Barriers to Access of Healthcare Services for Rural Women—Applying Gender Lens on TB in a Rural District of Sindh, Pakistan
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Data Management and Analysis
2.4. Ethical Considerations
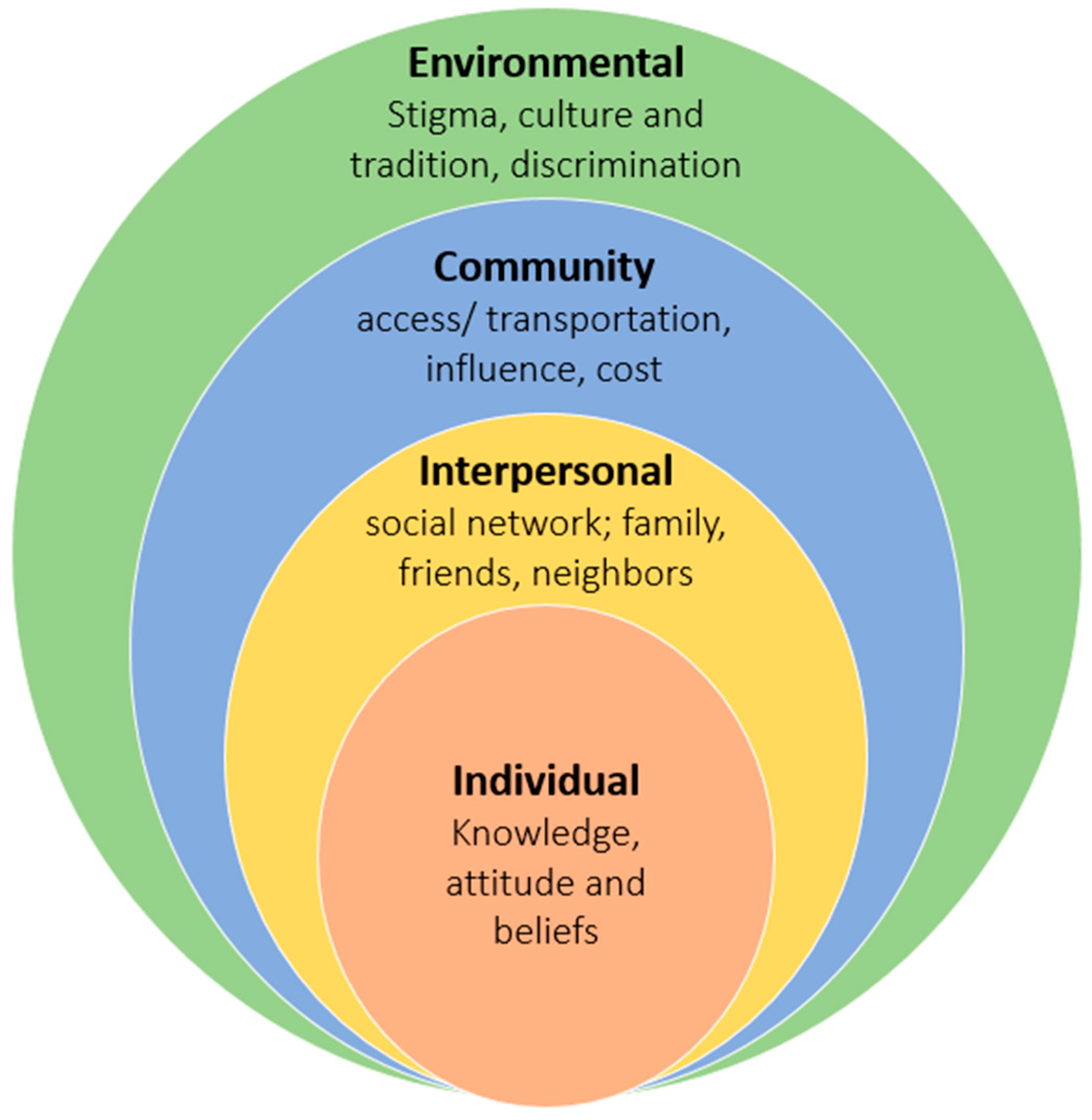
3. Results
3.1. Individual Level Analysis
“There is sugar and blood pressure. If someone with blood pressure issues consumes sugar, then they immediately become diabetic. Besides that, there is fever, cough, TB; these problems have become more prevalent.”—Lay community woman, 26 to 49 years group
“Many women lose their first child. Often the new-born’s heart doesn’t work or stops working after a few days.”—Lay community woman, 18 to 25 years group
“TB is a common disease and it is curable. I’ve heard when one person has TB in the household then it spreads to the entire family. If the person has children, then the children may also get it.”—Community Resource Person
“My mother had TB and then my three-year old daughter caught it as well. Now they are completely fine after completion of treatment.”—Community Resource Person
3.2. Interpersonal Level Analysis
“My husband says that children should be engaged in active labour work and earn money while I say that they should go to school.”—Lay community woman, 18 to 25 years group
“Men can stay alone in the hospital while there should be someone with the woman. When a woman goes to the hospital, her husband or brother goes with her. When the breadwinner of the house goes with the woman then everyone in the family gets worried. There are all kinds of resources in Kotri, but because of these reasons, women don’t go.”—Lay community woman, 26 to 49 years group
“If we need to travel to the city for any purpose, we must seek our husband’s permission and travel with a male family member. If the husband does not give us permission, we do not go”—Lay community woman, 26 to 49 years group
“If the son falls ill, he is sent to the hospital immediately but if the girl falls ill, she is told to take a tablet to make it better.”—Lay community woman, 26 to 49 years group
“If there is a big issue, for example, if there is a need to travel to Hyderabad or Karachi due to sickness, we obviously cannot travel without our husband or brother-in-law. We are not independent in doing such big things, but can take care of smaller issues ourselves.”—Community Resource Person
3.3. Community Level Analysis
“You know that ‘maahol” (environment) is not suitable for girls that’s why we do not send them out of the house unless needed. Small kids roam in the streets all day, but we do not send our daughters outside as they grow slightly older”—Lay community woman, 26 to 49 years group
“If a woman has vocational skills then she will never have to beg anyone for money.”—Lay community woman, 26 to 49 years group
“Women who are “khud-mukhtaar” (self-reliant) can take better care of their own health and well-being. They buy groceries and food items for the house and hence are free to consume those whichever way they like”—Lay community woman, 18 to 25 years group
3.4. Environmental/Structural Level Analysis
“Everything is done on referential requests [bribes]; if you have a reference then you immediately get the treatment or else you are made to wait and often the doctor leaves and you have to come again. Therefore, we don’t go to Civil (Hospital) and prefer to go to private facilities.”—Lay community woman, 18 to 25 years group
“How can they go to the doctor; transport is an issue, cost of treatment is an issue, having small kids to take care of at home is an issue…”—Community Resource Person
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fikree, F.F.; Pasha, O. Role of gender in health disparity: The South Asian context. BMJ 2004, 328, 823–826. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, N.; Gkiouleka, A.; Milner, A.; Montag, D.; Gallo, V. Girls’ hidden penalty: Analysis of gender inequality in child mortality with data from 195 countries. BMJ Glob. Health 2018, 3, e001028. [Google Scholar] [CrossRef]
- Azad, A.D.; Charles, A.G.; Ding, Q.; Trickey, A.W.; Wren, S.M. The gender gap and healthcare: Associations between gender roles and factors affecting healthcare access in Central Malawi, June–August 2017. Arch. Public Health 2020, 78, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.B.; Phillips, J.F.; Pence, B. The Effect of Women’s Status on Infant and Child Mortality in four rural areas of bangladesh. J. Biosoc. Sci. 2007, 39, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Zodpey, S.; Negandhi, P. Inequality in health and social status for women in India—A long-standing bane. Indian J. Public Health 2020, 64, 325–327. [Google Scholar] [CrossRef]
- Kennedy, E.; Binder, G.; Humphries-Waa, K.; Tidhar, T.; Cini, K.; Comrie-Thomson, L.; Vaughan, C.; Francis, K.; Scott, N.; Wulan, N.; et al. Gender inequalities in health and wellbeing across the first two decades of life: An analysis of 40 low-income and middle-income countries in the Asia-Pacific region. Lancet Glob. Health 2020, 8, e1473–e1488. [Google Scholar] [CrossRef]
- Fotso, J.C.; Ezeh, A.C.; Essendi, H. Maternal health in resource-poor urban settings: How does women’s autonomy influence the utilization of obstetric care services? Reprod. Health 2009, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Habib, S.S.; Zaidi, S.M.A.; Jamal, W.Z.; Azeemi, K.S.; Khan, S.; Khowaja, S.; Domki, A.K.; Khan, A.; Khan, F.A. Gender-based differences in community-wide screening for pulmonary tuberculosis in Karachi, Pakistan: An observational study of 311 732 individuals undergoing screening. Thorax 2021. [Google Scholar] [CrossRef]
- Chauhan, K. Patriarchal Pakistan: Women’s representation, access to resources, and institutional practices. In Gender Inequality in the Public Sector in Pakistan; Palgrave Macmillan: New York, NY, USA, 2014; pp. 57–87. [Google Scholar]
- Ali, S.M. Gender and Health Care Utilisation in Pakistan. Pak. Dev. Rev. 2000, 39, 213–234. [Google Scholar] [CrossRef]
- World Economic Forum. Global Gender Gap Report 2020. Available online: http://www3.weforum.org/docs/WEF_GGGR_2020.pdf (accessed on 22 September 2021).
- Mumtaz, Z.; Salway, S.; Waseem, M.; Umer, N. Gender-based barriers to primary health care provision in Pakistan: The experi-ence of female providers. Health Policy Plan. 2003, 18, 261–269. [Google Scholar] [CrossRef]
- Mahmood, N. Women’s role in domestic decision-making in Pakistan: Implications for reproductive behaviour. Pak. Dev. Rev. 2002, 41, 121–148. [Google Scholar] [CrossRef]
- Country Briefing Paper WOMEN IN PAKISTAN Adb.org. 2000. Available online: https://www.adb.org/sites/default/files/institutional-document/32562/women-pakistan.pdf (accessed on 22 September 2021).
- Tuberculosis in Women. World Health Organization, 2019. Available online: https://www.who.int/tb/publications/tb_women_factsheet.pdf?ua=1 (accessed on 31 August 2021).
- Qadeer, E.; Fatima, R.; Yaqoob, A.; Tahseen, S.; Haq, M.U.; Ghafoor, A.; Asif, M.; Straetemans, M.; Tiemersma, E.W. Population Based National Tuberculosis Prevalence Survey among Adults (>15 Years) in Pakistan, 2010–2011. PLoS ONE 2016, 11, e0148293. [Google Scholar] [CrossRef]
- Global Tuberculosis Report 2019; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2019.
- Global Tuberculosis Report 2020; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2020.
- Khan, M.S.; Khan, M.S.; Hasan, R.; Godfrey-Faussett, P. Unusual sex differences in tuberculosis notifications across Pakistan and the role of environmental/structural factors. East Mediterr Health J. 2013, 19, 821–825. [Google Scholar] [CrossRef] [PubMed]
- Codlin, A.J.; Khowaja, S.; Chen, Z.; Rahbar, M.H.; Qadeer, E.; Ara, I.; McCormick, J.B.; Fisher-Hoch, S.P.; Khan, A.J. Gender Differences in Tuberculosis Notification in Pakistan. Am. J. Trop. Med. Hyg. 2011, 85, 514–517. [Google Scholar] [CrossRef] [PubMed]
- United Nations Development Programme. Multidimensional Poverty in Pakista. Available online: https://www.undp.org/content/dam/pakistan/docs/MPI/Multidimensional%20Poverty%20in%20Pakistan.pdf (accessed on 22 September 2021).
- Asim, M.; Nawaz, Y. Child Malnutrition in Pakistan: Evidence from Literature. Children 2018, 5, 60. [Google Scholar] [CrossRef]
- Nutrition Profile—District Tando Allahyar. 2021. Available online: http://www.rspn.org/wp-content/uploads/2019/03/Nutrition-Profile_Tando-Allahyar.pdf (accessed on 5 July 2021).
- National Population Data (District wise). National TB Control Program; 2021. Available online: http://ntp.gov.pk/ntp-old/uploads/pi/DISTRICTS_POPULATION_2015.pdf (accessed on 31 August 2021).
- Ltd. G. Sehat Kahani | The Story of Health. Sehat Kahani. Available online: https://sehatkahani.com/ (accessed on 19 July 2021).
- National Rural Support Programme. Nrsp.org.pk. Available online: https://nrsp.org.pk/ (accessed on 19 July 2021).
- Golden, S.D.; Earp, J.A. Social ecological approaches to individuals and their contexts: Twenty years of health education & be-havior health promotion interventions. Health Educ. Behav. 2012, 39, 364–372. [Google Scholar]
- Program for Improved Nutrition in Sindh (PINS). 2021. Available online: http://www.rspn.org/wp-content/uploads/2020/05/Consolidated-Report-of-CRPs-on-WASH-Activities-SBCC-Toolkit.pdf (accessed on 31 August 2021).
- Khan, A. Mobility of women and access to health and family planning services in Pakistan. Reprod. Health Matters 1999, 7, 39–48. [Google Scholar] [CrossRef]
- Country Gender Profile: Islamic Republic of Pakistan [Internet]. Jica.go.jp. 2015. Available online: https://www.jica.go.jp/english/our_work/thematic_issues/gender/background/c8h0vm0000anjqj6-att/pakistan_2015.pdf (accessed on 22 September 2021).
- Khan, A.; Shaikh, B.T.; Baig, M.A. Knowledge, Awareness, and Health-Seeking Behaviour regarding Tuberculosis in a Rural District of Khyber Pakhtunkhwa, Pakistan. BioMed Res. Int. 2020, 2020, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, B.T.; Hatcher, J. Health seeking behaviour and health service utilization in Pakistan: Challenging the policy makers. J. Public Health 2004, 27, 49–54. [Google Scholar] [CrossRef]
- Riaz, A.; Zaidi, S.; Khowaja, A.R. Perceived barriers to utilizing maternal and neonatal health services in contracted-out versus government-managed health facilities in the rural districts of Pakistan. Int. J. Health Policy Manag. 2015, 4, 279–284. [Google Scholar] [CrossRef]
- Panezai, S.; Ahmad, M.M.; Saqib, S.E. Factors affecting access to primary health care services in Pakistan: A gender-based analy-sis. Dev. Pract. 2017, 27, 813–827. [Google Scholar] [CrossRef]
- Rizvi, N.; Nishtar, S. Pakistan’s health policy: Appropriateness and relevance to women’s health needs. Health Policy 2008, 88, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Mumtaz, Z.; Salway, S.M. Gender, pregnancy and the uptake of antenatal care services in Pakistan. Sociol. Health Illn. 2007, 29, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Chandra-Mouli, V.; McCarraher, D.R.; Phillips, S.J.; Williamson, N.E.; Hainsworth, G. Contraception for adolescents in low and middle income countries: Needs, barriers, and access. Reprod. Health 2014, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shah, I.; Åhman, E. Age Patterns of Unsafe Abortion in Developing Country Regions. Reprod. Health Matters 2004, 12, 9–17. [Google Scholar] [CrossRef][Green Version]
- Rimande-Joel, R.; Ekenedo, G.O. Knowledge, Belief and practice of cervical cancer screening and prevention among women of Taraba, North-East Nigeria. Asian Pac. J. Cancer Prev. APJCP 2019, 20, 3291. [Google Scholar] [CrossRef]
- Mumtaz, Z.; Salway, S. ‘I never go anywhere’: Extricating the links between women’s mobility and uptake of reproductive health services in Pakistan. Soc. Sci. Med. 2005, 60, 1751–1765. [Google Scholar] [CrossRef]
- King, T.L.; Kavanagh, A.; Scovelle, A.J.; Milner, A. Associations between gender equality and health: A systematic review. Health Promot. Int. 2020, 35, 27–41. [Google Scholar] [CrossRef]
- Bustamante-Gavino, M.I.; Rattani, S.; Khan, K. Women’s Empowerment in Pakistan–Definitions and Enabling and Disenabling Factors: A Secondary Data Analysis. J. Transcult. Nurs. 2011, 22, 174–181. [Google Scholar] [CrossRef]
- Rizvi, N.; Khan, K.S.; Shaikh, B.T. Gender: Shaping personality, lives and health of women in Pakistan. BMC Women’s Health 2014, 14, 53. [Google Scholar] [CrossRef]
- Lönnroth, K.; Jaramillo, E.; Williams, B.; Dye, C.; Raviglione, M. Drivers of tuberculosis epidemics: The role of risk factors and social determinants. Soc. Sci. Med. 2009, 68, 2240–2246. [Google Scholar] [CrossRef] [PubMed]
- Benazir Income Support Programme. Available online: https://www.bisp.gov.pk/ (accessed on 22 September 2021).
- Berg, S. Snowball Sampling: Overview. Available online: https://onlinelibrary.wiley.com/doi/10.1002/9781118445112.stat03370 (accessed on 22 September 2021).
- Tuberculosis Information Note. The Global Fund, 2019. Available online: https://www.theglobalfund.org/media/4762/core_tuberculosis_infonote_en.pdf (accessed on 1 June 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habib, S.S.; Jamal, W.Z.; Zaidi, S.M.A.; Siddiqui, J.-U.-R.; Khan, H.M.; Creswell, J.; Batra, S.; Versfeld, A. Barriers to Access of Healthcare Services for Rural Women—Applying Gender Lens on TB in a Rural District of Sindh, Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 10102. https://doi.org/10.3390/ijerph181910102
Habib SS, Jamal WZ, Zaidi SMA, Siddiqui J-U-R, Khan HM, Creswell J, Batra S, Versfeld A. Barriers to Access of Healthcare Services for Rural Women—Applying Gender Lens on TB in a Rural District of Sindh, Pakistan. International Journal of Environmental Research and Public Health. 2021; 18(19):10102. https://doi.org/10.3390/ijerph181910102
Chicago/Turabian StyleHabib, Shifa Salman, Wafa Zehra Jamal, Syed Mohammad Asad Zaidi, Junaid-Ur-Rehman Siddiqui, Hira Mustafa Khan, Jacob Creswell, Srichand Batra, and Anna Versfeld. 2021. "Barriers to Access of Healthcare Services for Rural Women—Applying Gender Lens on TB in a Rural District of Sindh, Pakistan" International Journal of Environmental Research and Public Health 18, no. 19: 10102. https://doi.org/10.3390/ijerph181910102
APA StyleHabib, S. S., Jamal, W. Z., Zaidi, S. M. A., Siddiqui, J.-U.-R., Khan, H. M., Creswell, J., Batra, S., & Versfeld, A. (2021). Barriers to Access of Healthcare Services for Rural Women—Applying Gender Lens on TB in a Rural District of Sindh, Pakistan. International Journal of Environmental Research and Public Health, 18(19), 10102. https://doi.org/10.3390/ijerph181910102






