The Impact of COVID-19 on Individuals with Hearing and Visual Disabilities during the First Pandemic Wave in Italy
Abstract
:1. Background
2. Materials and Methods
2.1. Inclusion Criteria
- -
- suffering from pre-lingual deafness;
- -
- with a mean sensorineural hearing deficit ≥60 dB for 500 Hz, 1000 Hz, and 2000 Hz frequency tones in the best ear.
- -
- residual visus < 3/10 in both eyes or in the best eye, even with refractory correction;
- -
- binocular perimetric residue <30%.
2.2. The Questionnaire
- The first collected demographic data of study subjects: sex, age, type of disability, and geographical area of residence.
- In the second, the impact of the COVID-19 pandemic on education and working activities and on any changes in social relationships was delved into.
- The third dealt with aspects of health/social care, rehabilitation care, use of PPE, and their eventual side-effects.
- The last part of the questionnaire analyzed eventual repercussions of the COVID-19 pandemic on patients’ quality of life in terms of sleep disorders, concentration difficulties, and use of symptomatic drugs. Further free answers provided understanding and insights.
2.3. Lifestyle, Stress Management, and Related Stressors
3. Results
3.1. Lifehabits and Perceived Well-Being
3.2. Education
3.3. Work
3.4. Health, Social and Rehabilitation Services
3.5. Emotional Aspects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hui, D.S.; Azhar, E.I.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; Mchugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The Continuing 2019-nCoV Epidemic. Threat of Novel Coronaviruses to Global Health-The Latest 2019 Novel Coronavirus Outbreak in Wuhan. China Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef]
- World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. Available online: https://www.who.int/publications-detail/report-of-the-who-china-jointmission-oncoronavirus-disease-2019-(COVID-19) (accessed on 17 April 2020).
- Bubbico, L.; Mastrangelo, G.; Larese-Filon, F.; Basso, P.; Rigoli, R.; Maurelli, M.; Ferlito, S.; Capelli, M.; Gisabella, C.; Javanbakht, M.; et al. Community Use of Face Masks against the Spread of COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 3214. [Google Scholar] [CrossRef] [PubMed]
- Pulvirenti, F.; Cinetto, F.; Milito, C.; Bonanni, L.; Pesce, A.M.; Leodori, G.; Garzi, G.; Miglionico, M.; Tabolli, S.; Quinti, I. Health-Related-Quality of Life in Common Variable Immunodeficiency Italian patients switched to remote assistance during the COVID-19 pandemic. J. Allergy Clin. Immunol. 2020, 8, 1894–1899. [Google Scholar] [CrossRef] [PubMed]
- Shultz, J.M.; Baingana, F.; Neria, Y. The 2014 Ebola outbreak and mentalhealth: Current status and recommendedresponse. JAMA 2015, 313, 567–568. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessel, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- United Nations. UN Leads Call to Protect Most Vulnerable from Mental Health Crisis during and after COVID-19. 2020. Available online: https://news.un.org/en/story/2020/05/1063882 (accessed on 21 September 2021).
- Daly, M.; Sutin, A.; Robinson, E. Longitudinal changes in mental health and the COVID-19 pandemic: Evidence from the UK house hold longitudinal study. Psychol. Med. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef]
- Colten, H.R.; Prendergast, K.B.; Schofield, G.M.; Mackay, L.M. Associations between lifestyle behaviours and optimal wellbeing in a diverse sample of New Zealand adults. BMC Public Health 2015, 16, 62. [Google Scholar]
- Rotarou, E.S.; Sakellariou, D.; Kakoullis, E.J.; Warren, N. Disabled people in the time of COVID-19: Identifying needs, promoting inclusivity. J. Glob. Health 2021, 11, 03007. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Disability 2011; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Office for National Statistics. Coronavirus (COVID-19) Related Deaths by Disability Status, England and Wales: 2 March to 15 May 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coro-naviruscovid19relateddeathsbydisabilitystatusenglandandwales/2marchto15may2020 (accessed on 28 August 2020).
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P.A. Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- ISTAT (2019). Knowking the Disability World: People, Relationships and Institutions. Available online: https://www.istat.it/it/archivio/236301 (accessed on 21 September 2021).
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, e37–e38. [Google Scholar] [CrossRef]
- World Health Organization. WHO Releases New International Classification of Diseases (ICD 11). Available online: https://www.who.int/news/item/18–06-2018-who-releases-new-international-classification-of-diseases-(icd-11) (accessed on 16 August 2021).
- World Health Organization. World Report on Hearing. Available online: https://www.who.int/publications/i/item/world-report-on-hearing (accessed on 21 September 2021).
- Delic, V.; Seƒcujski, M.; Vujnoviƒá Sedlar, N.; Miskovic, D.; Mak, R.; Bojanic, M. How Speech Technologies Can Help People with Disabilities. SPECOM 2014; Lecture Notes in Computer Sciences; Springer: Cham, Switzerland, 2014; Volume 8773. [Google Scholar] [CrossRef]
- Tang, W.; Hu, T.; Hu, B.; Jin, C.; Wang, G.; Xie, C.; Chen, S.; Xu, J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020, 274, 1–7. [Google Scholar] [CrossRef]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychologicaleffects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef]
- World Health Organization. Advice on the Use of Masks in the Context of COVID-19. Available online: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (accessed on 5 June 2021).
- Recio-Barbero, M.; Herrero, M.S.; Segarra, R. Deafness and mental health: Clinical challenges during the COVID-19 pandemic. Psychol. Trauma 2020, 12, S212–S213. [Google Scholar] [CrossRef] [PubMed]
- Dirks, C.; Grünewald, D.; Young, P.; Heidbreder, A. Pilot study to investigate sleep disorders in the blind and persons with relevant visual impairment. Der Ophthalmol. 2019, 116, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; BaHammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.A.; Vitiello, M.V. Sleep problems during COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Alimoradi, Z.; Broström, A.; Tsang, H.W.; Griffiths, M.D.; Haghayegh, S.; Ohayon, M.M.; Pakpour, A.H. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. Lancet 2021, 36, 100916. [Google Scholar]
- Majd, N.R.; Broström, A.; Ulander, M.; Lin, C.Y.; Griffiths, M.D.; Imani, V.; Pakpour, A.H. Efficacy of a Theory-Based Cognitive Behavioral Technique App-Based Intervention for Patients With Insomnia: Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e1584. [Google Scholar]
- Hattie, J. Visible Learning: A Synthesis of over 800 Meta-Analyses Relating to Achievement; Routledge: London, UK, 2008. [Google Scholar]
- Halverson, R.; Smith, A. How new technologies have and have not changed teaching and learning in schools. J. Comput. Teach. Educ. 2009, 26, 49–54. [Google Scholar]
- Thai-Van, H.; Bakhos, D.; Bouccara, D.; Loundon, N.; Marx, M.; Mom, T.; Mosnier, I.; Roman, S.; Villerabel, C.; Vincent, C.; et al. Telemedicine in Audiology. Best practice recommendations from the French Society of Audiology (SFA) and the French Society of Otorhinolaryngology-Head and Neck Surgery (SFORL). Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2020. [Google Scholar] [CrossRef]
- US Food & Drug Admistration. Enforcement Policy for Face Masks, Barrier Face Coverings, Face Shields, Surgical Masks, and Respirators during the Coronavirus Disease (COVID-19) Public Health Emergency (Revised). Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enforcement-policy-face-masks-barrier-face-coverings-face-shields-surgical-masks-and-respirators (accessed on 21 September 2021).
- ANSI-American National Standards Institute. Available online: https://www.ansi.org/ (accessed on 21 September 2021).
- Bubbico, L.; Bellizzi, S.; Ferlito, S.; Cegolon, L. The role of social medicine in the COVID-19 pandemic era. J. Glob. Health 2021, 11, 03068. [Google Scholar] [CrossRef] [PubMed]
- European Commission. The Organisation of Resilient Health and Social Care Following the COVID-19 Pandemic. Available online: https://ec.europa.eu/health/sites/default/files/expert_panel/docs/026_health_socialcare_covid19_en.pdf (accessed on 16 August 2021).
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [PubMed]
| VARIABLES | STRATA | Total (n = 163) (Col %) | DISABILITY TYPE | Univariable Logistic Analysis | ||
|---|---|---|---|---|---|---|
| Hearing n = 109 (66.9%) | Visual n = 54 (33.1%) | OR (95%CI) | p Value | |||
| Sociodemographic Factors | ||||||
| Sex (Missing: 3) | Female | 90 (56.3) | 67 (62.6) | 23 (43.4) | reference | |
| Male | 70 (43.7) | 40 (37.4) | 30 (56.6) | 2.18 (1.12; 4.27) | 0.020 | |
| Age (years) 38.4 ± 20.2 | <23 | 41 (25.2) | 25 (22.9) | 16 (29.6) | reference | |
| 23–38 | 40 (24.5) | 29 (26.6) | 11 (20.4) | 0.59 (0.23; 1.51) | N.S. | |
| 39–53 | 38 (23.3) | 23 (21.1) | 15 (27.8) | 1.02 (0.41; 2.51) | N.S. | |
| 54+ | 44 (26.9) | 32 (29.4) | 12 (22.2) | 0.59 (0.24; 1.46) | N.S. | |
| Geographic area (Missing: 1) | Northern Italy | 97 (59.9) | 62 (56.9) | 35 (66.0) | reference | |
| Central Italy | 46 (28.4) | 35 (32.1) | 11 (20.8) | 0.56 (0.25; 1.23) | N.S. | |
| Southern Italy | 19 (11.7) | 12 (11.0) | 7 (13.2) | 1.03 (0.37; 2.07) | N.S. | |
| Occupational status (Missing: 5) | Unemployed | 11 (6.9) | 11 (10.4) | 0 | 1 | |
| Retired | 34 (21.4) | 20 (18.9) | 14 (26.9) | 1.12 (0.44; 2.87) | N.S. | |
| Student | 39 (24.5) | 24 (22.6) | 15 (28.1) | reference | N.S. | |
| Worker | 75 (47.2) | 51 (48.1) | 23 (44.2) | 0.72 (0.32; 1.62) | N.S. | |
| Who do you live with? (Missing: 18) | At least with one family member | 126 (86.9) | 86 (88.7) | 40 (83.3) | reference | |
| Alone | 17 (11.7) | 11 (11.3) | 6 (12.5) | 1.17 (0.41; 3.40) | N.S. | |
| in a care home | 2 (1.4) | 0 | 2 (4.2) | 1 | N.S. | |
| External open space available in your place (M: 18) | No | 33 (22.6) | 26 (26.8) | 7 (14.6) | reference | |
| Yes | 113 (77.4) | 71 (73.2) | 41 (85.4) | 2.14 (0.86; 5.38) | N.S. | |
| VARIABLES | STRATA | Total (n = 163) (Col %) | DISABILITY TYPE | Univariable Logistic Analysis | ||
|---|---|---|---|---|---|---|
| Hearing n = 109 (66.9%) | Visual n = 54 (33.1%) | OR (95%CI) | p Value | |||
| Health status and Lifestyle Habits | ||||||
| Recreational activities before the COVID-19 emergency (M: 20) | No | 35 (24.5) | 28 (29.2) | 7 (14.9) | reference | |
| Yes | 108 (75.5) | 68 (70.0) | 40 (85.1) | 2.35 (0.94; 5.87) | N.S. | |
| Recreational activities during the COVID-19 emergency (M: 39) | No | 79 (63.7) | 54 (67.5) | 25 (56.8) | reference | |
| Yes | 45 (36.3) | 26 (32.5) | 19 (43.2) | 1.58 (0.74; 3.37) | N.S. | |
| Everyday habits during lock down (M: 23) | I always dress as I should go out | 103 (73.6) | 69 (71.9) | 34 (77.3) | reference | |
| I always wear pajamas all day | 37 (26.4) | 27 (28.2) | 10 (22.7) | 0.75 (0.33; 1.73) | N.S. | |
| Sleeping habits during lock down (M: 19) | Regular schedule | 106 (73.6) | 68 (70.0) | 38 (79.2) | reference | |
| Whenever I wish | 38 (26.4) | 28 (29.2) | 10 (20.8) | 0.64 (0.28; 1.46) | N.S. | |
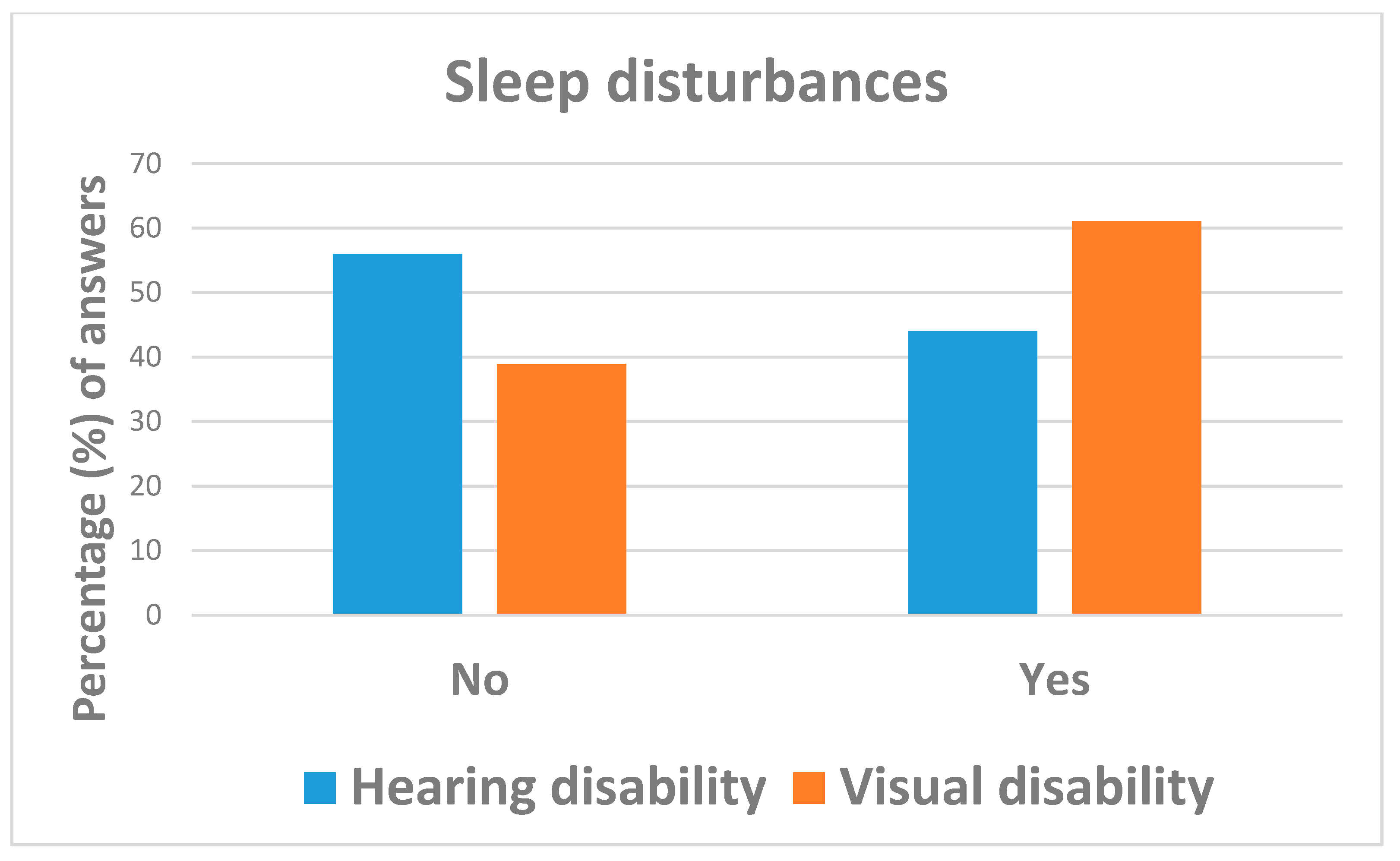
| Sleep disorders during lock down (M: 2) | No | 82 (50.3) | 61 (56.0) | 21 (38.9) | reference | |
| Yes | 81 (49.7) | 48 (44.0) | 33 (61.1) | 2.00 (1.03; 3.88) | 0.042 | |
| Eating habits during lock down (M: 21) | Regular schedule | 122 (85.9) | 81 (85.3) | 41 (87.2) | reference | |
| Whenever I wish | 20 (14.1) | 14 (14.7) | 6 (12.8) | 0.85 (0.30; 2.37) | N.S. | |
| BMI (kg/m2) (M: 9) | <25 | 106 (68.8) | 72 (71.3) | 34 (64.2) | reference | |
| 25+ | 48 (31.2) | 29 (28.7) | 19 (35.1) | 1.38 (0.68; 2.82) | N.S. | |
| Increase in body weight during lock down | No | 90 (55.2) | 61 (56.0) | 29 (53.7) | reference | |
| Yes | 73 (44.8) | 48 (44.0) | 25 (46.3) | 1.10 (0.57; 2.11) | N.S. | |
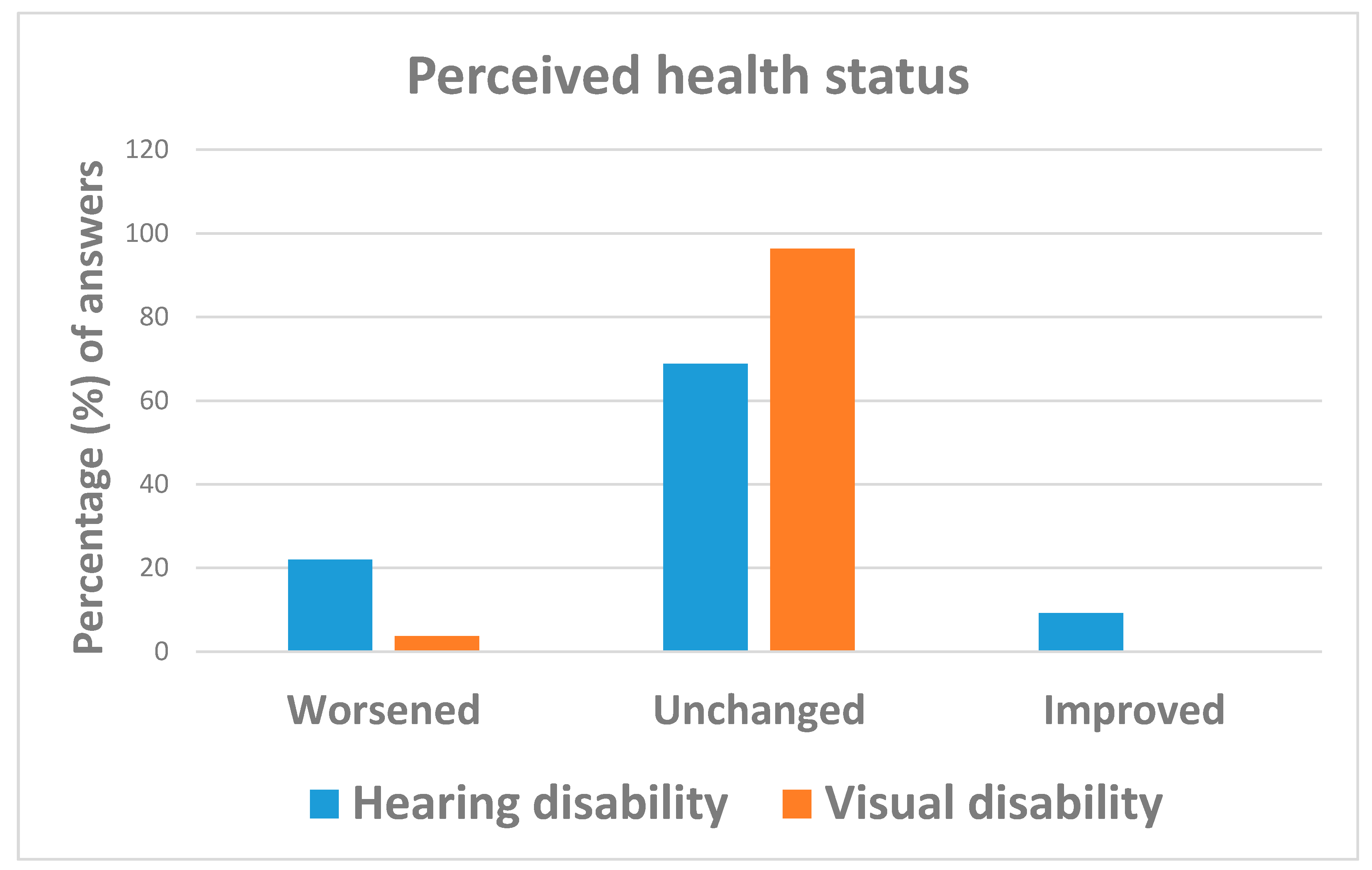
| How has your perceived health state changed as compared to before the COVID-19 emergency? | Improved | 10 (6.1) | 10 (9.2) | 0 | 1 | |
| Unchanged | 127 (77.9) | 75 (68.8) | 52 (96.3) | reference | N.S. | |
| Worsened | 26 (16.0) | 24 (22.0) | 2 (3.7) | 0.12 (0.03; 0.53) | 0.005 | |
| Keeping in contact with friends/family through remote modern technology during lock-down? (M:3) | More than before | 61 (38.1) | 46 (42.2) | 15 (29.4) | reference | |
| As before | 82 (51.3) | 56 (51.4) | 26 (51.0) | 1.42 (0.68; 3.00) | N.S. | |
| Less than before | 17 (10.6) | 7 (6.4) | 10 (19.6) | 4.38 (1.42; 13.54) | 0.010 | |
| How do you rate your family relationships during lock-down? (M: 18) | Improved | 29 (20.0) | 21 (21.7) | 8 (16.7) | reference | |
| Unchanged | 95 (65.5) | 66 (68.0) | 29 (60.4) | 1.14 (0.45; 2.86) | N.S. | |
| Worsened | 11 (7.6) | 5 (5.2) | 6 (12.5) | 3.15 (0.75; 13.29) | N.S. | |
| Do not know | 10 (6.9) | 5 (5.2) | 5 (10.4) | 2.63 (0.60; 11.57) | N.S. | |
| VARIABLES | STRATA | Total (n = 163) (Col %) | DISABILITY TYPE | Univariable Logistic Analysis | ||
|---|---|---|---|---|---|---|
| Hearing n = 109 (66.9%) | Visual n = 54 (33.1%) | OR (95%CI) | p Value | |||
| Analysis restricted to students (n = 39) | ||||||
| School activities ongoing during the COVID-19 emergency | No | 6 (15.4) | 3 (12.5) | 3 (20.0) | reference | |
| Yes | 33 (84.6) | 21 (87.5) | 12 (80.0) | 1.49 (0.59; 3.72) | N.S. | |
| Support teacher available before the COVID-19 emergency (M: 1) | No | 12 (31.6) | 11 (47.8) | 1 (6.7) | reference | |
| Yes | 26 (68.4) | 12 (52.2) | 1 (93.3) | 7.37 (1.43; 38.08) | 0.022 | |
| Support teacher interrupted during the COVID-19 emergency (M: 1) | No | 15 (48.4) | 8 (53.3) | 7 (43.8) | reference | |
| Yes | 16 (52.6) | 7 (46.7) | 9 (56.3) | 1.47 (0.36; 6.05) | N.S. | |
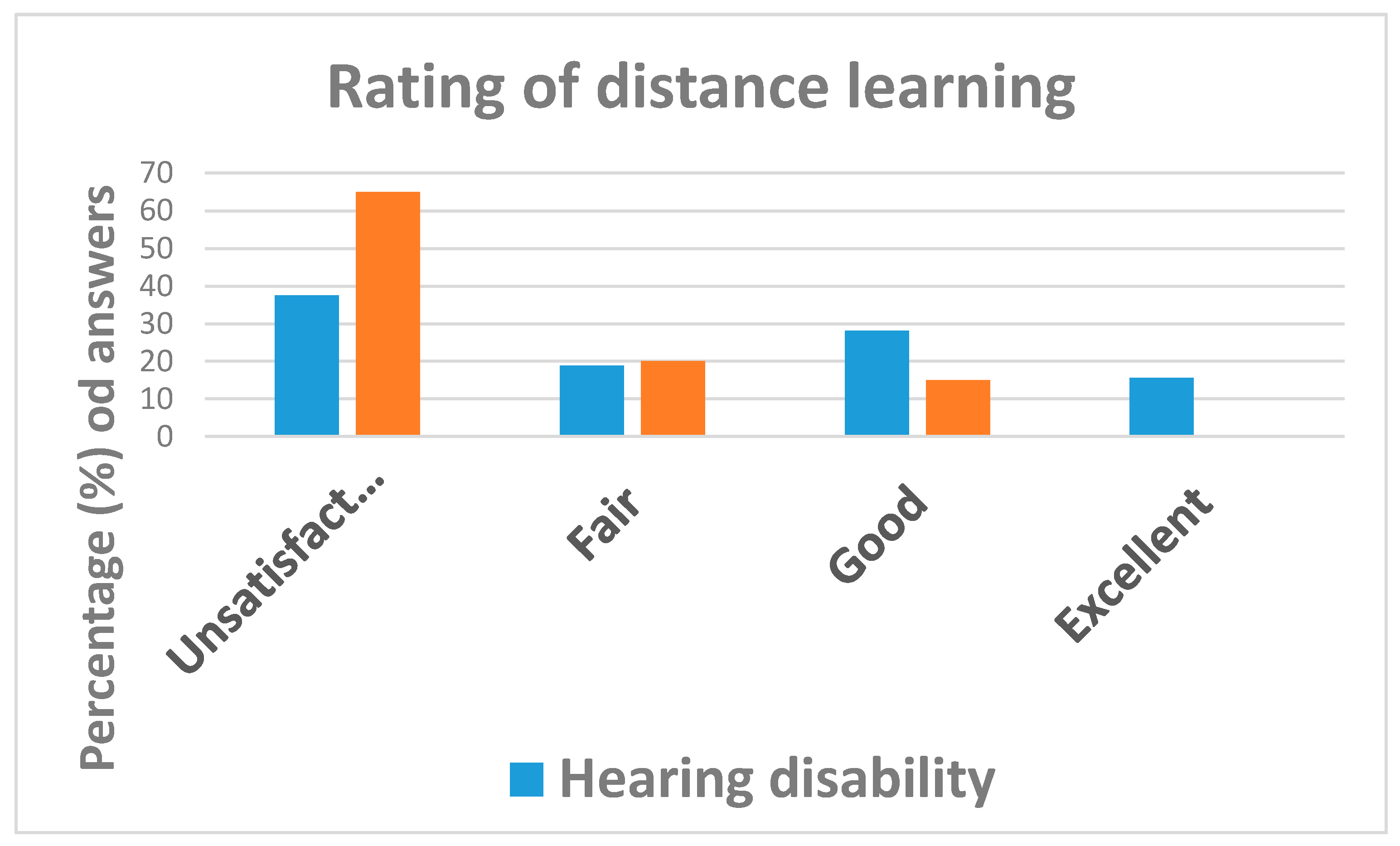
| How do you consider | Excellent | 5 (12.8) | 5 (15.6) | 0 | 1 | |
| distance learning for | Good | 8 (20.5) | 9 (28.1) | 3 (15.0) | 0.31 (0.07; 1.41) | N.S. |
| your disability? | Fair | 9 (23.1) | 6 (18.8) | 4 (20.0) | 0.62 (0.14; 2.73) | N.S. |
| Unsatisfactory | 17 (43.6) | 12 (37.5) | 13 (65.0) | reference | ||
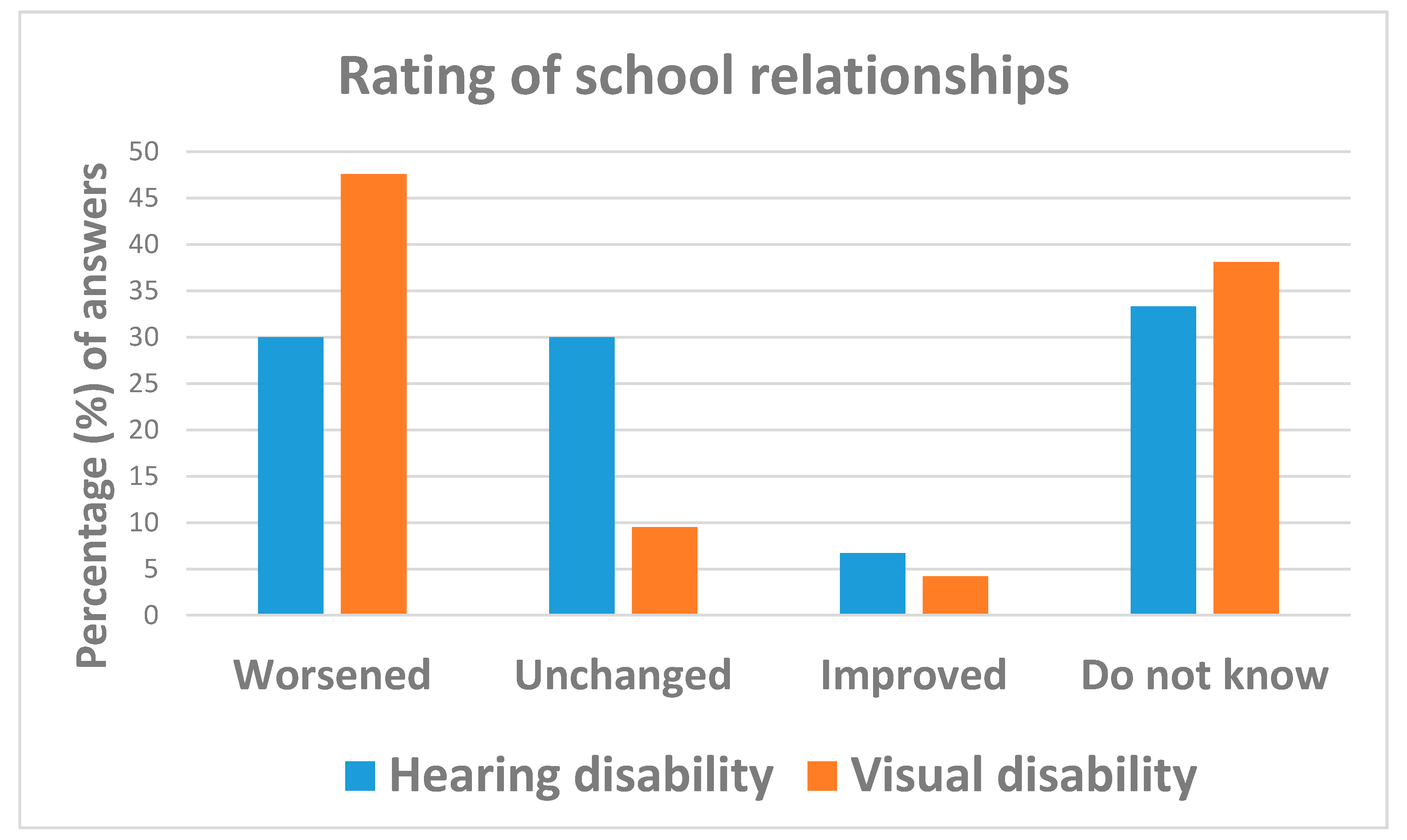
| How do you rate your current school relationships as compared to before the COVID-19 emergency? | Improved | 3 (5.9) | 2 (6.7) | 1 (4.2) | reference | |
| Unchanged | 11 (21.6) | 9 (30.0) | 2 (9.5) | 0.44 (0.03; 7.67) | N.S. | |
| Worsened | 19 (37.3) | 9 (30.0) | 10 (47.6) | 2.22 (0.17; 28.86) | N.S. | |
| Do not Know | 18 (35.3) | 10 (33.3) | 8 (38.1) | 1.60 (0.12; 20.99) | N.S. | |
| Analysis restricted to workers (n=74) | ||||||
| Have you continued your job during the COVID-19 emergency? (M: 2) | No | 11 (15.3) | 6 (11.8) | 5 (23.8) | reference | |
| Yes | 61 (84.7) | 45 (88.2) | 16 (76.2) | 0.42 (0.11; 1.59) | N.S. | |
| Remote-working facilitated by the employer duringthe COVID-19 emergency (M: 2) | No | 23 (33.3) | 17 (33.3) | 7 (33.3) | reference | |
| Yes | 46 (66.7) | 32 (66.7) | 14 (66.7) | 1.00 (0.34; 2.97) | N.S. | |
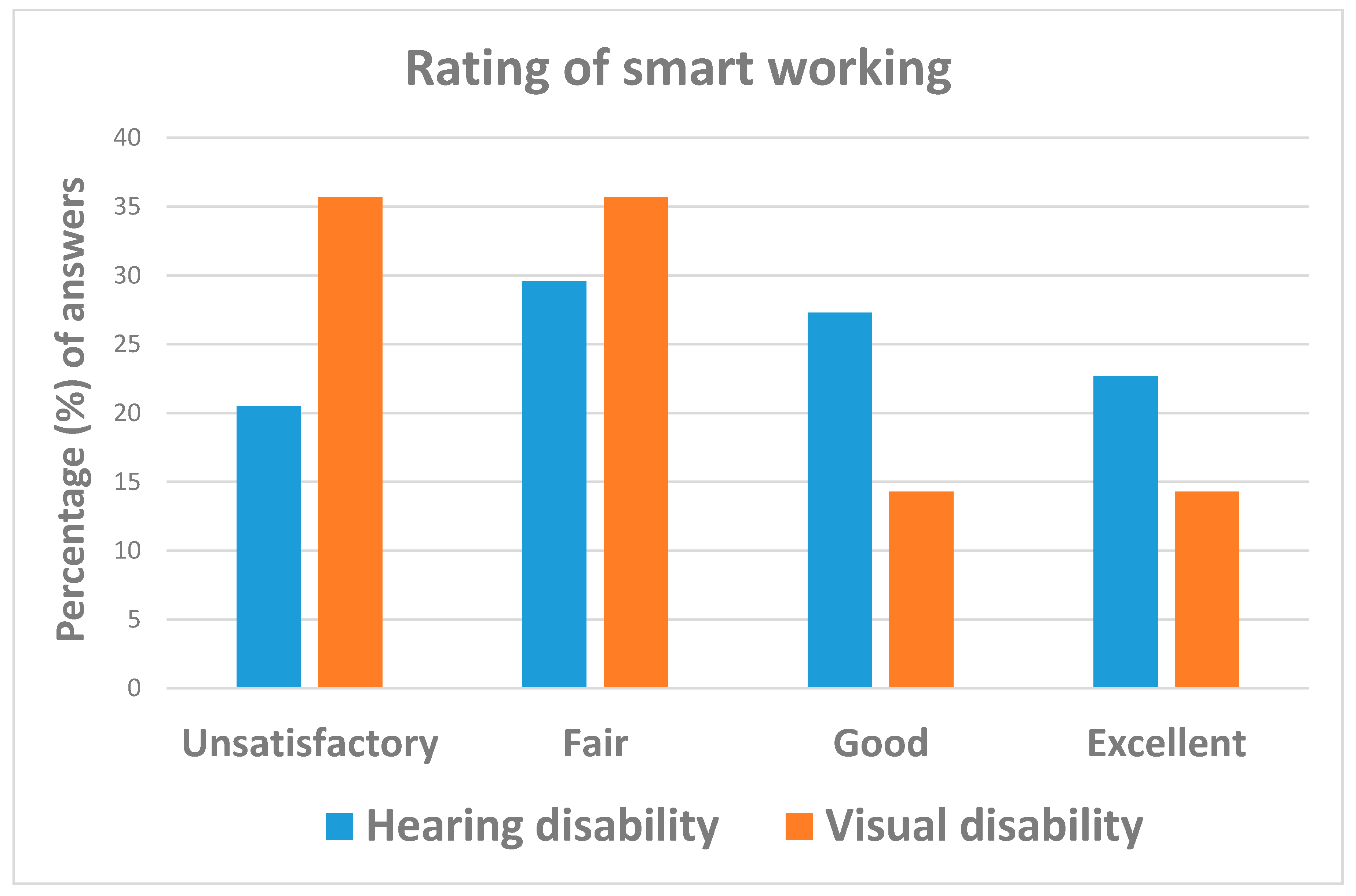
| How do you rate remote working? (M: 18) | Excellent | 13 (23.3) | 8 (19.1) | 5 (35.7) | reference | |
| Good | 18 (32.1) | 13 (31.0) | 5 (35.7) | 0.62 (0.13; 2.82) | N.S. | |
| Fair | 14 (25.0) | 12 (28.6) | 2 (14.3) | 0.27 (0.04; 1.73) | N.S. | |
| Unsatisfactory | 11 (19.6) | 9 (22.4) | 2 (14.3) | 0.36 (0.05; 2.37) | N.S. | |
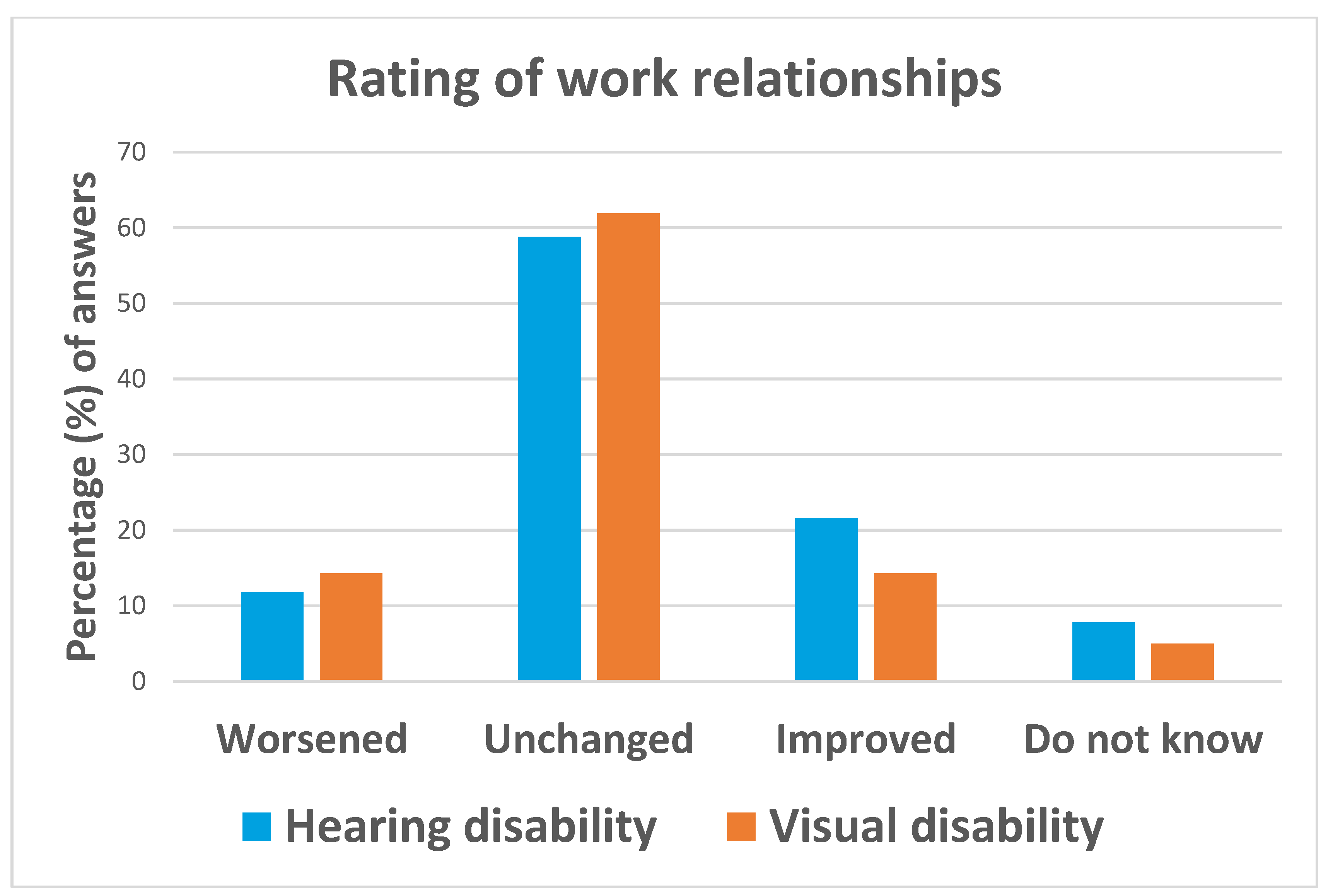
| How do you rate your relationships with colleagues as compared to before the COVID-19 emergency? (M: 5) | Improved | 9 (12.5) | 6 (11.8) | 3 (14.3) | reference | |
| Unchanged | 43 (59.7) | 30 (58.8) | 13 (61.9) | 0.87 (0.19; 4.01) | N.S. | |
| Worsened | 14 (19.4) | 11 (21.6) | 3 (14.3) | 0.55 (0.08; 3.59) | N.S. | |
| Not answered | 6 (8.3) | 4 (7.8) | 2 (5.00) | 1.00 (0.11; 8.95) | N.S. | |
| VARIABLES | STRATA | Total (n = 163) (Col %) | DISABILITY TYPE | Univariable Logistic Analysis | ||
|---|---|---|---|---|---|---|
| Hearing n = 109 (66.9%) | Visual n = 54 (33.1%) | OR (95%CI) | p Value | |||
| Access to health and social care services | ||||||
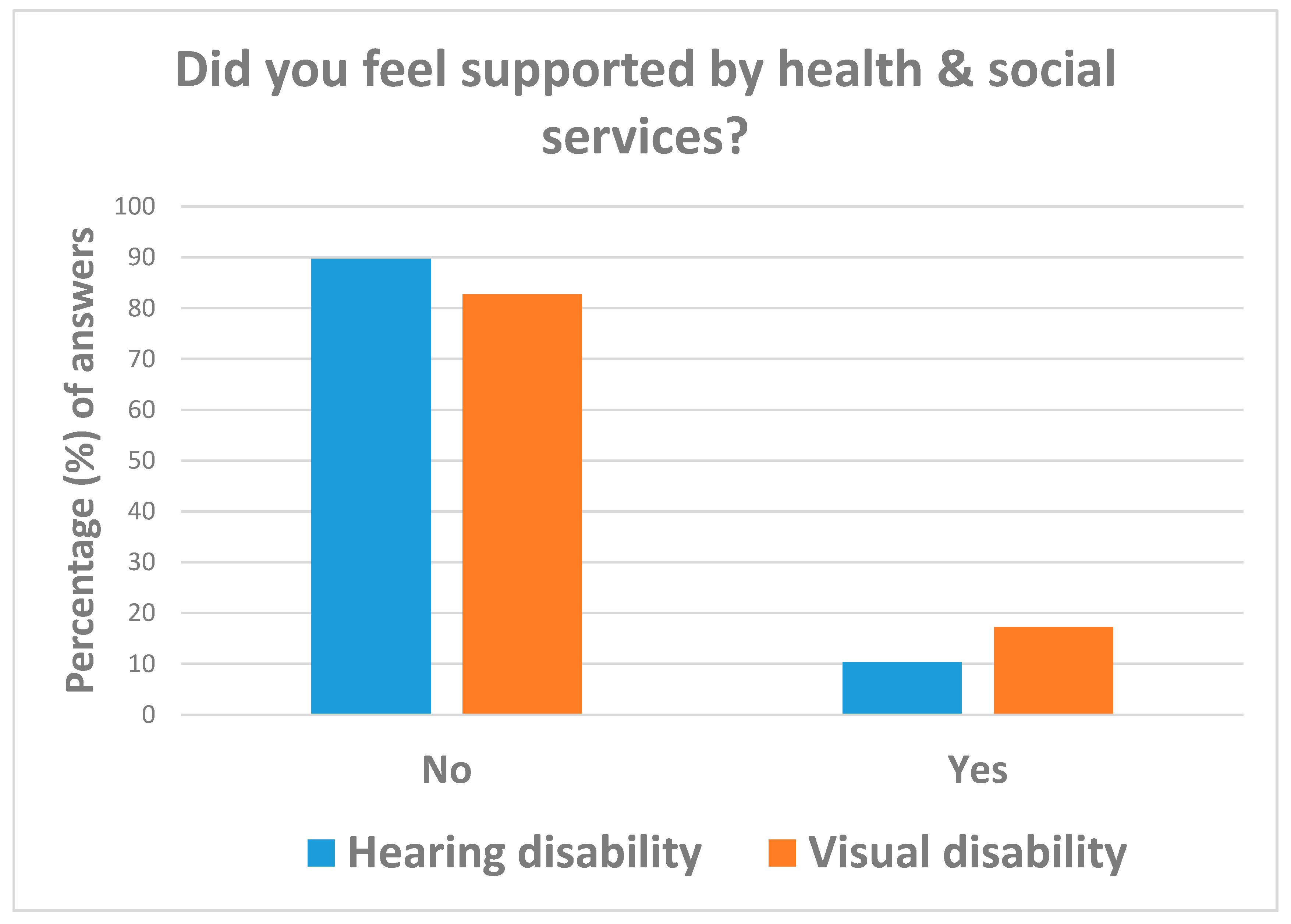
| Did you feel supported by health & social services during the COVID-19 emergency? (M: 14) | No | 130 (87.3) | 87 (89.7) | 43 (82.7) | reference | |
| Yes | 19 (12.8) | 10 (10.3) | 9 (17.3) | 1.82 (0.69; 4.81) | N.S | |
| Rehabilitation programs before the COVID-19 emergency (M: 46) | No | 79 (67.5) | 58 (7.3) | 21 (51.2) | reference | |
| Yes | 38 (32.5) | 18 (23.7) | 20 (48.8) | 3.06 (1.37; 6.89) | 0.007 | |
| Rehabilitation programs during the COVID-19 emergency (M: 82) | No | 23 (60.5) | 9 (50.0) | 14 (70.0) | reference | |
| Yes | 15 (39.5) | 9 (50.0) | 6 (30.0) | 0.12 (0.02; 0.68) | 0.017 | |
| Remote rehabilitation during COVID-19 emergency | No | 4 (21.1) | 1 (25.0) | 3 (75.0) | reference | |
| Yes | 15 (79.0) | 11 (73.3) | 4 (67.7) | 0.35 (0.02; 1.37) | N.S. | |
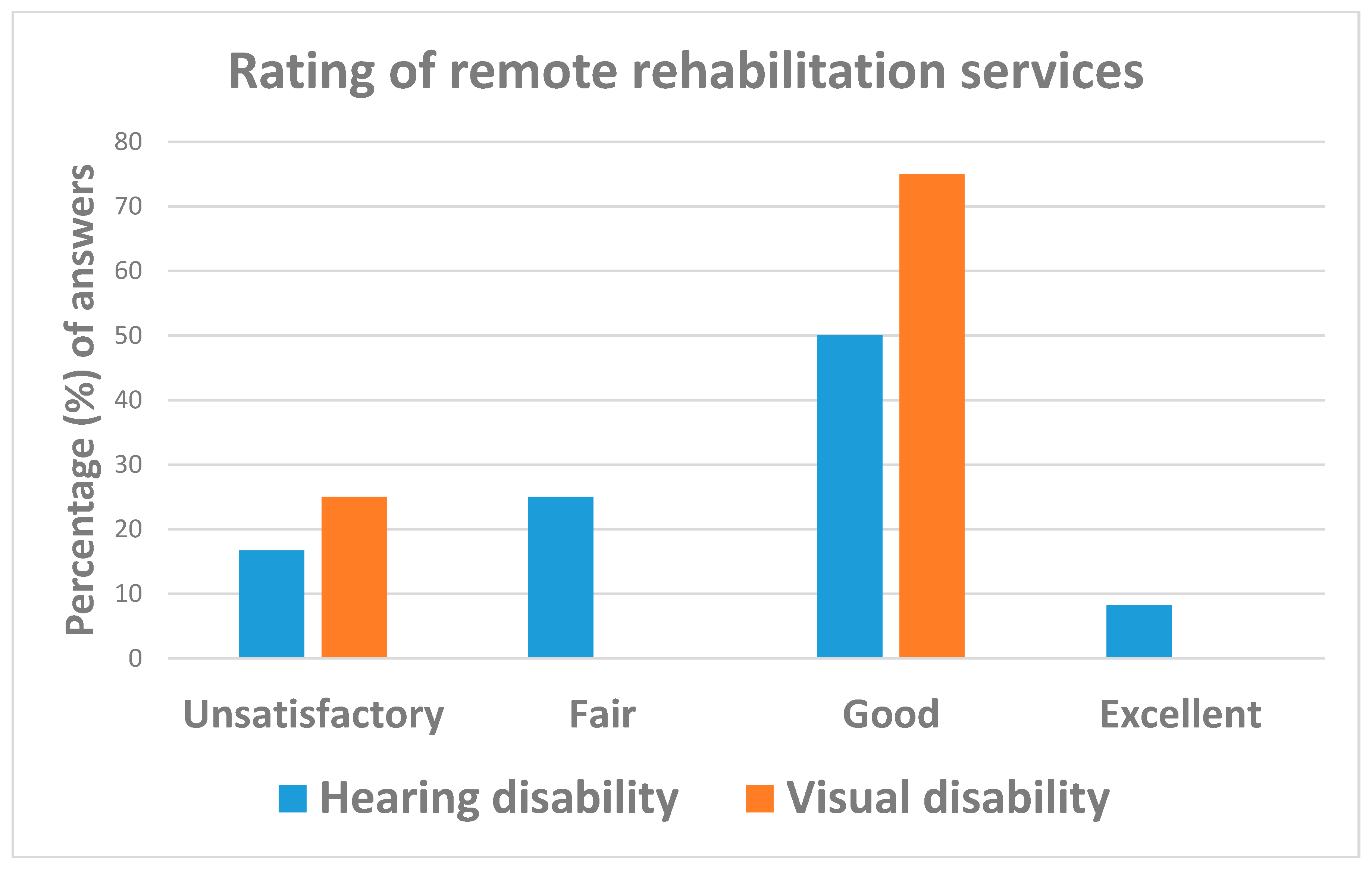
| If you are following remote rehabilitation during the COVID-19 emergency, how do you rate these distance services? | Excellent | 1 (6.3) | 1 (8.3) | 0 | NA | N.S. |
| Good | 9 (56.3) | 6 (50.0) | 3 (75.0) | reference | ||
| Fair | 3 (18.8) | 3 (25.0) | 0 | NA | N.S. | |
| Unsatisfactory | 3 (18.8) | 2 (16.7) | 1 (25.0) | 1.41 (0.06; 15.99) | N.S. | |
| Emotional impact of COVID-19 pandemic | ||||||
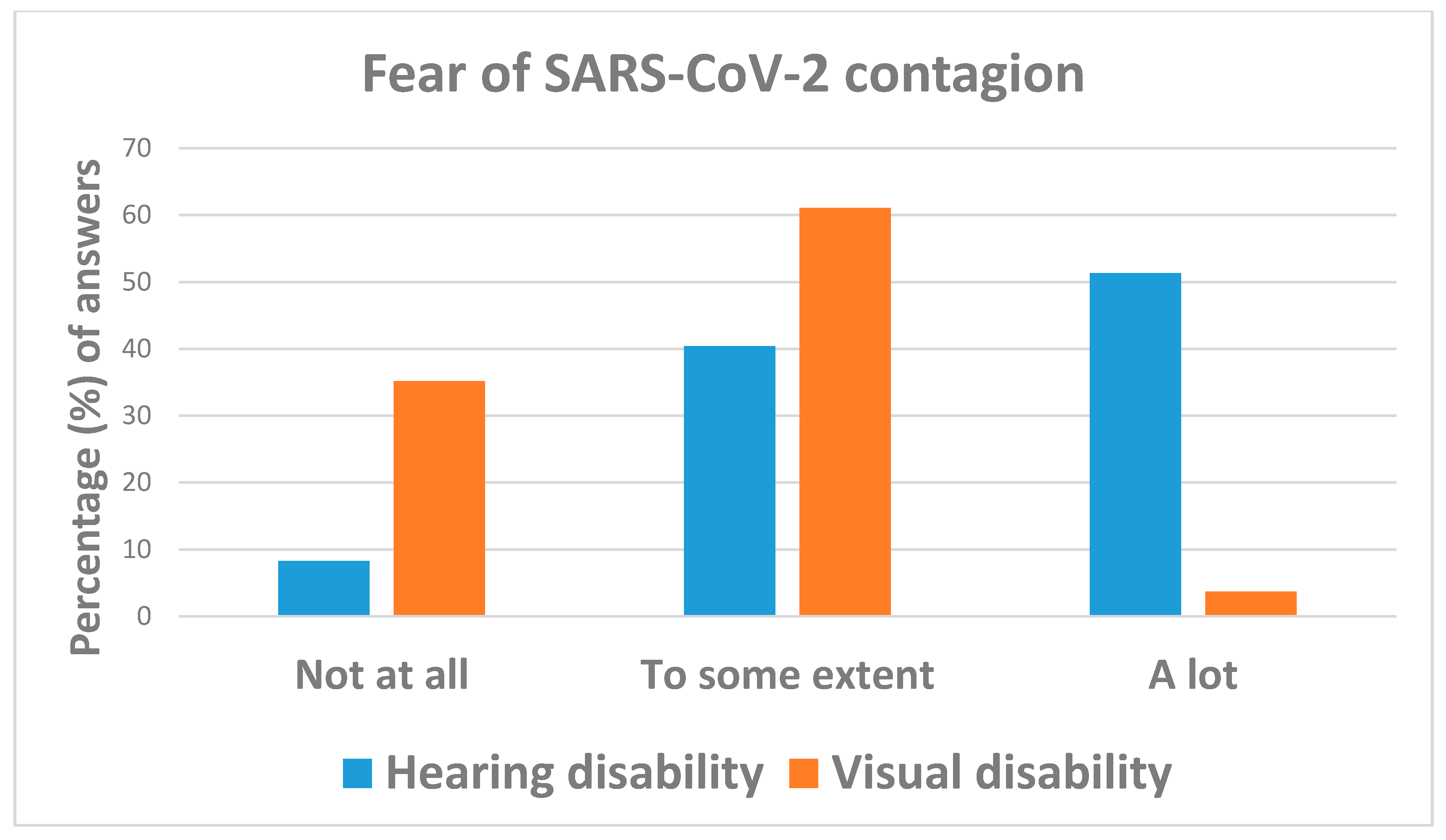
| Are you worried about the risk of SARS-CoV-2 contagion and hospitalization? (M: 2) | Not at all | 28 (17.2) | 9 (8.3) | 19 (35.2) | reference | |
| To some extent | 77 (47.2) | 44 (40.4) | 33 (61.1) | 0.36 (0.14; 0.88) | 0.026 | |
| A lot | 58 (35.6) | 56 (51.4) | 2 (3.7) | 0.02 (0.00; 0.08) | <0.001 | |
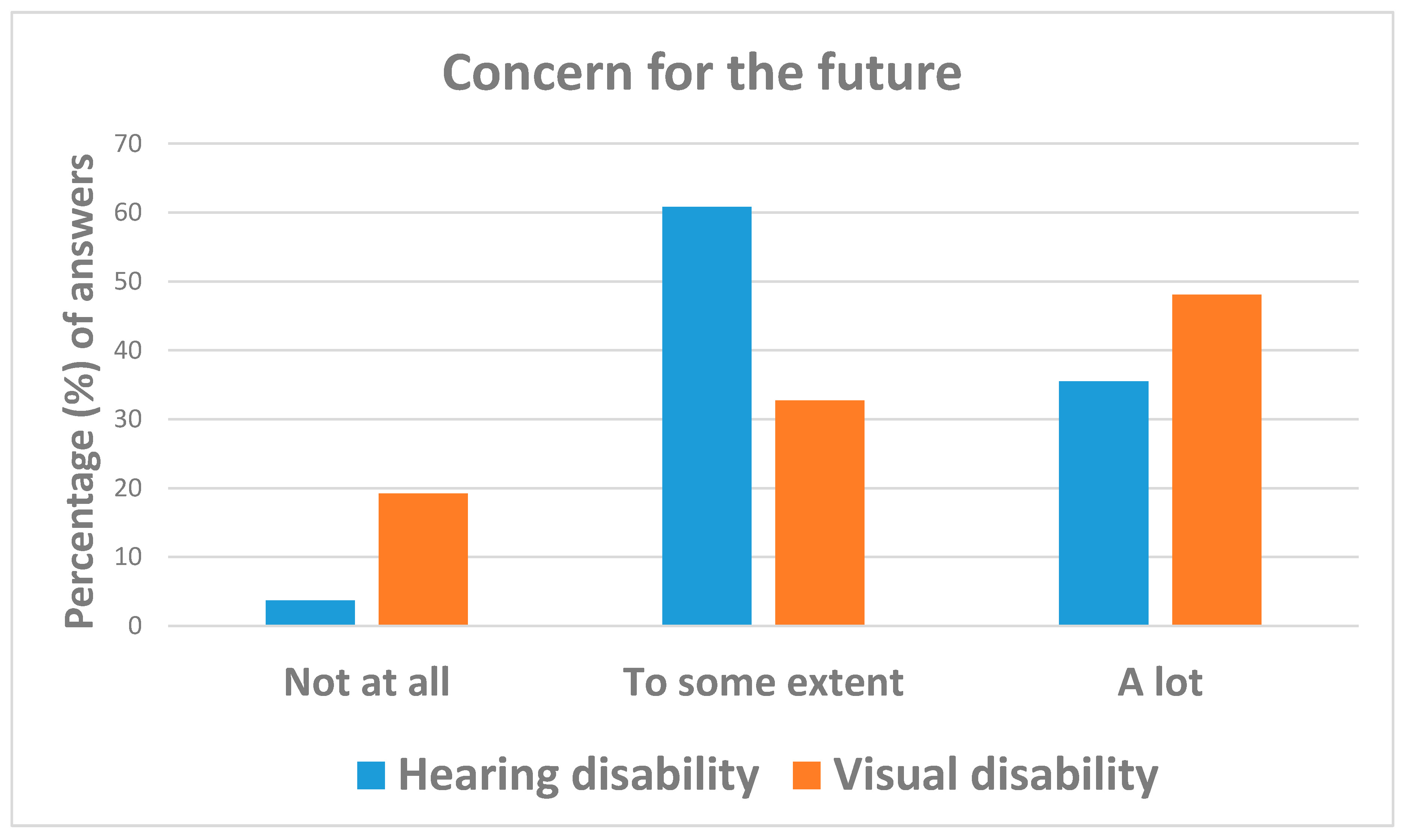
| Are you worried about the future? (M: 4) | Not at all | 14 (8.8) | 4 (3.7) | 10 (19.2) | reference | |
| To some extent | 82 (51.6) | 65 (60.8) | 17 (32.7) | 0.10 (0.03; 0.37) | 0.001 | |
| A lot | 63 (39.6) | 38 (35.5) | 25 (48.1) | 0.26 (0.07; 0.93) | 0.039 | |
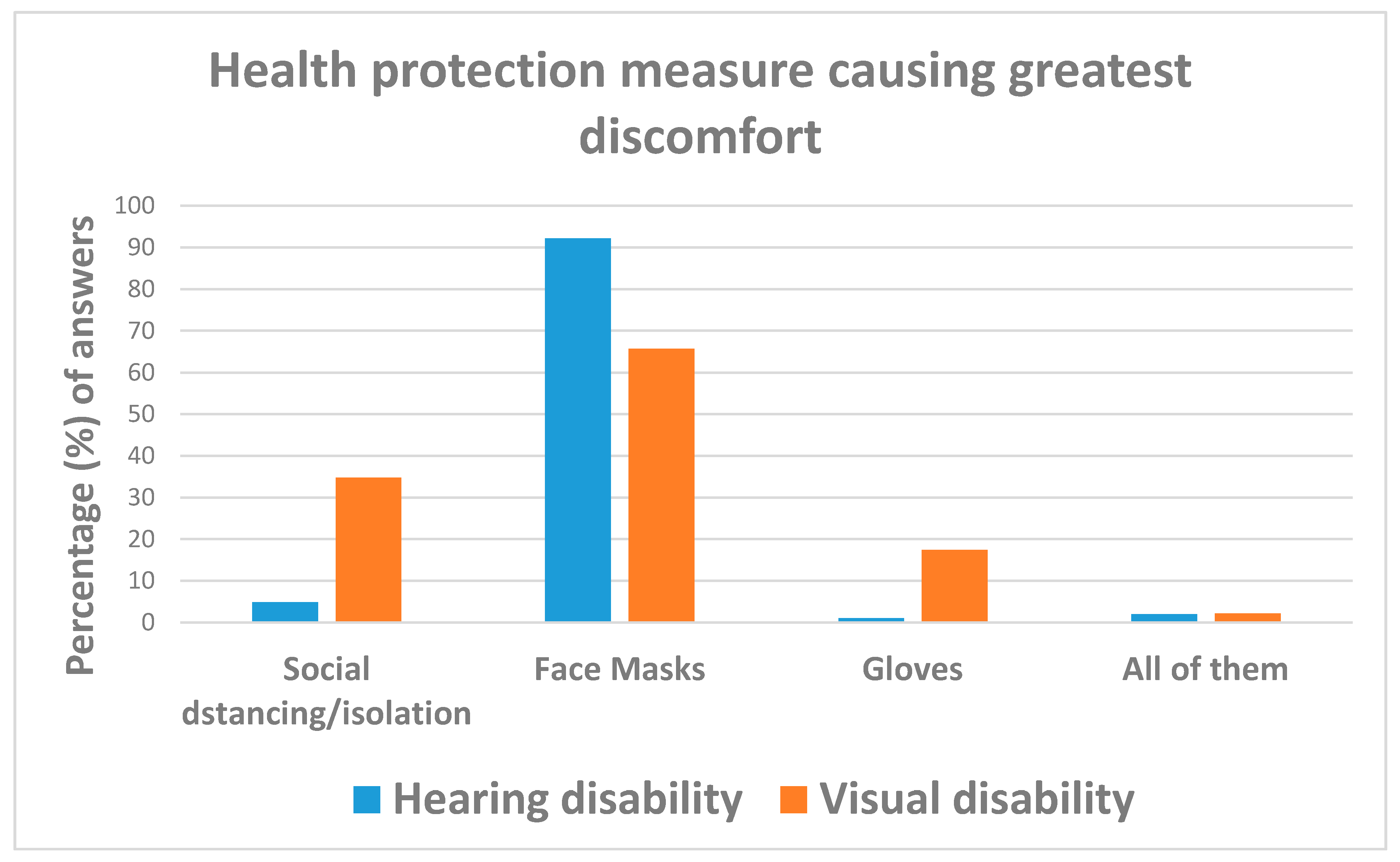
| Which health protection measure caused the greatest discomfort to you? (Total free answers: 149) (M: 15) | Social distancing/isolation | 21 (14.1) | 5 (4.9) | 16 (34.8) | reference | |
| Face masks | 115 (77.7) | 94 (92.2) | 21 (45.7) | 0.07 (0.02; 0.21) | <0.001 | |
| Gloves | 9 (6.1) | 1 (1.0) | 8 (17.4) | 2.50 (025; 25.15) | N.S. | |
| All of them | 3 (2.0) | 2 (2.0) | 1 (2.2) | 0.16 (0.01; 2.11) | N.S. | |
| Solutions proposed to improve quality of life of sensorineural disabled in the COVID-19 emergency (Total free answers: 114) (M: 49) | Improving access/delivery of health care and social services to disabled | 22 (19.3) | 10 (13.0) | 12 (32.4) | reference | |
| Use of transparent masks | 20 (17.5) | 18 (23.4) | 2 (5.4) | 0.09 (0.02; 0.50) | 0.006 | |
| Mitigating social restrictions | 21 (18.4) | 13 (16.9) | 8 (21.6) | 0.51 (0.15; 1.73) | N.S. | |
| Better information/communications on COVID-19 | 19 (16.7) | 13 (16.9) | 6 (16.2) | 0.38 (0.11; 1.38) | N.S. | |
| Better security control (n = 6) | 20 (17.5) | 15 (19.5) | 5 (13.5) | 0.28 (0.07; 1.03) | 0.056 | |
| More awareness on disabilities (n = 8) | ||||||
| Other (n = 6) | ||||||
| Do not know | 12 (10.5) | 8 (10.4) | 4 (10.8) | 0.42 (0.10; 1.80) | N.S. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bubbico, L.; Bellizzi, S.; Ferlito, S.; Maniaci, A.; Leone Guglielmotti, R.; Antonelli, G.; Mastrangelo, G.; Cegolon, L. The Impact of COVID-19 on Individuals with Hearing and Visual Disabilities during the First Pandemic Wave in Italy. Int. J. Environ. Res. Public Health 2021, 18, 10208. https://doi.org/10.3390/ijerph181910208
Bubbico L, Bellizzi S, Ferlito S, Maniaci A, Leone Guglielmotti R, Antonelli G, Mastrangelo G, Cegolon L. The Impact of COVID-19 on Individuals with Hearing and Visual Disabilities during the First Pandemic Wave in Italy. International Journal of Environmental Research and Public Health. 2021; 18(19):10208. https://doi.org/10.3390/ijerph181910208
Chicago/Turabian StyleBubbico, Luciano, Saverio Bellizzi, Salvatore Ferlito, Antonino Maniaci, Raffaella Leone Guglielmotti, Giulio Antonelli, Giuseppe Mastrangelo, and Luca Cegolon. 2021. "The Impact of COVID-19 on Individuals with Hearing and Visual Disabilities during the First Pandemic Wave in Italy" International Journal of Environmental Research and Public Health 18, no. 19: 10208. https://doi.org/10.3390/ijerph181910208
APA StyleBubbico, L., Bellizzi, S., Ferlito, S., Maniaci, A., Leone Guglielmotti, R., Antonelli, G., Mastrangelo, G., & Cegolon, L. (2021). The Impact of COVID-19 on Individuals with Hearing and Visual Disabilities during the First Pandemic Wave in Italy. International Journal of Environmental Research and Public Health, 18(19), 10208. https://doi.org/10.3390/ijerph181910208










