Stroke and Athletes: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Definitions
2.2. Information Sources and Search Strategy
2.3. Literature Search
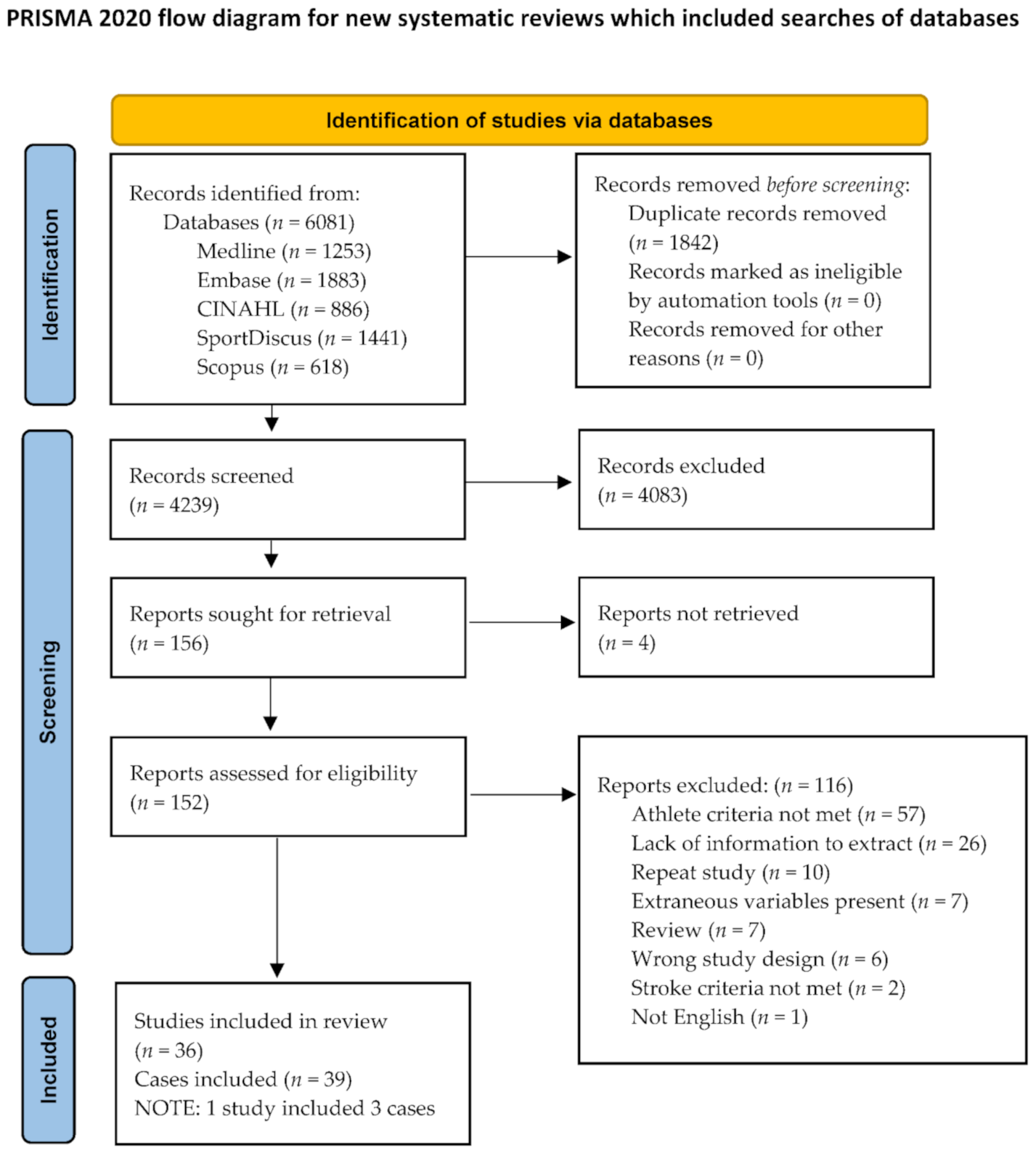
2.4. Study Selection
2.5. Charting the Data
3. Results
3.1. Search Results
3.2. Characteristics of Included Cases
3.3. Inciting Events Prior to Stroke
3.4. Vascular Mechanisms of Stroke
4. Discussion
4.1. Lifestyle Risk Factors
4.1.1. Performance Enhancing Drugs
4.1.2. Supplements
4.1.3. Hydration Status
4.2. Genetic Risk Factor
Genetic and Lifestyle Risk Factor
4.3. Sport and Stroke Triggers
4.3.1. Rugby Football
4.3.2. Boxing
4.3.3. American Football
4.3.4. Baseball
5. Summary
5.1. Implications or Future Directions
5.2. Limitations
5.3. Future Research
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Different Strokes—Heart and Stroke Foundation of Canada. Stroke Report. Stroke in Younger Adults. 2017. Available online: https://www.heartandstroke.ca/-/media/pdf-files/canada/stroke-report/strokereport2017en.ashx. (accessed on 5 July 2020).
- McCrory, P. Stroke in athletes. In Neurologic Athletic Head and Spine Injuries; Cantu, R., Ed.; WB Saunders & Co: Philadelphia, PA, USA, 1999. [Google Scholar]
- Rohr, J.; Kittner, S.; Feeser, B.; Hebel, J.R.; Whyte, M.G.; Weinstein, A.; Kanarak, N.; Buchholz, D.; Earley, C.; Johnson, C.; et al. Traditional risk factors and ischemic stroke in young adults: The Baltimore-Washington cooperative young stroke study. Arch. Neurol. 1996, 53, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Alexandrino, G.M.; Damásio, J.; Canhão, P.; Geraldes, R.; Melo, T.P.; Correia, C.; Ferro, J.M. Stroke in sports: A case series. J. Neurol. 2014, 261, 1570–1574. [Google Scholar] [CrossRef]
- Fragoso, Y.D.; Adoni, T.; Amaral, L.L.F.D.; Braga, F.T.; Brooks, J.B.B.; Campos, C.S.; Comini-Frota, E.R.; Ferreira, N.P.F.D.; Giacon, L.M.T.; Gomes, S.; et al. Cerebrum-cervical arterial dissection in adults during sports and recreation. Arq. Neuro-Psiquiatr. 2016, 74, 275–279. [Google Scholar] [CrossRef]
- Chippenham Hospital Blog. 9 Athletes under 40 Who Suffered a Stroke. Available online: https://chippenhammed.com/blog/entry/9-athletes-under-40-who-suffered-strokes (accessed on 31 August 2020).
- Florek, A.G.; Dellavalle, R.P. Case reports in medical education: A platform for training medical students, residents, and fellows in scientific writing and critical thinking. J. Med. Case Rep. 2016, 10. [Google Scholar] [CrossRef]
- Grau, A.J.; Barth, C.; Geletneky, B.; Ling, P.; Palm, F.; Lichy, C.; Becher, H.; Buggle, F. Association between recent sports activity, sports activity in young adulthood, and stroke. Stroke 2008, 40, 426–431. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peters, M.D.J.; Godfrey, C.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Araujo, C.G. The Terms “Athletes” and ‘Exercisers”. 2016. Available online: https://www.acc.org/latest-in-cardiology/articles/2016/06/27/07/06/the-terms-athlete-and-exercisers (accessed on 31 August 2020).
- Abbott, A.L.; Silvestrini, M.; Topakian, R.; Golledge, J.; Brunser, A.M.; de Borst, G.J.; Harbaugh, R.E.; Doubal, F.N.; Rundek, T.; Thapar, A.; et al. Optimizing the definitions of stroke, transient ischemic attack, and infarction for research and application in clinical practice. Front. Neurol. 2017, 8, 537. [Google Scholar] [CrossRef]
- Aho, K.; Harmsen, P.; Hatano, S.; Marquardsen, J.; Smirnov, V.E.; Strasser, T. Cerebrovascular disease in the community: Results of a WHO collaborative study. Bull. World Health Organ. 1980, 58, 113–130. [Google Scholar]
- Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://training.cochrane.org/handbook/current/chapter-04#section-4-6 (accessed on 30 October 2020).
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBL, 2020; Available online: https://synthesismanual.jbi.global (accessed on 5 July 2020). [CrossRef]
- Meeuwisse, W.H. Assessing causation in sport injury: A multifactorial model. Clin. J. Sport Med. 1994, 46, 166–170. [Google Scholar] [CrossRef]
- Rogers, L.; Sweeney, P.J. Stroke: A neurologic complication of wrestling: A case of brainstem stroke in a 17-year-old athlete. Am. J. Sports Med. 1979, 7, 352–354. [Google Scholar] [CrossRef]
- Phillips, J.; Horner, B.; Doorly, T.; Toland, J. Cerebrovascular accident in a 14-year-old marathon runner. Br. Med J. Clin. Res. Ed. 1983, 286, 351–352. [Google Scholar] [CrossRef]
- Fields, W.; Lemak, N.A.; Ben-Menachem, Y. Thoracic outlet syndrome: Review and reference to stroke in a major league pitcher. Am. J. Roentgenol. 1986, 146, 809–814. [Google Scholar] [CrossRef]
- Weinstein, S.M.; Cantu, R.C. Cerebral stroke in a semi-pro football player: A case report. Med. Sci Sports Exerc. 1991, 23, 1119–1121. [Google Scholar] [CrossRef] [PubMed]
- Litt, D.W. Acute subdural hematoma in a high school football player. J. Athl. Train. 1995, 30, 69. [Google Scholar]
- Mann, S.J.; Callaway, H.; Barnes, R.P.; Warren, R. Lacunar stroke in a hypertensive football player: Implications in managing hypertension in athletes. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 1997, 7, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Kersey, R.D. Acute subdural hematoma after a reported mild concussion: A case report. J. Athl. Train. 1998, 33, 264–268. [Google Scholar]
- Malek, A.M.; Halbach, V.V.; Phatouros, C.C.; Meyers, P.M.; Dowd, C.F.; Higashida, R.T. Endovascular treatment of a ruptured intracranial dissecting vertebral aneurysm in a kickboxer. J. Trauma Acute Care Surg. 2000, 48, 143. [Google Scholar] [CrossRef]
- Bruzzone, E.; Cocito, L.; Pisani, R. Intracranial delayed epidural hematoma in a soccer player: A case report. Am. J. Sports Med. 2000, 28, 901–903. [Google Scholar] [CrossRef] [PubMed]
- McCrory, P. Vertebral artery dissection causing stroke in sport. J. Clin. Neurosci. 2000, 7, 298–300. [Google Scholar] [CrossRef]
- Foxford, R.J.; Sahlas, D.J.; Wingfield, K.A. Vasospasm-induced stroke in a varsity athlete secondary to ephedrine ingestion. Clin. J. Sport Med. 2003, 13, 183–185. [Google Scholar] [CrossRef]
- De Giorgio, F.; Vetrugno, G.; De Mercurio, D.D.; Pascali, V.L.; Rainio, J.; Carbone, A.; Fernandez, E. Dissection of the vertebral artery during a basketball game: A case report. Med. Sci. Law. 2004, 44, 80–86. [Google Scholar] [CrossRef]
- Petzold, A.; Keir, G.; Appleby, I. Marathon related death due to brainstem herniation in rehydration-related hyponatraemia: A case report. J. Med. Case Rep. 2007, 1, 186. [Google Scholar] [CrossRef]
- Kanwar, M.; Desai, D.; Joumaa, M.; Guduguntla, V. Traumatic brachiocephalic pseudoaneurysm presenting as stroke in a seventeen-year-old. Clin. Cardiol. 2009, 32, E43–E45. [Google Scholar] [CrossRef]
- Miyazawa, A.; Vardiman, P.; Magee, L.M.; Washington, E. Cryptogenic stroke associated with patent foramen ovale in a collegiate volleyball athlete: A case report. Sports Health 2010, 2, 395–397. [Google Scholar] [CrossRef]
- Cohen, J.E.; Margolin, E.; Moscovici, S.; Paldor, I.; Itshayek, E. Life-threatening massive subarachnoid hemorrhage after Taekwondo-associated head trauma. Isr. Med. Asso. J. 2010, 12, 509–510. [Google Scholar]
- Smith, H. Physician as patient. In Sleep, Stroke and Cardiovascular Disease; Culebras, A., Ed.; Cambridge University Press: Cambridge, UK, 2012; pp. 151–154. [Google Scholar] [CrossRef]
- Hart, M.G.; Trivedi, R.A.; Hutchinson, P. Boxing sparring complicated by an acute subdural haematoma and brainstem haemorrhage. Br. J. Neurosurg. 2012, 26, 776–778. [Google Scholar] [CrossRef]
- Matsumoto, H.; Yoshida, Y. Posttraumatic cerebellar infarction after repeated sport-related minor head injuries in a young adult: A case report. Neurol. Med-Chir. 2015, 55, 179–182. [Google Scholar] [CrossRef]
- Nelson, J.A.; Ho, C.Y.; Golomb, M.R. Spinal cord stroke presenting with acute monoplegia in a 17-year-old tennis player. Pediatric Neurol. 2016, 56, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Degen, R.M.; Fink, M.E.; Callahan, L.; Fibel, K.; Ramsay, J.; Kelly, B.T. Internal carotid artery dissection after indirect blunt cervical trauma in an ice hockey goaltender. Am. J. Orthop. (Belle Mead NJ) 2017, 46, E139. [Google Scholar]
- Esianor, B.I.; Haider, A.S.; Engelhardt, M.I.; Osumah, T.; Vayalumkal, S.; Thakur, R.; Leonard, D.; Haithcock, J.; Layton, K.F. Intracranial ischemic infarct due to blunt force trauma in a high school football player. Cureus 2017, 9. [Google Scholar] [CrossRef]
- Demartini, Z.; Rodrigues Freire, M.; Lages, R.O.; Francisco, A.N.; Nanni, F.; Maranha Gatto, L.A.; Koppe, G.L. Internal carotid artery dissection in Brazilian jiu-jitsu. J. Cerebrovasc. Endovasc. Neurosurg. 2017, 19, 111–116. [Google Scholar] [CrossRef]
- Ellis, M.J.; Barnes, J.; Cordingley, D.M.; Bunge, M.; McDonald, P.J.; Ritchie, L. Management of an adolescent athlete with sports-related concussion and intraparenchymal hemorrhage. Curr. Sports Med. Rep. 2018, 17, 7–9. [Google Scholar] [CrossRef]
- Kumar, G.; Ludwig, B.; Patel, V.V. Vertebral artery dissection masquerading as concussion in an adolescent. Pediatric Emerg. Care 2018, 34, e97–e99. [Google Scholar] [CrossRef]
- Kariyana, P.T.; Charles, A.; Ahmed, M.F.; Jayarangaiah, A.; Das, S.; Al-Sadawi, M.; McFarlane, S.I. Rare case of bilateral cerebellar hemorrhage in a male boxer. Am. J. Med Case Rep. 2019, 7, 236. [Google Scholar] [CrossRef][Green Version]
- Cheng, C.D.; Gu, X.; Li, H.X.; Duan, R.Y.; Sun, L.; Zhang, Y.; Zhu, Y. Can men with atrial fibrillation really rest easy with a CHA2 DS2-VASc score of 0? BMC Cardiovasc. Disord. 2019, 19, 178. [Google Scholar] [CrossRef]
- David, M.; Rindlisbacher, T. Return to play considerations following spontaneous subarachnoid hemorrhage: A case report. Spor Hekim. Dergisi. 2020, 55, 52–55. [Google Scholar] [CrossRef]
- Muthalagappan, S.; Robbins, T.; Mehta, H.; Murthy, N. Facial twitching: Calcium or concussion conundrum? Hypocalcaemia in a young American football player masking an internal carotid artery dissection. BMJ Case Rep. 2020, 13. [Google Scholar] [CrossRef]
- Nack, W. Now Everyone Believes Him. It Took a Near-Fatal Stroke to Convince Doubters That Houston’s J.R. Richard Wasn’t Faking When He Complained of Arm Troubles. 1980. Available online: https://vault.si.com/vault/1980/08/18/now-everyone-believes-him-it-took-a-near-fatal-stroke-to-convince-doubters-that-houstons-jr-richard-wasnt-faking-when-he-complained-of-arm-troubles (accessed on 30 October 2020).
- Cannella, S. Inside Baseball. 2002. Available online: https://vault.si.com/vault/2002/04/22/inside-baseball (accessed on 5 July 2020).
- Schmidt, M.S.; Caldwell, D. High school football player dies. Sports Illus. 2008, 109, 18–19. Available online: https://www.nytimes.com/2008/10/17/sports/17preps.html (accessed on 5 July 2020).
- Holland, T.; Broudy, O. The death and life of Nick Chisholm. Men’s Health 2010, 25, 180. Available online: https://www.menshealth.com/trending-news/a19543391/nick-chisholm/ (accessed on 5 July 2020).
- Beresini, E. Flatline to Finish Line: Triathlete Faces Heart Disorder, Becomes Ironman. 2013. Available online: https://www.triathlete.com/culture/people/flatline-to-finish-line-triathlete-shakes-off-cardiac-problems-to-become-an-ironman/ (accessed on 5 July 2020).
- Pilcher, K.J. Upper Iowa’s Maleek Williams Overcomes Early-Season Stroke to Reach NCAA Championships. 2016b. Available online: https://www.thegazette.com/subject/sports/upper-iowas-maleek-williams-overcomes-early-season-stroke-to-reach-ncaa-championships-20160309 (accessed on 5 July 2020).
- Corhern, T. Tennessee Tech’s Josh Poplar Finds Deeper Meaning Following Stroke. 2017. Available online: https://www.ncaa.com/news/football/article/2017-08-22/college-football-tennessee-techs-josh-poplar-finds-deeper-meaning (accessed on 5 July 2020).
- Boehme, A.K.; Esenwa, C.; Elkind, M.S. Stroke risk factors, genetics, and prevention. Circ. Res. 2017, 120, 472–495. [Google Scholar] [CrossRef]
- Maron, B.J.; Bodison, S.A.; Wesley, Y.E.; Tucker, E.; Green, K.J. Results of screening a large group of intercollegiate competitive athletes for cardiovascular disease. J. Am. Coll. Cardiol. 1987, 10, 1214–1221. [Google Scholar] [CrossRef]
- Blomqvist, C.G.; Saltin, B. Cardiovascular adaptations to physical training. Annu. Rev. Physiol. 1983, 45, 169–189. [Google Scholar] [CrossRef]
- Alén, M. Androgenic steroid effects on liver and red cells. Br. J. Sports Med. 1985, 19, 15–20. [Google Scholar] [CrossRef]
- Ghuran, A.; Nolan, J. Recreational drug misuse: Issues for the cardiologist. Heart 2000, 83, 627. [Google Scholar] [CrossRef] [PubMed]
- Hallstrom, A.P.; Cobb, L.A.; Ray, R. Smoking as a risk factor for recurrence of sudden cardiac arrest. N. Engl. J. Med. 1986, 314, 271–275. [Google Scholar] [CrossRef]
- NIDA. References. 2020. Available online: https://www.drugabuse.gov/publications/research-reports/steroids-other-appearance-performance-enhancing-drugs-apeds/references (accessed on 22 September 2020).
- Baggish, A.L.; Weiner, R.B.; Kanayama, G.; Hudson, J.I.; Lu, M.T.; Hoffman, U.; Pope, H.G., Jr. Cardiovascular toxicity of illicit anabolic-androgenic steroid use. Circulation 2017, 135, 1991–2002. [Google Scholar] [CrossRef]
- Santamarina, R.D.; Besocke, A.G.; Romano, L.M.; Ioli, P.L.; Gonorazky, S.E. Ischemic stroke related to anabolic abuse. Clin. Neuropharmacol. 2008, 31, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Tsatsakis, A.; Docea, A.O.; Calina, D.; Tsarouhas, K.; Zamfira, L.M.; Mitrut, R.; Sharifi-Rad, J.; Kovatsi, L.; Siokas, V.; Dardiotis, E.; et al. A mechanistic and pathophysiological approach for stroke associated with drugs of abuse. J. Clin. Med. 2019, 8, 1295. [Google Scholar] [CrossRef]
- Frati, P.; Busardò, F.P.; Cipolloni, L.; Dominicis, E.D.; Fineschi, V. Anabolic androgenic steroid (AAS) related deaths: Autoptic, histopathological and toxicological findings. Curr. Neuropharmacol. 2015, 13, 146–159. [Google Scholar] [CrossRef] [PubMed]
- Christou, G.A.; Christou, K.A.; Nikas, D.N.; Goudevenos, J.A. Acute myocardial infarction in a young bodybuilder taking anabolic androgenic steroids: A case report and critical review of the literature. Eur. J. Prev. Cardiol. 2016, 23, 1785–1796. [Google Scholar] [CrossRef]
- Bouchard, R.; Weber, A.R.; Geiger, J.D. Informed decision-making on sympathomimetic use in sport and health. Clin. J. Sport Med. 2002, 12, 209–224. [Google Scholar] [CrossRef]
- Canadian Centre for Ethics in Sport. Should You Use Supplements? Canadian Centre for Ethics in Sport Advisory. Available online: http://www.cces.ca (accessed on 20 July 2020).
- Pipe, A.; Ayotte, C. Nutritional supplements and doping. Clin. J. Sport Med. 2002, 12, 245–249. [Google Scholar] [CrossRef]
- Perrotta, D.M. Adverse events associated with ephedrine-containing products: Texas, December 1993–September 1995. JAMA 1996, 276, 1711–1712. [Google Scholar]
- Wooltorton, E.; Sibbald, B. Ephedra/ephedrine: Cardiovascular and CNS effects. CMAJ 2002, 166, 633. Available online: https://www.cmaj.ca/content/166/5/633 (accessed on 5 July 2020).
- Haller, C.A.; Benowitz, N.L. Adverse cardiovascular and central nervous system events associated with dietary supplements containing ephedra alkaloids. N. Engl. J. Med. 2000, 343, 833–838. [Google Scholar] [CrossRef]
- Powers, M.E. Ephedra and its application to sport performance: Another concern for the athletic trainer? J. Athl. Train. 2001, 36, 420–424. [Google Scholar]
- Pedoe, D.T.; Wyse, R.H. Marathon running and creatine kinase levels. Lancet 1982, 320, 154–155. [Google Scholar] [CrossRef]
- Kalita, J.; Singh, R.K.; Misra, U.K. Cerebral salt wasting is the most common cause of hyponatremia in stroke. J. Stroke Cerebrovasc. Dis. 2017, 26, 1026–1032. [Google Scholar] [CrossRef]
- Wu, F.F.; Hung, Y.C.; Tsai, Y.H.; Yang, J.T.; Lee, T.H.; Liow, C.W.; Lee, J.D.; Lin, C.J.; Peng, T.I.; Lin, L.C. The influence of dehydration on the prognosis of acute ischemic stroke for patients treated with tissue plasminogen activator. BMC Cardiovasc. Disord. 2017, 17, 154. [Google Scholar] [CrossRef]
- Tucker, R. Dangerous exercise: The hype of dehydration and heatstroke. Sci. Sport Part Guard. Sport Netw. 2013. Available online: https://www.theguardian.com/sport/blog/2013/jan/14/dangerous-exercise-dehydration-heatstroke-sport-network (accessed on 5 July 2020).
- Hew-Butler, T.; Loi, V.; Pani, A.; Rosner, M.H. Exercise-associated hyponatremia: 2017 update. Front. Med. 2017, 4, 21. [Google Scholar] [CrossRef] [PubMed]
- Watso, J.C.; Farquhar, W.B. Hydration status and cardiovascular function. Nutrients 2019, 11, 1866. [Google Scholar] [CrossRef] [PubMed]
- Ehtesham, M.; Mohmand, M.; Raj, K.; Hussain, T.; Kavita, F.N.U.; Kumar, B. Clinical spectrum of hyponatremia in patients with stroke. Cureus 2019, 11, 8. [Google Scholar] [CrossRef]
- Wasfy, M.M.; Hutter, A.M.; Weiner, R.B. Sudden cardiac death in athletes. Methodist DeBakey Cardiovasc. J. 2016, 12, 76–80. [Google Scholar] [CrossRef]
- Mandola, J. Young People, Stroke, and Hole in the Heart (PFO). 2017. Available online: https://www.drjohnm.org/category/doctoring/ (accessed on 5 July 2020).
- Schneider, R.C. Serious and fatal neurosurgical football injuries. Clin. Neurosurg. 1964, 12, 226–236. [Google Scholar] [CrossRef]
- Pilcher, C.A. Perspective: Posterior Circulation Stroke—Why Is It Missed? 2016a. Available online: https://pilchermd.com/2016/02/06/perspective-posterior-circulation-stroke-missed/ (accessed on 5 July 2020).
- Strege, R.J.; Kiefer, R.; Herrmann, M. Contributing factors to quality of life after vertebral artery dissection: A prospective comparative study. BMC Neurol. 2019, 19, 312. [Google Scholar] [CrossRef]
- Sturzenegger, M. Headache and neck pain: The warning symptoms of vertebral artery dissection. Headache J. Head Face Pain 1994, 34, 187–193. [Google Scholar] [CrossRef]
- Blennow, K.; Hardy, J.; Zetterberg, H. The neuropathology and neurobiology of traumatic brain injury. Neuron 2012, 76, 886–899. [Google Scholar] [CrossRef] [PubMed]
- Falvey, É.C.; McCrory, P. Because not all blows to the head are the same. Br. J. Sports Med. 2015, 49, 1091–1093. [Google Scholar] [CrossRef]
- Atha, J.; Yeadon, M.R.; Sandover, J.; Parsons, K.C. The damaging punch. BMJ Clin. Res. Ed. 1985, 291, 1756–1757. [Google Scholar] [CrossRef]
- Corsellis, J.A.; Bruton, C.J.; Freeman-Browne, D. The aftermath of boxing. Psychol. Med. 1973, 3, 270–303. [Google Scholar] [CrossRef]
- Constantoyannis, C.; Partheni, M. Fatal head injury from boxing: A case report from Greece. Br. J. Sports Med. 2004, 38, 78–79. [Google Scholar] [CrossRef] [PubMed]
- May, T.; Foris, L.A.; Donnally, C.J., III. Second Impact Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK448119/ (accessed on 5 January 2021).
- Harmon, K.G.; Drezner, J.A.; Gammons, M.; Guskiewicz, K.M.; Halstead, M.; Herring, S.A.; Kutcher, J.S.; Pana, A.; Putukian, M.; Roberts, W.O. American Medical Society for Sports Medicine position statement: Concussion in sport. Br. J. Sports Med. 2013, 47, 15–26. [Google Scholar] [CrossRef]
- Chrisman, S.P.; Quitiquit, C.; Rivara, F.P. Qualitative study of barriers to concussive symptom reporting in high school athletics. J. Adolesc. Health 2013, 52, 330–335. [Google Scholar] [CrossRef]
- Chandra, V.; Little, C.; Lee, J.T. Thoracic outlet syndrome in high-performance athletes. J. Vasc. Surg. 2014, 60, 1012–1018. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. Shoulder injuries in overhead athletes: The “dead arm” revisited. Clin. Sports Med. 2000, 19, 125–158. [Google Scholar]
- Meumann, E.M.; Chuen, J.; Fitt, G.; Perchyonok, Y.; Pond, F.; Dewey, H.M. Thromboembolic stroke associated with thoracic outlet syndrome. J. Clin. Neurosci. 2013, 21, 886–889. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.T.; Bieuzen, F.; Bleakley, C.M. Where are all the female participants in sports and exercise medicine research? Eur. J. Sport Sci. 2014, 14, 847–851. [Google Scholar] [CrossRef]
- Gupta, V.; Dhawan, N.; Bahl, J. Minor trauma causing stroke in a young athlete. Case Rep. Neurol Med. 2015, 182875. [Google Scholar] [CrossRef]
- Patel, D.R.; Shivdasani, V.; Baker, R.J. Management of sport-related concussion in young athletes. Sports Med. 1995, 35, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Morales Vidal, S.; Lara, C.; Gordin, A. Sequential bilateral vertebral artery dissections with prompt resolution of initial insult. Case Rep. Neurol. 2020, 12, 189–198. [Google Scholar] [CrossRef]
- Hathidara, M.Y.; Saini, V.; Malik, A.M. Stroke in the young: A global update. Curr. Neurol. Neurosci. Rep. 2019, 19, 91. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.P.; Jenkinson, A.J.; Leathley, M.J.; Watkins, C.L. Stroke knowledge and awareness: An integrative review of the evidence. Age Ageing 2010, 39, 11–22. [Google Scholar] [CrossRef]
- Saw, A.E.; McIntosh, A.S.; Kountouris, A.; Newman, P.; Gaida, J.E. Vertebral artery dissection in sport: A systematic review. Sports Med. 2019, 49, 553–564. [Google Scholar] [CrossRef]
- Suzuki, S.; Tsuchimochi, R.; Abe, G.; Yu, I.; Inoue, T.; Ishibashi, H. Traumatic vertebral artery dissection in high school rugby players: A report of two cases. J. Clin. Neurosci. 2018, 47, 137–139. [Google Scholar] [CrossRef] [PubMed]
- Pinkerton, J.A., Jr.; MacGee, E.E.; Romine, K.G. Traumatic aneurysm of the intrathoracic left carotid artery with cerebral embolization. J. Trauma 1977, 17, 975–977. [Google Scholar] [CrossRef]
- Cruikshank, J.K.; Higgins, C.S.; Gray, J.H. Two cases of acute intracranial haemorrhage in young amateur boxers. Lancet 1980, 1, 626–627. [Google Scholar] [CrossRef]
- Franks, A.J.; Hiss, J.; Sivaloganathan, S. Congenital absence of the left vertebral artery with traumatic thrombosis of the right artery. Med. Sci. Law 1987, 27, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Kohno, K. Posttraumatic cerebral infarction due to progressive occlusion of the internal carotid artery after minor head injury in childhood: A case report. Child’s Nerv. Syst. 2011, 27, 1169. [Google Scholar] [CrossRef]
- Lu, A.; Shen, P.; Lee, P.; Dahlin, B.; Waldau, B.; Nidecker, A.E.; Nundkumar, A.; Bobinski, M. CrossFit-related cervical internal carotid artery dissection. Emerg. Radiol. 2015, 22, 449–452. [Google Scholar]
- Davidson, E.; Rotenbeg, Z.; Fuchs, J.; Weinberger, I.; Agmon, J. Transient ischemic attack-related syncope. Clin Cardiol. 1991, 2, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Gliklich, R.E.; Dreyer, N.A.; Leavy, M.B. Registries for Evaluating Patient Outcomes: A User’s Guide, 3rd ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK208609 (accessed on 5 November 2020).
- Block, C.K.; West, S.E.; Goldin, Y. Misconceptions and misattributions about traumatic brain injury: An integrated conceptual framework. Phys. Med. Rehabil. 2016, 8, 58–68. [Google Scholar] [CrossRef] [PubMed]
- McCarron, M.O.; Patterson, J.; Duncan, R. Stroke without dissection from a neck holding manoeuvre in martial arts. Br. J. Sports Med. 1997, 31, 346–347. [Google Scholar] [CrossRef]
- Kerwin, A.J.; Bynoe, R.P.; Murray, J.; Hudson, E.R.; Close, T.P.; Gifford, R.M.; Carson, K.W.; Smith, L.P.; Bell, R.M. Liberalized screening for blunt carotid and vertebral artery injuries is justified. J. Trauma 2001, 1, 308–314. [Google Scholar] [CrossRef]
- Newman-Toker, D.E.; Moy, E.; Valente, E.; Coffey, R.; Hines, A.L. Missed diagnosis of stroke in the emergency department: A cross-sectional analysis of a large population-based sample. Diagnosis (Brel) 2014, 1, 155–166. [Google Scholar] [CrossRef]
| Year | Author | Country | Sport | Age | Inciting Event |
|---|---|---|---|---|---|
| (A) | |||||
| 1979 [19] | Rogers | USA | Wrestling | 17 | 10 days prior to admission participated in neck “bridging” exercises by using the top of the head as a fulcrum. During a wrestling match was placed in several neck holds, and developed vertigo, ataxia, and numbness associated tingling on the left face and body half. Athlete was unable to swallow fluids. |
| 1983 [20] | Phillips | UK | Marathon | 14 | After 10 miles of running felt unwell, developed heaviness in right leg, and collapsed with right-sided weakness. On hospital arrival was alert although dysphasic with right hemiplegia. |
| 1986 [21] | Fields | USA | Baseball | 30 | Thoracic outlet syndrome with Raynaud phenomenon: compressed subclavian artery leading to thrombosed/foci |
| 1991 [22] | Weinstein | USA | Football | 29 | Forced cervical flexion injury; 10 days prior to evaluation. |
| 1995 [23] | Litt | USA | Football | 16 | Headache following a collision on the last play of the game; continued to complain of a headache the following week. Cleared for play, blindsided in another game followed by dizziness and headache with projectile vomiting; become pale and unresponsive. |
| 1997 [24] | Mann | USA | Football | 28 | Slurring of speech and tendency to veer to the right post 60 min after a game. Over the next few days slurred speech persisted and experienced a mild headache and lethargy. |
| 1998 [25] | Kersey | USA | Football | 19 | Mild concussion sustained during a game. Disclosed to trainer had mild to moderate headaches -left sided and sometimes associated with nausea. Persisted for 12 days and 5 weeks later sustained a head injury in game followed by immediate head pain, vertigo, and bilateral leg paresthesia. |
| 2000 [26] | Malek | USA | Kick Boxer | 42 | Ruptured intracranial dissecting vertebral aneurysm |
| 2000 [27] | Bruzzone | Italy | Soccer | 19 | Ball headed and crashed, striking right frontoparietal region against the opponent’s left frontal scalp. Fell to the ground, unconscious for 20 to 30 s. 20 min after was alert and conscious without neurologic deficit. Developed amnesia followed by nausea, vomiting, and headache. |
| 2000 [28] | McCrory | Australia | 1–2: AFB 3: Rugby League | 15; 20; 27 | 1. Struck on the right mastoid process by an elbow during the collision, collapsed and unconscious, died (subdural and subarachnoid hemorrhage). 2. Left side head blow; unconscious, died (subarachnoid hemorrhage). 3. Neck strike during a tackle, left the field complaining of arm “pins and needles” with deep neck pain. Originally refused medical treatment; became ataxic with slurred speech following morning. Discharged from the Emerg, no neurological abnormalities were found. Sought chiropractic treatment and after 3rd visit suddenly deteriorated with tinnitus, face alteration, slurred speech. Died in Emerg (vertebral arterial dissection) |
| 2003 [29] | Foxford | USA | Football | 24 | Ingestion of Xenadrine prior to football training. Severe right sided headache and vasospasm. |
| 2004 [30] | DeGiorgio | Italy | Basketball | 23 | Stiff neck complaint at the beginning of a practice, fell and lost consciousness. Taken to the Emerg. One-week general condition worsened and died. |
| 2007 [31] | Petzold | UK | Marathon | 30′s | Athlete suffered from a thunderclap headache, subsequently developed morning headaches. Collapsed following rehydration, went into respiratory arrest, became hyponatraemic and died of hydrocephalus and brain stem herniation. |
| 2009 [32] | Kanwar | USA | Football | 17 | Sudden onset of slurred speech and drooling during game warm up. Neurological defects were noted on the left side of face along with left-sided extremity weakness. History identified prior injury to the right shoulder 3 months earlier. |
| 2010 [33] | Miyazawa | USA | Volleyball | 22 | Presented with acute right-side facial droop, aphasia, loss of muscular control and sensation in the right upper extremity during a match. |
| 2010 [34] | Cohen | Israel | Taekwondo | 23 | During a championship match an attacker‘s heel kick landed on the unprotected nuchal region resulting in severe head trauma: athlete collapsed developed acute respiratory arrest. |
| 2012 [35] | Smith | Unknown | Running | ? | 50 plus miles per week. On an aborted training run experienced neurological confusion, diagnosed with right internal carotid artery dissection at Emerg Rehab followed with two pulmonary emboli. Some discussion about disrupted sleep architecture. |
| 2012 [36] | Hart | USA | Boxing | 23 | Headaches from sparring during training; no protective head gear. |
| 2015 [37] | Matsumoto | Japan | Football | 23 | Helmet collision during game. Experienced mild nausea/dizziness, resolved in 15-min and team director allowed him to RTS the next day. 3 days prior another head collision was encountered. |
| 2016 [38] | Nelson | USA | Tennis | 17 | Complained of back and left leg pain, followed by flaccid left leg paralysis after 1 week of heavy training. Spinal cord infarct: likely fibrocartilaginous embolism (monoplegia) |
| 2017 [39] | Degen | USA | Ice Hockey | 32 | Experienced discomfort and dizziness from falling to the ice. Symptoms resolved and continued to play. Two days post, complained of severe headache (frontotemporal) which persisted overnight. |
| 2017 [40] | Esianor | USA | Football | 16 | Transient loss of consciousness after two simultaneous head-to-head collisions during a game. |
| 2017 [41] | Demartini | Brazil | Brazilian Jiu-Jitsu | 27 | Presented to the Emerg with headache, right motor deficit, and aphasia, all commencing 16 h earlier. History showed severe neck pain one week earlier while practicing a submission maneuver known as the Rear Naked Choke or Lion Killer, with persistent pain locally thereafter. |
| 2018 [42] | Ellis | Canada | Soccer | 16 | Attempted to head the ball, fell backwards; head struck the goalpost. Knocked out followed by a 30 s seizure. |
| 2018 [43] | Kumar | USA | Wrestling | 16 | Headlock and “face-planted” into the mat; dazed and slow to stand. Complained of headache and nausea on route to hospital. Followed by persistent headache and uncontrolled vomiting. |
| 2019 [44] | Kariyanna | USA | Boxing | 26 | Knocked out: protective head gear slipped; Multiple strikes sustained to face and head. |
| 2019 [45] | Cheng | China | Table Tennis | 56 | Developed sudden syncope and right hemiplegia within 2 h of a match; admitted to Emerg. |
| 2020 [46] | David | Turkey | Ice Hockey | 17 | Severe Headache during final minute of game. |
| 2020 [47] | Muthalagappan | UK | Football | 30 | Seizure-like activity with hand and lip tingling in athlete with a history of Graves’ disease and previous thyroidectomy. Calcitriol, ergocalciferol and high dose levothyroxine were prescribed. |
| (B) | |||||
| 1980 [48] | Nack | USA | Pro Baseball | 30 | Dead arm followed by stroke 6 weeks later. |
| 2002 [49] | Cannella | USA | Pro Baseball | Pain in head resulting from cerebral hemorrhage. | |
| 2008 [50] | Schmidt | USA | Football | 16 | 3 weeks post-concussion, cleared to play, game tackle resulted in from cerebral hemorrhage. |
| 2010 [51] | Holland | USA | Rugby | 27 | Series of strokes likely triggered by a clot in vertebral artery which was pinched during a twist to pass the ball to the wing. |
| 2013 [52] | Beresini | USA | Former Football Collegiate/Marathoner | 32 | Collapsed in a triathlon. Bicuspid aortic valve: congenital disorder. |
| 2016b [53] | Pilcher | USA | Wrestling | 20 | During a practice developed partial paralysis to left side: facial droop, migraines, and slurred speech. |
| 2017 [54] | Corhern | USA | Football Collegiate | ? | Congenital disorder. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doyle-Baker, P.K.; Mitchell, T.; Hayden, K.A. Stroke and Athletes: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 10047. https://doi.org/10.3390/ijerph181910047
Doyle-Baker PK, Mitchell T, Hayden KA. Stroke and Athletes: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(19):10047. https://doi.org/10.3390/ijerph181910047
Chicago/Turabian StyleDoyle-Baker, Patricia K., Timothy Mitchell, and K. Alix Hayden. 2021. "Stroke and Athletes: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 19: 10047. https://doi.org/10.3390/ijerph181910047
APA StyleDoyle-Baker, P. K., Mitchell, T., & Hayden, K. A. (2021). Stroke and Athletes: A Scoping Review. International Journal of Environmental Research and Public Health, 18(19), 10047. https://doi.org/10.3390/ijerph181910047







