Measurement Invariance of Perfectionism Measures in Students with and without a History of Non-Suicidal Self-Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Inventory of Statements about Self-Injury
2.2.2. Frost Multidimensional Perfectionism Scale-Brief
2.2.3. Clinical Perfectionism Questionnaire
2.3. Data Analysis
3. Results
3.1. Frost Multidimensional Perfectionism Scale—Brief
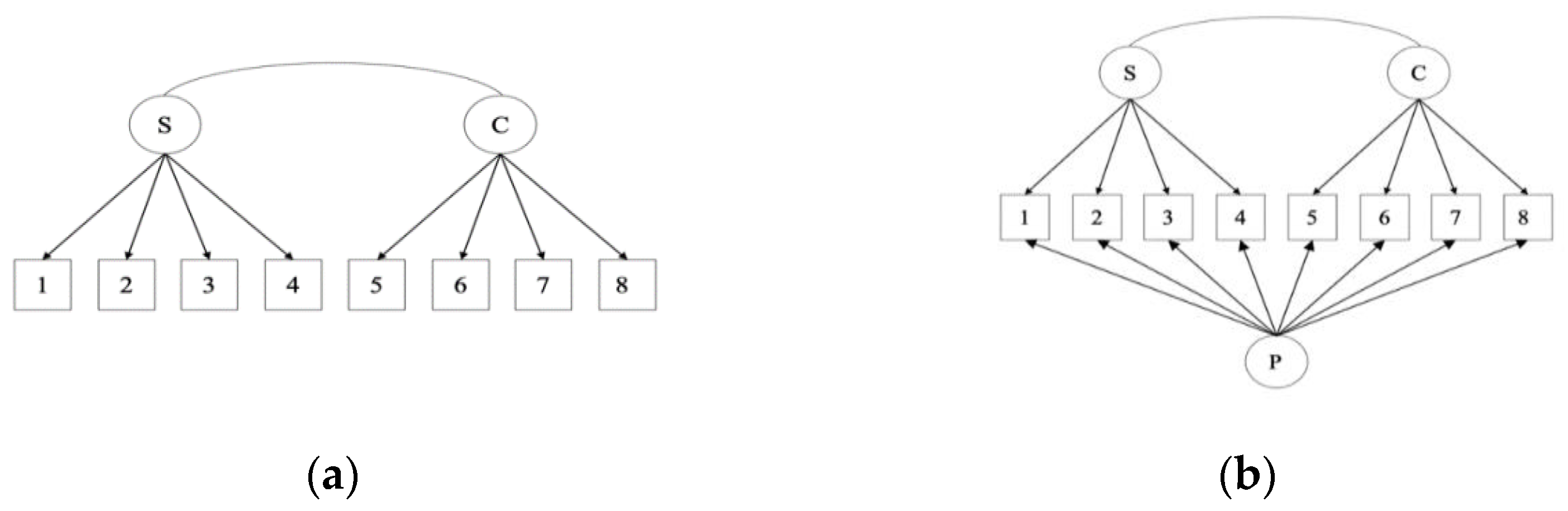
3.1.1. Two-Factor Solution
3.1.2. Bifactor Solution
3.2. Clinical Perfectionism Questionnaire
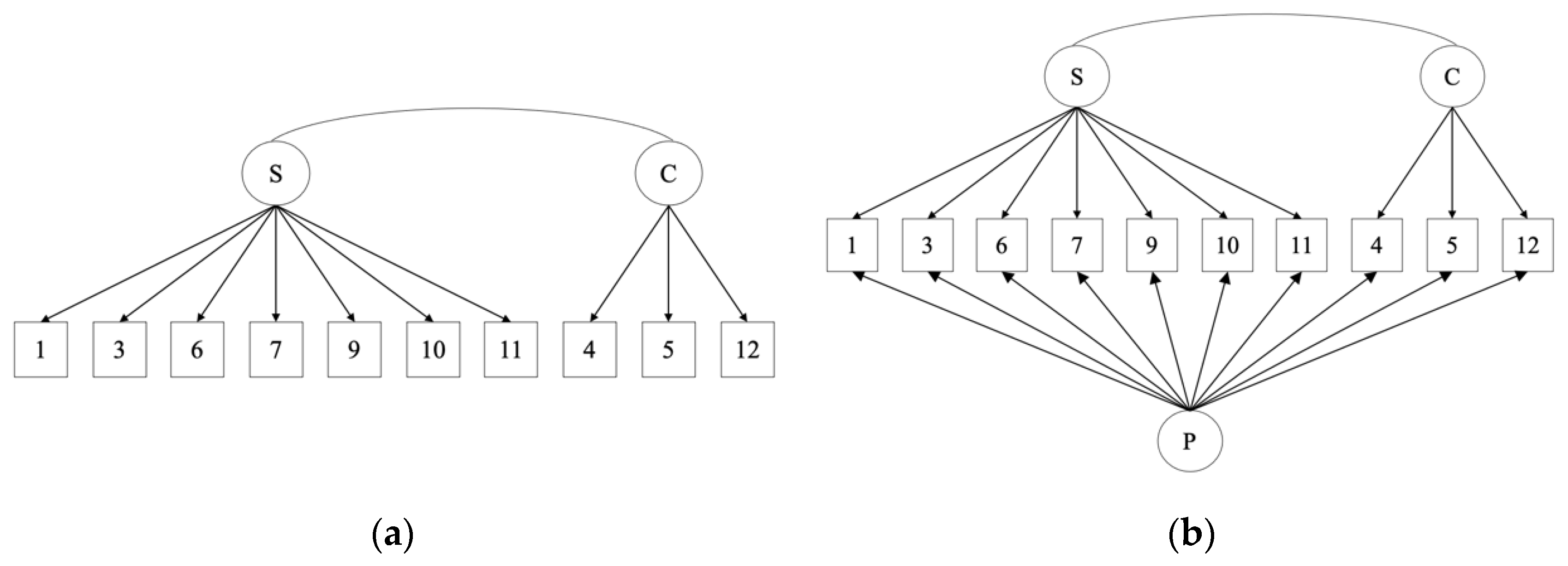
3.2.1. Two-Factor Solution
3.2.2. Bifactor Solution
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organisation. Suicide Worldwide in 2019: Global Health Estimates; World Health Organisation: Geneva, Switzerland, 2021. [Google Scholar]
- Maple, M.; Sanford, R.; Pirkis, J.; Reavley, N.; Nicholas, A. Exposure to suicide in Australia: A representative random digit dial study. J. Affect. Disord. 2019, 259, 221–227. [Google Scholar] [CrossRef]
- International Society for the Study of Self-Injury. What is Self-Injury? Available online: https://itriples.org/category/about-self-injury/ (accessed on 11 June 2021).
- Victor, S.E.; Klonsky, E.D. Correlates of suicide attempts among self-injurers: A meta-analysis. Clin. Psychol. Rev. 2014, 34, 282–297. [Google Scholar] [CrossRef] [PubMed]
- Pompili, M.; Baldessarini, R.J. Risk of suicide and all-cause mortality after self-harm. Lancet Psychiatry 2015, 2, 769–770. [Google Scholar] [CrossRef]
- American Psychiatric Association. Conditions for further study. In Diagnostic and Statistical Manual of Mental Disorders (DSM-5); American Psychiatric Association: Arlington, TX, USA, 2013. [Google Scholar]
- Hawton, K.; Casey, D.; Bale, E.; Ryall, J.; Brand, F.; Geulayov, G. Self-Harm in Oxford. 2014. Available online: https://www.psych.ox.ac.uk/research/csr (accessed on 8 September 2021).
- Geulayov, G.; Kapur, N.; Turnbull, P.; Clements, C.; Waters, K.; Ness, J.; Townsend, E.; Hawton, K. Epidemiology and trends in non-fatal self-harm in three centres in England, 2000–2012: Findings from the Multicentre Study of Self-harm in England. BMJ Open 2016, 6, e010538. [Google Scholar] [CrossRef]
- Ostertag, L.; Golay, P.; Dorogi, Y.; Brovelli, S.; Bertran, M.; Cromec, I.; Van Der Vaeren, B.; Khan, R.; Costanza, A.; Wyss, K.; et al. The implementation and first insights of the French-speaking Swiss programme for monitoring self-harm. Swiss Med. Wkly. 2019, 149, w20016. [Google Scholar] [CrossRef] [Green Version]
- Swannell, S.V.; Martin, G.E.; Page, A.; Hasking, P.; St John, N.J. Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide Life-Threat. Behav. 2014, 44, 273–303. [Google Scholar] [CrossRef]
- Baertschi, M.; Costanza, A.; Canuto, A.; Weber, K. The function of personality in suicidal ideation from the perspective of the Interpersonal-Psychological Theory of Suicide. Int. J. Environ. Res. Public Health 2018, 15, 636. [Google Scholar] [CrossRef] [Green Version]
- Kiekens, G.; Bruffaerts, R.; Nock, M.K.; Van de Ven, M.; Witteman, C.; Mortier, P.; Demyttenaere, K.; Claes, L. Non-suicidal self-injury among Dutch and Belgian adolescents: Personality, stress and coping. Eur. Psychiatry 2015, 30, 743–749. [Google Scholar] [CrossRef]
- Goddard, A.; Hasking, P.; Claes, L.; McEvoy, P. Big five personality clusters in relation to non-suicidal self-injury. Arch. Suicide Res. 2021, 25, 390–405. [Google Scholar] [CrossRef]
- Smith, M.M.; Sherry, S.B.; Chen, S.; Saklofske, D.H.; Mushquash, C.; Flett, G.L.; Hewitt, P.L. The perniciousness of perfectionism: A meta-analytic review of the perfectionism–suicide relationship. J. Personal. 2018, 86, 522–542. [Google Scholar] [CrossRef]
- Zeifman, R.J.; Antony, M.M.; Kuo, J.R. When being imperfect just won’t do: Exploring the relationship between perfectionism, emotion dysregulation, and suicidal ideation. Personal. Individ. Differ. 2020, 152, 109612. [Google Scholar] [CrossRef]
- Gyori, D.; Balazs, J. Nonsuicidal self-injury and perfectionism: A systematic review. Front. Psychiatry 2021, 12. [Google Scholar] [CrossRef]
- Limburg, K.; Watson, H.J.; Hagger, M.S.; Egan, S.J. The relationship between perfectionism and psychopathology: A meta-analysis. J. Clin. Psychol. 2017, 73, 1301–1326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egan, S.J.; Wade, T.D.; Shafran, R. Perfectionism as a transdiagnostic process: A clinical review. Clin. Psychol. Rev. 2011, 31, 203–212. [Google Scholar] [CrossRef]
- Luyckx, K.; Gandhi, A.; Bijttebier, P.; Claes, L. Non-suicidal self-injury in female adolescents and psychiatric patients: A replication and extension of the role of identity formation. Personal. Individ. Differ. 2015, 77, 91–96. [Google Scholar] [CrossRef]
- Hoff, E.R.; Muehlenkamp, J.J. Nonsuicidal self-injury in college students: The role of perfectionism and rumination. Suicide Life-Threat. Behav. 2009, 39, 576–587. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.M.; Frost, R.O.; DiBartolo, P.M. Development and validation of the Frost Multidimensional Perfectionism Scale–Brief. J. Psychoeduc. Assess. 2016, 34, 620–633. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. The Clinical Perfectionism Questionnaire. 2003; Unpublished scale. [Google Scholar]
- Woodfin, V.; Binder, P.-E.; Molde, H. The psychometric properties of the Frost Multidimensional Perfectionism Scale—Brief. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef]
- Stoeber, J.; Damian, L.E. The Clinical Perfectionism Questionnaire: Further evidence for two factors capturing perfectionistic strivings and concerns. Personal. Individ. Differ. 2014, 61–62, 38–42. [Google Scholar] [CrossRef]
- Howell, J.; Anderson, R.; Egan, S.; McEvoy, P. One factor? Two factor? Bi-factor? A psychometric evaluation of the Frost Multidimensional Scale and the Clinical Perfectionism Questionnaire. Cogn. Behav. Ther. 2020, 49, 518–530. [Google Scholar] [CrossRef] [PubMed]
- Prior, K.L.; Erceg-Hurn, D.M.; Raykos, B.C.; Egan, S.J.; Byrne, S.; McEvoy, P.M. Validation of the clinical perfectionism questionnaire in an eating disorder sample: A bifactor approach. Int. J. Eat. Disord. 2018, 51, 1176–1184. [Google Scholar] [CrossRef]
- Putnick, D.L.; Bornstein, M.H. Measurement invariance conventions and reporting: The state of the art and future directions for psychological research. Dev. Rev. 2016, 41, 71–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiekens, G.; Hasking, P.; Boyes, M. Measurement Invariance of Three Brief Emotion Regulation Questionnaires in People with and without a History of Non-Suicidal Self-Injury. Eur. J. Psychol. Assess. 2018, 35, 835–841. [Google Scholar] [CrossRef]
- Tonta, K.E.; Hasking, P.; Boyes, M.; Howell, J.; McEvoy, P.; Kiekens, G. Measurement invariance of three brief measures of rumination in young adults with and without a history of self-injury. Eur. J. Psychol. Assess. 2020, 37, 266–273. [Google Scholar] [CrossRef]
- Slabbert, A.; Hasking, P.; Greene, D.; Boyes, M. Measurement invariance of the distress tolerance scale among university students with and without a history of non-suicidal self-injury. PeerJ 2021, 9, e10915. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D.; Glenn, C.R. Assessing the functions of non-suicidal self-injury: Psychometric properties of the Inventory of Statements about Self-injury (ISAS). J. Psychopathol. Behav. Assess. 2009, 31, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Glenn, C.R.; Klonsky, E.D. One-year test-retest reliability of the Inventory of Statements about Self-Injury (ISAS). Assessment 2011, 18, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Egan, S.J.; Shafran, R.; Lee, M.; Fairburn, C.G.; Cooper, Z.; Doll, H.A.; Palmer, R.L.; Watson, H.J. The Reliability and Validity of the Clinical Perfectionism Questionnaire in Eating Disorder and Community Samples. Behav. Cogn. Psychother. 2016, 44, 79–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shu, C.Y.; O’Brien, A.; Watson, H.J.; Anderson, R.A.; Wade, T.D.; Kane, R.T.; Lampard, A.; Egan, S.J. Structure and validity of the Clinical Perfectionism Questionnaire in female adolescents. Behav. Cogn. Psychother. 2020, 48, 268–279. [Google Scholar] [CrossRef]
- Shafran, R.; Cooper, Z.; Fairburn, C.G. “Clinical perfectionism” is not “multidimensional perfectionism”: A reply to Hewitt, Flett, Besser, Sherry & McGee. Behav. Res. Ther. 2003, 41, 1217–1220. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Li, C.H. Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav. Res. Methods 2016, 48, 936–949. [Google Scholar] [CrossRef] [Green Version]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guildford Publications: New York, NY, USA, 2015. [Google Scholar]
- Meade, A.W.; Johnson, E.C.; Braddy, P.W. Power and sensitivity of alternative fit indices in tests of measurement invariance. J. Appl. Psychol. 2008, 93, 568–592. [Google Scholar] [CrossRef]
- Kiekens, G.; Hasking, P.; Claes, L.; Boyes, M.; Mortier, P.; Auerbach, R.P.; Cuijpers, P.; Demyttenaere, K.; Green, J.G.; Kessler, R.C.; et al. Prediciting the incidence of non-suicidal self-injury in college students. Eur. Psychiatry 2019, 59, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Bresin, K.; Schoenleber, M. Gender differences in the prevalence of nonsuicidal self-injury: A meta-analysis. Clin. Psychol. Rev. 2015, 38, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Victor, S.E.; Muehlenkamp, J.J.; Hayes, N.A.; Lengel, G.J.; Styer, D.M.; Washburn, J.J. Characterizing gender differences in nonsuicidal self-injury: Evidence from a large clinical sample of adolescents and adults. Compr. Psychiatry 2018, 82, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Dawkins, J.C.; Hasking, P.A.; Boyes, M.E.; Greene, D.; Passchier, C. Applying a cognitive-emotional model to nonsuicidal self-injury. Stress Health 2019, 35, 39–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| FMPS | CPQ | |||
|---|---|---|---|---|
| N = 708 | N = 711 | |||
| n/M | %/SD | n/M | %/SD | |
| Female gender | 533 | 75.28% | 535 | 75.20% |
| Age | 20.48 | 2.21 | 20.48 | 2.22 |
| Lifetime history of NSSI | 299 | 42.23% | 299 | 42.10% |
| Sample means | ||||
| Strivings | 2.93 | 1.01 | 2.41 | 0.61 |
| Concerns | 3.34 | 1.01 | 2.39 | 0.69 |
| General factor | 3.13 | 0.85 | 2.41 | 0.56 |
| Χ2 | df | RMSEA [90% CI] | CFI | SRMR | NCI | |
|---|---|---|---|---|---|---|
| FMPS (N = 708) | ||||||
| Two factor | 140.52 | 19 | 0.095 [0.081, 0.110] | 0.990 | 0.025 | 0.918 |
| Bifactor | 48.41 | 11 | 0.069 [0.050, 0.090] | 0.997 | 0.016 | 0.974 |
| CPQ (N = 711) | ||||||
| Two factor | 306.14 | 34 | 0.106 [0.095, 0.117] | 0.837 | 0.069 | 0.826 |
| Two factor allowing items 3 and 10 to covary | 261.87 | 33 | 0.099 [0.088, 0.110) | 0.863 | 0.065 | 0.876 |
| Two factor (removing item 7 and allowing 3 and 10 to covary) | 155.47 | 25 | 0.086 [0.073, 0.099] | 0.899 | 0.059 | 0.894 |
| Χ2 | Df | NCI | CFI | Model Comparison | ΔNCI a | ΔCFI b | p MLR Δχ2 | |
|---|---|---|---|---|---|---|---|---|
| FMPS—two factor | ||||||||
| M1: Configural | 159.69 | 38 | 0.918 | 0.959 | - | - | - | - |
| M2: Full metric | 162.69 | 44 | 0.919 | 0.960 | M1–M2 | 0.0019 + | 0.001 + | 0.809 + |
| M3: Full scalar | 167.75 | 50 | 0.920 | 0.961 | M2–M3 | 0.0006 + | 0.001 + | 0.536 + |
| M4: Full residual error | 181.29 | 58 | 0.916 | 0.959 | M3–M4 | 0.0036 + | 0.002 + | 0.095 + |
| FMPS—Bifactor | ||||||||
| M1: Configural | 51.32 | 22 | 0.980 | 0.987 | - | - | - | - |
| M2: Full metric | 70.94 | 35 | 0.975 | 0.984 | M1–M2 | 0.0046 + | 0.003 − | 0.105 + |
| M3: Full scalar | 77.73 | 40 | 0.974 | 0.983 | M2–M3 | 0.0012 + | 0.001 + | 0.237 + |
| M4: Full residual error | 93.96 | 48 | 0.968 | 0.980 | M3–M4 | 0.0057 + | 0.003 − | 0.039 − |
| M4: Partial residual error c | 80.26 | 47 | 0.977 | 0.985 | M3–M4.1 | 0.0031 + | 0.002 + | 0.925 + |
| CPQ | ||||||||
| M1: Configural | 172.51 | 50 | 0.917 | 0.900 | - | - | - | - |
| M2: Full metric | 176.127 | 57 | 0.920 | 0.903 | M1–M2 | 0.0022 + | 0.003 − | 0.823 + |
| M3: Full scalar d | 192.93 | 64 | 0.923 | 0.895 | M2–M3 | 0.0063 + | 0.008 − | 0.019 − |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tonta, K.E.; Boyes, M.; Howell, J.; McEvoy, P.; Hasking, P. Measurement Invariance of Perfectionism Measures in Students with and without a History of Non-Suicidal Self-Injury. Int. J. Environ. Res. Public Health 2021, 18, 10171. https://doi.org/10.3390/ijerph181910171
Tonta KE, Boyes M, Howell J, McEvoy P, Hasking P. Measurement Invariance of Perfectionism Measures in Students with and without a History of Non-Suicidal Self-Injury. International Journal of Environmental Research and Public Health. 2021; 18(19):10171. https://doi.org/10.3390/ijerph181910171
Chicago/Turabian StyleTonta, Kate E., Mark Boyes, Joel Howell, Peter McEvoy, and Penelope Hasking. 2021. "Measurement Invariance of Perfectionism Measures in Students with and without a History of Non-Suicidal Self-Injury" International Journal of Environmental Research and Public Health 18, no. 19: 10171. https://doi.org/10.3390/ijerph181910171
APA StyleTonta, K. E., Boyes, M., Howell, J., McEvoy, P., & Hasking, P. (2021). Measurement Invariance of Perfectionism Measures in Students with and without a History of Non-Suicidal Self-Injury. International Journal of Environmental Research and Public Health, 18(19), 10171. https://doi.org/10.3390/ijerph181910171







