Would Older Adults Perform Preventive Practices in the Post-COVID-19 Era? A Community-Based Cross-Sectional Survey in China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Socio-Demographic Characteristics of the Study Participants
3.2. Knowledge, Perceived Vulnerability, Response Efficacy and Anxiety towards COVID-19 among Old Adults
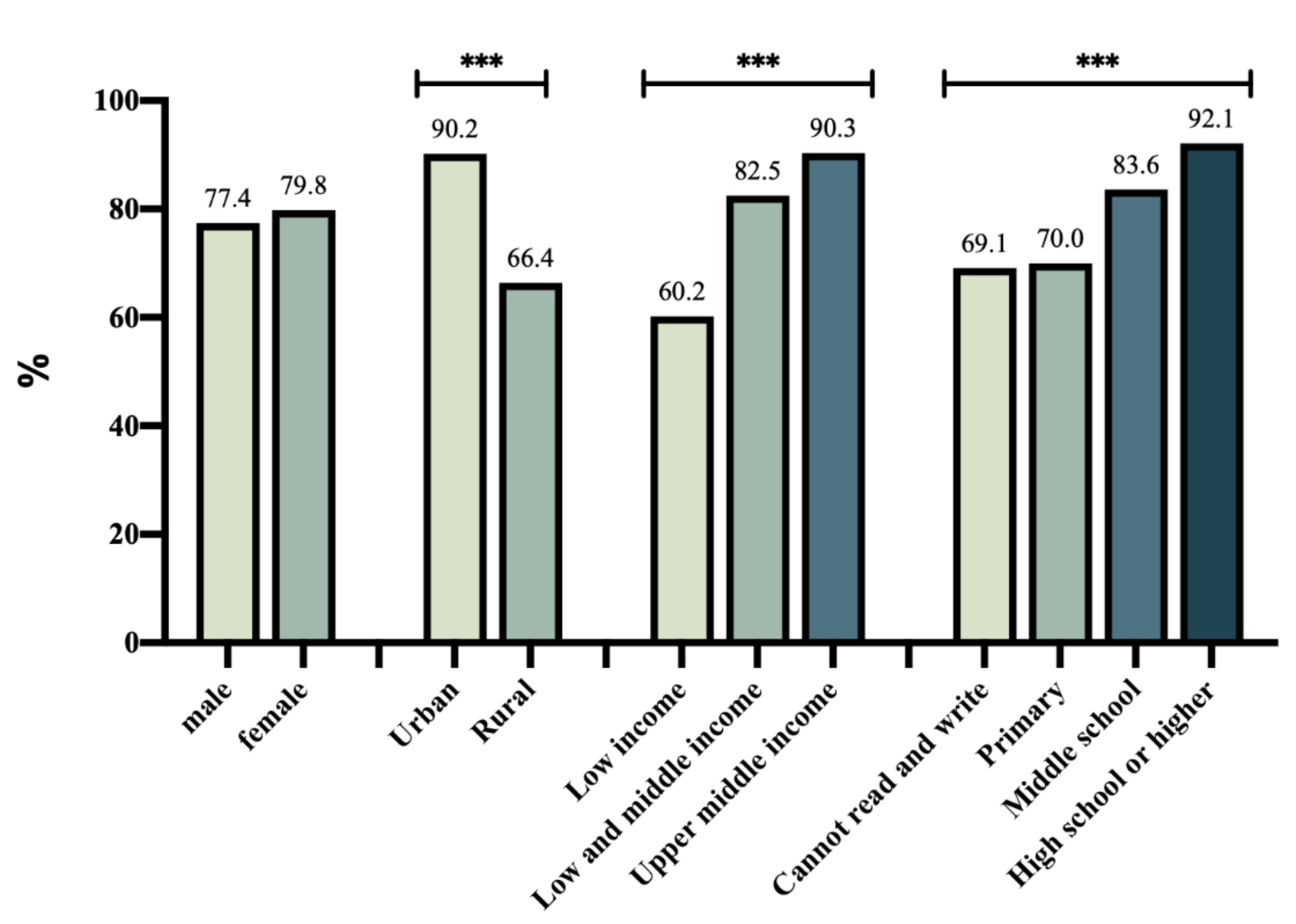
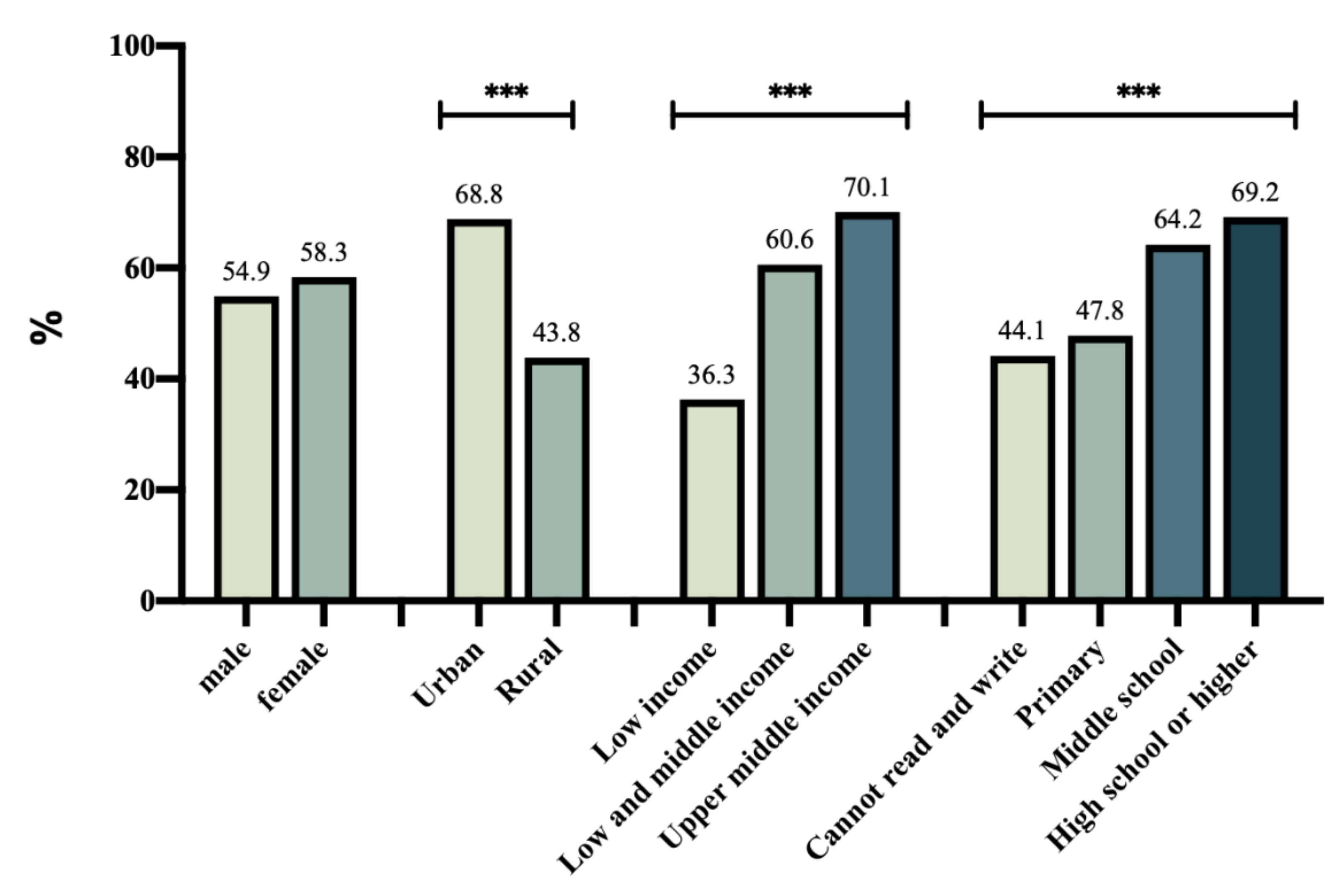
3.3. Preventive Practices toward COVID-19 among Older Adults
3.4. Factors Associated with Preventive Practice toward COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Xu, H.; Gan, Y.; Zheng, D.; Wu, B.; Zhu, X.; Xu, C.; Liu, C.; Tao, Z.; Hu, Y.; Chen, M.; et al. Relationship Between COVID-19 Infection and Risk Perception, Knowledge, Attitude, and Four Nonpharmaceutical Interventions During the Late Period of the COVID-19 Epidemic in China: Online Cross-Sectional Survey of 8158 Adults. J. Med. Internet Res. 2020, 22, e21372. [Google Scholar] [CrossRef]
- Teslya, A.; Pham, T.M.; Godijk, N.G.; Kretzschmar, M.E.; Bootsma, M.C.J.; Rozhnova, G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: A modelling study. PLoS Med. 2020, 17, e1003166. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Si, H.; Shen, L.; Liu, W.; Wu, G. Uncovering people’s mask-saving intentions and behaviors in the post-COVID-19 period: Evidence from China. Sustain. Cities Soc. 2021, 65, 102626. [Google Scholar] [CrossRef]
- Lau, J.T.; Yang, X.; Tsui, H.Y.; Kim, J.H. Impacts of SARS on health-seeking behaviors in general population in Hong Kong. Prev. Med. 2005, 41, 454–462. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, R.; Chen, B.; Chen, H.; Li, Y.; Chen, Z.; Zhu, H.; Wang, H. Knowledge, Perceived Beliefs, and Preventive Behaviors Related to COVID-19 Among Chinese Older Adults: Cross-Sectional Web-Based Survey. J. Med. Internet Res. 2020, 22, e23729. [Google Scholar] [CrossRef]
- Suzuki, Y.; Maeda, N.; Hirado, D.; Shirakawa, T.; Urabe, Y. Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2020, 17, 6591. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhang, J.; Wu, W.; Liang, M.; Wu, Q.S. Willingness to receive future COVID-19 vaccines following the COVID-19 epidemic in Shanghai, China. BMC Public Health 2021, 21, 1103. [Google Scholar] [CrossRef]
- Christie, A.; Henley, S.J.; Mattocks, L.; Fernando, R.; Lansky, A.; Ahmad, F.B.; Adjemian, J.; Anderson, R.N.; Binder, A.M.; Carey, K.; et al. Decreases in COVID-19 Cases, Emergency Department Visits, Hospital Admissions, and Deaths Among Older Adults Following the Introduction of COVID-19 Vaccine—United States, 6 September 2020–1 May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 858–864. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, M.W.; Olson, S.M.; Self, W.H.; Talbot, H.K.; Lindsell, C.J.; Steingrub, J.S.; Shapiro, N.I.; Ginde, A.A.; Douin, D.J.; Prekker, M.E.; et al. Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 Among Hospitalized Adults Aged ≥ 65 Years—United States, January–March 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.E.; Frenck, R.W., Jr.; Falsey, A.R.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Neuzil, K.; Mulligan, M.J.; Bailey, R.; et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. N. Engl. J. Med. 2020, 383, 2439–2450. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Perez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Xia, S.; Zhang, Y.; Wang, Y.; Wang, H.; Yang, Y.; Gao, G.F.; Tan, W.; Wu, G.; Xu, M.; Lou, Z.; et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: A randomised, double-blind, placebo-controlled, phase 1/2 trial. Lancet Infect. Dis. 2021, 21, 39–51. [Google Scholar] [CrossRef]
- Prasetyo, Y.T.; Castillo, A.M.; Salonga, L.J.; Sia, J.A.; Seneta, J.A. Factors affecting perceived effectiveness of COVID-19 prevention measures among Filipinos during Enhanced Community Quarantine in Luzon, Philippines: Integrating Protection Motivation Theory and extended Theory of Planned Behavior. Int. J. Infect. Dis. 2020, 99, 312–323. [Google Scholar] [CrossRef]
- Ezati Rad, R.; Mohseni, S.; Kamalzadeh Takhti, H.; Hassani Azad, M.; Shahabi, N.; Aghamolaei, T.; Norozian, F. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: A cross-sectional study. BMC Public Health 2021, 21, 466. [Google Scholar] [CrossRef] [PubMed]
- Dixon, D.; Den Daas, C.; Hubbard, G.; Johnston, M. Using behavioural theory to understand adherence to behaviours that reduce transmission of COVID-19; evidence from the CHARIS representative national study. Br. J. Health Psychol. 2021. Early view. [Google Scholar] [CrossRef] [PubMed]
- Barber, S.J.; Kim, H. COVID-19 Worries and Behavior Changes in Older and Younger Men and Women. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, e17–e23. [Google Scholar] [CrossRef]
- Puterman, E.; DeLongis, A.; Lee-Baggley, D.; Greenglass, E. Coping and health behaviours in times of global health crises: Lessons from SARS and West Nile. Glob. Public Health 2009, 4, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Wu, Q.; Wang, P.; Xu, Y.; Wang, L.; Zhao, Y.; Yao, D.; Xu, Y.; Lv, Q.; Xu, S. Measures Undertaken in China to Avoid COVID-19 Infection: Internet-Based, Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e18718. [Google Scholar] [CrossRef] [PubMed]
- Khasawneh, A.I.; Humeidan, A.A.; Alsulaiman, J.W.; Bloukh, S.; Ramadan, M.; Al-Shatanawi, T.N.; Awad, H.H.; Hijazi, W.Y.; Al-Kammash, K.R.; Obeidat, N.; et al. Medical Students and COVID-19: Knowledge, Attitudes, and Precautionary Measures. A Descriptive Study From Jordan. Front. Public Health 2020, 8, 253. [Google Scholar] [CrossRef]
- Beaudoin, C.E.; Hong, T. Predictors of COVID-19 Preventive Perceptions and Behaviors: Two Cross-Sectional Studies of Millennials. J. Med. Internet Res. 2021, in press. [Google Scholar] [CrossRef]
- Coroiu, A.; Moran, C.; Campbell, T.; Geller, A.C. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS ONE 2020, 15, e0239795. [Google Scholar] [CrossRef]
- Gotanda, H.; Miyawaki, A.; Tabuchi, T.; Tsugawa, Y. Association Between Trust in Government and Practice of Preventive Measures During the COVID-19 Pandemic in Japan. J. Gen. Intern. Med. 2021, 1–7. [Google Scholar] [CrossRef]
- Leung, G.M.; Ho, L.M.; Chan, S.K.; Ho, S.Y.; Bacon-Shone, J.; Choy, R.Y.; Hedley, A.J.; Lam, T.H.; Fielding, R. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 2005, 40, 1713–1720. [Google Scholar] [CrossRef]
- Garcia-Continente, X.; Serral, G.; Lopez, M.J.; Perez, A.; Nebot, M. Long-term effect of the influenza A/H1N1 pandemic: Attitudes and preventive behaviours one year after the pandemic. Eur. J. Public Health 2013, 23, 679–681. [Google Scholar] [CrossRef][Green Version]
- Lau, J.T.; Tsui, H.Y.; Kim, J.H.; Chan, P.K.; Griffiths, S. Monitoring of perceptions, anticipated behavioral, and psychological responses related to H5N1 influenza. Infection 2010, 38, 275–283. [Google Scholar] [CrossRef]
- Yazdanpanah, M.; Abadi, B.; Komendantova, N.; Zobeidi, T.; Sieber, S. Some at Risk for COVID-19 Are Reluctant to Take Precautions, but Others Are Not: A Case from Rural in Southern Iran. Front. Public Health 2020, 8, 562300. [Google Scholar] [CrossRef] [PubMed]
- Hromatko, I.; Tonkovic, M.; Vranic, A. Trust in Science, Perceived Vulnerability to Disease, and Adherence to Pharmacological and Non-pharmacological COVID-19 Recommendations. Front. Psychol. 2021, 12, 664554. [Google Scholar] [CrossRef]
- Brewer, N.T.; Weinstein, N.D.; Cuite, C.L.; Herrington, J.E. Risk perceptions and their relation to risk behavior. Ann. Behav. Med. 2004, 27, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Renner, B.; Schüz, B.; Sniehotta, F.F. Preventive health behavior and adaptive accuracy of risk perceptions. Risk Anal. 2008, 28, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Klepper, S.; Odenwald, M.; Rösner, S.; Senn, S.; Menning, H.; Pereyra-Kröll, D.; Rockstroh, B. Experience-Induced Change of Alcohol-Related Risk Perception in Patients with Alcohol Use Disorders. Front. Psychol. 2017, 8, 1967. [Google Scholar] [CrossRef]
- Chen, L.S.; Kaphingst, K.A.; Tseng, T.S.; Zhao, S. How are lung cancer risk perceptions and cigarette smoking related?—Testing an accuracy hypothesis. Transl. Cancer Res. 2016, 5 (Suppl. 5), S964–S971. [Google Scholar] [CrossRef] [PubMed]
- Techasatian, L.; Lebsing, S.; Uppala, R.; Thaowandee, W.; Chaiyarit, J.; Supakunpinyo, C.; Panombualert, S.; Mairiang, D.; Saengnipanthkul, S.; Wichajarn, K.; et al. The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. J. Prim. Care Community Health 2020, 11, 2150132720966167. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Participants |
|---|---|
| Age | |
| 60~69 | 1737 (58.0) |
| ≥70 | 1259 (42.0) |
| Gender a | |
| male | 1317 (44.0) |
| female | 1672 (55.8) |
| Education | |
| Illiterate/Barely literate | 493 (16.4) |
| Primary | 964 (32.2) |
| Middle school | 890 (29.7) |
| High school or higher | 649 (21.7) |
| Marital status b | |
| married | 2439 (81.7) |
| Unmarried/divorce/widowed | 547 (18.0) |
| Household income c | |
| Low | 791 (26.4) |
| Low and middle | 1398 (46.7) |
| Upper middle | 796 (26.7) |
| Region d | |
| Urban | 1547 (51.6) |
| Rural | 1448 (48.3) |
| Household composition | |
| Living with others | 2736 (91.3) |
| Living alone | 260 (8.7) |
| Medical insurance | |
| No insurance | 40 (1.3) |
| Basic old-age insurance for urban workers | 999 (33.3) |
| Basic medical insurance for urban residents | 837 (27.9) |
| Rural cooperative medical care | 1062 (35.4) |
| Others (commercial insurance, state medicine, etc.) | 161 (5.4) |
| Number of chronic diseases | |
| 0 | 1212 (40.5) |
| 1 | 1014 (33.8) |
| ≥2 | 761 (25.7) |
| Total | 2996 |
| Knowledge Score | Felt Anxiety or Panic Since the Outbreak of Epidemic | Perceived High Risk of Being Infected in the Future | Believed That Personal Preventive Practices Were Effective | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥4 | χ2 | p | Yes | χ2 | p | Yes | χ2 | p | Yes | χ2 | p | |
| Gender | 0.258 | 0.612 | 6.134 | 0.013 | 0.184 | 0.668 | 0.015 | 0.904 | ||||
| Male | 1127, 85.6 | 582, 44.2 | 104, 7.9 | 1090, 82.8 | ||||||||
| Female | 1441, 86.2 | 815, 48.7 | 125, 7.5 | 1381, 82.6 | ||||||||
| Region | 27.233 | 0.000 | 11.092 | 0.001 | 1.771 | 0.183 | 23.305 | 0.000 | ||||
| Urban | 1379, 89.1 | 678, 43.8 | 128, 8.3 | 1329, 85.9 | ||||||||
| Rural | 1194, 82.5 | 722, 49.9 | 101, 7 | 1148, 79.3 | ||||||||
| Education level | 47.896 | 0.000 | 1.756 | 0.625 | 3.973 | 0.264 | 88.674 | 0.000 | ||||
| Illiterate | 379, 77 | 218, 44.3 | 46, 9.3 | 353, 71.7 | ||||||||
| Primary | 827, 85.8 | 450, 46.7 | 63, 6.5 | 766, 79.5 | ||||||||
| Middle school | 776, 87.2 | 426, 47.9 | 72, 8.1 | 767, 86.2 | ||||||||
| High school or higher | 591, 91.1 | 306, 47.1 | 48, 7.4 | 591, 91.1 | ||||||||
| Income level | 41.156 | 0.000 | 15.089 | 0.001 | 0.317 | 0.853 | 46.627 | 0.000 | ||||
| Low | 628, 79.4 | 412, 52.1 | 60, 7.6 | 594, 75.1 | ||||||||
| Low and middle | 1230, 88 | 646, 46.2 | 111, 7.9 | 1186, 84.8 | ||||||||
| Upper middle | 710, 89.2 | 338, 42.5 | 58, 7.3 | 692, 86.9 | ||||||||
| Number of chronic diseases | 15.200 | 0.001 | 7.642 | 0.022 | 0.068 | 0.967 | 20.330 | 0.000 | ||||
| 0 | 1011, 83.4 | 531, 43.8 | 94, 7.7 | 971, 80.1 | ||||||||
| 1 | 871, 85.9 | 500, 49.3 | 76, 7.5 | 828, 81.7 | ||||||||
| ≥2 | 684, 89.9 | 368, 48.4 | 58, 7.6 | 671, 88.2 | ||||||||
| Predictors | Model 1 | Model 2 | Model 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | Wald | Exp(B) | p-Value | B | Wald | Exp(B) | p-Value | B | Wald | Exp(B) | p-Value | |
| Gender | 0.198 | 3.773 | 1.219 | 0.052 | 0.184 | 3.230 | 1.202 | 0.072 | 0.172 | 2.777 | 1.187 | 0.096 |
| Age | −0.012 | 2.350 | 0.988 | 0.125 | −0.012 | 2.223 | 0.988 | 0.136 | −0.012 | 2.149 | 0.989 | 0.143 |
| Education | 22.949 | 0.000 | 20.560 | 0.000 | 18.158 | 0.000 | ||||||
| Primary | −0.050 | 0.147 | 0.951 | 0.701 | −0.128 | 0.936 | 0.880 | 0.333 | −0.167 | 1.550 | 0.847 | 0.213 |
| Middle school | 0.281 | 3.525 | 1.324 | 0.060 | 0.188 | 1.530 | 1.206 | 0.216 | 0.132 | 0.740 | 1.141 | 0.390 |
| High school or higher | 0.772 | 14.808 | 2.164 | 0.000 | 0.664 | 10.755 | 1.943 | 0.001 | 0.582 | 8.115 | 1.790 | 0.004 |
| Marital status | −0.126 | 1.007 | 0.882 | 0.316 | −0.076 | 0.358 | 0.927 | 0.550 | −0.104 | 0.659 | 0.902 | 0.417 |
| Income level | 40.416 | 0.000 | 37.851 | 0.000 | 33.757 | 0.000 | ||||||
| Low and middle | 0.659 | 32.939 | 1.933 | 0.000 | 0.638 | 30.524 | 1.892 | 0.000 | 0.601 | 26.600 | 1.824 | 0.000 |
| Upper middle | 0.897 | 27.196 | 2.451 | 0.000 | 0.887 | 25.888 | 2.404 | 0.000 | 0.846 | 23.845 | 2.330 | 0.000 |
| Region | −0.874 | 44.917 | 0.417 | 0.000 | −0.875 | 45.092 | 0.417 | 0.000 | −0.924 | 49.502 | 0.397 | 0.000 |
| Chronic disease | −0.038 | 0.047 | 0.963 | 0.428 | −0.056 | 1.385 | 0.945 | 0.239 | −0.071 | 2.136 | 0.932 | 0.144 |
| COVID-19 knowledge | 0.108 | 18.795 | 1.114 | 0.000 | 0.084 | 10.578 | 1.088 | 0.001 | ||||
| Response efficacy | 0.474 | 15.033 | 1.607 | 0.000 | ||||||||
| Anxiety | 0.386 | 0.824 | ||||||||||
| A little | 0.099 | 0.386 | 1.104 | 0.534 | ||||||||
| Very | 0.019 | 0.001 | 1.020 | 0.978 | ||||||||
| Perceived vulnerability | −0.614 | 13.447 | 0.541 | 0.000 | ||||||||
| Model Chi-square | 344.992 | 363.495 | 390.456 | |||||||||
| Degree of freedom | 10 | 11 | 15 | |||||||||
| Model significance | <0.001 | <0.001 | <0.001 | |||||||||
| Predictors | Model 1 | Model 2 | Model 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | Wald | Exp(B) | p-Value | B | Wald | Exp(B) | p-Value | B | Wald | Exp(B) | p-Value | |
| Gender | 0.180 | 4.725 | 1.198 | 0.030 | 0.163 | 3.795 | 1.177 | 0.051 | 0.158 | 3.496 | 1.171 | 0.062 |
| Age | −0.007 | 1.136 | 0.993 | 0.287 | −0.006 | 0.816 | 0.994 | 0.366 | −0.006 | 0.808 | 0.994 | 0.369 |
| Education | 18.108 | 0.000 | 11.177 | 0.011 | 8.652 | 0.034 | ||||||
| Primary | 0.116 | 0.951 | 1.123 | 0.329 | 0.009 | 0.006 | 1.009 | 0.939 | −0.027 | 0.050 | 0.973 | 0.824 |
| Middle school | 0.455 | 12.702 | 1.577 | 0.000 | 0.321 | 6.063 | 1.379 | 0.014 | 0.266 | 4.069 | 1.305 | 0.044 |
| High school or higher | 0.443 | 9.103 | 1.558 | 0.003 | 0.281 | 3.500 | 1.324 | 0.061 | 0.196 | 1.672 | 1.217 | 0.196 |
| Marital status | −0.012 | 0.014 | 0.988 | 0.906 | 0.051 | 0.222 | 1.052 | 0.637 | 0.040 | 0.136 | 1.041 | 0.713 |
| Income level | 47.336 | 0.000 | 43.283 | 0.000 | 39.620 | 0.000 | ||||||
| Low and middle | 0.655 | 38.443 | 1.924 | 0.000 | 0.633 | 35.186 | 1.884 | 0.000 | 0.605 | 31.545 | 1.831 | 0.000 |
| Upper middle | 0.856 | 39.633 | 2.354 | 0.000 | 0.828 | 36.224 | 2.289 | 0.000 | 0.807 | 33.819 | 2.240 | 0.000 |
| Region | −0.460 | 20.643 | 0.631 | 0.000 | −0.466 | 20.722 | 0.628 | 0.000 | −0.492 | 22.696 | 0.611 | 0.000 |
| Chronic disease | 0.134 | 12.208 | 1.143 | 0.000 | 0.108 | 7.701 | 1.114 | 0.006 | 0.106 | 7.171 | 1.112 | 0.007 |
| COVID-19 knowledge | 0.177 | 62.104 | 1.193 | 0.000 | 0.156 | 45.857 | 1.168 | 0.000 | ||||
| Response efficacy | 0.530 | 23.182 | 1.699 | 0.000 | ||||||||
| Anxiety | 4.731 | 0.094 | ||||||||||
| A little | −0.213 | 2.686 | 0.808 | 0.101 | ||||||||
| Very | 0.918 | 1.869 | 2.505 | 0.172 | ||||||||
| Perceived vulnerability | −0.336 | 5.138 | 0.715 | 0.023 | ||||||||
| Model Chi-square | 287.245 | 351.328 | 383.658 | |||||||||
| Degree of freedom | 10 | 11 | 15 | |||||||||
| Model significance | <0.001 | <0.001 | <0.001 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, M.; Wang, X.; Yun, Q.; Lin, Y.; Wu, Q.; Yang, Q.; Wan, D.; Tian, D.; Chang, C. Would Older Adults Perform Preventive Practices in the Post-COVID-19 Era? A Community-Based Cross-Sectional Survey in China. Int. J. Environ. Res. Public Health 2021, 18, 10169. https://doi.org/10.3390/ijerph181910169
Chen M, Wang X, Yun Q, Lin Y, Wu Q, Yang Q, Wan D, Tian D, Chang C. Would Older Adults Perform Preventive Practices in the Post-COVID-19 Era? A Community-Based Cross-Sectional Survey in China. International Journal of Environmental Research and Public Health. 2021; 18(19):10169. https://doi.org/10.3390/ijerph181910169
Chicago/Turabian StyleChen, Meijun, Xiaoqi Wang, Qingping Yun, Yuting Lin, Qingqing Wu, Qinghua Yang, Dezhi Wan, Dan Tian, and Chun Chang. 2021. "Would Older Adults Perform Preventive Practices in the Post-COVID-19 Era? A Community-Based Cross-Sectional Survey in China" International Journal of Environmental Research and Public Health 18, no. 19: 10169. https://doi.org/10.3390/ijerph181910169
APA StyleChen, M., Wang, X., Yun, Q., Lin, Y., Wu, Q., Yang, Q., Wan, D., Tian, D., & Chang, C. (2021). Would Older Adults Perform Preventive Practices in the Post-COVID-19 Era? A Community-Based Cross-Sectional Survey in China. International Journal of Environmental Research and Public Health, 18(19), 10169. https://doi.org/10.3390/ijerph181910169





