CrossRef]
- Tzoulaki, I.; Elliott, P.; Kontis, V.; Ezzati, M. Worldwide Exposures to Cardiovascular Risk Factors and Associated Health Effects: Current Knowledge and Data Gaps. Circulation 2016, 133, 2314–2333. [Google Scholar] [CrossRef] [PubMed]
- Pearson-Stuttard, J.; Guzman-Castillo, M.; Penalvo, J.L.; Rehm, C.D.; Afshin, A.; Danaei, G.; Kypridemos, C.; Gaziano, T.; Mozaffarian, D.; Capewell, S.; et al. Modeling Future Cardiovascular Disease Mortality in the United States: National Trends and Ra-cial and Ethnic Disparities. Circulation 2016, 133, 967–978. [Google Scholar] [CrossRef] [PubMed]
- Mosca, L.; Benjamin, E.J.; Berra, K.; Bezanson, J.L.; Dolor, R.J.; Lloyd-Jones, D.M.; Newby, L.K.; Piña, I.L.; Roger, V.L.; Shaw, L.J.; et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: A guide-line from the American heart association. Circulation 2011, 123, 1243–1262. [Google Scholar] [CrossRef]
- WHO. Global Health Observatory Data Repository: Noncommunicable Diseases. 2019. Available online: http://apps.who.int/gho/data/node.main.A858?lang=en (accessed on 20 September 2020).
- WHO. WHO Methods and Data Sources for Country-Level Causes of Death 2000–2016. 2018. Available online: http://terrance.who.int/mediacentre/data/ghe/GlobalCOD_method_2000_2016.pdf?ua=1 (accessed on 18 September 2020).
- Peto, R.; Lopez, A.D.; Norheim, O.F. Halving premature death. Science 2014, 345, 1272. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.; Lozano, R.; Inoue, M. Age Standardization of Rates: A New Who Standard; In GPE Discussion Paper Series; EIP/GPE/EBD World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- WHO. Assessing National Capacity for the Prevention and Control of Noncommunicable Diseases: Report of the 2015 Global Survey. 2016. Available online: https://apps.who.int/iris/bitstream/handle/10665/246223/9789241565363-eng.pdf?sequence=1&isAllowed=y (accessed on 21 March 2021).
- World Health Organization. Everybody’s Business—Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action. 2007. Available online: https://apps.who.int/iris/handle/10665/43918 (accessed on 29 September 2021).
- Kontis, V.; Mathers, C.D.; Bonita, R.; Stevens, G.A.; Rehm, J.; Shield, K.D.; Riley, L.M.; Vladimir Poznyak, V.; Jabbour, S.; Garg, R.M.; et al. Regional contributions of six preventable risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: A modelling study. Lancet Glob. Health 2015, 3, e746–e757. [Google Scholar] [CrossRef]
- Kontis, V.; Mathers, C.D.; Rehm, J.; Stevens, G.A.; Shield, K.D.; Bonita, R.; Riley, L.M.; Poznyak, V.; Beaglehole, R.; Ezzati, M. Contribution of six risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: A modelling study. Lancet 2014, 384, 427–437. [Google Scholar] [CrossRef]
- Dugani, S.; Gaziano, T.A. 25 by 25: Achieving Global Reduction in Cardiovascular Mortality. Curr. Cardiol. Rep. 2016, 18, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Joseph, P.; Leong, D.; McKee, M.; Anand, S.S.; Schwalm, J.-D.; Teo, K.; Mente, A.; Yusuf, S. Reducing the Global Burden of Cardiovascular Disease, Part 1. Circ. Res. 2017, 121, 677–694. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Corsi, D.J.; Gilmore, A.; Kruger, A.; Igumbor, E.; Chifamba, J.; Yang, W.; Wei, L.; Iqbal, R.; Mony, P.; et al. Tobacco control environment: Cross-sectional survey of policy implementation, social unacceptability, knowledge of tobacco health harms and relationship to quit ratio in 17 low-income, middle-income and high-income countries. BMJ Open 2017, 7, e013817. [Google Scholar] [CrossRef]
- Martinez-Lacoba, R.; Pardo-Garcia, I.; Amo-Saus, E.; Sotos, F.E. Mediterranean diet and health outcomes: A systematic meta-review. Eur. J. Public Health 2018, 28, 955–961. [Google Scholar] [CrossRef]
- Montagnese, C.; Santarpia, L.; Iavarone, F.; Strangio, F.; Sangiovanni, B.; Buonifacio, M.; Caldara, A.R.; Silvestri, E.; Contaldo, F.; Pasanisi, F. Food-Based Dietary Guidelines around the World: Eastern Mediterranean and Middle Eastern Countries. Nutrients 2019, 11, 1325. [Google Scholar] [CrossRef]
- Dorbala, S.; Shaw, L.J. Changing the trajectory of ischemic heart disease in women: Role of imaging. J. Nucl. Cardiol. 2016, 23, 973–975. [Google Scholar] [CrossRef]
- Lopez, A.D.; Adair, T. Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics. Int. J. Epidemiol. 2019, 48, 1815–1823. [Google Scholar] [CrossRef] [PubMed]
- Ni, H.; Coady, S.; Rosamond, W.; Folsom, A.R.; Chambless, L.; Russell, S.D.; Sorlie, P.D. Trends from 1987 to 2004 in sudden death due to coronary heart disease: The Atherosclerosis Risk in Communi-ties (ARIC) study. Am. Heart J. 2009, 157, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Gulati, M. Improving the Cardiovascular Health of Women in the Nation: Moving Beyond the Bikini Boundaries. Circulation 2017, 135, 495–498. [Google Scholar] [CrossRef] [PubMed]
- De Smedt, D.; De Bacquer, D.; De Sutter, J.; Dallongeville, J.; Gevaert, S.; De Backer, G.; Bruthans, J.; Kotseva, K.; Reiner, Ž.; Tokgözoğlu, L.; et al. The gender gap in risk factor control: Effects of age and education on the control of cardiovascular risk factors in male and female coronary patients. The EUROASPIRE IV study by the European Society of Cardiology. Int. J. Cardiol. 2016, 209, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Saliba, M.; Zurayk, H. Expanding concern for women’s health in developing countries: The case of the Eastern Mediter-ranean Region. Womens Health Issues 2010, 20, 171–177. [Google Scholar] [CrossRef]
- Leal, M.T.B.C.; Passos, L.S.A.; Guarçoni, F.V.; Aguiar, J.M.D.S.; Da Silva, R.B.R.; De Paula, T.M.N.; Dos Santos, R.F.; Nassif, M.C.L.; Gomes, N.F.A.; Tan, T.C.; et al. Rheumatic heart disease in the modern era: Recent developments and current challenges. Rev. Soc. Bras. Med. Trop. 2019, 52, e20180041. [Google Scholar] [CrossRef] [PubMed]
- Sliwa, K.; Ojji, D.; Bachelier, K.; Böhm, M.; Damasceno, A.; Stewart, S. Hypertension and hypertensive heart disease in African women. Clin. Res. Cardiol. 2014, 103, 515–523. [Google Scholar] [CrossRef]
- Huxley, R.; Barzi, F.; Woodward, M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: Meta-analysis of 37 prospective cohort studies. BMJ 2005, 332, 73–78. [Google Scholar] [CrossRef]
- Domanski, M.J.; Jablonski, K.A.; Rice, M.M.; Fowler, S.E.; Braunwald, E. Obesity and cardiovascular events in patients with established coronary disease. Eur. Heart J. 2006, 27, 1416–1422. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prescott, E.; Hippe, M.; Schnohr, P.; Hein, H.O.; Vestbo, J. Smoking and risk of myocardial infarction in women and men: Longitudinal population study. BMJ 1998, 316, 1043–1047. [Google Scholar] [CrossRef] [PubMed]
- Ståhl, T. Health in All Policies: From rhetoric to implementation and evaluation—The Finnish experience. Scand. J. Public Health 2018, 46, 38–46. [Google Scholar] [CrossRef]
- Lencucha, R.; Reddy, S.K.; Labonté, R.; Drope, J.; Magati, P.; Goma, F.; Zulu, R.; Makoka, D. Global tobacco control and economic norms: An analysis of normative commitments in Kenya, Malawi and Zambia. Health Policy Plan. 2018, 33, 420–428. [Google Scholar] [CrossRef]

| Region | 2000 | 2010 | 2015 | 2016 | N | APC | p for Trend | |
|---|---|---|---|---|---|---|---|---|
| Relative Gender Differences (%) | Overall | 35.6 | 39.0 | 39.8 | 40.5 | 183 | 0.79 | 0.177 |
| (32.2, 38.9) | (35.6, 42.4) | (36.4, 43.2) | (37.1, 43.9) | |||||
| Eastern Mediterranean | 27.9 | 30.0 | 30.3 | 30.5 | 21 | 0.07 | 0.855 | |
| (22.2, 33.7) | (25.3, 34.6) | (25.9, 34.8) | (25.9, 35.2) | |||||
| Europe | 57.6 | 61.6 | 62.3 | 62.5 | 50 | 0.51 | 0.02 | |
| (54.8, 60.4) | (59.0., 64.2) | (59.9, 64.6) | (60.2, 64.7) | |||||
| Western Pacific | 39.9 | 45.8 | 47.2 | 48.8 | 21 | 0.13 | 0.457 | |
| (31.5, 48.3) | (37.0, 54.6) | (38.5, 55.9) | (40.0, 57.7) | |||||
| South-East Asia | 25.3 | 33.8 | 38.0 | 38.8 | 11 | 2.72 | 0.525 | |
| (7.8, 42.9) | (18.1, 49.5) | (23.2, 52.9) | (23.7, 54) | |||||
| Africa | 14.5 | 15.7 | 15.5 | 16.5 | 47 | 0.66 | 0.971 | |
| (8.5, 20.4) | (9.8, 21.6) | (9.1, 21.8) | (10.6, 22.5) | |||||
| America | 37.7 | 41.1 | 42.3 | 43.0 | 33 | 0.8 | 0.358 | |
| (33.0, 42.4) | (36.3, 45.9) | (37.9, 46.6) | (38.5, 47.5) | |||||
| Men (per 100,000 people) | Overall | 139.4 | 116.1 | 106.1 | 104.7 | 183 | −1.79 | <0.0001 |
| (130.3, 148.6) | (107.4, 124.7) | (98.4, 113.9) | (97.1, 112.3) | |||||
| Eastern Mediterranean | 158.2 | 131.1 | 121.3 | 120.5 | 21 | −1.72 | 0.061 | |
| (136.5, 179.9) | (107.5, 154.6) | (97.9, 144.6) | (97.1, 143.8) | |||||
| Europe | 155.2 | 124.8 | 107.1 | 103.6 | 50 | −2.48 | 0.007 | |
| (129.5, 180.9) | (99.7, 149.9) | (86.1, 128.1) | (83.4, 123.8) | |||||
| Western Pacific | 141.7 | 118.8 | 112.7 | 112.0 | 21 | −1.48 | 0.376 | |
| (110.4, 173) | (91.2, 146.5) | (85.6, 139.8) | (84.6, 139.4) | |||||
| South-East Asia | 135.0 | 125.4 | 120.2 | 118.9 | 11 | −0.78 | 0.723 | |
| (111.4, 158.6) | (101.7, 149.1) | (94.7, 145.7) | (93.8, 143.9) | |||||
| Africa | 132.7 | 113.3 | 105.5 | 105.0 | 47 | −1.48 | 0.0001 | |
| (122.2, 143.2) | (104.0, 122.6) | (96.3, 114.8) | (95.8, 114.2) | |||||
| America | 113.2 | 92.2 | 87.1 | 86.6 | 33 | −1.69 | 0.016 | |
| (98.1, 128.3) | (79.6, 104.8) | (73.8, 100.3) | (73.3, 99.9) | |||||
| Women (per 100,000 people) | Overall | 88.9 | 70.9 | 64.4 | 63.0 | 183 | −2.13 | <0.0001 |
| (82.6, 95.3) | (65.1, 76.7) | (58.9, 70.0) | (57.5, 68.5) | |||||
| Eastern Mediterranean | 113.5 | 91.5 | 84.5 | 83.6 | 21 | −1.91 | 0.072 | |
| (94.8, 132.2) | (72.6, 110.5) | (65.9, 103.1) | (65.1, 102.1) | |||||
| Europe | 68.2 | 49.9 | 41.4 | 39.6 | 50 | −3.32 | 0.0004 | |
| (55.5, 80.8) | (38.9, 60.9) | (32.3, 50.4) | (31.0, 48.2) | |||||
| Western Pacific | 86.7 | 66.0 | 61.2 | 58.5 | 21 | −2.37 | 0.099 | |
| (64.6, 108.9) | (48.6, 83.3) | (44.8, 77.5) | (42.4, 74.7) | |||||
| South-East Asia | 98.1 | 82.4 | 74.4 | 73.0 | 11 | −1.83 | 0.286 | |
| (73.3, 122.9) | (60.5, 104.3) | (52.9, 95.9) | (51.4, 94.6) | |||||
| Africa | 111.2 | 94.6 | 88.2 | 87.0 | 47 | −1.53 | 0.001 | |
| (101.6, 120.9) | (85.0, 104.2) | (78.5, 97.8) | (77.3, 96.6) | |||||
| America | 71.4 | 55.2 | 51.6 | 50.6 | 33 | −2.13 | 0.021 | |
| (59.3, 83.5) | (45.2, 65.2) | (41.2, 62.1) | (40.2, 61.0) | |||||
| Total (per 100,000 people) | Overall | 113.2 | 92.6 | 84.5 | 82.9 | 183 | −1.93 | <0.0001 |
| (106.1, 120.3) | (86.0, 99.1) | (78.4, 90.6) | (76.9, 88.9) | |||||
| Eastern Mediterranean | 136.7 | 112.4 | 104.0 | 103.1 | 21 | −1.77 | 0.056 | |
| (117.3, 156.1) | (91.7, 133.0) | (83.7, 124.4) | (82.9, 123.4) | |||||
| Europe | 108.6 | 84.5 | 71.9 | 69.3 | 50 | −2.75 | 0.002 | |
| (90.6, 126.6) | (67.7, 101.4) | (57.8, 86.0) | (55.8, 82.8) | |||||
| Western Pacific | 114.1 | 92.7 | 86.4 | 84.1 | 21 | −1.86 | 0.188 | |
| (88.1, 140.0) | (71.2, 114.2) | (65.6, 107.1) | (63.6, 104.6) | |||||
| South-East Asia | 115.4 | 103.5 | 96.4 | 94.9 | 11 | −1.21 | 0.383 | |
| (94.6, 136.3) | (84.1, 122.9) | (75.8, 117.1) | (74.4, 115.5) | |||||
| Africa | 121.8 | 103.3 | 96.4 | 95.5 | 47 | −1.52 | <0.0001 | |
| (112.6, 130.9) | (94.4, 112.2) | (87.6, 105.2) | (86.7, 104.3) | |||||
| America | 91.7 | 73.1 | 69.0 | 67.9 | 33 | −1.86 | 0.015 | |
| (78.5, 104.9) | (62.2, 84.0) | (57.3, 80.6) | (56.4, 79.5) | |||||
| Income Groups | 2000 | 2010 | 2015 | 2016 | N | APC | p for Trend | |
|---|---|---|---|---|---|---|---|---|
| Relative Gender Differences (%) | HICs | 54.5 | 58.1 | 58.0 | 57.8 | 52 | 0.38 | 0.543 |
| (50.4, 58.7) | (54.1, 62.2) | (54.0, 62.0) | (53.7, 61.8) | |||||
| UMICs | 39.3 | 44.2 | 45.7 | 46.8 | 54 | 1.05 | 0.06 | |
| (35.5, 43.2) | (40.0, 48.4) | (41.4, 49.9) | (42.4, 51.1) | |||||
| LMICs | 20.4 | 24.0 | 25.4 | 27.0 | 46 | 1.63 | 0.618 | |
| (13.4, 27.5) | (16.9, 31.1) | (17.8, 33.0) | (19.6, 34.3) | |||||
| LICs | 19.6 | 20.0 | 20.5 | 20.8 | 31 | 0.32 | 0.993 | |
| (13.4, 25.9) | (14.5, 25.5) | (14.9, 26.0) | (15.2, 26.3) | |||||
| Men (per 100,000 people) | HICs | 103.9 | 76.4 | 66.6 | 64.8 | 52 | −2.91 | <0.0001 |
| (89.4, 118.5) | (63.2, 89.6) | (55.3, 77.8) | (53.9, 75.7) | |||||
| UMICs | 156.8 | 129.9 | 116.4 | 114.9 | 54 | −1.94 | 0.001 | |
| (136.9, 176.7) | (112.3, 147.5) | (101.9, 131.0) | (100.8, 129.0) | |||||
| LMICs | 151.2 | 133.7 | 125.8 | 124.6 | 46 | −1.21 | 0.063 | |
| (134.6, 167.7) | (117.4, 150.1) | (110.7, 140.9) | (110.0, 139.2) | |||||
| LICs | 151.3 | 132.2 | 125.3 | 124.5 | 31 | −1.23 | 0.047 | |
| (134.7, 168) | (116.8, 147.5) | (110.4, 140.3) | (109.7, 139.2) | |||||
| Women (per 100,000 people) | HICs | 47.2 | 32.3 | 28.2 | 27.6 | 52 | −3.33 | <0.0001 |
| (39.8, 54.5) | (26.2, 38.3) | (22.9, 33.4) | (22.4, 32.7) | |||||
| UMICs | 89.6 | 67.4 | 59.5 | 57.6 | 54 | −2.71 | <0.0001 | |
| (81.0, 98.2) | (60.4, 74.4) | (53.0, 65.9) | (51.2, 63.9) | |||||
| LMICs | 113.9 | 95.6 | 87.9 | 85.6 | 46 | −1.74 | 0.0002 | |
| (103.4, 124.5) | (86.2, 105.0) | (78.5, 97.4) | (76.2, 95.1) | |||||
| LICs | 120.8 | 105.2 | 99.1 | 98.2 | 31 | −1.3 | 0.077 | |
| (105.5, 136.1) | (91.4, 119.1) | (85.8, 112.4) | (84.9, 111.5) | |||||
| Total (per 100,000 people) | HICs | 74.2 | 53.8 | 47.3 | 45.9 | 52 | −2.96 | <0.0001 |
| (64.2, 84.2) | (44.8, 62.7) | (39.5, 55.1) | (38.4, 53.3) | |||||
| UMICs | 121.6 | 97.3 | 86.4 | 84.6 | 54 | −2.25 | <0.0001 | |
| (108.7, 134.6) | (86.3, 108.3) | (77, 95.7) | (75.4, 93.7) | |||||
| LMICs | 132.4 | 113.7 | 106.0 | 104.1 | 46 | −1.48 | <0.0001 | |
| (120.3, 144.4) | (102.2, 125.2) | (95.1, 116.9) | (93.6, 114.7) | |||||
| LICs | 135.4 | 118.1 | 111.6 | 110.7 | 31 | −1.26 | 0.002 | |
| (120.0, 150.8) | (104.1, 132.1) | (98.2, 125.0) | (97.3, 124.1) | |||||
| Indicators of National Capacity | Gender Differences | Mortality of Men | Mortality of Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Multivariable Model | Unadjusted | Multivariable Model | Unadjusted | Multivariable Model | |||||||
| β Coefficient | p Value | β Coefficient | p Value | β Coefficient | p Value | β Coefficient | p Value | β Coefficient | p Value | β Coefficient | p Value | |
| Existence of an operational unit, Branch, or dept. in the ministry of health with responsibility for NCDs | 15.03 | <0.0001 | 10.08 | 0.0099 | −19.25 | 0.0336 | −13.8 | 0.1627 | −28.37 | <0.0001 | −20.65 | 0.0015 |
| Existence of a national multisectoral commission, agency or mechanism for NCDs | 12.92 | 0.0006 | 7.98 | 0.0338 | −2.66 | 0.7674 | 3.33 | 0.7259 | −16.54 | 0.0079 | −7.34 | 0.2341 |
| Existence of an operational, multisectoral national NCD policy, strategy, or action plan that integrates several NCDs and their risk factors | 4.00 | 0.2785 | −1.31 | 0.7522 | 2.87 | 0.7392 | 11.36 | 0.284 | −5.17 | 0.3914 | 6.63 | 0.3346 |
| Existence of operational policy/strategy/action plan for cardiovascular diseases | 7.14 | 0.0703 | −1.54 | 0.7421 | −9.76 | 0.2911 | −7.93 | 0.5052 | −15.93 | 0.0131 | −5.76 | 0.4548 |
| Availability of cardiovascular risk stratification in 50% or more primary health care facilities | 16.43 | 0.0001 | 13.13 | 0.0021 | −6.85 | 0.5049 | −2.88 | 0.7882 | −22.2 | 0.0017 | −16.08 | 0.0216 |
| Has a STEPS survey or a comprehensive health examination survey every 5 years | 11.22 | 0.0107 | 4.96 | 0.245 | −14.08 | 0.1735 | −6.18 | 0.5687 | −18.95 | 0.0083 | −8.21 | 0.2433 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Jin, Y.; Jia, P.; Li, N.; Zheng, Z.-J. Global Gender Disparities in Premature Death from Cardiovascular Disease, and Their Associations with Country Capacity for Noncommunicable Disease Prevention and Control. Int. J. Environ. Res. Public Health 2021, 18, 10389. https://doi.org/10.3390/ijerph181910389
Zhang J, Jin Y, Jia P, Li N, Zheng Z-J. Global Gender Disparities in Premature Death from Cardiovascular Disease, and Their Associations with Country Capacity for Noncommunicable Disease Prevention and Control. International Journal of Environmental Research and Public Health. 2021; 18(19):10389. https://doi.org/10.3390/ijerph181910389
Chicago/Turabian StyleZhang, Ji, Yinzi Jin, Peng Jia, Na Li, and Zhi-Jie Zheng. 2021. "Global Gender Disparities in Premature Death from Cardiovascular Disease, and Their Associations with Country Capacity for Noncommunicable Disease Prevention and Control" International Journal of Environmental Research and Public Health 18, no. 19: 10389. https://doi.org/10.3390/ijerph181910389
APA StyleZhang, J., Jin, Y., Jia, P., Li, N., & Zheng, Z.-J. (2021). Global Gender Disparities in Premature Death from Cardiovascular Disease, and Their Associations with Country Capacity for Noncommunicable Disease Prevention and Control. International Journal of Environmental Research and Public Health, 18(19), 10389. https://doi.org/10.3390/ijerph181910389








