Can Face- and Smartphone-Touching Behaviors Be Altered with Personal Hygiene Reminders during the COVID-19 Pandemic Period? An Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
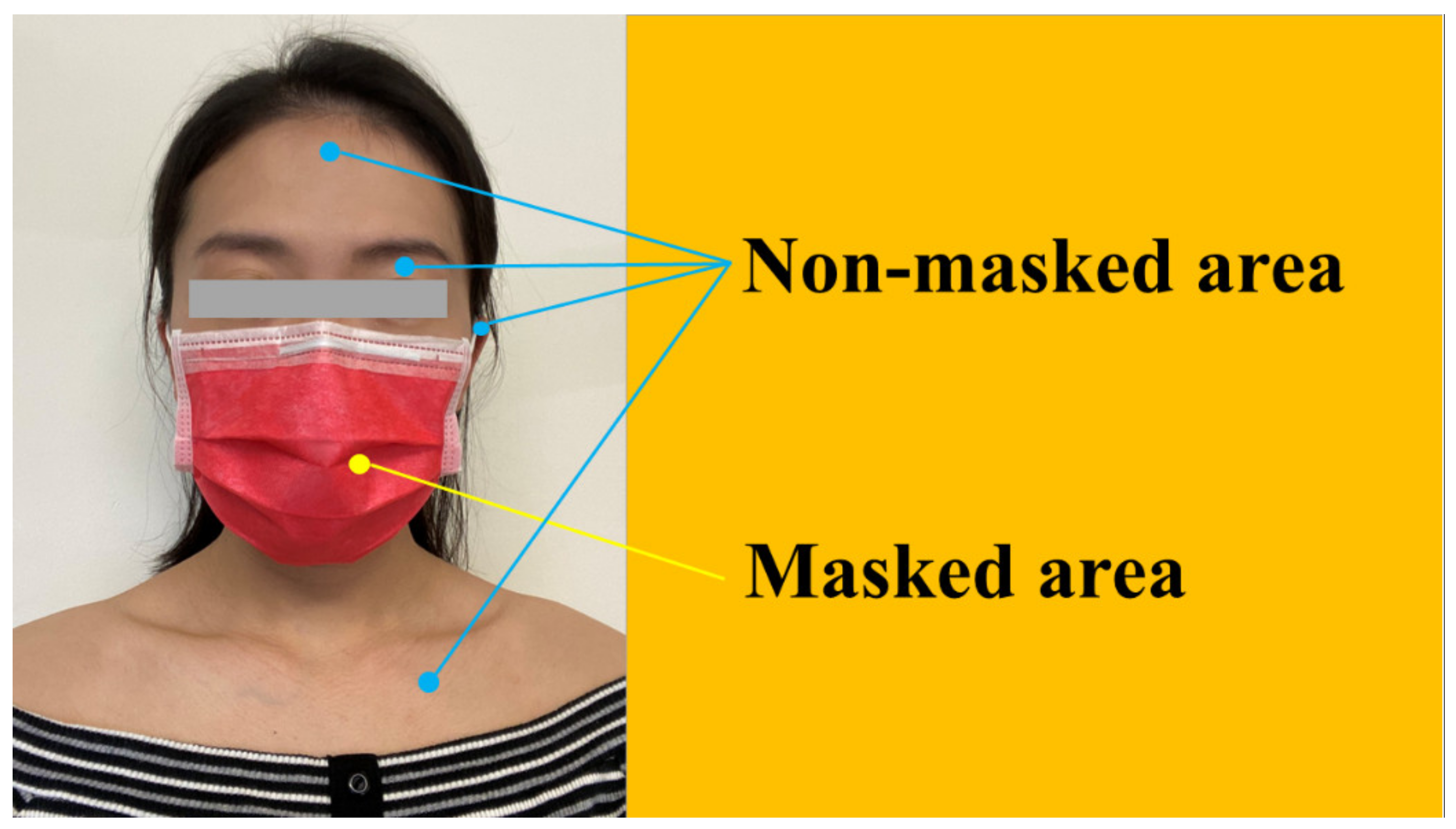
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Olsen, M.; Campos, M.; Lohning, A.; Jones, P.; Legget, J.; Bannach-Brown, A.; McKirdy, S.; Alghafri, R.; Tajouri, L. Mobile phones represent a pathway for microbial transmission: A scoping review. Travel Med. Infect. Dis. 2020, 35, 101704. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Advice on the Use of Masks in the Context of COVID-19. Interim Guidance 6 June 2020. Available online: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-careand-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (accessed on 10 July 2020).
- Wertheim, H.F.; Melles, D.C.; Vos, M.C.; van Leeuwen, W.; van Belkum, A.; Verbrugh, H.A.; Nouwen, J.L. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 2005, 5, 751–762. [Google Scholar] [CrossRef]
- Macias, A.E.; de la Torre, A.; Moreno-Espinosa, S.; Leal, P.E.; Bourlon, M.T.; Ruiz-Palacios, G.M. Controlling the novel A (H1N1) influenza virus: Don’t touch your face! J. Hosp. Infect. 2009, 73, 280–281. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Clinical Signs and Symptoms of Influenza: Influenza Prevention & Control Recommendations. Available online: www.cdc.gov/flu/professionals/acip/clinical.htm (accessed on 1 March 2014).
- Peltola, V.; Waris, M.; Osterback, R.; Susi, P.; Ruuskanen, O.; Hyypiä, T. Rhinovirus transmission within families with children: Incidence of symptomatic and asymptomatic infections. J. Infect. Dis. 2008, 197, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Peltola, V.; Waris, M.; Osterback, R.; Susi, P.; Hyypiä, T.; Ruuskanen, O. Clinical effects of rhinovirus infections. J. Clin. Virol. 2008, 43, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Thomas, Y.; Boquete-Suter, P.; Koch, D.; Pittet, D.; Kaiser, L. Survival of influenza virus on human fingers. Clin. Microbiol. Infect. 2014, 20, O58–O64. [Google Scholar] [CrossRef] [Green Version]
- Barasheed, O.; Almasri, N.; Badahdah, A.M.; Heron, L.; Taylor, J.; McPhee, K.; Ridda, I.; Haworth, E.; Dwyer, D.E.; Rashid, H.; et al. Hajj Research Team. Pilot Randomised Controlled Trial to Test Effectiveness of Facemasks in Preventing Influenza-like Illness Transmission among Australian Hajj Pilgrims in 2011. Infect. Disord. Drug Targets 2014, 14, 110–116. [Google Scholar] [CrossRef]
- Shiraly, R.; Shayan, Z.; McLaws, M.L. Face touching in the time of COVID-19 in Shiraz, Iran. Am. J. Infect. Control 2020, 48, 1559–1561. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chen, M.B.; Cui, W.Y.; Xu, H.L.; Zheng, Q.H. The efficacy of masks for influenza-like illness in the community: A protocol for systematic review and meta-analysis. Medicine 2020, 99, e20525. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J. COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Chughtai, A.A. A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int. J. Nurs. Stud. 2020, 108, 103629. [Google Scholar] [CrossRef] [PubMed]
- Machida, M.; Nakamura, I.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; Amagasa, S.; et al. Changes in implementation of personal protective measures by ordinary Japanese citizens: A longitudinal study from the early phase to the community transmission phase of the COVID-19 outbreak. Int. J. Infect. Dis. 2020, 96, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Qin, G.; Chen, J.; Xu, J.L.; Feng, D.Y.; Wu, X.Y.; Li, X. Comparison of Face-Touching Behaviors Before and During the Coronavirus Disease 2019 Pandemic. JAMA Netw. Open 2020, 3, e2016924. [Google Scholar] [CrossRef] [PubMed]
- Kwok, Y.L.; Gralton, J.; McLaws, M.L. Face touching: A frequent habit that has implications for hand hygiene. Am. J. Infect. Control 2015, 43, 112–114. [Google Scholar] [CrossRef] [PubMed]
- Wellenius, G.A.; Vispute, S.; Espinosa, V.; Fabrikant, A.; Tsai, T.C.; Hennessy, J.; Dai, A.; Williams, B.; Gadepalli, K.; Boulanger, A.; et al. Impacts of social distancing policies on mobility COVID-19 case growth in the, U.S. Nat. Commun. 2021, 12, 3118. [Google Scholar] [CrossRef] [PubMed]
| Before Personal Hygiene Reminder | After Personal Hygiene Reminder | p Value | |
|---|---|---|---|
| Total face-touching incidents | 777 | 441 | |
| Average face-touching incidents, mean ± 1 SD (%) | 9.71 ± 7.49 | 5.51 ± 4.07 | <0.01 |
| Total smartphone-touching incidents | 517 | 335 | |
| Average smartphone-touching incidents, mean ± 1 SD (%) | 6.46 ± 6.94 | 4.19 ± 3.86 | <0.01 |
| All Facial Areas | Masked Area | Unmasked Area | |
|---|---|---|---|
| Face-touching behavioral analysis before the delivery of a personal hygiene reminder | |||
| Total face-touching incidents | 777 | 291 | 486 |
| Average face-touching incidents, mean ± 1 SD (%) | 9.71 ± 7.49 | 3.64 ± 3.13 | 6.08 ± 5.35 |
| Face-touching behavioral analysis after the delivery of a personal hygiene reminder | |||
| Total face-touching incidents | 441 | 196 | 245 |
| Average face-touching incidents, mean ± 1 SD (%) | 5.51 ± 4.07 | 2.45 ± 3.09 | 3.06 ± 2.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, L.-Y.J.; Wang, S.-Y.; Yang, J.-M.; Chen, C.-J.; Tsai, C.-Y.; Wu, L.Y.-Y.; Wu, C.-J. Can Face- and Smartphone-Touching Behaviors Be Altered with Personal Hygiene Reminders during the COVID-19 Pandemic Period? An Observational Study. Int. J. Environ. Res. Public Health 2021, 18, 10038. https://doi.org/10.3390/ijerph181910038
Li L-YJ, Wang S-Y, Yang J-M, Chen C-J, Tsai C-Y, Wu LY-Y, Wu C-J. Can Face- and Smartphone-Touching Behaviors Be Altered with Personal Hygiene Reminders during the COVID-19 Pandemic Period? An Observational Study. International Journal of Environmental Research and Public Health. 2021; 18(19):10038. https://doi.org/10.3390/ijerph181910038
Chicago/Turabian StyleLi, Lok-Yee Joyce, Shin-Yi Wang, Jinn-Moon Yang, Chih-Jou Chen, Cheng-Yu Tsai, Lucas Yee-Yan Wu, and Cheng-Jung Wu. 2021. "Can Face- and Smartphone-Touching Behaviors Be Altered with Personal Hygiene Reminders during the COVID-19 Pandemic Period? An Observational Study" International Journal of Environmental Research and Public Health 18, no. 19: 10038. https://doi.org/10.3390/ijerph181910038
APA StyleLi, L.-Y. J., Wang, S.-Y., Yang, J.-M., Chen, C.-J., Tsai, C.-Y., Wu, L. Y.-Y., & Wu, C.-J. (2021). Can Face- and Smartphone-Touching Behaviors Be Altered with Personal Hygiene Reminders during the COVID-19 Pandemic Period? An Observational Study. International Journal of Environmental Research and Public Health, 18(19), 10038. https://doi.org/10.3390/ijerph181910038






